Abstract
Background
Hepatitis C virus (HCV) direct-acting antivirals are highly effective. Less is known about changes in markers of immune activation in persons with human immunodeficiency virus (HIV) in whom a sustained virologic response (SVR) is achieved.
Methods
We conducted a nonrandomized clinical trial of 12 or 24 weeks of paritaprevir-ritonavir-ombitasvir plus dasabuvir (PrOD) with or without ribavirin in persons with HCV-1/HIV coinfection suppressed with antiretroviral therapy. Plasma HCV, soluble CD14 (sCD14), interferon-inducible protein 10, soluble CD163 (sCD163), interleukin 6 (IL-6), interleukin 18, monocyte chemoattractant protein (MCP-1), autotaxin (ATX), and Mac2-binding protein (Mac2BP) were measured over 48 weeks.
Results
Participants were treated with PrOD for 12 (n = 9) or 24 (n = 36) weeks; the SVR rate at 12 weeks was 93%. At baseline, cirrhosis was associated with higher ATX and MCP-1, female sex with higher ATX and IL-6, older age with higher Mac2BP, higher body mass index with higher ATX, and HIV-1 protease inhibitor use with higher sCD14 levels. In those with SVR, interferon-inducible protein 10, ATX, and Mac2BP levels declined by week 2, interleukin 18 levels declined by the end of treatment, sCD14 levels did not change, and sCD163, MCP-1, and IL-6 levels changed at a single time point.
Conclusions
During HIV/HCV coinfection, plasma immune activation marker heterogeneity is in part attributable to age, sex, cirrhosis, body mass index, and/or type of antiretroviral therapy. HCV treatment with paritaprevir-ritonavir-ombitasvir plus dasabuvir is highly effective and is associated with variable rate and magnitude of decline in markers of immune activation.
Clinical Trials Registration
NCT02194998.
Keywords: human, immunity, hepatitis C, inflammation, DAA therapy
During human immunodeficiency virus/hepatitis C virus (HCV) coinfection heterogeneity in markers of immune activation is likely in part attributable to age, sex, cirrhosis, body mass index, and/or type of antiretroviral therapy. HCV treatment with direct-acting antiviral PrOD is highly effective and associated with variable decline in immune activation markers.
Coinfection with hepatitis C virus (HCV) is common among persons with human immunodeficiency virus (HIV) infection, and before the advent of HCV direct acting antivirals (DAAs) it was a major cause of liver-related disease and death, including cirrhosis, liver failure, and hepatocellular carcinoma [1–4]. Currently, HCV treatment leads to sustained virologic response (SVR) in most patients and has been linked to decreased mortality and cancer rates [5–7]. HCV infection is also associated with other nonhepatic conditions, including cardiovascular disease, Parkinson disease, and type 2 diabetes mellitus [8, 9]. Although the causal relationship between HCV infection and these extrahepatic conditions is not fully established, it may be mediated, in part, by HCV induced systemic inflammation. Chronic systemic inflammation is associated with immune dysfunction, disease, and death [10–14]. Although a number of studies have evaluated the effect of DAAs on systemic inflammation in persons with HCV monoinfection [15–20], few have been conducted in the setting of HCV-HIV coinfection [21]. Therefore, the impact of successful HCV treatment on systemic inflammation in persons with HIV-HCV coinfection is not well understood.
In AIDS Clinical Trials Group study A5329, we evaluated the safety, tolerability, and efficacy of HCV treatment with paritaprevir-ritonavir-ombitasvir plus dasabuvir (PrOD) with or without ribavirin (RBV) in persons with antiretroviral therapy (ART)–suppressed HIV infection and chronic HCV genotype 1 coinfection. We also examined changes in plasma inflammatory markers over the course of treatment.
METHODS
Study Design and Participants
Study A5329 (NCT02194998) was a nonrandomized, open-label, phase 2 trial of interferon-free HCV therapy for 24 or 12 weeks in sequentially enrolled cohorts of participants with HIV-1 coinfection taking protocol-defined ART. Version 1 was opened in May 2014. Trial participants were HCV treatment naive or experienced, with genotype 1a or 1b infection, and were taking ART based on integrase strand-transfer inhibitors (INSTIs; raltegravir or dolutegravir, allowed with version 2 in 2016) or an HIV-1 protease inhibitor (PI) (darunavir or atazanavir [version 2 only]). The inclusion criteria were age 18–70 years, CD4 T-cell count >200/µL, and HIV-1 RNA level <50 copies/mL for >6 months before study entry; the exclusion criteria were history of HIV-1 virologic failure (version 1 only), active HBV infection, decompensated liver disease, body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) ≥38 or <18, and pregnancy (including a pregnant sexual partner), and breastfeeding. Persons with compensated cirrhosis were eligible. Institutional review board committees at each study site approved the study, and written informed consent was obtained from each participant.
The study provided HCV treatment with PrOD. Paritaprevir-ritonavir-ombitasvir was administered as 2 tablets once daily with food, and dasabuvir was taken twice daily with food. Under version 1, all participants received RBV. Under version 2, RBV use was limited to persons with HCV genotype 1a. RBV was dosed twice daily with food according to body weight (1000 mg to participants with body weight ≤75 kg and 1200 mg to all others).
Procedures
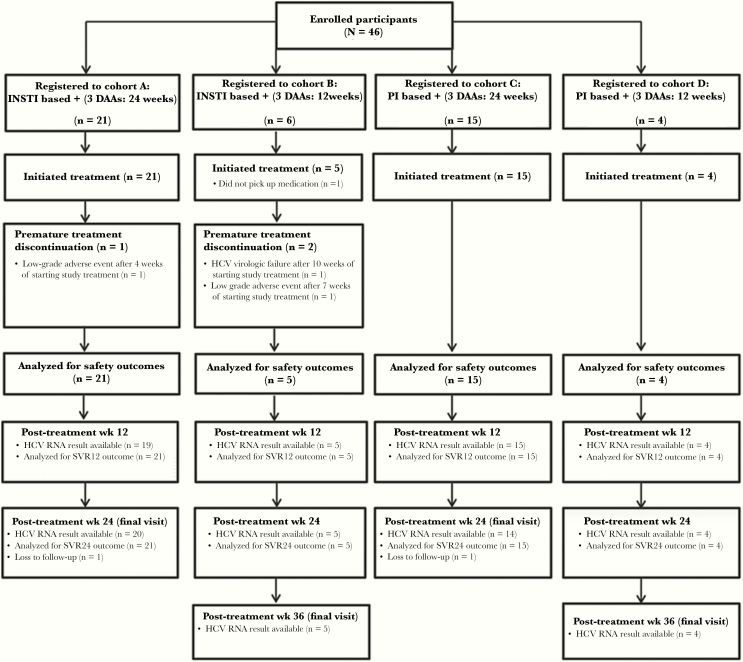
Within 45 days of the screening visit, enrolled participants started the study regimen in 1 of 4 cohorts (Figure 1) defined by antiretroviral regimen (INSTI or PI) and duration of PrOD treatment (12 or 24 weeks), as follows: cohort A, INSTI/24 weeks; cohort B, INSTI/12 weeks; cohort C, HIV-1 PI/24 weeks, and cohort D, HIV-1 PI/12 weeks. Participants entered the cohorts sequentially, starting with the 24-week cohorts (A and C), followed by the 12-week cohorts (B and C); participants were not randomized. Owing to the rapid evolution of the standard of care for HCV and HIV coinfection, study enrollment closed before full accrual (December 2017).
Figure 1.
Study design and cohort retention, showing study group distribution and cohort retention for the enrolled study participants. Abbreviations: DAAs, direct-acting antivirals; HCV, hepatitis C virus; INSTI, integrase strand-transfer inhibitor; PI, protease inhibitor; SVR12, sustained virologic response at 12 weeks; and SVR24, sustained virologic response at 24 weeks.
Postentry evaluations during PrOD treatment were performed at study weeks 2, 4, 6, 8, 10, and 12 for the 12-week cohorts, with the addition of weeks 16, 20, and 24 for the 24-week cohorts. After completion of PrOD, follow-up evaluations were performed 4, 12, and 24 weeks after treatment completion, with the addition of 36 weeks for the 12-week cohorts. HCV RNA was measured at each visit (>95% of measurements with COBAS TaqMan, Roche; remainder with Roche COBAS 6800/8800 or COBAS HCV nucleic acid test; Quest Diagnostics). The lower limit of quantitation (LLOQ) for both assays was 15 IU/mL. Plasma was stored at each study visit for analysis of soluble markers of immune activation and for HIV resistance testing in persons with virologic
failure. IL28B/IFN lambda-3 rs12979860 single nucleotide-polymorphism (SNP; CC, CT, or TT) genotyping was performed using the post–quantitative polymerase chain reaction high-resolution melt analysis method, adapted from Kovanda and Poljak [22].
Adverse events were graded by site investigators according to the Division of AIDS, National Institute of Allergy and Infectious Diseases guidelines. All adverse events grade ≥3 or any grade that led to treatment discontinuation were reported. Virologic failure for HIV-1 infection was defined as an increase in HIV-1 RNA to ≥200 copies/mL at any time after study entry. HCV virologic failure was defined: 1) An increase >1 log10 IU/mL from nadir in HCV RNA on 2 consecutive time points; or 2) The failure to achieve HCV RNA <LLOQ by treatment week 6 or 3) An HCV RNA ≥LLOQ on 2 consecutive time points after HCV RNA <LLOQ.
Markers of Immune Activation
Plasma was assessed at baseline, treatment weeks 2, 4, 8, 12, 16, 20, and 24 (as applicable based on treatment duration), and posttreatment weeks 4, 12, and 24 for the following inflammatory markers: soluble CD14 (sCD14; detection limit, 250.0 pg/mL; R&D Systems), interferon-inducible protein 10 (IP-10; 7.5 pg/mL; R&D Systems), autotaxin (ATX; 0.8 ng/mL; R&D Systems), soluble CD163 (sCD163; 1.6 ng/mL; R&D Systems), interleukin 6 (IL-6; 3.1 pg/mL; R&D Systems), interleukin 18 (IL-18; 25.6 pg/mL; Invitrogen, Thermo Fisher Scientific), Mac2-binding protein (Mac2BP 12.5 ng/mL; Invitrogen, Thermo Fisher Scientific), and monocyte chemoattractant protein 1 (MCP-1; 31.2 pg/mL; R&D Systems) by enzyme-linked immunosorbent assay.
Objectives
The primary objectives were to evaluate the safety and tolerability of PrOD with or without RBV and to estimate its efficacy in participants coinfected with HCV genotype 1 and HIV-1. Efficacy was assessed by means of SVR at 12 weeks after discontinuation of PrOD with or without RBV (SVR12, defined as HCV RNA level below the LLOQ). Among key secondary objectives was the assessment of the relationship of markers of immune activation, including IP-10 and sCD14, measured before, during, and after administration of PrOD with or without RBV. Exploratory objectives included analysis of a broader panel of soluble markers of systemic inflammation (sCD163, IL-6, ATX, Mac2BP, IL-18, and MCP-1).
Statistical Analyses
Participants not starting PrOD were excluded. SVR12 was defined as HCV RNA less than the LLOQ ≥10 weeks after completion of HCV treatment. Early responses before SVR12 evaluation meeting the protocol definition for HCV virologic failure were defined as nonresponses. Missing data were considered nonresponses only in cases of loss to follow-up; otherwise, the next available HCV RNA level was used to define the SVR outcome. SVR12 was estimated among all participants starting PrOD, and associated exact (Clopper-Pearson method), 2-sided 90% confidence interval (CIs) were calculated.
Any of the following events was considered a primary safety outcome: premature HCV study treatment discontinuation due to anything other than virologic failure, grade ≥3 signs or symptoms, grade ≥3 laboratory abnormalities, and diagnoses leading to study treatment discontinuation. For the secondary objectives related to immune activation, the participants who completed PrOD and experienced SVR12 were analyzed using log10-transformed plasma biomarker levels. Rank-based (Spearman) correlations explored associations between baseline covariates (age, CD4 T-cell count, BMI, and fibrosis 4 index) and biomarker concentrations. Geometric means of concentrations over time and fold changes of concentrations from baseline were summarized, along with corresponding 95% confidence intervals over the analysis sample, as well as within subgroups defined by baseline cirrhosis status, sex, or antiretroviral regimen. All P values and CIs presented, unless as noted above, were 2 sided, nominal, and unadjusted for interim analysis and multiple comparisons. Analyses were performed using SAS software, version 9.4 (SAS Institute).
RESULTS
Study Accrual
Between September 2015 and December 2017, a total of 46 participants were enrolled from 16 sites in the United States; 45 started DAAs and were included in analyses. Accrual was stopped with 36 of 50 planned participants enrolled in the 24-week cohorts (INSTI, n = 21; HIV-1 PI, n = 15). The 12-week cohorts opened to accrual after 24-week cohorts were closed; accrual was stopped with 9 of the planned 50 participants enrolled in 12-week cohorts (INSTI, n = 5; HIV-1 PI, n = 4) (Figure 1) short of accrual goals owing to the availability of the study regimen and other DAA regimens by prescription.
Participant Characteristics
HIV disease was well controlled, with HIV-1 RNA levels <40 copies/mL in all but 1 participant, and the median CD4 T-cell count was 665/µ L (Table 1). ART included INSTI-based ART (raltegravir [n = 21] or dolutegravir [n = 5]) and PI-based ART (ritonavir-boosted darunavir [n = 15] or ritonavir-boosted atazanavir [n = 4]). Comorbid diagnoses included psychiatric disorders (38%), hypertension (38%), prior intravenous drug use (69%), and diabetes mellitus (16%). Participants taking PIs were significantly older and reported previous injection drug use more frequently than those taking INSTIs (median age, 57 vs 48 years, respectively [P < .001]; history of injection drug use, 89% vs 50% [P = .009]). Participants taking INSTIs were heavier than those taking PIs (obesity [BMI ≥30] in 50% vs 5%, respectively; P = .004). Participants taking PIs were infected with HCV longer than those taking INSTIs (median time since HCV diagnosis, 16.5 vs 4.5 years; P < .001).
Table 1.
Baseline Characteristics of Study Participants
| Characteristic | Participants, No. (%)a | P Value (INSTI vs PI; n = 41)b | ||||
|---|---|---|---|---|---|---|
| PrOD ± RBV for 24 wk | PrOD ± RBV for 12 wk | Total (N = 45) | ||||
| INSTI (n = 21) | HIV-1 PI (n = 15) | INSTI (n = 5) | HIV-1 PI (n = 4) | |||
| Age, years median (IQR), y | 48 (40, 49) | 58 (55, 61) | 50 (49, 54) | 55 (49, 59) | 53 (47, 58) | <.001 |
| Male sexc | 14 (67) | 12 (80) | 4 (80) | 2 (50) | 32 (71) | 1.0 |
| Race/ethnicity | ||||||
| White, non-Hispanic | 5 (24) | 3 (20) | 1 (20) | 2 (50) | 11 (24) | .37 |
| Black, non-Hispanic | 6 (29) | 8 (53) | 3 (60) | 1 (25) | 18 (40) | |
| Hispanic (regardless of race) | 10 (48) | 4 (27) | 1 (20) | 1 (25) | 16 (36) | |
| Weight, median (IQR), kg 2 | 85 (78, 93) | 71 (65, 88) | 86 (84, 99) | 58 (52, 75) | 81 (68, 91) | .007 |
| HCV genotype 1a | 16 (76) | 13 (87) | 5 (100) | 4 (100) | 38 (84) | .42 |
| HCV RNA, median (IQR), log10 IU/mL | 6.5 (6.0, 6.8) | 6.5 (5.8, 7.0) | 5.9 (5.1, 6.3) | 6.2 (5.9, 6.5) | 6.4 (5.8, 6.8) | .84 |
| IL28B rs12979860 | . | |||||
| CC | 3 (14) | 3 (20) | 1 (20) | 2 (50) | 9 (20) | 78 |
| CT | 11 (52) | 8 (53) | 3 (60) | 0 (0) | 22 (49) | |
| TT | 7 (33) | 4 (27) | 1 (20) | 2 (50) | 14 (31) | |
| Cirrhosisd | 6 (29) | 2 (13) | 0 (0) | 0 (0) | 8 (18) | .25 |
| FIB-4 score, median (IQR) | 1.3 (0.8, 2.1) | 1.7 (1.3, 2.3) | 1.3 (1.0, 1.9) | 1.0 (0.6, 1.3) | 1.4 (1.0, 2.2) | .37 |
| HCV treatment naive | 20 (95) | 12 (80) | 5 (100) | 3 (75) | 40 (89) | .16 |
| CD4 T-cell count, median (IQR), cells/µ L | 752 (467, 1064) | 646 (466, 849) | 674 (528, 726) | 525 (404, 683) | 665 (464, 894) | .64 |
| HIV RNA >40 copies/mL | 0 (0) | 1 (7) | 0 (0) | 0 (0) | 1 (2) | .46 |
| Interval between HCV diagnosis and study entry, median (IQR), y | 4.4 (2.8, 14.3) | 16.5 (14.4, 17.7) | 13.7 (11.2, 16.7) | 14.0 (8.8, 19.0) | 14.0 (4.1, 17.4) | <.001 |
Abbreviations: FIB-4, fibrosis 4 index; HCV, hepatitis C virus; HIV-1, human immunodeficiency virus type 1; INSTI, integrase strand-transfer inhibitor; IQR, interquartile range; PI, protease inhibitor; PrOD, paritaprevir-ritonavir-ombitasvir plus dasabuvir; RBV, ribavirin.
aData represent no. (%) of participants unless otherwise identified as median (IQR) values.
bComparisons between subsets of nonrandomized INSTI groups (24- and 12-week cohorts; n = 22) and PI groups (24- and 12-week cohorts; n = 19), who completed PrOD treatment with or without RBV and were responders with a sustained virologic response. P values are based on Fisher exact tests for categorical and Wilcoxon rank sum tests for continuous variables.
cGender identity was not collected for the 24-week cohorts; all 9 participants in the 12-week cohorts self-identified as cisgender.
dCirrhosis status was determined by means of biopsy (n = 1), transient elastography (n = 27), or a combination of peripheral blood markers (FibroSURE test and aspartate aminotransferase–platelet ratio index; n = 17).
Study Retention
Three participants discontinued PrOD prematurely owing to adverse events (RBV-related anemia [n = 2] or virologic failure [n = 1]).
Efficacy
The overall SVR12 rate was 93% (90% CI, 84%–98%; 42 of 45 participants starting DAA treatment) (Table 2). All 3 without SVR had genotype 1a infection. Among those assigned to 24 weeks of therapy, 1 participant who received INSTI-based ART had virologic nonresponse, with HCV RNA not detected during treatment but detected at posttreatment weeks 12 and 24; this individual was treated for only 4 weeks, was female without evidence of cirrhosis, and had IL28B/IFN lambda-3 rs12979860 SNP TT genotype (associated with nonresponse to interferon-based therapy). Among persons treated for 12 weeks, 2 who received INSTI-based ART had nonresponse; 1 did not suppress HCV RNA before treatment week 6 and the other had HCV RNA detected 12 weeks after treatment. Both participants were treatment naive and did not have cirrhosis (IL28B/IFN-lambda-3 rs12979860 SNP TT and CT). The latter was re-treated with sofosbuvir-velpatasvir-voxilaprevir during the posttreatment period and had HCV RNA levels below the LLOQ at the last study visit. No participant who achieved SVR12 had detectable HCV RNA at posttreatment week 24; however, 2 persons were lost to follow-up and had missing HCV RNA data. HIV-1 virologic failure was observed in 1 participant with premature discontinuation of HCV DAAs and ART. No HIV-1 genotypic mutations conferring resistance to antiretrovirals were detected at the time of HIV virologic failure.
Table 2.
Hepatitis C Virus SVR12 Response, Overall and by Key Subgroups
| SVR12, No/Total (%; 90% CI)a | |
|---|---|
| All participants | 42/45 (93; 84, 98) |
| By Cohort | |
| PrOD ± RBV for 24 wk/INSTI ARV regimen | 20/21 (95; 79, 100) |
| PrOD ± RBV for 24 wk/HIV-1 PI ARV regimen | 15/15 (100; 82, 100) |
| PrOD ± RBV for 12 wk/INSTI ARV regimen | 3/5 (60; 19, 92) |
| PrOD ± RBV for 12 wk/HIV-1 PI ARV regimen | 4/4 (100; 47, 100) |
| By HCV genotype | |
| Genotype 1A | 35/38 (92; 81, 98) |
| Genotype 1B | 7/7 (100; 65, 100) |
| By baseline cirrhosis status | |
| Non-cirrhotic | 34/37 (92; 80, 98) |
| Cirrhotic | 8/8 (100; 69, 100) |
| By natal sex | |
| Female | 12/13 (92; 68, 100) |
| Male | 30/32 (94; 82, 100) |
Abbreviations: CI, confidence interval; HIV-1 human immunodeficiency virus type 1; INSTI, integrase strand-transfer inhibitor; PI, protease inhibitor; PrOD, paritaprevir-ritonavir-ombitasvir plus dasabuvir; RBV, ribavirin; SVR12, sustained virologic response at 12 weeks after completion of therapy.
aExact 2-sided, 90% CIs (Clopper-Pearson method).
Safety
Sixteen (36%) participants had ≥1 primary safety outcome (Table 3). Signs or symptoms grade ≥3 included neuropathic foot pain, acute bronchitis, left-sided weakness, myocardial infarction, abdominal pain, and fatigue. RBV was used with PrOD by most participants (42 of 45), including all with genotype 1a infection. RBV dose reduction or discontinuation occurred in 10 of 42 participants (24%) who received it.
Table 3.
Primary Safety and Tolerability Outcomes
| Safety or Tolerability Outcome | Participants, No. (%) | ||||
|---|---|---|---|---|---|
| PrOD ± RBV for 24 wk | PrOD ± RBV for 12 wk | Total (N = 45) | |||
| INSTI (n = 21) | HIV-1 PI (n = 15) | INSTI (n = 5) | HIV-1 PI (n = 4) | ||
| ≥1 Qualifying event | 7 (33) | 6 (40) | 3 (60) | 0 (0) | 16 (36) |
| SAE by ICH criteria | 1 (5) | 2 (13) | 1 (20) | 0 (0) | 4 (9) |
| Grade ≥3 sign or symptom | 0 (0) | 3 (20) | 2 (40) | 0 (0) | 5 (11) |
| Grade ≥3 laboratory abnormality | 5 (24) | 3 (20) | 3 (60) | 0 (0) | 11 (24) |
| Premature discontinuation of HCV treatment | 1 (5) | 0 (0) | 1 (20) | 0 (0) | 2 (4) |
| Diagnosis leading to discontinuation HCV or HIV-1 treatment | 0 (0) | 0 (0) | 1 (20) | 0 (0) | 1 (2) |
Abbreviations: HCV, hepatitis C virus; HIV human immunodeficiency virus; ICH, International council for harmonization of technical requirements for pharmaceuticals for human use; INSTI, integrase strand-transfer inhibitor; PI, protease inhibitor; PrOD, paritaprevir-ritonavir-ombitasvir plus dasabuvir; RBV, ribavirin; SAE, serious adverse event.
Biomarkers of Immune Activation
To understand the timing and magnitude of normalization of inflammatory parameters associated with disease during HCV and HIV infection [10–14, 23–25] we evaluated plasma levels of IP-10, ATX, Mac2BP, IL-6, IL-18, sCD163, sCD14, and MCP1 before, during, and after DAA therapy. The entry distribution of each biomarker is summarized in Table 4. Levels of each marker, with the exception of IL-6, varied substantially. Before HCV therapy, HIV-PI use was associated with higher sCD14 levels (P = .01), diagnosis of cirrhosis was associated with higher ATX (P = .01) and MCP1 (P = .02) levels, and women had higher ATX (P < .001) and IL-6 (P = .02) levels than men. In addition, the following associations were observed between markers of immune activation and continuous clinical variables (Table 5): older age was correlated with higher Mac2BP levels (r = 0.34; P = .03), and higher BMI was correlated with higher ATX levels (r = 0.35; P = .05).
Table 4.
Baseline Levels of Plasma Markers Before Hepatitis C Virus Direct-Acting Antiviral Treatment in Participants Who Completed Treatment and Had a Sustained Virologic Responsea
| Marker | Geometric Mean (Antilog of SD)b | P Valuec (Cirrhotic vs Noncirrhotic) | Geometric Mean (Antilog of SD)b | P Valuec (Male vs Female Sex) | |||
|---|---|---|---|---|---|---|---|
| Total Group (N = 41) | Cirrhotic (n = 8) | Noncirrhotic (n = 33) | Female Sex (n = 11) | Male Sex (n = 30) | |||
| IP-10, pg/mL | 272 (2.5) | 225 (3.0) | 285 (2.5) | .59 | 237 (2.2) | 286 (2.7) | .53 |
| ATX, ng/mL | 366 (2.0) | 688 (2.0) | 313 (1.8) | .02d | 678 (1.8) | 290 (1.8) | <.001d |
| Mac2BP, ng/mL | 15659 (2.9) | 19640 (2.6) | 14796 (3.1) | .48 | 23045 (2.3) | 13766 (3.1) | .14 |
| IL-6, pg/mL | 1.91 (1.9) | 2.94 (2.1) | 1.73 (1.8) | .08 | 2.93 (2.0) | 1.64 (1.8) | .03d |
| IL-18, pg/mL | 234 (2.8) | 278 (2.9) | 223 (2.8) | .61 | 190 (2.2) | 256 (3.0) | .36 |
| MCP-1, pg/mL | 258 (1.8) | 423 (1.8) | 228 (1.6) | .02d | 231 (1.5) | 269 (1.9) | .37 |
| sCD163, ng/mL | 1312 (2.9) | 836 (3.5) | 1469 (2.7) | .27 | 787 (3.4) | 1593 (2.6) | .11 |
| sCD14, ng/mL | 2275 (2.1) | 1982 (1.8) | 2355 (2.2) | .50 | 2544 (1.8) | 2181 (2.3) | .51 |
Abbreviations: ATX, autotaxin; IL-6, interleukin 6; IL-18, interleukin 18; IP-10, interferon-inducible protein 10; Mac2BP, Mac2-binding protein; MCP-1, monocyte chemoattractant protein 1; sCD14, soluble CD14; sCD163, soluble CD163; SD, standard deviation.
aValues are shown for total group and subgroups by cirrhosis status and by sex at birth.
bAntilog of the SD of the log10-transformed biomarker values.
c P values based on t tests with unequal variance.
dSignificant at P ≤ .05.
Table 5.
Rank-Based Correlations (and P Values) Between Baseline Biomarker Levels and Selected Continuous Baseline Characteristics
| Inflammatory Marker | Correlation (r); P Value | |||
|---|---|---|---|---|
| Age | BMI | CD4 T-Cell Count | FIB-4 | |
| IP-10 | –0.03; .85 | 0.23; .16 | −0.20; .23 | 0.09; .59 |
| Mac2BP | 0.34; .03a | 0.10; .54 | 0.31; .06 | 0.25; .12 |
| ATX | −0.05; .74 | 0.32; .05a | 0.25; .12 | 0.27; .10 |
| IL-18 | −0.20; .24 | 0.16; .35 | 0.12; .50 | −0.02; .91 |
| IL-6 | −0.03; .85 | 0.19; .22 | −0.07; .66 | 0.01; .95 |
| sCD163 | −0.17; .30 | 0.00; .99 | −0.27; .10 | −0.20; .24 |
| MCP1 | −0.10; .54 | 0.17; .31 | −0.02; .88 | 0.12; .49 |
| sCD14 | 0.21; .20 | −0.30; .06 | 0.07; .69 | 0.08; .63 |
Abbreviations: ATX, autotaxin; BMI, body mass index; FIB-4, fibrosis 4 index; IL-6, interleukin 6; IL-18, interleukin 18; IP-10, interferon-inducible protein 10; Mac2BP, Mac2-binding protein; MCP-1, monocyte chemoattractant protein 1; sCD14, soluble CD14; sCD163, soluble CD163.
aNominal P ≤ .05.
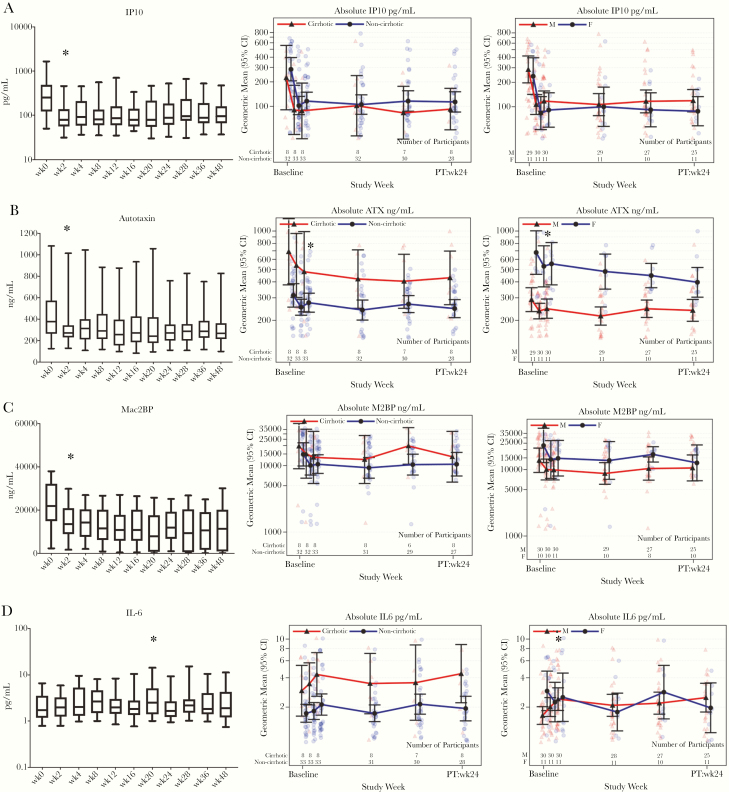
Figure 2 and Supplementary Figure 1 show the change in inflammatory markers from baseline during and after HCV therapy in all participants and in those with an SVR. IP-10 levels declined by treatment week 2 (mean fold change, 0.37; 95% CI, .31–.45); this decline was maintained at posttreatment week 24 (mean fold change, 0.38). Change in IP-10 levels did not differ by cirrhosis status or sex. Similarly, ATX and Mac2BP levels declined rapidly after initiation of HCV therapy in persons with SVR (mean fold change [95% CI], 0.81 [.71–.91] and 0.69 [.60–.80], respectively), and remained lower than baseline levels at posttreatment week 24 (mean fold change, 0.74 and 0.69, respectively). Changes in ATX or Mac2BP levels did not vary according to cirrhosis status, whereas women had a greater decline in ATX than men from baseline to 24 weeks after treatment completion (mean fold change, 0.59 vs 0.82, respectively; P = .04). Decline in IL-18 level was not observed until the end of treatment for all participants with SVR (mean fold change, 0.82; 95% CI, .67–.99), and this decline persisted through posttreatment week 24 (mean fold change, 0.68). Although there were no significant differences in change in IL-18 by cirrhosis status, women were observed to have a greater change from baseline to treatment week 2 (P = .04).
Figure 2.
Heterogeneity in markers of inflammation (by cirrhosis state and sex) at baseline and over the course of direct-acting antiviral (DAA) therapy. Left panels show inflammatory marker levels (median, interquartile range, and 5%/95% confidence intervals [CIs]) for all study participants as horizontal bar, box, and whiskers; x-axis labels represent time (weeks) from start of therapy, regardless of study arm or treatment duration. Middle panels show inflammatory marker levels for participants with sustained virologic response (SVR) by cirrhosis status (mean with 95% CI); x-axis labels indicate the times of sampling during and after therapy, with sample numbers indicated in insets. Right panels show inflammatory marker levels for participants with SVR by sex (mean with 95% CI); x-axis labels indicate the times during and after therapy, with sample numbers indicated in insets. Asterisks represent the first statistically significant differences, comparing baseline and time point during or after therapy (left panels) or comparing subgroups (middle and right panels). Panel A: IP-10; Panel B: Autotaxin; Panel C: Mac2BP; Panel D: IL-6. Abbreviations: ATX, autotaxin; IL-6, interleukin 6; IP-10, interferon-inducible protein 10; Mac2BP, Mac2-binding protein; PT, posttreatment.
Three markers (IL-6, sCD163, and MCP-1) changed from baseline at only a single time point (mean fold change [95% CI] for IL-6, sCD163, and MCP-1, respectively, 1.29 [1.02–1.63] at posttreatment week 12 [this seemed to differ by sex], 0.77 [.62–.96] at week 2, and 0.90 [.82–.98] at week 2). For sCD163 there were sex differences in marker change during study treatment, with increases in women at week 4 and at the end of treatment (mean fold changes, 1.85 and 1.88, respectively) and decreases in men (0.75 and 0.51, respectively), which were no longer observed in the posttreatment period. sCD14 levels did not change significantly in those with SVR, nor did they differ by cirrhosis status or sex subgroup.
DISCUSSION
Our study findings support prior observations of high-level safety, tolerability, and efficacy of HCV treatment with DAAs in persons with HIV coinfection, but they also underscore the adverse impact of RBV on the safety and tolerability of HCV DAAs. The potential for drug interactions between the drug regimens used to treat HIV and HCV remains an important consideration. Our findings confirm that an HCV regimen containing the HIV-1 PI ritonavir as a pharmacologic booster can be safely administered to persons with HIV infection taking ART [26]. Although currently recommended HCV DAA regimens in the United States do not rely on pharmacologic boosting with ritonavir, such regimens remain in use in other regions of the world [27].
Because the PrOD regimen includes low-dose RTV, the potential for HIV-1 viral failure during HCV treatment presented a unique issue. If participants exposed to 100 mg of RTV daily were to experience HIV-1 viral failure, there would be the potential for the selection of HIV-1 mutations, beginning with the V82A/F mutant followed by the accumulation of additional mutants at positions 54, 71, and 36 in the protease gene [28]. One participant had HIV-1 viral failure that was likely due to ART nonadherence, with no evidence for HIV-1 mutations in the protease or other regions of the genome. Although our study does not exclude HIV-1 resistance emergence with low-dose ritonavir, our data support the use of this and other ritonavir-boosted HCV regimens, such as the HCV PI, nalaprevir, in persons with suppressed HIV-1 infection [29].
We also examined the relationship between HCV decline and markers of immune activation. Our findings indicate that IP-10, a chemokine for CXCR3 that is expressed by monocytes and Kupffer cells [30], is elevated at baseline in most persons with HIV and active HCV infection, and is normalized rapidly (<2 weeks) after initiation of HCV DAA therapy to levels compatible with historical controls [31–33]. This finding is consistent with those of other studies in HCV monoinfection and HCV-HIV coinfection [31–35], and likely reflects cessation of virus-mediated innate interferon signaling.
We also found evidence of normalization or partial normalization of other inflammatory markers associated with fibrosis or fibrogenesis in persons with HIV/HCV coinfection, including ATX, Mac2BP, MCP-1, and IL-18. Notably, the decline in IL-18 levels was modest in magnitude, sex specific (women only early during therapy), and occurred more slowly than that in IP-10, ATX, and Mac2BP. This may in part be attributable to relatively normal IL-18 levels at baseline in the majority of participants [36, 37], though even in those with exceptionally high baseline IL-18 levels (>1000 pg/mL), the decline was modest and gradual (not shown). Unlike IP-10, levels of ATX were only partially normalized compared with historical uninfected controls [19, 20, 25]. ATX levels are elevated during chronic HCV infection, particularly in individuals with liver fibrosis, and they are known to be partially normalized early during the course of HCV DAA therapy in HCV monoinfection [18–20, 25], consistent with a component due to reversible liver inflammation or edema and an irreversible component potentially attributable to liver fibrosis.
Results stratified by cirrhosis state here are in agreement, and they further indicate that both cirrhotic and noncirrhotic participants have similar degrees of ATX decline. ATX plasma levels are, for unclear reasons, higher in women than in men [38], and our data indicate that women may have greater declines in ATX levels over the course of DAA therapy. Mac2BP levels are partially normalized during DAA therapy for HCV monoinfection [19, 20], and our current findings extend this to HIV-HCV coinfection [19, 20]. It has been proposed that Mac2BP levels reflect ongoing fibrogenesis. We did not observe consistent changes in other markers of chronic immune activation. At baseline, levels of IL-6, MCP1, sCD163, and sCD14 were elevated (modestly in some cases) compared with historical uninfected controls (HIV infected and HCV uninfected or, in some cases, HIV and HCV uninfected) [19, 20, 23, 39] and were not normalized over the course of the study.
In the case of sCD14, baseline levels differed by HIV treatment status, with higher levels observed in those receiving PI therapy. Notably, participants taking PIs had a longer duration of HCV infection, older age, and lower BMI, and BMI did nearly correlate with baseline sCD14 levels (Table 4; r = –0.3; P = .06), providing a potential link. IL-6 has been associated with chronic inflammation and progression of cardiovascular disease and frailty [40]. Here IL-6 levels were higher in women at baseline and only temporarily increased 12 weeks after treatment, consistent with a number of factors driving IL-6 levels (sex, HIV status, and host immune status after removal of HCV). Although it is possible that these and other markers of inflammation will be normalized over longer periods of time after HCV cure, our findings may reflect a state driven by controlled HIV infection, sex, and other potential stimuli that need to be considered over longer time windows.
With respect to safety, our study largely confirms the safety profile of the PrOD regimen observed in other studies. However, our results also demonstrate laboratory and clinical adverse events associated with the use of RBV that causes anemia due to drug-induced hemolysis. The majority of grade ≥3 adverse events were consistent with known adverse events associated with hemolytic anemia, including weakness, fatigue, shortness of breath, and elevated total bilirubin. Although RBV is infrequently used in combination with DAA regimens recommended by the American Association for the Study of Liver Diseases/Infectious Diseases Society of America guidelines panel, it could conceivably play a role in selected patients. In such circumstances, the potential antiviral benefits of RBV would have to be carefully weighed against its known side effect profile.
Our study is subject to several important limitations. The clinical trial was designed before the regulatory approval of the PrOD regimen and completion of studies of PrOD in persons with HIV. The standard of care for HCV (additional HCV DAA regimens) and HIV (shift from HIV-1 PIs to INSTI) changed rapidly during the enrollment phase of the study, which limited accrual. In addition, the PrOD regimen is no longer used in the United States; however, this and other ritonavir-boosted HCV PI-based regimens remain in use in some countries, and the effect of HCV response on immune activation is not expected to be HCV regimen specific. Inflammatory biomarker levels were not measured in uninfected controls as part of this study, so whereas change was observed for many markers, the degree of normalization is difficult to fully assess. Finally, this study was not powered to adjust for contributions of age, BMI, sex, race and cirrhosis versus HCV infection status on biomarker level, though declines over the course of therapy do establish a definitive reversible contribution of active HCV infection and indicate that these other clinical factors warrant additional attention in future studies.
In summary, HCV treatment with PrOD led to high SVR rates in persons with well-controlled HIV infection, with clinically manageable interactions with antiretroviral drugs. Control of HCV replication was associated with declines in plasma IP-10 levels and markers of liver fibrosis or fibrogenesis (ATX and Mac2BP), modest and more delayed declines in IL-18, but little or no changes in levels of other markers of chronic inflammation, including IL-6, sCD14, sCD163, and MCP-1. Heterogeneity in baseline levels of inflammatory markers, and in some cases degree of change in markers over the course of therapy, may be influenced by age, sex, cirrhosis, BMI, and HIV treatment. Further study is needed to understand the relationship of HCV eradication, immune activation, and chronic disease outcomes in HCV-HIV infection.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. We thank the study participants for their time and dedication to this effort.
Financial support. This study was supported by AbbVie, the AIDS Clinical Trials Group (ACTG) under Award Numbers UM1 AI106701, UM1 AI068634, Statistical and Data Management Center (SDMC) for ACTG, IK2CX001471 (C. S. I.), BX001894 and CX001791 (D. D. A.), K24DA034621 (M. S. S.).
Potential conflicts of interest. Dr Cohen is employed by AbbVie. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Cacoub P, Geffray L, Rosenthal E, et al. Mortality among human immunodeficiency virus-infected patients with cirrhosis or hepatocellular carcinoma due to hepatitis C virus in French departments of internal medicine/infectious diseases, in 1995 and 1997. Clin Infect Dis 2001; 32:1207–14. [DOI] [PubMed] [Google Scholar]
- 2. Greub G, Ledergerber B, Battegay M, et al. Clinical progression, survival, and immune recovery during antiretroviral therapy in patients with HIV-1 and hepatitis C virus coinfection: the Swiss HIV Cohort Study. Lancet 2000; 356:1800–5. [DOI] [PubMed] [Google Scholar]
- 3. Sulkowski MS, Moore RD, Mehta SH, Chaisson RE, Thomas DL. Hepatitis C and progression of HIV disease. JAMA 2002; 288:199–206. [DOI] [PubMed] [Google Scholar]
- 4. Zylberberg H, Pol S. Reciprocal interactions between human immunodeficiency virus and hepatitis C virus infections. Clin Infect Dis 1996; 23:1117–25. [DOI] [PubMed] [Google Scholar]
- 5. Backus LI, Belperio PS, Shahoumian TA, Mole LA. Direct-acting antiviral sustained virologic response: impact on mortality in patients without advanced liver disease. Hepatology 2018; 68:827–38. [DOI] [PubMed] [Google Scholar]
- 6. Grandhe S, Frenette CT. Occurrence and recurrence of hepatocellular carcinoma after successful direct-acting antiviral therapy for patients with chronic hepatitis C virus infection. Gastroenterol Hepatol (N Y) 2017; 13:421–5. [PMC free article] [PubMed] [Google Scholar]
- 7. Simmons B, Saleem J, Heath K, Cooke GS, Hill A. Long-term treatment outcomes of patients infected with hepatitis C virus: a systematic review and meta-analysis of the survival benefit of achieving a sustained virological response. Clin Infect Dis 2015; 61:730–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Drazilova S, Gazda J, Janicko M, Jarcuska P. Chronic hepatitis C association with diabetes mellitus and cardiovascular risk in the era of DAA therapy. Can J Gastroenterol Hepatol 2018; 2018:6150861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wijarnpreecha K, Chesdachai S, Jaruvongvanich V, Ungprasert P. Hepatitis C virus infection and risk of Parkinson’s disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 2018; 30:9–13. [DOI] [PubMed] [Google Scholar]
- 10. Furman D, Chang J, Lartigue L, et al. Expression of specific inflammasome gene modules stratifies older individuals into two extreme clinical and immunological states. Nat Med 2017; 23:174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hunt PW, Sinclair E, Rodriguez B, et al. Gut epithelial barrier dysfunction and innate immune activation predict mortality in treated HIV infection. J Infect Dis 2014; 210:1228–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tenorio AR, Zheng Y, Bosch RJ, et al. Soluble markers of inflammation and coagulation but not T-cell activation predict non-AIDS-defining morbid events during suppressive antiretroviral treatment. J Infect Dis 2014; 210:1248–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wikby A, Nilsson BO, Forsey R, et al. The immune risk phenotype is associated with IL-6 in the terminal decline stage: findings from the Swedish NONA immune longitudinal study of very late life functioning. Mech Ageing Dev 2006; 127:695–704. [DOI] [PubMed] [Google Scholar]
- 14. Zampino R, Marrone A, Restivo L, et al. Chronic HCV infection and inflammation: clinical impact on hepatic and extra-hepatic manifestations. World J Hepatol 2013; 5:528–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yamazaki T, Joshita S, Umemura T, et al. Association of serum autotaxin levels with liver fibrosis in patients with chronic hepatitis C. Sci Rep 2017; 7:46705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mascia C, Vita S, Zuccalà P, et al. Changes in inflammatory biomarkers in HCV-infected patients undergoing direct acting antiviral-containing regimens with or without interferon. PLoS One 2017; 12:e0179400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Malone DF, Falconer K, Weiland O, Sandberg JK. The dynamic relationship between innate immune biomarkers and interferon-based treatment effects and outcome in hepatitis C virus infection is altered by telaprevir. PLoS One 2014; 9:e105665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yamazaki T, Joshita S, Umemura T, et al. Changes in serum levels of autotaxin with direct-acting antiviral therapy in patients with chronic hepatitis C. PLoS One 2018; 13:e0195632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kostadinova L, Shive CL, Zebrowski E, et al. Soluble markers of immune activation differentially normalize and selectively associate with improvement in AST, ALT, albumin, and transient elastography during IFN-free HCV therapy. Pathog Immun 2018; 3:149–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kostadinova L, Shive CL, Judge C, et al. During hepatitis C virus (HCV) infection and HCV-HIV coinfection, an elevated plasma level of autotaxin is associated with lysophosphatidic acid and markers of immune activation that normalize during interferon-free HCV therapy. J Infect Dis 2016; 214:1438–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. López-Cortés LF, Trujillo-Rodríguez M, Báez-Palomo A, et al. Eradication of hepatitis C virus (HCV) reduces immune activation, microbial translocation, and the HIV DNA level in HIV/HCV-coinfected patients. J Infect Dis 2018; 218:624–32. [DOI] [PubMed] [Google Scholar]
- 22. Kovanda A, Poljak M. Real-time polymerase chain reaction assay based on high-resolution melting analysis for the determination of the rs12979860 polymorphism involved in hepatitis C treatment response. J Virol Methods 2011; 175:125–8. [DOI] [PubMed] [Google Scholar]
- 23. Sandler NG, Koh C, Roque A, et al. Host response to translocated microbial products predicts outcomes of patients with HBV or HCV infection. Gastroenterology 2011; 141:1220–30, 30 e1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sandler NG, Wand H, Roque A, et al. ; INSIGHT SMART Study Group Plasma levels of soluble CD14 independently predict mortality in HIV infection. J Infect Dis 2011; 203:780–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kostadinova L, Shive CL, Anthony DD. Elevated autotaxin and LPA levels during chronic viral hepatitis and hepatocellular carcinoma associate with systemic immune activation. Cancers (Basel) 2019; 11:1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rockstroh JK, Orkin C, Viani RM, et al. Safety and efficacy of ombitasvir, paritaprevir with ritonavir ± dasabuvir with or without ribavirin in patients with human immunodeficiency virus-1 and hepatitis C virus genotype 1 or genotype 4 coinfection: TURQUOISE-I part 2. Open Forum Infect Dis 2017; 4:ofx154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ghany MG, Marks KM, Morgan TR, et al. Hepatitis C guidance 2019 update: AASLD-IDSA recommendations for testing, managing, and treating hepatitis C virus infection. Hepatology 2020; 71:686–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Molla A, Korneyeva M, Gao Q, et al. Ordered accumulation of mutations in HIV protease confers resistance to ritonavir. Nat Med 1996; 2:760–6. [DOI] [PubMed] [Google Scholar]
- 29. Isakov V, Koloda D, Tikhonova N, et al. Pharmacokinetics of the new hepatitis C virus NS3 protease inhibitor narlaprevir following single-dose use with or without ritonavir in patients with liver cirrhosis. Antimicrob Agents Chemother 2016; 60:7098–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zeremski M, Petrovic LM, Chiriboga L, et al. Intrahepatic levels of CXCR3-associated chemokines correlate with liver inflammation and fibrosis in chronic hepatitis C. Hepatology 2008; 48:1440–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Umemura T, Yamazaki T, Joshita S, et al. Quantitative analysis of serum chemokines associated with treatment failure of direct-acting antivirals in chronic hepatitis C. Cytokine 2018; 111:357–63. [DOI] [PubMed] [Google Scholar]
- 32. Serti E, Chepa-Lotrea X, Kim YJ, et al. Successful interferon-free therapy of chronic hepatitis C virus infection normalizes natural killer cell function. Gastroenterology 2015; 149:190–200e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Spaan M, van Oord G, Kreefft K, et al. Immunological analysis during interferon-free therapy for chronic hepatitis C virus infection reveals modulation of the natural killer cell compartment. J Infect Dis 2016; 213:216–23. [DOI] [PubMed] [Google Scholar]
- 34. Carlton-Smith C, Holmes JA, Naggie S, et al. ACTG A5327 study group IFN-free therapy is associated with restoration of type I IFN response in HIV-1 patients with acute HCV infection who achieve SVR. J Viral Hepat 2018; 25:465–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carlin AF, Aristizabal P, Song Q, et al. Temporal dynamics of inflammatory cytokines/chemokines during sofosbuvir and ribavirin therapy for genotype 2 and 3 hepatitis C infection. Hepatology 2015; 62:1047–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vergara C, Thio C, Latanich R, et al. Genetic basis for variation in plasma IL-18 levels in persons with chronic hepatitis C virus and human immunodeficiency virus-1 infections. Genes Immun 2017; 18:82–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Veenhuis RT, Astemborski J, Chattergoon MA, et al. Systemic elevation of proinflammatory interleukin 18 in HIV/HCV coinfection versus HIV or HCV monoinfection. Clin Infect Dis 2017; 64:589–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pleli T, Martin D, Kronenberger B, et al. Serum autotaxin is a parameter for the severity of liver cirrhosis and overall survival in patients with liver cirrhosis—a prospective cohort study. PLoS One 2014; 9: e103532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lidofsky A, Holmes JA, Feeney ER, et al. Macrophage activation marker soluble CD163 is a dynamic marker of liver fibrogenesis in human immunodeficiency virus/hepatitis C virus coinfection. J Infect Dis 2018; 218:1394–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Harris TB, Ferrucci L, Tracy RP, et al. Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med 1999; 106:506–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.