Introduction
Intracardiac mapping of accessory pathways has continued to evolve and contribute to high success rates for catheter ablations in pediatrics, ranging from 78% to 98%.1, 2, 3 With 3-dimensional electroanatomic mapping, increasing point density improves the accuracy of substrate prediction and modeling, particularly as the course of atrioventricular (AV) accessory pathways can be variable, with oblique atrial and ventricular insertion sites or multiple pathways that make accurate mapping challenging.4 The Advisor high-density HD Grid catheter (Abbott Laboratories, Abbott Park, IL) allows for bipolar recordings on 2 orthogonal planes among 18 electrodes to facilitate both the identification of small-amplitude high-frequency electrical impulses and the direction of impulse propagation. Although several adult studies have shown the utility of the HD Grid for mapping arrhythmia substrate5, 6, 7, 8 including accessory pathways,9 to our knowledge there are no studies showing the utilization of the HD Grid for mapping accessory pathways in pediatrics. In this case series, we describe our initial experience utilizing the HD Grid for mapping accessory pathways in the pediatric population.
Key Teaching Points.
-
•
Pediatric accessory pathways are common and historically have had a high cure rate with ablation. There are new techniques and technologies being developed to potentially increase efficacy of ablation with improved mapping.
-
•
There may be a role in utilizing open-window mapping and the HD Grid catheter (Abbott Laboratories, Abbott Park, IL) to delineate difficult or refractory accessory pathways in pediatrics.
-
•
New technology that allows for bipolar orthogonal electrograms can be safely used in the pediatric population.
Advisor HD Grid catheter design
The Advisor HD Grid is a high-definition mapping catheter that has 18 electrodes and allows for assessment of voltage, activation, and directionality of conduction. This unique design consists of 4 parallel splines equally spaced 3 mm apart, each with four 1-mm electrodes that are spaced 3 mm apart (4 × 4 electrode configuration), with 2 additional electrodes on the shaft. Figure 1 incorporates a depiction of the HD Grid catheter. When compared to conventional linear catheters, the HD Grid is able to utilize its electrodes in orthogonal orientations along and across adjacent splines to collect multiple bipolar electrograms (EGMs) at any given time. EnSite Precision (Abbott Laboratories) then compares the orthogonal bipolar EGMs in a single location by factoring in local activation timing, peak-to-peak voltage, and other algorithms to display the best point at that site. We utilized a high-density open-window mapping technique, where all local atrial, pathway, and ventricular signals are recorded. The absolute dV/dt detection algorithm identifies and annotates the highest absolute slope on the bipolar EGM, which directly corresponds to the largest local timing difference between the positive and negative electrode unipolar EGM.10 The system calculates this sharpest, near-field location by calculating the derivative of the bipolar EGM for the entire mapping window, then annotates the point in that window with the highest positive or negative slope. The near-field annotation does not specifically differentiate between atrial and ventricular EGMs in a single point, but instead the mapping technique utilizes thousands of points to map the conduction across the pathway and guide ablation strategy. This technique differs from the conventional mapping approach, which maps the earliest activation site only in the chamber activated by the pathway and relies on subjective analysis for local timing when annotating fused annular signals.
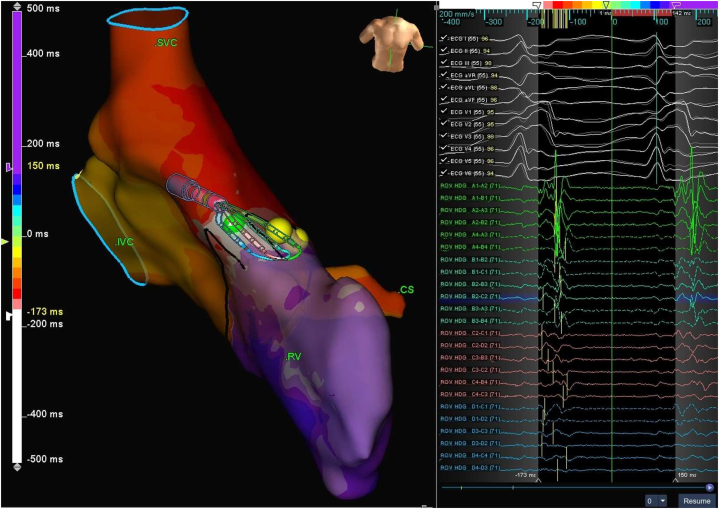
Figure 1.
Patient 1. HD Grid (Abbott Laboratories, Abbott Park, IL) local activation timing map is depicted while mapping in sustained orthodromic atrioventricular tachycardia for this para-Hisian accessory pathway. The HD Grid is positioned at the accessory pathway and near the location of initial successful ablation lesion (green dot), which was slightly superior to the His bundle (yellow dots). The intracardiac electrograms from the HD Grid are shown on the right. CS = coronary sinus; IVC = inferior vena cava; RV = right ventricle; SVC = superior vena cava.
Despite its larger mapping surface, the HD Grid is atraumatic and positioned with the 3D electroanatomical mapping system without the use of fluoroscopy. Of note, it is our institution’s practice to anticoagulate when the HD Grid is deployed for both right- and left-sided procedures.
Mapping is conducted in pre-excited sinus rhythm, coronary sinus atrial paced rhythm, orthodromic AV reentrant tachycardia, or ventricular paced rhythm, as determined by the arrhythmia substrate and the discretion of the pediatric electrophysiologists. After mapping was performed with the HD Grid, limited micromovements of the ablation catheter allowed for confirmation of the pathway location and lesion(s) were subsequently placed.
Case report
From January to March 2020, 5 patients had invasive electrophysiology studies for accessory pathways utilizing the HD Grid. All patients had normal heart structures, with the exception of 1 who had a small atrial septal defect. Pathway location and characteristics are presented in Table 1. Table 2 reports the specifics of the HD Grid maps for each patient. Of note, although the patients in this study were in the pediatric age range, they were all near adult sized (83, 48, 89, 45, and 80 kg).
Table 1.
Summary of patient characteristics and findings of electrophysiology study and ablation procedures
| Patient # | Weight (kg) | Prior ablation(s) | Pathway location | Pathway characteristics | AP block cycle length (ms) | Ablation energy | Total ablation time (s) | Successful ablation of pathway |
|---|---|---|---|---|---|---|---|---|
| 1 | 83 | 3 | Para-Hisian | Antegrade and retrograde | 350 | Cryoablation | 1149 | Yes |
| 2 | 48 | 1 | Right lateral | Antegrade | 350 | Radiofrequency | 393 | Yes |
| 3 | 89 | 0 | Para-Hisian | Antegrade and retrograde | 340 | Cryoablation | 508 | Yes |
| 4 | 45 | 0 | Right posterior septal | Antegrade | 350 | Radiofrequency | 211 | Yes |
| 5 | 80 | 1 | Para-Hisian | Retrograde | 360 | Cryoablation | 363 | No, secondary to intermittent heart block |
AP = accessory pathway.
Table 2.
Summary of mapping with the Advisor high-definition HD Grid catheter (Abbott Laboratories, Abbott Park, IL)
| Patient # | Pathway location | # of map(s) | Rhythm for map | Time per map | # of points displayed per map | Total # of points collected per map |
|---|---|---|---|---|---|---|
| 1 | Para-Hisian | 2 | Pre-excited sinus | 9 min 20 s | 976 | 11,213 |
| Orthodromic AV tachycardia | 3 min 43 s | 1075 | 11,257 | |||
| 2 | Right lateral | 1 | Pre-excited sinus | 8 min 53 s | 1123 | 13,974 |
| 3 | Para-Hisian | 1 | Pre-excited sinus | 11 min 3 s | 1905 | 15,412 |
| 4 | Right posterior septal | 2 | Pre-excited sinus | 9 min 27 s | 1329 | 10,814 |
| Coronary sinus atrial pacing | 6 min 2 s | 1403 | 8262 | |||
| 5 | Para-Hisian | 4 | RV apical pacing | 5 min 9 s | 1225 | 12,594 |
| RV mid-septal pacing | 14 min 30 s | 1055 | 20,037 | |||
| Orthodromic AV tachycardia 300 ms | 2 min 45 s | 833 | 22,512 | |||
| Orthodromic tachycardia 320 ms | 7 min 6 s | 1425 | 23,466 |
The median number of total points per map collected was 14,954 (range 8262–23,466) points and the median number of points displayed per map was 1174 (range 833–1905) points. The median time to create each map was 8 minutes (range 2.5–14 minutes).
AV = atrioventricular; RV = right ventricle.
Patient 1
A 16-year-old female patient (83 kg) was referred after 3 prior unsuccessful ablations for a para-Hisian accessory pathway with bidirectional properties. The HD Grid catheter was utilized to create 2 maps: 1 in pre-excited sinus rhythm and 1 in sustained orthodromic AV reentrant tachycardia. Both maps identified the same location for the accessory pathway, as seen in Figure 1. EGMs are displayed in Supplemental Figure S1. With the guidance of the maps created by the HD Grid, the first lesion was placed with a 6-mm-tip Freezor Xtra (Medtronic, Minneapolis, MN) cryoablation catheter in the para-Hisian position, slightly superior to the His bundle position. Of note, signals from the ablation catheter were low amplitude, suggesting possible scarring from prior ablation lesions. The accessory pathway disappeared as the ice ball formed, which was 20 seconds from cryoablation initiation.
Patients 2 and 3
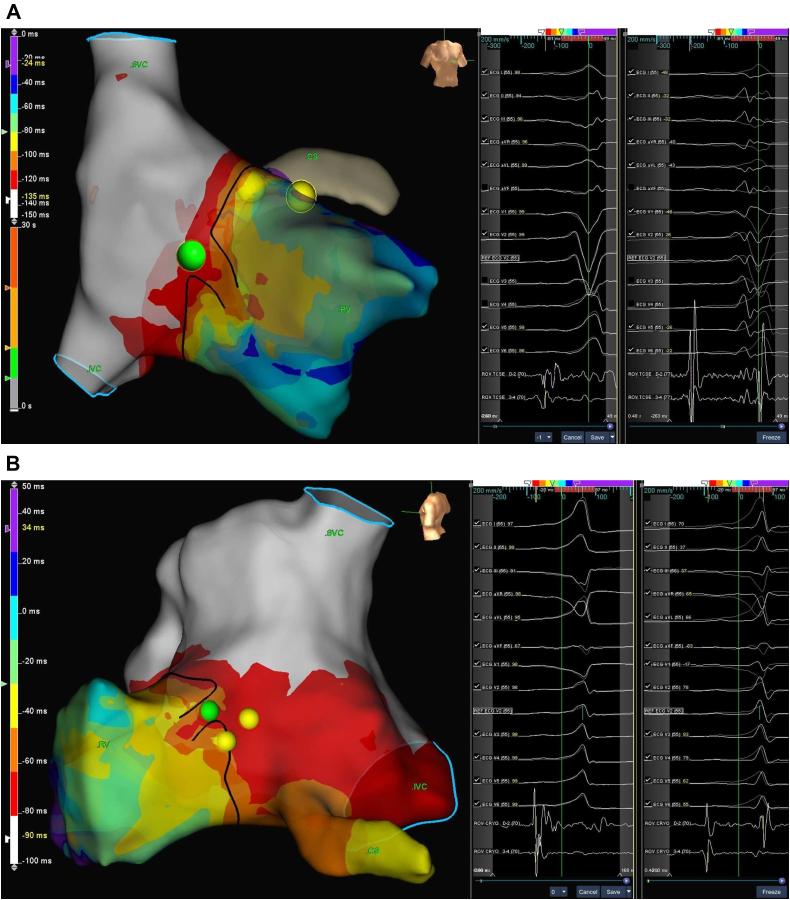
Patients 2 and 3 are presented together, as both had HD Grid mapping in pre-excited sinus rhythm (Figure 2A and B).
Figure 2.
A: Patient 2. B: Patient 3. Both HD Grid (Abbott Laboratories, Abbott Park, IL) local activation maps were created in pre-excited sinus rhythm with the ablation lesion (green dot) depicted relative to the His bundle (yellow dots). The intracardiac electrogram for each patient is shown to the right of the respective map. The views are angled to best show the mapping and successful ablation site. CS = coronary sinus; IVC = inferior vena cava; RV = right ventricle; SVC = superior vena cava.
Patient 2 was a 13-year-old female patient (48 kg) who had a prior successful ablation for 2 right-sided accessory pathways (right lateral and right anterior septal). She was referred because of recurrence of the right lateral pathway. This pathway conducted antegrade only and was able to sustain antidromic AV reentrant tachycardia. A TactiCath SE (Abbott Laboratories) radiofrequency irrigated catheter was used, and the first lesion placed resulted in prompt loss of the accessory pathway at 1.5 seconds.
Patient 3 was an 11-year-old female patient (89 kg) who had a para-Hisian pathway with bidirectional properties and a small secundum atrial septal defect. Mapping revealed the pathway location to be slightly anterior to the His bundle. Utilizing a 6-mm-tip Freezor Xtra cryoablation catheter, the first lesion was placed more superiorly than the map suggested, at the decision of the operator, and did not affect pathway conduction. The catheter was then moved to the location of the pathway as directed by the map. The time from cryoablation on to ice ball formation was 14 seconds and the accessory pathway disappeared 3.5 seconds after ice ball formation.
Patient 4
A 12-year-old female patient (45 kg) had an antegrade-only right posterior septal pathway. This pathway was mapped with the HD Grid in pre-excited sinus rhythm and coronary sinus atrial paced rhythm, as seen in Supplemental Figure S2. When the ablation catheter was advanced to the right AV groove and placed near but not on the site of the pathway, as guided by the HD Grid map, the ablation signal was assessed to be a good target for ablation. Initially, 2 lesions were placed with a Blazer II (Boston Scientific, Marlborough, MA) radiofrequency catheter and were unsuccessful in terminating the pathway. The ablation catheter was readjusted and brought to the precise site of the pathway in the inferior septal position, as guided by the HD Grid map. Ablation at this site resulted in accessory pathway block at 2.5 seconds after radiofrequency initiation.
Patient 5
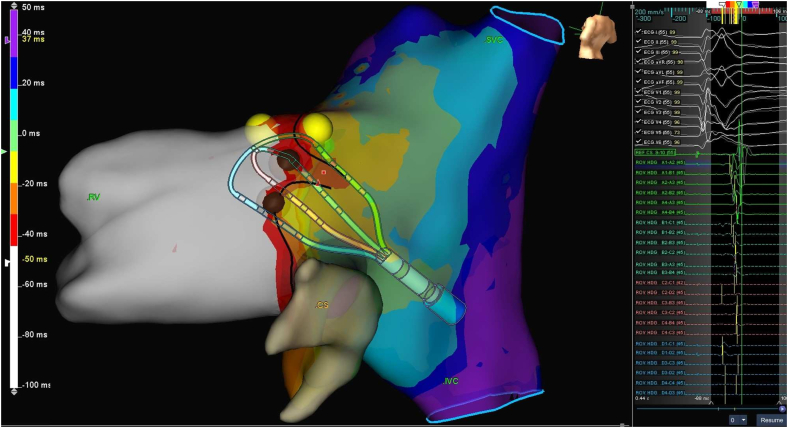
A 14-year-old female patient (80 kg) had been referred after an unsuccessful ablation for a retrograde para-Hisian pathway. Four separate HD Grid maps were created: (1) right ventricular apical pacing, (2) right ventricular mid-septal pacing, (3) orthodromic AV reentrant tachycardia (cycle length 300 ms), and (4) orthodromic AV reentrant tachycardia (320 ms). All 4 maps showed that the pathway consistently coursed just below the His bundle, as seen in Figure 3. Using a Freezor Xtra catheter, cryoablation lesions placed in this region repeatedly resulted in transient A-H prolongation and 2:1 AV node block. Mapping and ablation from the noncoronary aortic cusp was not performed secondary to family preference. Owing to risk of permanent AV nodal damage, no further attempts were made.
Figure 3.
Patient 5. HD Grid (Abbott Laboratories, Abbott Park, IL) local activation map was created in right ventricle (RV) mid-septal pacing. The HD Grid is positioned near the pathway location. The unsuccessful ablation lesions (brown dots) are depicted on the map in close proximity to the His bundle (yellow dots). The electrograms from the HD Grid catheter are depicted to the right of the map. IVC = inferior vena cava; SVC = superior vena cava.
Discussion
To our knowledge, this is the first study demonstrating utilization of the Advisor HD Grid in pediatric patients for intracardiac electroanatomic mapping of accessory pathways. This initial series shows that the HD Grid can be used safely and effectively in this patient population. There were no complications from the use of the HD Grid, including vascular access or anticoagulation complications. Of note, for these right-sided procedures, only the 3D EnSite system was utilized to track catheter movement. No fluoroscopy was necessary. Further studies are needed to delineate the utility of the HD Grid in all pathway locations.
Acknowledgments
The authors would like to thank Austin Davies, BS, BME, from Abbott Laboratories for his contribution to our understanding of the technical aspects of the HD Grid and preparation of the electroanatomic mapping figures.
Footnotes
Funding Sources: No honorarium, grant, or other form of payment was given to anyone to produce the manuscript. Disclosure: No conflicts of interest from any author.
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hrcr.2020.09.009.
Appendix. Supplementary data
Three bipolar EGMs are shown with the surface leads at the ablation site for Patient 1. The A1-A2 and A1-B1 are both measured simultaneously in an orthogonal fashion by the HD Grid and highlight that signals can vary based on orientation. The Tacticath D2 EGM is displayed at the same location. The ablation catheter by conventional analysis would not be deemed an ideal “fused” signal for ablation. Instead of relying on the subjective analysis of one signal to determine an ablation site, the HD Grid catheter uses a multitude of data points to find the best signal.
Patient 4. HD Grid local activation map was created in coronary sinus atrial pacing with the successful ablation site shown (green dot) in relation to the His Bundle (yellow dots). The electrograms depict the pre- and post-ablation electrograms from the ablation catheter at the successful site. The diagram is depicted in a non-standard view for best visualization of the pathway location. † Abbreviations: SVC = superior vena cava; IVC = inferior vena cava; RV = right ventricle; CS = coronary sinus.
References
- 1.van Hare G.F., Javitz H., Carmelli D. Prospective assessment after pediatric cardiac ablation: Demographics, medical profiles, and initial outcomes. J Cardiovasc Electrophysiol. 2004;15:759–770. doi: 10.1046/j.1540-8167.2004.03645.x. [DOI] [PubMed] [Google Scholar]
- 2.Kubuš P., Vít P., Gebauer R.A. Long-term results of paediatric radiofrequency catheter ablation: A population-based study. EP Europace. 2014;16:1808–1813. doi: 10.1093/europace/euu087. [DOI] [PubMed] [Google Scholar]
- 3.Kugler J.D., Danford D.A., Houston K.A., Felix G. Pediatric Radiofrequency Catheter Ablation Registry success, fluoroscopy time, and complication rate for supraventricular tachycardia: Comparison of early and recent eras. J Cardiovasc Electrophysiol. 2002;13:336–341. doi: 10.1046/j.1540-8167.2002.00336.x. [DOI] [PubMed] [Google Scholar]
- 4.Ceresnak S.R., Dubin A.M., Kim J.J. Success rates in pediatric WPW ablation are improved with 3-dimensional mapping systems compared with fluoroscopy alone: A multicenter study. J Cardiovasc Electrophysiol. 2015;26:412–416. doi: 10.1111/jce.12623. [DOI] [PubMed] [Google Scholar]
- 5.Tan V.H., Lyu M.Z., Tan P.C., Wong L.C., Yeo C., Wong K.C.K. Utility of directional high-density mapping catheter (Advisor TM HD Grid) in complex scar-related atrial tachycardia. J Arrhythm. 2020;36:180–183. doi: 10.1002/joa3.12256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okubo K., Frontera A., Bisceglia C. Grid mapping catheter for ventricular tachycardia ablation. Circ Arrhythm Electrophysiol. 2019;12 doi: 10.1161/CIRCEP.119.007500. [DOI] [PubMed] [Google Scholar]
- 7.Sawhney V., Garcia J., Daw H. 137 Validation and utility of a novel mapping system in ablation of complex arrhythmias in adult congenital heart disease: a multicentre UK study. Heart. 2019;105:A113–A114. [Google Scholar]
- 8.Hong K.L., Redfearn D., Chacko S., Baley J., Baranchuk A., Glover B.M. High-resolution mapping of the atria using the HD Grid catheter. HeartRhythm Case Rep. 2019;5:351–353. doi: 10.1016/j.hrcr.2018.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arroyo R.C., Chatzikyriakou S. Characterization of accessory pathways using an orientation-independent catheter. JACC Clin Electrophysiol. 2018;4:1379–1381. doi: 10.1016/j.jacep.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 10.Stevenson W.G., Soejima K. Recording techniques for clinical electrophysiology. J Cardiovasc Electrophysiol. 2005;16:1017–1022. doi: 10.1111/j.1540-8167.2005.50155.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Three bipolar EGMs are shown with the surface leads at the ablation site for Patient 1. The A1-A2 and A1-B1 are both measured simultaneously in an orthogonal fashion by the HD Grid and highlight that signals can vary based on orientation. The Tacticath D2 EGM is displayed at the same location. The ablation catheter by conventional analysis would not be deemed an ideal “fused” signal for ablation. Instead of relying on the subjective analysis of one signal to determine an ablation site, the HD Grid catheter uses a multitude of data points to find the best signal.
Patient 4. HD Grid local activation map was created in coronary sinus atrial pacing with the successful ablation site shown (green dot) in relation to the His Bundle (yellow dots). The electrograms depict the pre- and post-ablation electrograms from the ablation catheter at the successful site. The diagram is depicted in a non-standard view for best visualization of the pathway location. † Abbreviations: SVC = superior vena cava; IVC = inferior vena cava; RV = right ventricle; CS = coronary sinus.