Abstract
Objectives
Fitting philosophies for toric orthokeratology are based on elevation or corneal astigmatism, but it is unclear which is more effective. The purpose of this analysis was to further understand corneal shape and the relationship between peripheral elevation and central astigmatism in moderate to high astigmats.
Methods
Corneal tomography was measured three times on the right eyes of 25 moderate to high refractive myopic astigmatic adults. Corneal astigmatism and elevation were calculated at 4, 6 and 8 mm chords. Subjects were fitted with toric orthokeratology lenses following the manufacturer’s guidelines based on elevation. Twenty subjects completed 10 days of wear. A masked examiner assessed movement and centration via slit-lamp videos and quantified treatment zone and decentration from tangential power difference tomography maps. Correlations between variables were assessed.
Results
Average corneal astigmatism was 2.20±0.70 DC and peripheral elevation was 50.88±18.92 μm and they were strongly correlated (4 mm R2=0.96, 6 mm R2=0.92, 8 mm R2=0.86, all p<0.001). Each diopter of astigmatism equated to 25 μm of elevation at an 8 mm chord. Via slit-lamp, average treatment zone area was 12.73±4.62 mm2 and 13 lenses decentered. From tomography, average treatment zone area was 7.16±2.56 mm2 and 17 were decentered. Tomography treatment zone area was negatively correlated with central corneal astigmatism (R2=0.60) and elevation at an 8 mm chord (R2=0.64, both p<0.001).
Conclusions
For tomography images, central corneal astigmatism was highly correlated with peripheral elevation and may be a more expedient measure for clinical use. Treatment area decreased as corneal astigmatism and elevation increased.
Keywords: corneal elevation, astigmatism, orthokeratology, treatment zone, tomography
Modern overnight orthokeratology uses a reverse geometry gas permeable lens to flatten the central cornea to temporarily correct myopia. The reverse geometry design has a flatter central base curve, surrounded by a steeper secondary curve.1 The presence of astigmatism poses a challenge to traditional spherical orthokeratology because of the significant difference in corneal shape between the steep and flat axes.2,3 Spherical orthokeratology is not intended for corneal astigmatism greater than 1.50 D due to lens decentration and induced astigmatism.4 To attempt to address this issue, toric periphery orthokeratology lenses have two curvatures to align with the toric cornea.5,6
Clinical fitting guidelines for toric orthokeratology advise the use of either central corneal astigmatism or peripheral elevation difference. The paracentral zone is imperative in lens fitting because it is where the first alignment curve of the lens lands and it supports the weight of the lens, affecting lens stability and centration.7 Elevation is relative to a best-fit sphere that is calculated from the least squares method and can provide more information about the shape of the cornea.8,9 Previous studies have shown that the temporal cornea is steeper but lower in elevation than the nasal region, which may be the reason for temporal lens decentration.10,11
Many myopes are also astigmatic, having at least 1.00 D difference between the two principal meridians,12 with prevalence rates between 25 to 60%, depending on ethnicity.12–14 Therefore, the need for orthokeratology lenses to center appropriately and provide adequate treatment to the central corneal is crucial for allowing myopia control treatments for astigmatic children. Previous studies have examined spherical orthokeratology lenses on moderate to high astigmats (1.25 D or more of astigmatism),6 and found that they are more likely to decenter or induce astigmatism leading to decreased visual performance.15,16 To date, few studies have examined toric orthokeratology lenses on moderate astigmatic eyes but have suggested that peripheral toric lenses may partially correct astigmatism and, when successfully fitted would have similar myopia control effects as spherical orthokeratology.5,17,18 The purpose of this study was to further understand corneal shape and the relationship between peripheral elevation and central corneal astigmatism in moderate to high astigmats in order to improve the fitting process for myopic astigmats.
Methods
Subjects
A prospective, single-site study was conducted at the University of Houston College of Optometry. The inclusion criteria were adults, age 18 to 39 with myopia (plano to 5.00 DS), moderate to high astigmatism (1.25 to 3.50 DC), and no history of ocular disease or surgery. Subjects with gas permeable lens wear within the last month or with accommodative or binocular vision issues were excluded. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board. The study was registered on ClinicalTrials.gov (NCT03728218). All subjects were consented prior to beginning any assessments.
Clinical Measurements
To determine the relationship between anterior corneal elevation and astigmatism, the Oculus Pentacam HR (Oculus, Wetzlar, Germany) was used to collect three repeated measures19 on the right eye only. The Pentacam tomographer uses Scheimpflug technology to generate 50 sectional images yielding 138,000 distinct elevation values during a two second scan. Anterior keratometry values were recorded at the corneal apex, as well as 2, 3, and 4 mm from the apex along the principal meridians. The anterior corneal elevation values were also recorded at the same locations in reference to a best-fit sphere that is calculated by the instrument.
The difference between the average elevation value in the vertical meridian and the horizontal meridian at an 8 mm chord was calculated to define the total corneal elevation difference for each subject, as shown in Figure 1. Dual Axis Corneal Refractive Therapy (CRT) lenses (Paragon Vision Sciences, Gilbert, AZ) are approved by the United States Food and Drug Administration (FDA) for the correction of myopia up to 6.00 DS and astigmatism up to 1.75 DC in Paragon HDS 100 material. The calculated elevation difference was then used to empirically order a Dual Axis lens based on the recommended expansion of the manufacturer’s fitting guidelines (Table 1).20
Figure 1.
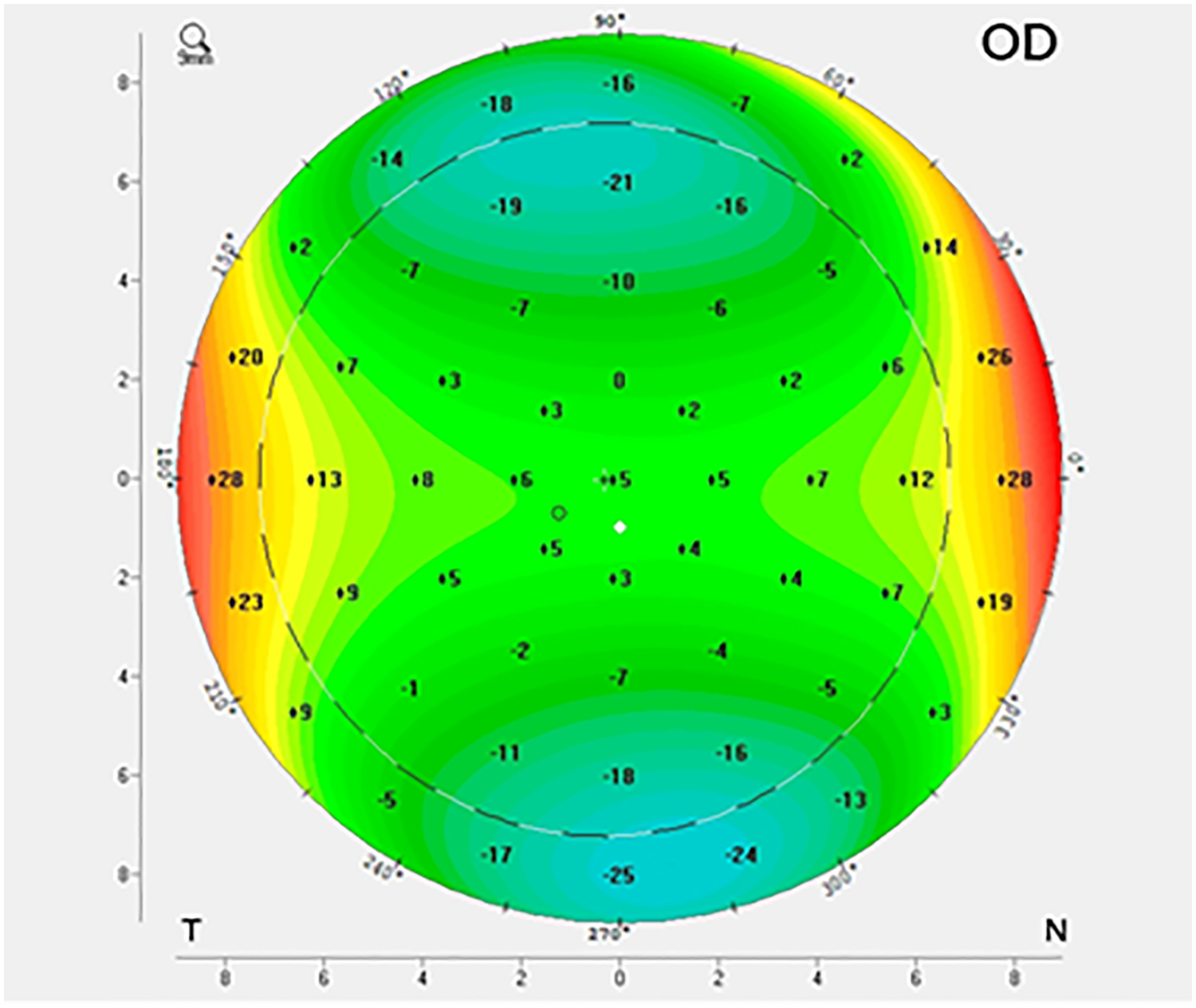
An elevation map showing the relative elevation in the vertical and horizontal meridians at an 8 mm chord. The difference between the average of the vertical and horizontal meridian is calculated.
Table 1.
Fitting guideline for Dual Axis CRT lens
| Elevation Difference in the Flat and Steep Meridians at 4 mm Reference Points | Steep RZD (Return Zone Depth) |
|---|---|
| 13–30 microns | 25 microns steeper than Flat RZD |
| 31–60 microns | 50 microns steeper than Flat RZD |
| > 61 microns | 75 microns steeper than Flat RZD |
The Return Zone Depth (RZD) is the reverse curve area of the lens that forms the mid-peripheral tear reservoir. This zone allows for proper fit and centration of the orthokeratology lens. The Return Zone Depth is toric in Dual Axis lenses.
At a subsequent visit, Dual Axis lenses were placed on the right eye and slit-lamp videos of the lens fit were recorded. The fit evaluation was performed with white light and with sodium fluorescein, cobalt blue light, and a standard yellow filter. The fit was deemed adequate to dispense if it demonstrated the classic bull’s eye pattern with an area of central bearing, mid-peripheral pooling, and adequate edge lift for lens movement.21 Although analysis was only performed on right eyes, both eyes were fitted with orthokeratology lenses. A pair of lenses were dispensed to the subject to be worn every day (10 ± 2 days),22 for a minimum of 7 hours each night.18,21,23 Although a first morning follow-up is often performed in clinical care, subjects were allowed to proceed without this follow-up due to the short duration of planned wear.24 Subjects were advised to contact the study investigators if they experienced any redness, pain, or problems with the contact lenses. Subjects then returned and were queried on hours of wear per night to ensure they met the minimum expected number of hours and Pentacam tomography was again repeated three times on the right eye and averaged.
Image Analysis
An examiner masked to the subject’s baseline astigmatism reviewed the slit-lamp videos of lens fits and tangential difference maps comparing tomography before and after lens wear. The fit videos were assessed for lens movement and centration. A screenshot of the video was captured and Image J (National Institutes of Health, Bethesda, MD) was used to measure the treatment zone area of the lens on eye by converting pixels of a known diameter (lens diameter) to millimeters. As well, Image J was used to measure the treatment zone area (Figure 2) and treatment zone decentration from pupil center using the tangential difference maps. The treatment zone was defined as the central flattened area not including the peripheral plus ring. The pupil was outlined by the tomography software.
Figure 2.
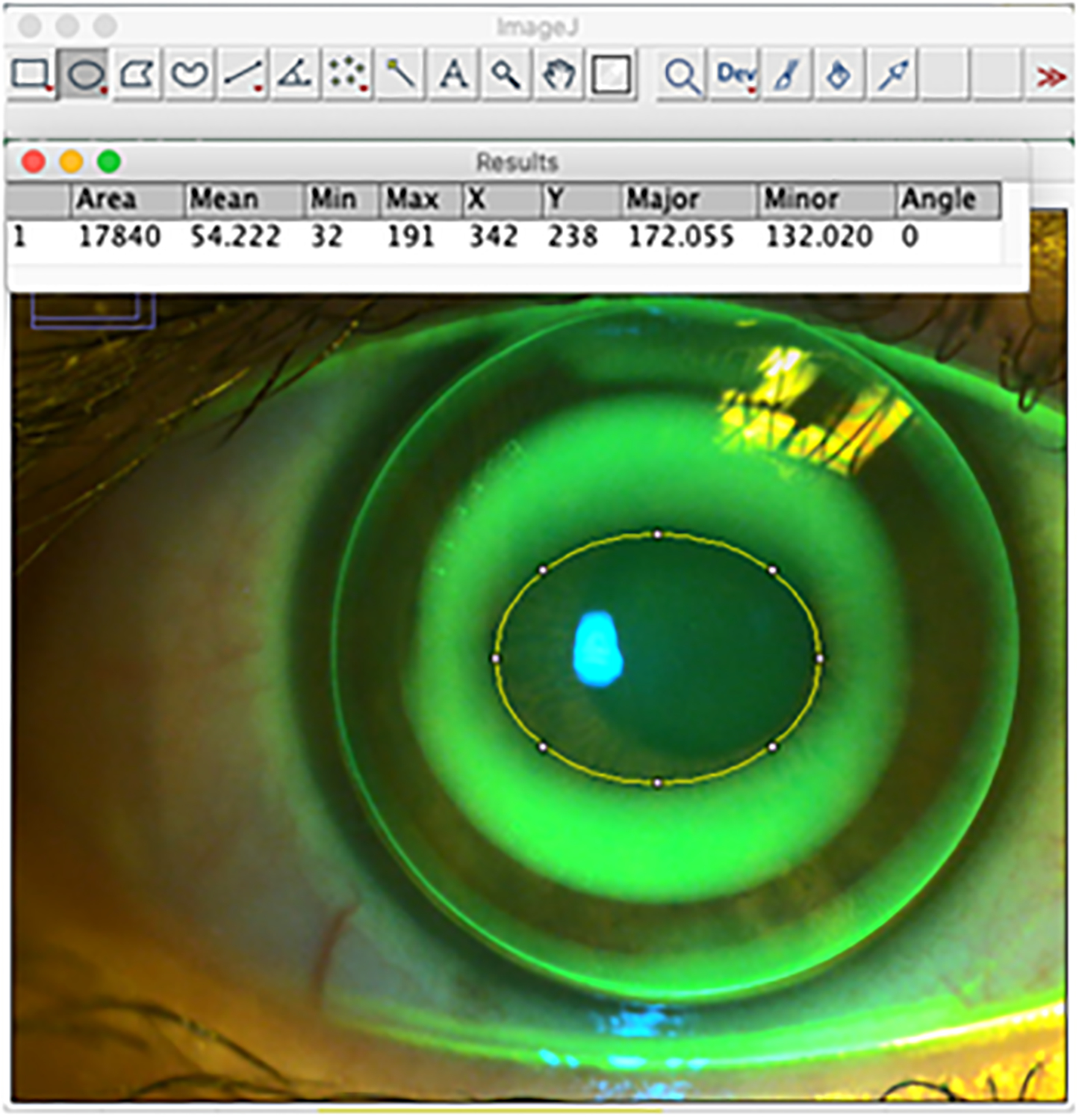
ImageJ software was used to fit a best fit ellipse to the screenshot of the slit-lamp video to calculate the size and area of the treatment zone of the lens (outlined in yellow).
Statistical Analysis
Data were entered in Microsoft Office Excel (Microsoft Corporation, Redmond, WA) and analyzed using commercial statistical software, SPSS (version 25.0; IBM Corporation, Armonk, NY). Pearson correlations and linear regressions were used to compare corneal shape factors. Bonferroni correction was used for multiple comparisons based on an initial p-value of <0.05 for statistical significance and dividing by the number of tests performed.
Results
Subjects
A total of 25 subjects, 13 male and 12 female, average age 25.2 ± 4.7 years were enrolled and completed the baseline visit. The average manifest refraction at baseline was sphere: −2.89 ± 1.30 DS and cylinder: −2.12 ± 0.52 DC. Average corneal astigmatism based on tomography at baseline was 2.20 ± 0.70 DC and average peripheral corneal elevation difference measured at an 8 mm chord was 50.88 ± 18.92 microns.
The corneal curvature was steeper temporally, but the elevation was higher nasally (Figure 3). The majority of subjects had astigmatism that extended to 8 mm.
Figure 3.
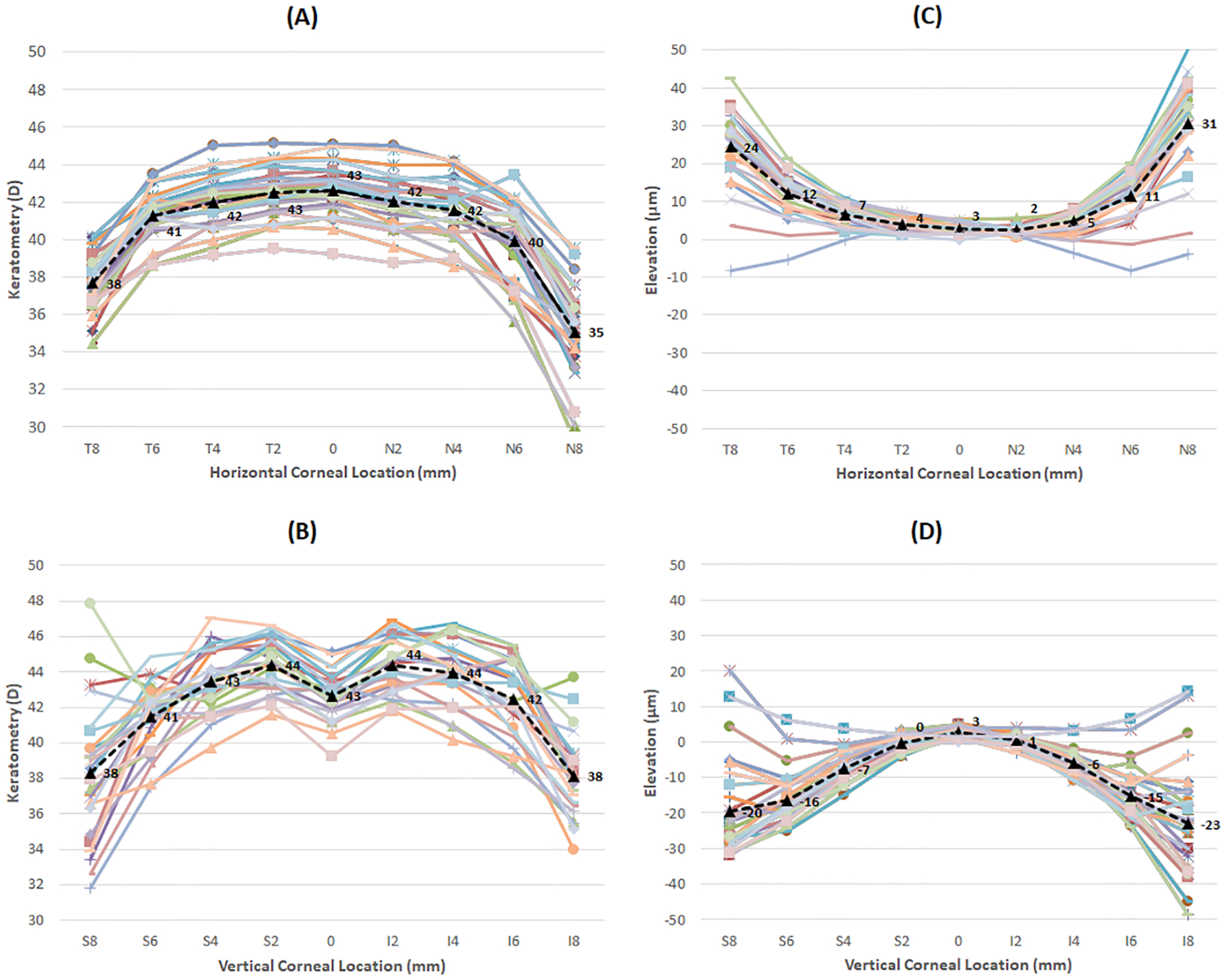
Keratometry (A, B) and elevation (C, D) values in both the horizontal (A, C) and vertical (B, D) meridians as measured by the Pentacam tomographer. Each individual line represents a subject. Black dashed line and values represent the average for each point. The x-axis shows the corneal location by the notation S (superior), I (inferior), N (nasal), or T (temporal). It also indicates the chord length in mm (2, 4, 6, 8).
Astigmatism and Elevation
There was a strong correlation between central corneal astigmatism and corneal elevation at the 4, 6, and 8 mm chords (R2 = 0.959, R2 = 0.923, R2 = 0.860, respectively; all p < 0.001). Each diopter of astigmatism equated to approximately 25 microns of elevation at an 8 mm chord, 14 microns at a 6 mm chord, and 6 microns at a 4 mm chord (Figure 4). The graph shows that the correlation between the two variables is much stronger at the shorter chord length and decreases towards the periphery.
Figure 4.
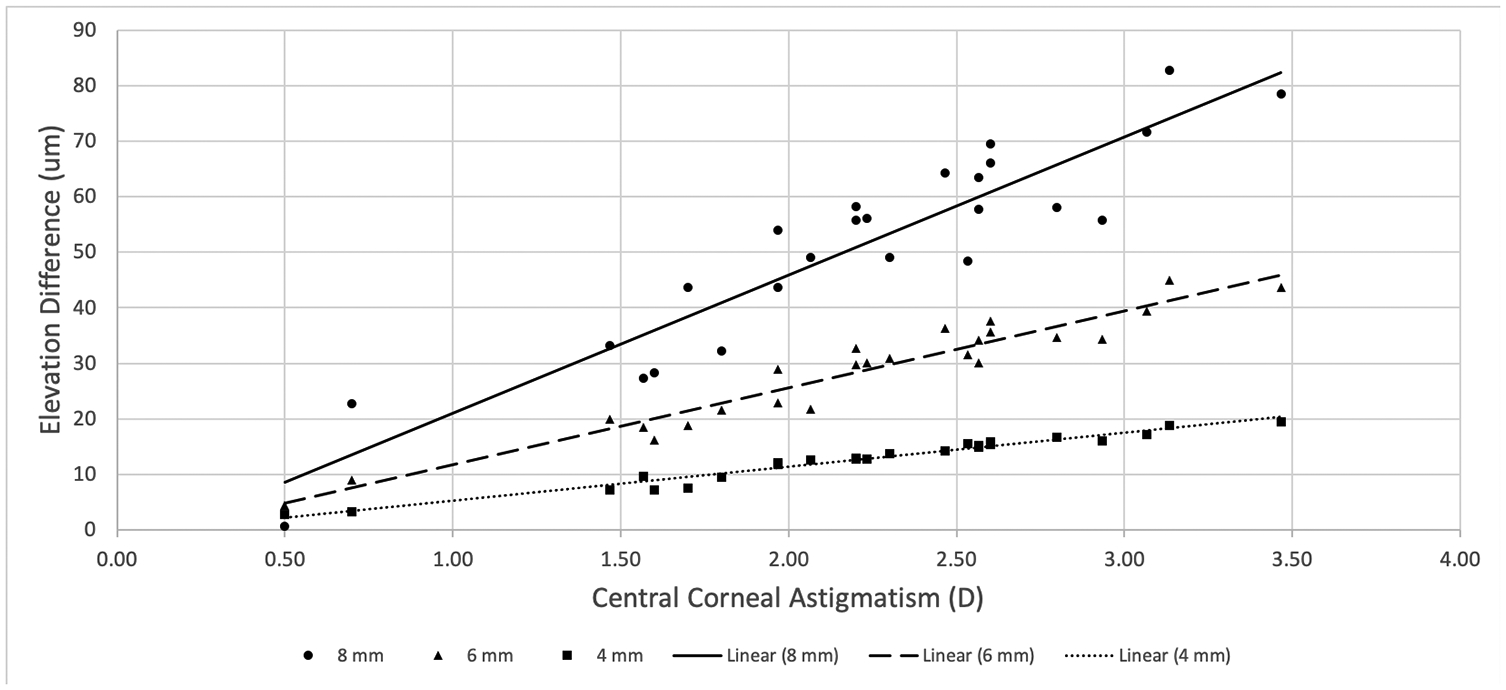
The relationship between central and corneal astigmatism and corneal elevation difference at the 4, 6, and 8 mm chords.
Fit Assessment
A subset of 20 subjects completed the follow-up visit after wearing the lenses an average of 10.2 ± 1.5 nights for 7.5 ± 0.6 hours per night. Five subjects were excluded from analysis because they either chose not to complete the study (three subjects) or did not have an acceptable lens fit to continue (two subjects). Based on the initial slit-lamp videos, one fit was graded as acceptably tight (>0 to 0.25 mm), one as acceptably loose (>0.5 to1.0 mm), and the other 18 as optimal movement (>0.25 to 0.50 mm) (90%). Seven of the 20 fits (35%) were centered with open eye lens wear. Of the 13 decentered lenses, eight were superior (40%), two nasal (10%), and three inferior (15%).
From the difference tomography maps, the average decentration of the treatment zone from the pupil center was 0.29 ± 0.23 mm temporal and 0.13 ± 0.26 mm inferior. In the horizontal meridian, 17 of the 20 tomography-based treatment zones (85%) were decentered temporally and in the vertical meridian, 15 of the 20 (75%) decentered inferiorly. Overall, 13 treatment zones (65%) were decentered to the infero-temporal quadrant (Figure 5).
Figure 5.
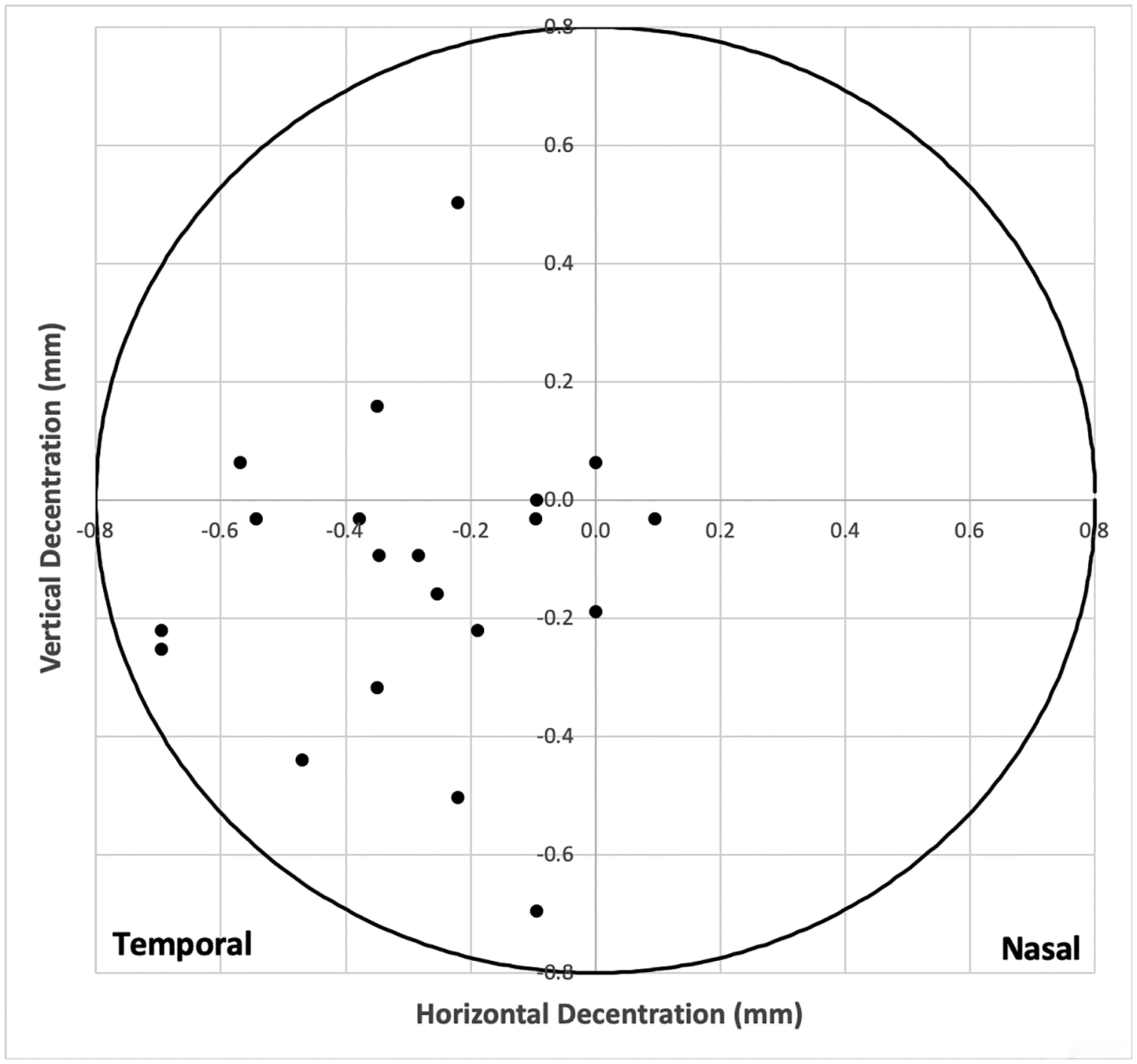
Treatment zone decentration from tomography difference maps. The center (0,0) represents the pupil center as designated by the Pentacam software. The black dots represent the treatment zone centers.
The average treatment zone as measured from the slit-lamp videos was 4.30 mm horizontally × 3.65 mm vertically, with a treatment zone area of 12.73 ± 4.62 mm2. In comparison, the average treatment zone as measured from a difference tomography map was 3.25 mm horizontally × 2.75 mm vertically, with a treatment zone area of 7.16 ± 2.56 mm2.
Elevation at an 8 mm chord was significantly negatively correlated with the treatment area as measured by tomography (R2 = 0.645, p < 0.001), but not with treatment area as measured by slit-lamp videos (R2 = 0.172, p = 0.069). Similarly, central corneal astigmatism was significantly negatively correlated with treatment area measured by tomography (R2 = 0.598, p < 0.001), but not with treatment area measured by slit-lamp videos (R2 = 0.067, p < 0.271). Therefore, as elevation and corneal astigmatism increased, the treatment area from tomography decreased.
Discussion
At baseline, the amount of corneal and refractive astigmatism was similar within subjects, indicating that most of the total astigmatism originated from the cornea. This agrees with Cheung et. al. who found a significant correlation between initial refractive astigmatism and initial corneal toricity.4 Additionally, baseline corneal toricity correlated well with baseline elevation difference. The data showed that each diopter of corneal toricity was equivalent to 25 microns of elevation difference for an 8 mm chord. Batres and colleagues calculated that each diopter of corneal toricity was equal to about 24 microns of elevation difference at an 8 mm chord in one randomly selected eye of 305 patients with up to 6 D of corneal toricity using the Oculus Pentacam tomographer.8
There was a strong correlation between the elevation difference and the central corneal astigmatism at the 4, 6, and 8 mm chords. The results were in agreement with a previous study that also showed a strong positive correlation between corneal toricity and corneal elevation difference, with the 4 mm chord showing the strongest correlation.8 With a strong relationship between these two variables, either value may be used to determine how much toricity to place in the reverse curve of the toric orthokeratology lens. Central corneal astigmatism may be a more expedient measure for clinical use because it does not require calculation as peripheral corneal elevation does.
When the Paragon Dual Axis lenses were placed on the eye, the lenses tended to decenter superiorly, likely due to upper lid attachment. However, the treatment zone decentration measured from the tangential difference topography maps tended to be inferior and temporal. Previous studies also show infero-temporal decentration of the lens with closed eye wear,21,23,25–27 perhaps due to the eyelid force and the asymmetric nature of the cornea, with the lowest and steepest portion temporal.10,21
The treatment zone measured from videos of on eye wear was larger than the actual treatment zone measured from tomography. The treatment zone was elliptical in shape due to the nature of the corneal astigmatism.27 The appearance of the treatment zone and lens decentration in the open eye condition was not indicative of the actual treatment zone size and decentration that was measured by tomography. There were limitations to the video method that may explain the lack of significant correlation between the treatment zone area and either elevation or corneal astigmatism. The masked examiner was asked to outline the treatment zone from a still photo captured from the slit-lamp video. The amount of sodium fluorescein instilled was not always uniform and the time after instillation before the photo was captured was not measured. The appearance of sodium fluorescein is transient and could have affected the visible appearance of the treatment zone area; however, as this is the same method usually performed clinically, it remains a useful assessment of clinical outcomes. Additionally, the slit-lamp lens fit videos were recorded at the initiation of lens wear, so the difference between the lens base curve and the anterior cornea is the greatest, which may have given the appearance of a larger treatment zone than if the treatment zone were re-measured at day 10.
The treatment zone measured from tomography was highly correlated with the elevation difference at 8 mm and the central corneal astigmatism. Both showed a negative correlation, meaning that the more astigmatism or more elevation the subject started with, the less treatment zone area size they achieved after lens wear. Two previous studies have shown that there is greater treatment zone decentration with greater magnitude of the baseline corneal toricity.25,26 Additionally, one study showed that when the decentration was limited (<1.5 mm), the spherical power of myopia correction was not affected but significant higher order aberrations were induced.27 The induced higher order aberrations and astigmatism from lens decentration can manifest as decreased visual acuity, contrast sensitivity, glare and halos.23,25,26,28 Decreased visual performance may also result from the mid-peripheral steepening of the orthokeratology lens falling within the pupillary zone.28,29
While the decentration of the treatment zone was inferior and temporal from the pupil center, the amount of decentration was minimal at less than 0.5 mm. Even with successful spherical lens fitting, mild to moderate lens decentration can still occur.23,25,26 Orthokeratology lens wear is often compared to refractive surgery since orthokeratology is a temporary flattening of the central cornea to correct for refractive error. A decentration scale used for refractive surgery suggests less than 0.5 mm is only mild decentration and would be an ideal outcome.30
Conclusion
For tomography images with the Pentacam, central corneal astigmatism and peripheral corneal elevation were highly correlated. Treatment zone area decreased as the amount of corneal astigmatism and elevation difference increased. Open eye lens assessment was not indicative of tomographic decentration and treatment area. Central corneal astigmatism was highly correlated to peripheral elevation and may be a more expedient measure for clinical use. Further studies are needed to understand how using corneal shape factors could improve lens fitting to maximize treatment zone and minimize lens decentration.
Support:
Orthokeratology lenses were supplied by Paragon Vision Sciences. The University of Houston Student Vision Research Support Grant and NEI P30 EY007551-31 provided support for this project.
Dr. Tomiyama is a consultant for Paragon Vision Sciences and previously received travel funding from Euclid Systems. Dr. Logan is a consultant for Bausch Health. Dr. Richdale is a consultant for Paragon Vision Sciences, Alcon, and Novartis. All authors have received research funding from Euclid Systems and Novartis. This work has been presented as an abstract at the American Academy of Optometry Meeting, “Corneal Elevation, Power, and Astigmatism to Assess Toric Orthokeratology Lenses in Moderate to High Astigmats,” Orlando, FL, October 25, 2019.
References
- 1.Nichols JJ, Marsich MM, Nguyen M, Barr JT, Bullimore MA. Overnight orthokeratology. Optom Vis Sci. 2000;77(5):252–259. [DOI] [PubMed] [Google Scholar]
- 2.Walline JJ, Rah MJ, Jones LA. The Children’s Overnight Orthokeratology Investigation (COOKI) pilot study. Optom Vis Sci. 2004;81(6):407–413. [DOI] [PubMed] [Google Scholar]
- 3.Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30(1):71–80. [DOI] [PubMed] [Google Scholar]
- 4.Cheung SW, Cho P, Chan B. Astigmatic changes in orthokeratology. Optom Vis Sci. 2009;86(12):1352–1358. [DOI] [PubMed] [Google Scholar]
- 5.Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci. 2012;89(6):849–855. [DOI] [PubMed] [Google Scholar]
- 6.Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study). Investig Ophthalmol Vis Sci. 2013;54(10):6510–6517. [DOI] [PubMed] [Google Scholar]
- 7.Tahhan N, Du Toit R, Papas E, Chung H, La Hood D, Holden AB. Comparison of reverse-geometry lens designs for overnight orthokeratology. Optom Vis Sci. 2003;80(12):796–804. [DOI] [PubMed] [Google Scholar]
- 8.Batres L, Piñero D, Carracedo G. Correlation Between Anterior Corneal Elevation Differences in Main Meridians and Corneal Astigmatism. Eye Contact Lens Sci Clin Pract. 2019;00(00):1. [DOI] [PubMed] [Google Scholar]
- 9.Zhang L, Zhang Y, Liu Y, Wang K, Zhao M. A novel fitting algorithm for alignment curve radius estimation using corneal elevation data in orthokeratology lens trial. Contact Lens Anterior Eye. 2017;40(6):401–407. [DOI] [PubMed] [Google Scholar]
- 10.Chen Z, Xue F, Zhou J, Qu X, Zhou X. Prediction of Orthokeratology Lens Decentration with Corneal Elevation. Optom Vis Sci. 2017;94(9):903–907. [DOI] [PubMed] [Google Scholar]
- 11.Woo GC, Chow E, Cheng D, Woo S. A study of the central and peripheral refractive power of the cornea with orthokeratology treatment. Int Contact Lens Clin. 1994. [Google Scholar]
- 12.Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121(8):1141–1147. [DOI] [PubMed] [Google Scholar]
- 13.Fan DSP, Rao SK, Cheung EYY, Islam M, Chew S, Lam DSC. Astigmatism in Chinese preschool children: Prevalence, change, and effect on refractive development. Br J Ophthalmol. 2004;88(7):938–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yoon K-C, Mun G-H, Kim S-D, et al. Prevalence of Eye Diseases in South Korea: Data from the Korea National Health and Nutrition Examination Survey 2008–2009. Korean J Ophthalmol. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan B, Cho P, Cheung SW. Orthokeratology practice in children in a university clinic in Hong Kong. Clin Exp Optom. 2008;91(5):453–460. [DOI] [PubMed] [Google Scholar]
- 16.Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom. 2002;85(5):284–293. [DOI] [PubMed] [Google Scholar]
- 17.Luo M, Ma S, Liang N. Clinical Efficacy of Toric Orthokeratology in Myopic Adolescent with Moderate to High Astigmatism. Eye Sci. 2014;29(4):209–213. [PubMed] [Google Scholar]
- 18.Lyu B, Hwang KY, Kim SY, Kim SY, Na KS. Effectiveness of Toric Orthokeratology in the Treatment of Patients with Combined Myopia and Astigmatism. Korean J Ophthalmol. 2016;30(6):434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen D, Lam AKC. Reliability and repeatability of the Pentacam on corneal curvatures. Clin Exp Optom. 2009;92(2):110–118. [DOI] [PubMed] [Google Scholar]
- 20.Perspectives on Fitting Paragon CRT ® Dual Axis TM Collected Fitting Suggestions from Experienced Paragon CRT ®. https://www.artoptical.com/storage/docs/CRT_Dual_Axis.pdf.
- 21.He L, Hu Y, Cui D, Yang X, Li Z, Long W. Predictive Role of Paracentral Corneal Toricity Using Elevation Data for Treatment Zone Decentration During Orthokeratology. Curr Eye Res. 2018;43(9):1083–1089. [DOI] [PubMed] [Google Scholar]
- 22.Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006;89(3):124–143. [DOI] [PubMed] [Google Scholar]
- 23.Hiraoka T, Mihashi T, Okamoto C, Okamoto F, Hirohara Y, Oshika T. Influence of induced decentered orthokeratology lens on ocular higher-order wavefront aberrations and contrast sensitivity function. J Cataract Refract Surg. 2009;35(11):1918–1926. [DOI] [PubMed] [Google Scholar]
- 24.Kang P, Gifford P, Swarbrick H. Can manipulation of orthokeratology lens. Optom Vis Sci. 2013;90(11):1237–1248. [DOI] [PubMed] [Google Scholar]
- 25.Maseedupally VK, Gifford P, Lum E, et al. Treatment zone decentration during orthokeratology on eyes with corneal toricity. Optom Vis Sci. 2016;93(9):1101–1111. [DOI] [PubMed] [Google Scholar]
- 26.Yang X, Zhong X, Gong X, Zeng J. Topographical evaluation of the decentration of orthokeratology lenses. Yan ke xue bao = Eye Sci. 2005;21(3):132–135, 195. [PubMed] [Google Scholar]
- 27.Zhu R, Jiang J, Huang W, Chen J, Li Y. Influence of overnight orthokeratology lens fitting decentration on corneal topography reshaping. Eye Vis. 2018;5(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiraoka T, Okamoto C, Ishii Y, Kakita T, Oshika T. Contrast sensitivity function and ocular higher-order aberrations following overnight orthokeratology. Investig Ophthalmol Vis Sci. 2007;48(2):550–556. [DOI] [PubMed] [Google Scholar]
- 29.Hiraoka T, Furuya A, Matsumoto Y, et al. Quantitative evaluation of regular and irregular corneal astigmatism in patients having overnight orthokeratology. J Cataract Refract Surg. 2004;30(7):1425–1429. [DOI] [PubMed] [Google Scholar]
- 30.Tsai YY, Lin JM. Ablation centration after active eye-tracker-assisted photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2000;26(1):28–34. [DOI] [PubMed] [Google Scholar]


