Abstract
Introduction
Given that people living with HIV (PLWH) are disproportionately burdened by tobacco-related morbidity and mortality, it is critically important to understand the degree to which evidence-based cessation interventions are utilized by and are effective among PLWH.
Aims and Methods
This secondary data analysis aimed to examine differences in Quitline treatment enrollment and 6-month cessation outcomes among smokers seeking care at 1 HIV clinic and 12 non-HIV clinics that were part of a large healthcare system in the greater Houston, Texas metropolitan area, United States. Data were from a 34-month (April 2013–February 2016) one-group implementation trial that evaluated the Ask-Advise-Connect (AAC) approach to linking smokers with Quitline treatment. Primary outcomes included (1) treatment enrollment and (2) 6-month self-reported and biochemically confirmed abstinence.
Results
The smoking status of 218 915 unique patients was recorded in the electronic health record; 5285 (2.7%) of these patients were seen at the HIV clinic where the smoking prevalence was 45.9%; smoking prevalence at the non-HIV clinics was 17.9%. The proportion of identified smokers who enrolled in treatment was 10.8% at the HIV clinic and 11.8% at the non-HIV clinics. The self-reported abstinence rate was 18.7% among HIV clinic patients and 16.5% among non-HIV clinic patients. Biochemically confirmed abstinence was lower at 4.2% and 4.5%, respectively (all ps > .05).
Conclusions
AAC resulted in rates of Quitline treatment enrollment and abstinence rates that were comparable among patients seen at an HIV clinic and non-HIV clinics. Findings suggest that AAC should be considered for widespread implementation in HIV clinics.
Implications
PLWH were as likely as other patients to enroll in evidence-based tobacco cessation treatment when it was offered in the context of a primary care visit. Cessation outcomes were also comparable. Therefore, standard care for PLWH should include routine screening for smoking status and referrals to cessation treatment.
Introduction
People living with HIV (PLWH) face disproportionally high risks of tobacco-related morbidity and mortality.1–6 Non-AIDS-defining cancers, particularly lung cancer, are now the leading non-AIDS causes of death among PLWH,7 and the overall mortality rate for PLWH who smoke is twice the mortality rate of nonsmoking PLWH.6,8 Smoking is also associated with poor viral and immunologic response to antiretroviral therapy.9 Therefore, tobacco cessation is critically important for this population.
Ask-Advise-Connect (AAC) is an electronic health record–based approach designed to streamline and facilitate enrollment in evidence-based tobacco treatment in primary care settings.10 This approach involves training clinic staff to (1) Ask every patient about their smoking status at every visit, (2) Advise all smokers to quit, and (3) offer to immediately Connect smokers with a state Quitline through an automated link within the electronic health record system. In two previous group-randomized trials among patients visiting primary care clinics in the greater Houston, Texas metropolitan area, AAC resulted in a 13- to 30-fold increase in treatment enrollment (7.8%–14.7% vs. 0.5%–0.6% in the control group).10,11 Furthermore, in our recent implementation study that evaluated AAC in 13 community health centers that were part of a large health system, we found that self-reported abstinence rates among patients linked with treatment via AAC (20% with nicotine replacement therapy [NRT] and 12.2% without NRT) were comparable to abstinence rates reported in the 2008 update of the Treating Tobacco Use and Dependence Clinical Practice Guideline (28.1% with medication and 12.7% without medication).12 This finding highlights that electronic referral–based approaches such as AAC have great potential to increase the reach of evidence-based tobacco cessation treatment among underserved smokers. However, given that the prevalence of smoking is dramatically higher among PLWH than among general primary care patients, it is important to examine whether simple electronic referral–based approaches such as AAC are effective in engaging high-risk patients such as PLWH in tobacco treatment. On the one hand, national data indicate that 97% of PLWH receive outpatient HIV care and that approximately half of these individuals receive ancillary or prevention services such as dental care, case management counseling, or nutrition assistance in these outpatient care settings.13 Therefore, given that PLWH are likely to be routinely offered prevention services in primary care settings, they may be more receptive than non-HIV patients to tobacco treatment when it is offered. On the other hand, comorbid mental health and substance abuse conditions are prevalent among PLWH and, as a result, treatment engagement and cessation outcomes may be poorer among PLWH than among non-HIV patients.13
The current study was unique in that 1 of the 13 community health centers that participated in the study specialized in providing care to PLWH. Therefore, the current study aimed to examine differences in treatment enrollment and 6-month smoking abstinence rates among smokers seeking care at 1 HIV clinic and those seeking care at 12 non-HIV clinics.
Methods
Details of the current study have been reported elsewhere.12 Briefly, this was a one-group implementation study. AAC was evaluated from April 2013 through February 2016 in 13 community health clinics that were part of a county health system in the greater Houston, Texas metropolitan area. One of the 13 clinics specialized in HIV/AIDS treatment and care and the remaining 12 were general primary care clinics. The patient population served was racially/ethnically diverse, all were uninsured or underinsured, and nearly half had annual household incomes below the poverty level.
Licensed vocational nurses were trained to ask all patients about their smoking status, give all smokers brief advice to quit, and offer connection to the Texas Quitline through an automated link within the electronic health record. Within 48 hours of receiving patients’ contact information, Quitline staff proactively called patients to offer enrollment in their standard proactive, 5-call counseling program. Approximately half of all patients who enrolled in Quitline treatment were provided with NRT after the first counseling call. The offer of NRT was based on the Quitline’s standard operating procedures, which were that NRT was provided only to participants residing in certain Texas counties, during certain months of the year, and when adequate funding was available.
This work is a post hoc secondary data analysis of our AAC implementation study.12 Primary outcomes included (1) treatment enrollment (ie, proportion of identified smokers that enrolled in treatment) and (2) 6-month self-reported and biochemically confirmed smoking abstinence rates among those who enrolled in treatment and agreed to be contacted for follow-up. Secondary outcomes included number of counseling calls completed and receipt of NRT. Due to the implementation focus of the study, it was not possible to collect other individual-level data such as sociodemographic and smoking history characteristics and we did not have Institutional Review Board approval to access to this information through the electronic health record. Treatment enrollment and abstinence rates were compared among PLWH and non-PLWH using chi-square tests. Logistic regression models were used to examine the impact of provision of NRT on self-reported and biochemically confirmed abstinence outcomes.
Results
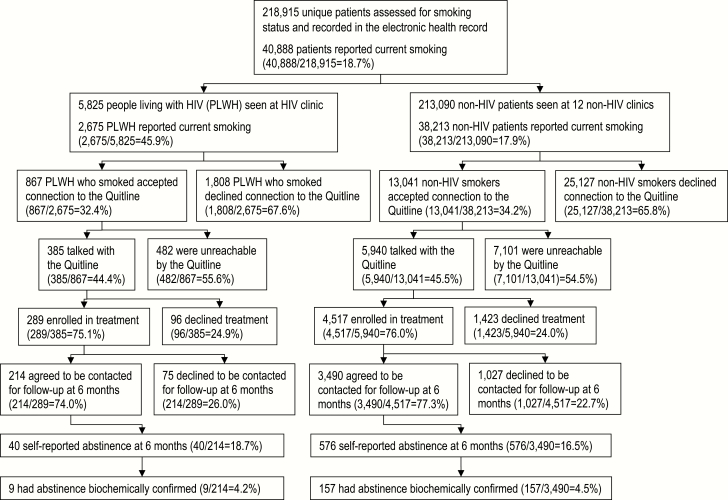
Figure 1 displays the participant flow through the study. The smoking status of 218 915 unique patients was assessed and recorded in the electronic health record. The prevalence of smoking was 45.9% (2675/5825) among PLWH seen at the HIV clinic and 17.9% (38 213/213 090) among patients seen at the other 12 non-HIV clinics. Thus, smoking prevalence among PLWH was more than 2.5 times that observed in the non-HIV patients. Overall, the treatment enrollment rates were 10.8% (289/2675) for identified PLWH who smoked and 11.8% (4517/38 213) for non-HIV smokers. Among smokers who enrolled in treatment and agreed to be contacted for follow-up at 6 months, utilizing an intention-to-treat approach (ie, missing = smoking), the self-reported abstinence rate was 18.7% (40/214) among PLWH and 16.5% (576/3490) among non-HIV group. Biochemically confirmed abstinence rate was 4.2% (9/214) among PLWH and 4.5% (157/3490) among non-HIV group. Treatment enrollment and smoking abstinence rates were not statistically different among PLWH and non-HIV patients (all ps > .05).
Figure 1.
Participant flow and cessation outcomes.
Table 1 displays the receipt of NRT and the number of counseling calls completed among smokers who enrolled in treatment and agreed to be contacted for follow-up in each group. PLWH who smoked completed fewer counseling sessions than non-HIV smokers (χ 2 p < .001). Overall, 40.2% in the PLWH group and 57.6% in the non-HIV group were provided with NRT (ie, patch, lozenge, or gum) by the Quitline. The receipt of NRT was statistically associated with a higher self-reported abstinence and higher biochemically confirmed abstinence at 6 months in non-HIV group but not among PLWH.
Table 1.
Receipt of Counseling Calls and NRT Among Patients Receiving Care at the HIV Clinic Versus Non-HIV Clinics
| HIV clinic | All other non-HIV clinics | |||||
|---|---|---|---|---|---|---|
| n/N | % | OR (95% CI) | n/N | % | OR (95% CI) | |
| Smokers who enrolled in the treatment with the Quitline and agreed to be contacted at the 6-month follow-up | 214 | 3490 | ||||
| Numbers of counseling calls completed | ||||||
| 0 | 80/214 | 37.4 | 1001/3490 | 28.7 | ||
| 1 | 68/214 | 31.8 | 1245/3490 | 35.7 | ||
| 2 | 36/214 | 16.8 | 570/3490 | 16.3 | ||
| 3–5 | 30/214 | 14.0 | 674/3490 | 19.3 | ||
| Provided with NRT by the Quitline | 86/214 | 40.2 | 2009/3490 | 57.6 | ||
| Self-reported abstinence rate at 6 months | ||||||
| Among patients provided with NRT | 20/86 | 23.3 | 1.64 (0.82 to 3.27) | 400/2009 | 20.0 | 1.84(1.52–2.23) |
| Among patients not provided with NRT | 20/128 | 15.6 | ref. | 176/1481 | 11.9 | ref. |
| Biochemically confirmed abstinence at 6 months | ||||||
| Among patients provided with NRT | 6/86 | 7.0 | 3.13 (0.76 to 12.85) | 118/2009 | 5.9 | 2.31 (1.59–3.34) |
| Among patients not provided with NRT | 3/128 | 2.3 | ref. | 39/1481 | 2.6 | ref. |
NRT = nicotine replacement therapy (ie, patch, lozenge, or gum); OR = odds ratio; CI = confidence interval.
Discussion
Our main finding is that there were no differences in Quitline treatment enrollment rates or 6-month smoking abstinence rates among PLWH and non-HIV smokers when AAC was implemented as part of standard clinical practice in a large healthcare system serving predominantly low-income, racial/ethnic minority patients who were uninsured or underinsured. Although the overall treatment enrollment rate of identified PLWH who smoked was modest (10.8%), the rate was consistent with that observed in non-HIV smokers in our sample (11.8%) and with enrollment rates observed in our previous trials evaluating AAC in primary care settings. Specifically, the current results were consistent with enrollment rates observed among patients receiving care at family practice clinics in our previous pair-matched group-randomized trial that established the efficacy of AAC (7.8%),10 and in other studies that used a similar electronic referral–based approach.14 It is encouraging that PLWH were just as likely as non-HIV smokers to enroll in evidence-based tobacco treatment when offered in the context of a primary care visit, and just as likely to have quit smoking at the 6-month follow-up assessment. This finding suggests that broad public health–based approaches involving simple electronic referrals for smoking cessation treatment are likely to have a meaningful impact among PLWH.
Nonetheless, the smoking prevalence observed among PLWH (45.9%) was 2.5 times higher than that observed among the non-HIV patients in our study and is consistent with the results of a recent meta-analysis that found a smoking prevalence of 54% among PLWH in high-income countries including the United States.15 Given the dramatically higher prevalence of smoking among PLWH, we should consider ways to increase the impact of AAC and other similar approaches to facilitating smoking cessation among PLWH. Our data showed that two-thirds of PLWH who smoked declined connection with the Quitline. Some previous studies have also reported that between 50% and 80% of PLWH who smoked were not interested in quitting in the next 30 days or in using a cessation program if available.16 Interventions designed specifically to enhance motivation to quit among PLWH who smoke may be needed.
Additionally, it may be necessary to consider improvement at both provider and systems levels. For example, healthcare team members who provide care for PLWH (eg, physicians, nurses, peer educators, and social workers) should be trained to consider tobacco cessation treatment a high priority in overall care for PLWH and should be encouraged to educate patients on the HIV-specific health benefits of cessation in the Advise component of AAC. In cases where patients may not be ready to quit following brief advice (ie, the Advise component of AAC), another HIV care provider (eg, a physician or peer educator) could be prompted to advise these patients again at future clinic visits. Since HIV is a chronic condition with antiretroviral therapy, the repeated clinic visits for HIV care also provide opportunities to monitor relapse and to offer additional or alternative cessation treatments. In general, smoking status should be frequently assessed and cessation treatments should be routinely offered to PLWH because even nonsustained periods of abstinence have demonstrated proven health benefits.17 Finally, NRT should be available to all PLWH who smoke and should be covered by HIV care or insurance programs.
This report has some important limitations. Given that the number of PLWH who enrolled in Quitline treatment and agreed to be contacted for follow-up was relatively small, it was not possible to make meaningful comparisons between subgroups (eg, those who received NRT and those who completed more counseling calls). Due to the unavailability of individual-level demographic and smoking history data, we could not examine differences by individual characteristics, including other substance use, sexual identities, and sexual orientations. This lack of individual sociodemographic data also limits the generalizability of our findings.
In conclusion, AAC resulted in Quitline treatment enrollment and cessation rates that were comparable for PLWH and non-HIV patients. Therefore, AAC should be widely implemented in HIV clinics to improve the health of PLWH. However, given the dramatically higher prevalence of smoking among PLWH, enhanced strategies tailored to the unique needs of PLWH may be needed to facilitate cessation. Specifically, interventions targeting provider- and systems-level factors may also have a meaningful impact on enhancing both treatment engagement and cessation outcomes.
Acknowledgments
This work was supported in part by the Cancer Prevention Research Institute of Texas (PP120191; PI: JI Vidrine), the Oklahoma Tobacco Settlement Endowment Trust (092-016-0002; PI: JI Vidrine), The University of Texas MD Anderson’s Cancer Center’s Cancer Center Support Grant (P30CA016672; PI: P. Pisters), and the Stephenson Cancer Center’s Cancer Center Support Grant (P30CA225520; PI: R. Mannel).
Declaration of Interests
All authors declare no conflicts of interest.
References
- 1. Shirley DK, Kaner RJ, Glesby MJ. Effects of smoking on non-AIDS-related morbidity in HIV-infected patients. Clin Infect Dis. 2013;57(2):275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nahvi S, Cooperman NA. Review: the need for smoking cessation among HIV-positive smokers. AIDS Educ Prev. 2009;21(3 suppl):14–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rahmanian S, Wewers ME, Koletar S, Reynolds N, Ferketich A, Diaz P. Cigarette smoking in the HIV-infected population. Proc Am Thorac Soc. 2011;8(3):313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reynolds NR. Cigarette smoking and HIV: more evidence for action. AIDS Educ Prev. 2009;21(3 suppl):106–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lifson AR, Neuhaus J, Arribas JR, van den Berg-Wolf M, Labriola AM, Read TR; INSIGHT SMART Study Group Smoking-related health risks among persons with HIV in the Strategies for Management of Antiretroviral Therapy clinical trial. Am J Public Health. 2010;100(10):1896–1903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Helleberg M, May MT, Ingle SM, et al. Smoking and life expectancy among HIV-infected individuals on antiretroviral therapy in Europe and North America. AIDS. 2015;29(2):221–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goncalves PH, Montezuma-Rusca JM, Yarchoan R, Uldrick TS. Cancer prevention in HIV-infected populations. Semin Oncol. 2016;43(1):173–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Crothers K, Griffith TA, McGinnis KA, et al. The impact of cigarette smoking on mortality, quality of life, and comorbid illness among HIV-positive veterans. J Gen Intern Med. 2005;20(12):1142–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Feldman JG, Minkoff H, Schneider MF, et al. Association of cigarette smoking with HIV prognosis among women in the HAART era: a report from the women’s interagency HIV study. Am J Public Health. 2006;96(6):1060–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vidrine JI, Shete S, Cao Y, et al. Ask-Advise-Connect: a new approach to smoking treatment delivery in health care settings. JAMA Intern Med. 2013;173(6):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vidrine JI, Shete S, Li Y, et al. The Ask-Advise-Connect approach for smokers in a safety net healthcare system: a group-randomized trial. Am J Prev Med. 2013;45(6):737–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pineiro B, Vidrine DJ, Wetter DW, et al. Implementation of Ask-Advise-Connect in a safety net healthcare system: quitline treatment engagement and smoking cessation outcomes. Transl Behav Med. 2018. [Epub ahead of print]. doi:10.1093/tbm/iby108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. Behavioral and clinical characteristics of persons with diagnosed HIV infection. Medical Monitoring Project, United States, 2016 Cycle (June 2016–May 2017); June 2019; Atlanta, GA. [Google Scholar]
- 14. Jenssen BP, Muthu N, Kelly MK, et al. Parent eReferral to tobacco quitline: a pragmatic randomized trial in pediatric primary care. Am J Prev Med. 2019;57(1):32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Park LS, Hernandez-Ramirez RU, Silverberg MJ, Crothers K, Dubrow R. Prevalence of non-HIV cancer risk factors in persons living with HIV/AIDS: a meta-analysis. AIDS. 2016;30(2):273–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Browning KK, Wewers ME, Ferketich AK, Diaz P. Tobacco use and cessation in HIV-infected individuals. Clin Chest Med. 2013;34(2):181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pool ER, Dogar O, Lindsay RP, Weatherburn P, Siddiqi K. Interventions for tobacco use cessation in people living with HIV and AIDS. Cochrane Database Syst Rev. 2016;6:Cd011120. [DOI] [PMC free article] [PubMed] [Google Scholar]