Highlights
-
•
The 24-h composition of movement behaviors may have important implications for health at all ages.
-
•
Children and youth who meet the 24-h movement guideline recommendations generally report more favorable health indicators than those who do not.
-
•
Adherence rates to the 24-h movement guideline recommendations were low.
-
•
Sociodemographic, lifestyle, and environmental factors were associated with guideline adherence.
-
•
A healthy composition of 24-h movement behaviors and meeting the recommended guidelines are important for disease prevention and health promotion across the lifespan.
Keywords: Compositional analysis, Movement behaviors, Physical activity, Sedentary behavior, Sleep
Abstract
Background
New research suggests that the composition (mix) of movement behaviors within a 24-h period may have important implications for health across the lifespan. Consistent with this integrated movement behavior paradigm, a number of countries across the world have developed and released 24-h movement guidelines for specific age groups. The purpose of this systematic review was to examine the associations between the 24-h time-use composition of movement behaviors, or adherence to 24-h movement guidelines, and multiple health indicators across the lifespan.
Methods
Five online databases (PsycINFO, PubMed, SPORTDiscus, Web of Science, and Ovid MEDLINE) were searched for relevant peer-reviewed studies published between January 2015 and January 2020 that met the a priori inclusion criteria, with no study design limits. The methodological quality of research evidence for each individual study and for each health indicator was assessed by using a modified version of the Downs and Black checklist.
Results
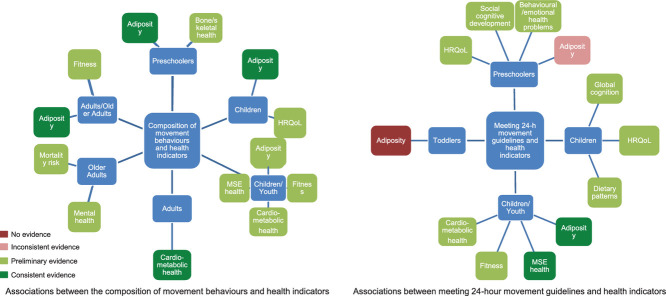
A total of 51 studies from 20 different countries met the inclusion criteria. A total of 31 studies examined adherence (meeting vs. not meeting) to 24-h movement guidelines, and 20 studies used compositional analyses to explore the 24-h time-use composition of movement behaviors. Findings indicated that meeting the 24-h movement guidelines were (1) not associated with adiposity among toddlers, (2) favorably associated with health-related quality of life, social-cognitive development, and behavioral and emotional problems among preschoolers, (3) favorably associated with global cognition, health-related quality of life, and healthy dietary patterns in children, and (4) favorably associated with adiposity, fitness, and cardiometabolic, mental, social, and emotional health among children and youth. Significant associations were also found between the composition of 24-h movement behaviors and indicators of (1) adiposity and bone and skeletal health among preschoolers, (2) health-related quality of life among children, (3) adiposity, fitness, and cardiometabolic, social, and emotional health among children and youth, (4) cardiometabolic health in adults, (5) adiposity and fitness among adults and older adults, and (6) mental health and risk of mortality among older adults. The quality of the available evidence ranged from poor to good.
Conclusion
The current evidence indicates that the composition of movement behaviors within a 24-h period may have important implications for health at all ages and that meeting the current 24-h movement guidelines is associated with a number of desirable health indicators in children and youth. Future studies should employ longitudinal and experimental designs, include valid and reliable measures of 24-h movement behaviors, and examine a wide array of health indicators across all age groups. Such studies would confirm the results from the primarily cross-sectional evidence drawn from studies included in our review and further advance our understanding of the relationships between 24-h movement behaviors and health.
Graphical Abstract
1. Introduction
From a movement perspective, the 24-h period is distributed among sleep, sedentary behavior (SB), and physical activity (PA) on a continuum from no movement to high movement. Over the past decade, an increasing number of studies have highlighted the separate health benefits of high PA, low SB, and sufficient sleep among children1, 2, 3, 4, 5, 6 and adults.7, 8, 9 Until recently, the health implications of time spent in each of these movement behaviors have traditionally been examined in isolation or with only partial adjustment for time spent in other movement behaviors.10
Consequently, researchers have begun to investigate the combined effects of 24-h movement behaviors on health. It has been shown that specific combinations of movement behaviors (e.g., high PA, low SB, and high sleep) are associated with desirable health indicators for the early years (0–4 years old; e.g., motor development, fitness) and for children (5–11 years old) and youth (12–17 years old; e.g., adiposity, cardiometabolic health).11,12 More recently, studies have also examined the associations between health indicators and the reallocation of a fixed duration of one movement behavior for another, using isotemporal substitution methodologies.13 A systematic review of studies that employed isotemporal substitution models in PA, SB, and sleep research was conducted in 2018, synthesizing 56 studies.14 The main conclusion of that review was that time reallocation between sleep, SB, light PA (LPA), and moderate-to-vigorous PA (MVPA) was associated with a number of health outcomes. In particular, reallocations of time spent in SB to LPA or MVPA were associated with significant reductions in mortality risk as well as indicators of adiposity, including body mass index (BMI), body fat percentage, and waist circumference in all age groups. Beneficial associations between the reallocation of time from SB to LPA or MVPA and cardiometabolic biomarkers were also reported among adults.14 Traditional isotemporal substitution models allow for a more comprehensive perspective on how movement behaviors relate to health, but one limitation of this method is its inability to provide an overall assessment of the association between the 24-h movement profile and health indicators due to multicollinearity issues that arise when all movement behaviors within a finite period are included in the same model.15 Traditional isotemporal substitution is based on regression modeling that assumes independence among variables and is unable to adjust correctly for all behaviors on the movement continuum.13,16 These methodological challenges prevent a complete understanding of the collective impact of these movement behaviors on health and well-being.
A technique new to the health field for analyzing 24-h movement behavior data—compositional data analysis—has recently been introduced.16 This approach addresses the challenges associated with examining the health implications of 24-h movement behaviors. The total time spent in various movement behaviors during a 24-h period is finite, intrinsically collinear, and codependent, and together they constitute a composite whole.16 Compositional analyses deal specifically with codependent data by conceptualizing movement behavior data as compositions that exist in a constrained space (i.e., simplex) governed by a specific geometry (Aitchison geometry).17 Compositional analyses can be used to examine both the combined and relative associations of 24-h movement behaviors with health indicators. Importantly, the compositional isotemporal substitution technique is not limited to creating estimates only for the substitution of a single behavior (e.g., SB) with another behavior (e.g., MVPA) but, rather, the behavior of interest could be substituted by several behaviors (e.g., MVPA and sleep).18 New research that has applied an integrated approach suggests that the composition (mix) of movement behaviors within a 24-h period may have important implications for health at all ages.16,19,20 An increasing number of studies using compositional analyses have recently been conducted and published, investigating outcomes, such as adiposity, cardiometabolic biomarkers, fitness, bone health, mortality, social and emotional health, and health-related quality of life. Collectively, current evidence suggests the whole 24-h time use is associated with health indicators in children and adults.
Consistent with this integrated vs. segregated movement-behavior paradigm, the Canadian 24-Hour Movement Guidelines for Children and Youth (aged 5–17 years old)21 (Supplementary Table 1) and the Early Years (aged 0–4 years old)22 (Supplementary Table 1) were developed and released in 2016 and 2017, respectively. Canada was the first country to establish these guidelines; however, a number of other countries, including Australia,23 New Zealand,24 South Africa,25 and the World Health Organization26 have recently developed similar guidelines. The world's first 24-h movement guidelines for adults and older adults will be released by Canada in October of 2020.
In setting these recommendations, the 24h movement guidelines establish measurable targets for surveillance and provide guidance to health professionals, researchers, decision makers, and the general public. Understanding the mix of PA, SB, and sleep on public health and well-being is in its infancy and requires further investigation using this new paradigm. Recently, a number of studies have examined whether adhering to each of the recommendations in the guidelines is associated with desirable health outcomes in children and youth.27, 28, 29 Now that 24h movement guidelines have been released and are under development in other countries, it is important to gain a more thorough understanding of the proportion of individuals who simultaneously achieve all of the movement-behavior recommendations and the associations between meeting the guideline recommendations, or portions thereof, and health indicators. This information could be used to inform the development of programs and policies to promote healthy movement behaviors and be used to compare movement behavior practices between jurisdictions. To our knowledge, no previous review has comprehensively examined the literature on the association between 24-h time-use composition of movement behaviors or adherence to 24-h movement guidelines and multiple health indicators across the lifespan.
Given the rapid adoption of the 24-h movement paradigm and in order to summarize the current evidence in this growing field and provide directions for future research, a comprehensive review of the 24-h composition of movement behaviors and compliance with 24-h movement guidelines, as well as their relationship with health outcomes, is warranted. Therefore, the purpose of this systematic review was to synthesize and critique the current evidence on 24-h movement guideline adherence, correlates, and associations with health indicators across the lifespan, as well as the relationships between the composition of 24-h movement behaviors and health indicators. Further objectives were to appraise the methodological quality of the studies and suggest future research directions in this area.
2. Methods
2.1. Protocol and registration
This review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (Registration no. CRD42020165779; available from www.crd.york.ac.uk/PROSPERO/) and conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.30
2.2. Information sources and search strategy
A systematic search of the following electronic databases was performed in January 2020: PsycINFO, PubMed, SPORTDiscus, Web of Science, and Ovid MEDLINE. Date limits of January 2015 and later were included in the search because the seminal paper using compositional analyses for examining 24-h movement behaviors was published in 2015,16 and the first 24-h movement guidelines were released only in 2016;21 hence, no eligible studies would have been conducted prior to 2015. The search strategy was agreed upon by SR, OA, and MST and involved entering the following search terms into the above-mentioned databases: ((24-hour OR integrated OR daily) AND (movement behaviours OR movement guidelines OR physical behaviours OR activity behaviours) OR ((physical activity AND sedentary OR screen time AND sleep). The search strategy was constructed for PubMed, and the search terms were then adapted for other research databases in combination with database-specific filters. Because this was the first systematic review to focus exclusively on the 24-h composition of movement behaviors and adherence to 24-h movement guidelines, the search was not limited to specific populations. For the purpose of this specifıc review, studies that involved populations of any age (e.g., infants, preschoolers, children, youth, adults, older adults) were included. No study design limits were included; however, searches were limited to publications in English.
After identification of studies through database searching, duplicate records were removed. Two independent reviewers screened titles and abstracts of all records retrieved, and full-text articles were obtained for potentially relevant records. Two independent reviewers then examined all full-text articles to determine eligibility. Agreement between reviewers was required for article inclusion. Discrepancies were resolved by discussion between reviewers or with a third reviewer, if necessary. In addition to the search of databases, the review team's personal databases and the reference lists of included articles were also checked for potentially relevant studies missed by the search.
2.3. Inclusion criteria
To be included in the current review, studies were required to meet the following criteria: (1) the study was published in an English-language, refereed journal with full-text availability; (2) the study contained original research (i.e., reviews were not considered); (3) the study included one or more assessment of each 24-h movement behavior, that is, PA, SB (or screen time), and sleep; and (4) the study examined adherence (meeting vs. not meeting) to 24-h movement guidelines—PA, screen time, and sleep—or used compositional analyses to explore the 24-h time-use composition of movement behaviors—PA, SB (or screen time), and sleep. Primary outcomes of interest were the associations between compliance with the overall 24-h movement-guideline recommendations or the composition of 24-h movement behaviors and health indicators or outcomes.
2.4. Data extraction and synthesis
All included articles were summarized in table format using Microsoft Excel (Microsoft 2010, Version 14.7.7; Redmond, WA, USA), and descriptive study characteristics (author, publication year, country, study design, population, sample size, and type of sample), exposure/comparator, outcome measures, and results information were extracted. Study findings were considered statistically significant at p < 0.05. Data extraction was conducted by one reviewer and checked for accuracy by a second reviewer. Reviewers were not blinded to the authors or journals when extracting data.
Meta-analyses were planned for data that were sufficiently homogeneous in terms of statistical, clinical, and methodological characteristics. However, because of high levels of heterogeneity for the above characteristics across studies, it was determined that meta-analyses were not possible. As a result, a narrative synthesis structured around the exposure type—(1) 24-h movement guideline adherence and (2) 24-h movement behavior composition—and specific health indicators was conducted. Results were also synthesized separately for different age groups (e.g., preschoolers, children, youth, and adults) and presence of health condition(s). For purposes of this review, the following age ranges were used to categorize study populations: infants (aged < 1 year), toddlers (aged 1–2 years), preschoolers (aged 3–4 years), children (aged 5–11 years), youth (aged 12–17 years), adults (aged 18–64 years), and older adults (aged ≥65 years). When possible, subgroup analyses were conducted within each indicator to examine potential differences in results according to sex (males vs. females).
2.5. Methodological quality appraisal
The methodological quality of individual studies was assessed using a modified version of the Downs and Black checklist.31 The Downs and Black instrument consists of 27 items that assess study quality, including strength of reporting, external validity, internal validity (bias), internal validity (confounding), and power. A modified version of the checklist was employed in our study, and 10 items that were not relevant to observational studies were removed (Items 8, 13–15, 17, 19, and 21–24) from the original checklist. The adapted checklist consisted of 19 items, including 12 items from the original list (Items 1–3, 6, 7, 10–12, 16, 18, 20, and 25); 5 items that were modified (Items 4, 5, 9, 26, and 27); and 2 items created for purposes of this review. Reporting Items 4, 5, and 9, and internal validity (confounding) Item 26, from the original list, were reworded to align with nonintervention (i.e., cross-sectional and prospective) studies being examined in this review. Item 27, concerning power, from the original list was modified to address the number of participants needed to detect a significant association between an exposure and outcome variable. Of the 2 items created, one was an internal validity criterion and one was concerned with study power. We believe that changes made to the original checklist had merit and that modifications held value in assessing the methodological quality of studies included in this review. Each quality criterion was assigned a positive (+), negative (−), or unknown/insufficiently described (?) rating. A positive sign (+) was given if the article provided a sufficient description of the item, per the predefined criteria, and met the quality criteria for the item. A negative sign (–) was assigned if the publication did not provide an adequate description or did not address and/or perform the quality criteria for the item. Finally, if an insufficient or unclear description of the item was provided, a question mark (?) was assigned. The maximum possible score that could be achieved with the modified checklist was 19 points (all positive signs), with a higher score indicating higher quality. The methodological quality of included studies was independently scored by SR and verified by OA. If disagreements between assessors occurred, consensus was achieved through discussion with a third senior investigator (MST). In the present review, overall methodological quality scores for each individual study and the percentage of studies meeting each quality criterion were calculated. Additionally, Downs and Black score ranges were given corresponding quality levels: excellent (18–19), good (14–17), fair (10–13), or poor (≤ 9). These levels were determined using similar score percentile ranges as previously reported.32,33 Sensitivity analyses were also performed to compare the results of studies examining adherence to the 24-h movement guidelines vs. those employing compositional analyses and studies that reported significant vs. null associations. Together, methodological quality results were used to assess the overall quality level of the evidence on 24-h movement guideline adherence and the composition of 24-h movement behaviors.
3. Results
3.1. Description of studies
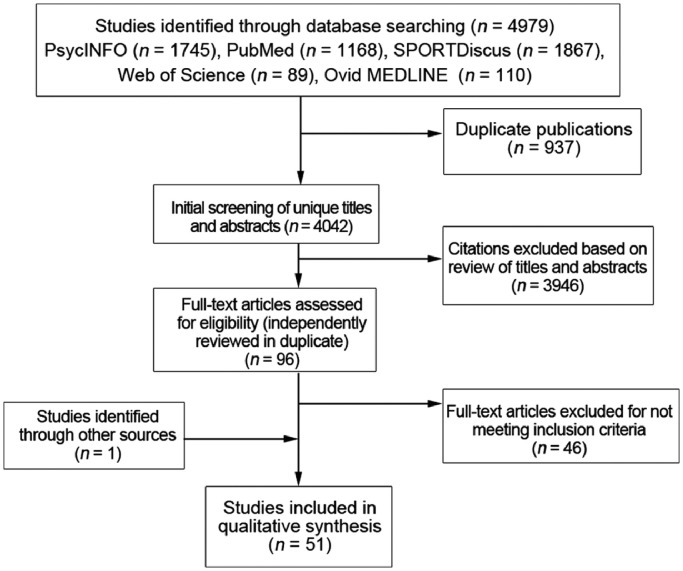
A total of 4979 records were identified through database searches (Fig. 1). After removing duplicates, 4042 records remained. After titles and abstracts were screened, 96 articles were obtained for full-text review. Of those, 50 studies met the inclusion criteria. By searching through personal databases and the reference lists of all the included articles, we identified 1 additional study relevant for this review. Therefore, a total of 51 studies published between the years 2015 and 2020 met the eligibility criteria and were included in this review (Fig. 1).16,18, 19, 20,27, 28, 29,34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for the identification, screening, eligibility, and inclusion of studies.
Of the 51 studies included in this review, 31 studies27, 28, 29,34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61 examined adherence (meeting vs. not meeting) to 24-h movement guidelines, and 20 studies16,18, 19, 20,62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77 used compositional analyses to explore the 24-h time-use composition of movement behaviors. Studies were conducted in 20 different countries but were most commonly conducted in Canada (n = 12),19,20,27, 28, 29,35,43,49,55,57,62,75 the United States (n = 10),16,40,41,44, 45, 46, 47, 48,61,72 Australia (n = 6),38,42,59,63,65,71 and the United Kingdom (n = 4),54,66,67,74 with 3 or fewer studies conducted in each other country.34,36,37,39,50, 51, 52, 53, 54,66, 67, 68, 69, 70,73,74,76,77 A total of 5 studies were multinational in nature and were conducted with participants from 4 or more different countries.18,56,58,60,64 A total of 46 studies employed a cross-sectional design, and 271,72 were prospective in nature. A total of 3 studies employed longitudinal, prospective designs, with additional cross-sectional analyses.34,53,77 Timelines for prospective studies ranged from 4 months71 to 5 years.72 In terms of age groups, 1 study42 was conducted with infants, 2 studies49,59 with toddlers, 11 studies28,34,35,37, 38, 39,46,51,53,62,77 with preschoolers, 14 studies18,36,40,48,52,56,58,60,61,64, 65, 66,75,76 with children, 4 studies45,47,50,54 with youth, 8 studies19,27,29,41,43,44,55,57 with both children and youth, 5 studies16,67, 68, 69, 70 with adults, 4 studies63,71,73,74 with older adults, and 2 studies20,72 with both adults and older adults. The sample sizes of the included studies ranged from 9374 to 59,39745 participants.
With regard to the measurement of 24-h movement behaviors, PA was measured objectively by using accelerometers in 36 studies and pedometers in 1 study; it was self-reported in 11 studies and parent-reported in 3 studies. Sedentary behavior and/or screen time were measured objectively by using accelerometers in 18 studies, were self-reported in 17 studies, and were parent-reported in 15 studies. One study included both self-reported and parent-reported SB measures because of the age of the participants. Sleep was measured objectively in 16 studies, self-reported in 18 studies, and parent-reported in 13 studies. Only 2 studies included both objective and self-reported measures of sleep; similarly, 2 studies included both self-reported and parent-reported measures because of the age of the participants. Study characteristics and results of the 51 individual studies are presented in Supplementary Tables 2 and 3.
3.2. Quality of evidence
3.2.1. Guideline-adherence studies
The modified Downs and Black checklist31 for assessment of the methodological quality of included studies examining adherence to 24-h movement guidelines, including the percentage of studies meeting each item, is presented in Table 1. The overall quality scores for each study are presented in Table 2. When the studies were evaluated, the methodological quality score of the publications ranged from 42% to 84%. The average quality score for included studies was 70%. Of the 31 studies, 3 studies37,45,54 had a score of less than 50%. A total of 12 studies41,42,44,46,48,49,51,56,57,59,60,61 had scores between 60% and 69%, 13 studies27, 28, 29,34, 35, 36,38,39,47,50,52,53,58 had scores between 70% and 79%, and 3 studies40,43,55 had scores between 80% and 89%. The average score of the included studies for the quality subscales of reporting, external validity, internal validity—bias, internal validity—confounding, and power were 88%, 32%, 79%, 74%, and 3%, respectively. Also highlighted through the assessment was the percentage of studies meeting each item on the checklist (Table 1). The majority of studies satisfied the reporting criteria (Items 1–9), with > 80% of the studies meeting each of Items 1–8. However, only 39% of the studies reported actual probability values for the main outcomes except where the probability value was less than 0.001 (Item 9). In terms of the external validity criteria, Items 10 and 11 addressed the representativeness of the findings of the study and whether they could be generalized to the population from which the study subjects were derived. Only 39% and 26% of the studies met these items, respectively. The proportion of studies meeting the quality items with respect to internal validity (Items 12–17) varied considerably per item, with only 26% of the studies measuring the exposure variables at a time prior to the assessment of outcomes (Item 13). Furthermore, only 58% of the studies scored positively on Item 17 and took losses of participants to follow-up and/or with missing data into account. For the power criteria (Items 18 and 19), 97% of the studies did not report a formal power calculation for determining the association between exposure(s) and outcome(s) variables (Item 18). Because of this, it was unknown whether the sample size used for analysis was sufficiently powered for these studies (Item 19).
Table 1.
Checklist for assessment of the methodological quality of included studies examining adherence to 24-h movement guidelines.
| Criteria checklist | Studies meeting the item (%) |
|---|---|
| Reporting | |
| 1. Is the hypothesis/aim/objective of the study clearly described? | 94 |
| 2. Are the main outcomes to be measured clearly described in the Introduction or Methods section? | 100 |
| 3. Are the characteristics of the participants included in the study clearly described? | 97 |
| 4. Is the study design clearly described (i.e., cross-sectional vs. prospective; if prospective, time of assessments)? | 97 |
| 5. When appropriate, were principal covariates clearly described? | 90 |
| 6. Are the main findings of the study clearly described? | 100 |
| 7. Does the study provide estimates of the random variability in the data for the main outcomes? | 94 |
| 8. Have the characteristics of participants lost to follow-up and/or with missing data been described? | 84 |
| 9. Have actual probability values been reported (e.g., 0.035 rather than <0.05) for the main outcomes except where the probability value is <0.001? | 39 |
| External validity | |
| 10. Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | 39 |
| 11. Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | 26 |
| Internal validity–bias | |
| 12. If any of the results of the study were based on “data dredging”, was this made clear? | 100 |
| 13. Were the exposure(s) of interest measured prior to the outcome(s) being measured? | 26 |
| 14. Were the statistical tests used to assess the main outcomes appropriate? | 100 |
| 15. Were the main exposure and outcome measures used accurate (valid and reliable)? | 90 |
| Internal validity–confounding (selection bias) | |
| 16. When appropriate, was there adequate adjustment for confounding (i.e., covariates) in the analyses from which the main findings were drawn? | 90 |
| 17. Were losses of participants to follow-up and/or with missing data taken into account? | 58 |
| Power | |
| 18. Did the study report a formal power calculation for determining the association between exposure(s) and outcome(s) variables? | 3 |
| 19. Was the sample size used for analyses reflective of the power calculation? | 3 |
Table 2.
Overall scores of the methodological quality assessment for the included studies examining adherence to 24-h movement guidelines.
| Author/Criteria (1–19) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | Sum/% |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Berglind et al. (2018)34 | + | + | + | + | + | + | + | + | ? | ? | ? | + | + | + | + | + | + | − | ? | 14/74 |
| Carson et al. (2017)27 | + | + | + | + | + | + | + | + | − | + | + | + | − | + | + | + | ? | − | ? | 14/74 |
| Carson et al. (2019)35 | + | + | + | + | + | + | + | + | + | ? | − | + | − | + | + | + | + | − | ? | 14/74 |
| Chaput et al. (2017)28 | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | ? | − | ? | 15/79 |
| Chen et al. (2019)36 | + | + | + | + | + | + | + | + | − | − | ? | + | + | + | + | + | + | − | ? | 14/74 |
| Chia et al. (2020)37 | + | + | + | + | ? | + | + | ? | − | ? | ? | + | − | + | + | ? | ? | − | ? | 9/47 |
| Cliff et al. (2017)38 | + | + | + | + | + | + | + | + | + | + | ? | + | − | + | + | + | + | − | ? | 15/79 |
| De Craemer et al. (2018)39 | + | + | + | + | + | + | ? | + | + | − | − | + | + | + | + | + | + | − | ? | 14/74 |
| Guerrero et al. (2019)40 | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | − | ? | 16/84 |
| Healy et al. (2019)41 | + | + | + | + | + | + | + | ? | − | + | ? | + | + | + | ? | + | ? | − | ? | 12/63 |
| Hesketh et al. (2017)42 | + | + | + | + | + | + | + | ? | + | ? | − | + | − | + | + | + | ? | − | ? | 12/63 |
| Janssen et al. (2017)43 | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | + | − | ? | 16/84 |
| Janssen et al. (2017)29 | + | + | + | + | + | + | + | + | − | + | + | + | − | + | + | + | ? | − | ? | 14/74 |
| Katzmarzyk & Staiano (2017)44 | + | + | + | + | + | + | + | ? | + | − | − | + | − | + | + | + | ? | − | ? | 12/63 |
| Knell et al. (2019)45 | ? | + | ? | + | + | + | + | ? | − | ? | ? | + | − | + | ? | + | ? | − | ? | 8/42 |
| Kracht et al. (2019)46 | + | + | + | + | + | + | − | + | + | − | − | + | − | + | + | + | + | − | ? | 13/68 |
| Laurson et al. (2015)47 | + | + | + | + | + | + | + | + | − | + | + | + | − | + | + | + | + | − | ? | 15/79 |
| Laurson et al. (2014)48 | + | + | + | + | + | + | + | + | − | − | − | + | − | + | + | + | ? | − | ? | 12/63 |
| Lee et al. (2017)49 | + | + | + | + | + | + | + | + | − | − | − | + | − | + | + | + | + | − | ? | 13/68 |
| Lee et al. (2018)50 | + | + | + | + | + | + | + | + | − | + | + | + | − | + | + | + | + | − | ? | 15/79 |
| Leppänen et al. (2019)51 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | ? | − | ? | 13/68 |
| Manyanga et al. (2019)52 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | + | − | ? | 14/74 |
| Meredith-Jones et al. (2019)53 | + | + | + | + | + | + | + | + | + | − | − | + | + | + | + | + | + | − | ? | 15/79 |
| Pearson et al. (2019)54 | ? | + | + | ? | ? | + | + | + | − | + | ? | + | ? | + | ? | ? | + | − | ? | 9/47 |
| Roberts et al. (2017)55 | + | + | + | + | + | + | + | + | − | + | + | + | + | + | + | + | + | − | ? | 16/84 |
| Roman-Viñas et al. (2016)56 | + | + | + | + | + | + | + | + | − | − | − | + | − | + | + | + | + | − | ? | 13/68 |
| Ronen & Janssen (2019)57 | + | + | + | + | ? | + | + | + | − | + | ? | + | + | + | + | ? | + | − | ? | 13/68 |
| Sampasa-Kanyinga et al. (2017)58 | + | + | + | + | + | + | + | + | − | − | − | + | − | + | + | + | + | + | + | 15/79 |
| Santos et al. (2017)59 | + | + | + | + | + | + | + | + | − | − | − | + | − | + | + | + | ? | − | ? | 12/63 |
| Thivel et al. (2019)60 | + | + | + | + | + | + | + | + | ? | ? | ? | + | − | + | + | + | ? | ? | ? | 12/63 |
| Walsh et al. (2018)61 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | ? | − | ? | 13/68 |
Note: Rating of criteria: “+” = yes, “−” = no, “?” = unable to determine.
3.2.2. Compositional analyses studies
The modified Downs and Black checklist31 for the methodological quality assessment of included studies examining the composition of 24-h movement behaviors, including the percentage of studies meeting each item, is presented in Table 3. The overall quality scores of each study are presented in Table 4. The methodological quality scores of these studies ranged from 58% to 84%. The average quality score for included studies was 74%. Of the 20 publications, 1 study74 had a score between 50% and 59%, 4 studies68, 69, 70,76 had scores between 60% and 69%, 11 studies16,18, 19, 20,62,64, 65, 66, 67,71,77 had scores between 70% and 79%, and 4 studies63,72,73,75 had scores between 80% and 89%. The average score of the included studies for the quality subscales of reporting, external validity, internal validity—bias, internal validity—confounding, and power were 96%, 35%, 78%, 68%, and 13%, respectively. Also highlighted through the assessment was the percentage of studies meeting each item on the checklist (Table 3). The majority of studies satisfied the reporting criteria (Items 1–9), with ≥ 85% of the studies meeting each of the items. In terms of the external validity criteria (Items 10–11), only 45% and 25% of the studies met these items, respectively. The proportion of studies meeting the quality items with respect to internal validity (Items 12–17) was high; however, only 10% of the studies measured the exposure variables at a time prior to the assessment of outcomes (Item 13). Furthermore, only 35% of the studies took losses of participants to follow-up and/or with missing data into account when presenting the findings (Item 17). For the power criteria (Items 18 and 19), 85% of the studies did not report a formal power calculation for determining the association between exposure(s) and outcome(s) variables (Item 18). Because of this, it was unknown whether the sample size used for analysis was sufficiently powered for these studies (Item 19).
Table 3.
Checklist for assessment of the methodological quality of included studies examining composition of 24-h movement behaviors.
| Criteria checklist | Studies meeting the item (%) |
|---|---|
| Reporting | |
| 1. Is the hypothesis/aim/objective of the study clearly described? | 100 |
| 2. Are the main outcomes to be measured clearly described in the Introduction or Methods section? | 100 |
| 3. Are the characteristics of the participants included in the study clearly described? | 100 |
| 4. Is the study design clearly described (i.e., cross-sectional vs. prospective; if prospective, time of assessments)? | 100 |
| 5. When appropriate, were principal covariates clearly described? | 100 |
| 6. Are the main findings of the study clearly described? | 100 |
| 7. Does the study provide estimates of the random variability in the data for the main outcomes? | 90 |
| 8. Have the characteristics of participants lost to follow-up and/or with missing data been described? | 90 |
| 9. Have actual probability values been reported (e.g., 0.035 rather than <0.05) for the main outcomes except where the probability value is <0.001? | 85 |
| External validity | |
| 10. Were the subjects asked to participate in the study representative of the entire population from which they were recruited? | 45 |
| 11. Were those subjects who were prepared to participate representative of the entire population from which they were recruited? | 25 |
| Internal validity–bias | |
| 12. If any of the results of the study were based on “data dredging”, was this made clear? | 100 |
| 13. Were the exposure(s) of interest measured prior to the outcome(s) being measured? | 10 |
| 14. Were the statistical tests used to assess the main outcomes appropriate? | 100 |
| 15. Were the main exposure and outcome measures used accurate (valid and reliable)? | 100 |
| Internal validity–confounding (selection bias) | |
| 16. When appropriate, was there adequate adjustment for confounding (i.e., covariates) in the analyses from which the main findings were drawn? | 100 |
| 17. Were losses of participants to follow-up and/or with missing data taken into account? | 35 |
| Power | |
| 18. Did the study report a formal power calculation for determining the association between exposure(s) and outcome(s) variables? | 15 |
| 19. Was the sample size used for analyses reflective of the power calculation? | 10 |
Table 4.
Overall scores of the methodological quality assessment for the included studies examining composition of 24-h movement behaviors.
| Author/Criteria (1−19) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | Sum/% |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carson et al. (2016)19 | + | + | + | + | + | + | + | + | + | + | ? | + | − | + | + | + | ? | − | ? | 14/74 |
| Carson et al. (2017)62 | + | + | + | + | + | + | + | + | + | + | ? | + | − | + | + | + | ? | − | ? | 14/74 |
| Chastin et al. (2015)16 | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | ? | − | ? | 15/79 |
| Dumuid et al. (2018)63 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | + | + | + | 16/84 |
| Dumuid et al. (2018)64 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | + | − | ? | 14/74 |
| Dumuid et al. (2018)18 | + | + | + | + | + | + | + | + | ? | − | − | + | − | + | + | + | + | + | ? | 14/74 |
| Dumuid et al. (2019)65 | + | + | + | + | + | + | + | + | + | + | − | + | − | + | + | + | ? | − | ? | 14/74 |
| Fairclough et al. (2017)66 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | + | − | ? | 14/74 |
| Foley et al. (2018)67 | + | + | + | + | + | + | + | + | ? | + | ? | + | − | + | + | + | + | − | ? | 14/74 |
| Gupta et al. (2018)68 | + | + | + | + | + | + | ? | + | + | − | − | + | − | + | + | + | ? | − | ? | 12/63 |
| Gupta et al. (2019)69 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | ? | − | ? | 13/68 |
| Gupta et al. (2019)70 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | ? | − | ? | 13/68 |
| Lewthwaite et al. (2019)71 | + | + | + | + | + | + | + | + | + | − | − | + | − | + | + | + | ? | + | + | 15/79 |
| McGregor et al. (2018)20 | + | + | + | + | + | + | ? | + | + | + | + | + | − | + | + | + | ? | − | ? | 14/74 |
| McGregor et al. (2019)72 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | ? | − | ? | 16/84 |
| Powell et al. (2019)73 | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | − | ? | 16/84 |
| Ryan et al. (2019)74 | + | + | + | + | + | + | + | ? | ? | − | − | + | − | + | + | + | ? | − | ? | 11/58 |
| Talarico & Janssen (2018)75 | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + | + | + | − | ? | 16/84 |
| Taylor et al. (2019)76 | + | + | + | + | + | + | + | ? | + | − | ? | + | − | + | + | + | ? | − | ? | 12/63 |
| Taylor et al. (2018)77 | + | + | + | + | + | + | + | + | + | ? | − | + | + | + | + | + | ? | − | ? | 14/74 |
Note: Rating of criteria: “+” = yes, “–” = no, “?” = unable to determine.
3.3. Associations between the composition of movement behaviors and health indicators
3.3.1. Adiposity
The relationships between the composition of 24-h movement behaviors and adiposity indicators were examined in 13 studies16,18, 19, 20,62,63,65,66,69,73,75, 76, 77 (Table 5). The quality of evidence ranged from fair to good across the studies. A total of 2 studies62,77 conducted with preschoolers reported cross-sectional associations between the composition of 24-h movement behaviors and BMI z-scores; however, no association was found with waist circumference.62 Furthermore, it was found that a 10% increase in sleep time was associated with a lower BMI z-score, whereas a 10% increase in time spent in SB or LPA was associated with a higher BMI z-score. The relationships between the composition of 24-h movement behaviors and adiposity indicators in children were examined in 5 studies.18,65,66,75,76 Of these, 3 studies18,65,66 reported unfavorable differences in indicators of adiposity (e.g., body fat percentage) when time was reallocated from MVPA to any other behavior, and 1 study75 found that the composition of 24-h movement behaviors was associated with BMI, waist circumference, and fat mass index. Relative to other movement behaviors, time spent in MVPA was negatively associated with obesity measures and time spent in LPA was positively associated with obesity measures, but time spent in SB and sleep were not associated with obesity measures. Last, 1 study76 found that compositional time use explained between 9% and 35% of the increased risk of obesity in children, depending on ethnicity. The relationships between the composition of 24-h movement behaviors and adiposity indicators in a sample including both children and youth were examined in 1 study.19 It was reported that the composition of movement behaviors was significantly associated with BMI z-scores and waist circumference. Relative to other movement behaviors, time spent in SB or LPA was adversely associated, and time spent in MVPA or sleep was favorably associated, with adiposity indicators. A total of 2 studies16,69 assessed the relationships between the composition of 24-h movement behaviors and adiposity indicators in adults, both of which found that the distribution of time spent in 24-h movement behaviors was significantly associated with BMI and waist circumference. In 1 study,16 the strongest favorable association was found for the proportion of time spent in MVPA, whereas unfavorable associations were found for the proportion of time spent in LPA and SB. The relationships between the composition of 24-h movement behaviors and adiposity indicators in older adults were examined in 2 studies;63,73 both studies found that the time-use composition was significantly associated with adiposity. Only 1 study63 reported the reallocation of 15 min to MVPA from any other behavior was associated with lower BMI and waist-to-hip ratio, whereas one other study73 reported reallocating 30 min from sleep, SB, or standing, to LPA was associated with significant decreases in BMI, body fat, and fat mass. The relationships between the composition of 24-h movement behaviors and adiposity indicators in a sample including adults and older adults were examined in 1 study,20 which found beneficial associations between larger proportions of MVPA relative to time in other behaviors and BMI and waist circumference among adults, but no associations were found among older adults.
Table 5.
Relationships between the 24-h movement behavior composition and health outcomes.
| Health outcome | Author (year) | Age group | Association with health outcome |
|---|---|---|---|
| Adiposity | |||
| BMI | |||
| Carson et al. (2017)62 | Preschoolers | ✓ | |
| Taylor et al. (2018)77 | Preschoolers | ✓ | |
| Fairclough et al. (2017)66 | Children | ✓ | |
| Talarico & Janssen (2018)75 | Children | ✓ | |
| Taylor et al. (2019)76 | Children | ✓ | |
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | ✓ | |
| Gupta et al. (2019)69 | Adults | ✓ | |
| Dumuid et al. (2018)63 | Older adults | ✓ | |
| Powell et al. (2019)73 | Older adults | ✓ | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Body composition | |||
| Dumuid et al. (2018)18 | Children | ✓ | |
| Dumuid et al. (2019)65 | Children | ✓ | |
| Talarico & Janssen (2018)75 | Children | ✓ | |
| Gupta et al. (2019)69 | Adults | ✓ | |
| Powell et al. (2019)73 | Older adults | ✓ | |
| Waist-to-hip ratio | Dumuid et al. (2018)63 | Older adults | ✓ |
| Waist-to-height ratio | Fairclough et al. (2017)66 | Children | ✓ |
| Waist circumference | |||
| Carson et al. (2017)62 | Preschoolers | × | |
| Talarico & Janssen (2018)75 | Children | ✓ | |
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | ✓ | |
| Gupta et al. (2019)69 | Adults | ✓ | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Cardiometabolic health | |||
| Resting heart rate | McGregor et al. (2018)20 | Adults/older adults | ✓ |
| Systolic blood pressure | |||
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | ✓ | |
| Gupta et al. (2018)68 | Adults | ✓ | |
| Gupta et al. (2019)70 | Adults | ✓ | |
| Dumuid et al. (2018)63 | Older adults | × | |
| McGregor et al. (2018)20 | Adults/older adults | × | |
| Diastolic blood pressure | |||
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | ✓ | |
| Gupta et al. (2018)68 | Adults | × | |
| Gupta et al. (2019)70 | Adults | ✓ | |
| Dumuid et al. (2018)63 | Older adults | × | |
| McGregor et al. (2018)20 | Adults/older adults | × | |
| Triglycerides | |||
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | ✓ | |
| Powell et al. (2019)73 | Older adults | ✓ | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Total cholesterol | |||
| Dumuid et al. (2018)63 | Older adults | × | |
| Powell et al. (2019)73 | Older adults | × | |
| HDL-cholesterol | |||
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | × | |
| Powell et al. (2019)73 | Older adults | × | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| LDL-cholesterol | |||
| Chastin et al. (2015)16 | Adults | × | |
| Powell et al. (2019)73 | Older adults | × | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| VLDL-cholesterol | Powell et al. (2019)73 | Older adults | × |
| C-reactive protein | |||
| Carson et al. (2016)19 | Children/youth | ✓ | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Glucose | |||
| Chastin et al. (2015)16 | Adults | ✓ | |
| Dumuid et al. (2018)63 | Older adults | × | |
| Powell et al. (2019)73 | Older adults | × | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Insulin | |||
| Carson et al. (2016)19 | Children/youth | ✓ | |
| Chastin et al. (2015)16 | Adults | ✓ | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Cardiometabolic profile | Ryan et al. (2019)74 | Older adults | ✓ |
| Fitness | |||
| Cardiorespiratory/aerobic fitness | |||
| Fairclough et al. (2017)66 | Children | ✓ | |
| Carson et al. (2016)19 | Children/youth | ✓ | |
| McGregor et al. (2018)20 | Adults/older adults | ✓ | |
| Dumuid et al. (2018)63 | Older adults | ✓ | |
| Grip strength | McGregor et al. (2018)20 | Adults/older adults | ✓ |
| Mental, social, and emotional health | |||
| Behavioral strengths and difficulties | Carson et al. (2016)19 | Children/youth | ✓ |
| Mental health | McGregor et al. (2018)20 | Adults/older adults | ✓ |
| Perceived health-related quality of life | |||
| Dumuid et al. (2018)64 | Children | ✓ | |
| Lewthwaite et al. (2019)71 | Older adults with COPD | Both ✓ and × | |
| Mortality | McGregor et al. (2019)72 | Adults/older adults | ✓ |
| Bone and skeletal health | Taylor et al. (2018)77 | Infants → Preschoolers | ✓ |
| Chronic diseases and conditions-Symptoms | Lewthwaite et al. (2019)71 | Older adults with COPD | Both ✓ and × |
Note: ✓ Statistically significant association present; × statistically significant association absent.
Abbreviations: BMI = body mass index; COPD = chronic obstructive pulmonary disease; HDL = high-density lipoprotein; LDL = low-density lipoprotein; VLDL = very low-density lipoprotein.
3.3.2. Cardiometabolic health
The relationships between the composition of 24-h movement behaviors and cardiometabolic biomarkers were examined in 8 studies16,19,20,63,68,70,73,74 (Table 5). The quality of evidence ranged from fair to good across studies. One study19 found that the composition of movement behaviors was associated with blood pressure, triglycerides, high-density lipoprotein (HDL)-cholesterol, C-reactive protein, and insulin in a sample of children and youth. Relative to other movement behaviors, LPA was positively associated, and sleep was negatively associated, with blood pressure; and MVPA was negatively associated with several cardiometabolic risk markers. The relationships between the composition of 24-h movement behaviors and cardiometabolic health were examined in adults in 3 studies16,68,70 and in older adults in 3 studies.63,73,74 Among adults, findings indicated that the daily composition of movement behaviors was significantly associated with triglycerides,16 plasma glucose,16 plasma insulin,16 and systolic16,68,70 and diastolic16,70 blood pressure. No associations were found with HDL- or low-density lipoprotein (LDL)-cholesterol.16 Among older adults, 1 study63 found the composition of movement behaviors was not associated with markers of cardiometabolic risk. Another study yielded similar findings,73 with the exception of triglycerides, which were favorably associated with standing time. A third study,74 however, found differences in the 24-h composition of movement behaviors between older adults with “healthy” and “unhealthy” cardiometabolic profiles. One study20 examined the relationships between the composition of 24-h movement behaviors and cardiometabolic biomarkers in a sample of both adults and older adults and found beneficial associations between larger proportions of MVPA relative to time in other behaviors and resting heart rate, HDL-cholesterol, triglycerides, blood glucose, and insulin levels for adults. Furthermore, more time spent in sleep relative to other movement behaviors was deleteriously associated with HDL-cholesterol, insulin, and C-reactive proteins but was beneficially associated with LDL-cholesterol.
3.3.3. Fitness
Four studies19,20,63,66 of good quality examined the relationships between the composition of 24-h movement behaviors and indicators of fitness (Table 5). Study samples included children,66 children and youth,19 adults and older adults,20 and older adults.63 Among children, replacing MVPA with any other movement behavior predicted lower cardiorespiratory fitness. Among children and youth, the composition of movement behaviors was found to be associated with aerobic fitness. Relative to other movement behaviors, time spent in SB was negatively associated, and time spent in MVPA was positively associated, with aerobic fitness. In 1 study20 that included both adults and older adults, beneficial associations were observed between larger proportions of MVPA relative to time in other behaviors and aerobic fitness, as well as between relative time spent in LPA and grip strength among adults. More time spent in sleep relative to other movement behaviors was deleteriously associated with aerobic fitness and grip strength among adults. No associations emerged among older adults. Last, 1 study63 found that reallocation of 15 min to MVPA from any of the other behaviors was beneficially associated with cardiorespiratory fitness in older adults.
3.3.4. Mental, social, and emotional health
Two studies19,20 of good quality examined the relationships between the composition of 24-h movement behaviors and indicators of mental, social, and emotional health among children and youth19 and adults and older adults20 (Table 5). In 1 study, the composition of movement behaviors was associated with behavioral strengths and difficulties in children and youth, such that LPA was positively associated, and sleep was negatively associated, with unfavorable scores. In the other study, larger proportions of MVPA were associated with better mental health in older adults.
3.3.5. Perceived health
The relationships between the composition of 24-h movement behaviors and perceived health-related quality of life were examined in 2 studies of good quality (Table 5).64,71 In an international sample of children, it was found that for children from countries with higher human development indexes, the movement behavior composition was significantly related to health-related quality of life, with MVPA relative to the remaining behaviors being positively associated with this health indicator.64 In a sample of older adults with chronic obstructive pulmonary disease, prospective associations were reported between a change in the 24-h movement behavior composition and changes in the health-related quality of life subdomain of mastery but not fatigue.71 Compositional isotemporal substitution models showed that reallocating more time to higher-intensity PA or sleep was associated with favorable changes in outcomes, whereas reallocating time to SB or LPA was associated with unfavorable changes.
3.3.6. Mortality
One study72 of good quality examined the relationship between the composition of 24-h movement behaviors and risk of mortality among adults 50–79 years old (Table 5). Results demonstrated a prospective association between the composition of 24-h movement behaviors and mortality rate after controlling for confounding effects (e.g., age, sex, state of health at outset). The association was driven primarily by time spent in MVPA relative to other movement behaviors.
3.3.7. Bone and skeletal health
One study77 of good quality examined the relationship between the composition of 24-h movement behaviors and bone and skeletal health in children from 1 through 5 years of age and found that higher levels of MVPA at 2 and 3.5 years were consistently associated with higher bone mineral content and bone mineral density at 5 years; however, no consistent relationships between other components of compositional time-use and bone health were apparent (Table 5).
3.3.8. Chronic diseases and conditions
The relationship between the composition of 24-h movement behaviors and chronic diseases and conditions was examined in 1 study71 of good quality (Table 5). In a sample of older adults with chronic obstructive pulmonary disease, prospective associations were reported between a change in the 24-h movement behavior composition and changes in symptoms, including anxiety but not breathlessness or depression. Compositional isotemporal substitution models showed that reallocating more time to higher intensity PA or sleep was associated with favorable changes in outcomes, whereas reallocating time to SB or LPA was associated with unfavorable changes.
3.3.9. Summary of evidence
In preschoolers, there was consistent evidence that the composition of 24-h movement behaviors, specifically more sleep and less SB, was associated with lower adiposity.62,77 Furthermore, there was initial prospective evidence that the composition of movement behaviors, specifically greater MVPA, was associated with greater bone and skeletal health.77
In children, there was consistent evidence for adiposity18,65,66,75,76 and preliminary evidence for health-related quality of life64 and cardiorespiratory fitness66 and that the composition of movement behaviors, specifically greater MVPA relative to other behaviors, was associated with favorable measures. For both children and youth, there was initial evidence that the composition of 24-h movement behaviors, specifically greater MVPA, more sleep, less LPA, and/or less SB relative to other behaviors, was associated with favorable indicators of adiposity and aerobic fitness, as well as cardiometabolic, social, and emotional health.19
For adults, there was consistent evidence that the daily composition of movement behaviors was associated with a number of cardiometabolic biomarkers;16,20,68,70 however, for older adults, evidence was inconsistent across studies.20,63,73,74 For both adults and older adults, there was fairly consistent evidence that the composition of 24-h movement behaviors, specifically greater time spent in MVPA and to a lesser extent LPA, and less time spent in SB, was associated with favorable indicators of adiposity.16,20,63,69,73 Furthermore, there was preliminary evidence that the composition of 24-h movement behaviors, specifically higher levels of LPA and MVPA and/or lower levels of sleep, relative to other behaviors, was associated with greater cardiorespiratory fitness.20,63 Specific to older adults, there was also initial evidence that the 24-h time-use composition, specifically higher levels of MVPA relative to other behaviors, was associated with better mental health20 and reduced risk of mortality.72
Among clinical populations, there was initial prospective evidence that the 24-h movement behavior composition was associated with symptoms of anxiety and health-related quality of life in individuals with chronic obstructive pulmonary disease, wherein greater time spent in MVPA or sleep was related to lower levels of anxiety and higher health-related quality of life.71
3.4. Associations between meeting 24-h movement guidelines and health indicators
3.4.1. Adiposity
The relationships between adherence to the 24-h movement guidelines and adiposity indicators were examined in 12 studies27, 28, 29,34,44,47, 48, 49,51,53,56,59 (Table 6). Indicators of adiposity (e.g., BMI) were measured objectively (e.g., anthropometry) or assessed subjectively (e.g., parent-reported height and weight). The quality of evidence ranged from fair to good across the studies. The relationships between adherence to 24-h movement guidelines and adiposity indicators in toddlers were examined in 2 studies.49,59 Both studies reported no associations between meeting specific and general combinations of the guideline recommendations and BMI z-scores. The relationships between adherence to 24-h movement guidelines and adiposity indicators in preschoolers were examined in 4 studies.28,34,51,53 One study34 reported that adherence to any single recommendation or any combination of recommendations at the age of 4 years was not associated with being overweight or obese or with BMI or BMI z-scores at age 4 or 5 years. In another investigation, adherence to meeting all 3 guidelines (PA, screen time, and sleep) at ages 1 and 2 years was not related to BMI z-score or body composition at age 5, either cross-sectionally or prospectively.53 One cross-sectional study28 reported no association between meeting individual or combined recommendations and adiposity (BMI z-scores and BMI status). Another cross-sectional study51 found that meeting guidelines separately for PA or sleep, or for both, was associated with lower waist circumference and that meeting guidelines for sleep or for both PA and sleep were associated with lower BMI. The relationships between adherence to 24-h movement guidelines and adiposity indicators in children were examined in 2 studies;48,56 both studies reported favorable associations between meeting all 3 recommendations and indicators of adiposity (BMI z-score and odds of obesity). One study48 reported that in comparison to meeting all 3 recommendations, meeting two, one, or none of the guidelines was associated with 2.5, 4.5, and 8.0 times increased odds of obesity, respectively. One study47 examined the relationship between adherence to 24-h movement guidelines and adiposity indicators in adolescents and reported that boys and girls not meeting any of the recommendations were 4.0 and 3.8 times more likely to being obese, respectively, compared to those meeting all 3 guideline recommendations. Finally, the relationships between adherence to 24-h movement guidelines and adiposity indicators in samples including children and youth were examined in 3 studies,27,29,44 all of which reported favorable associations between meeting all 3 recommendations and indicators of adiposity or risk of overweight/obesity.
Table 6.
Relationships between adherence to 24-h movement guidelines and health outcomes.
| Health outcome | Author (year) | Age group | Association with health outcome |
|---|---|---|---|
| Adiposity | |||
| BMI | |||
| Lee et al. (2017)49 | Toddlers | Ø | |
| Santos et al. (2017)59 | Toddlers | Ø | |
| Berglind et al. (2018)34 | Preschoolers | Ø | |
| Chaput et al. (2017)28 | Preschoolers | Ø | |
| Leppänen et al. (2019)51 | Preschoolers |  |
|
| Meredith-Jones et al. (2019)53 | Preschoolers | Ø | |
| Laurson et al. (2014)48 | Children |  |
|
| Roman-Viñas et al. (2016)56 | Children |  |
|
| Laurson et al. (2015)47 | Adolescents |  |
|
| Carson et al. (2017)27 | Children/youth |  |
|
| Janssen et al. (2017)29 | Children/youth |  |
|
| Katzmarzyk & Staiano (2017)44 | Children/youth |  |
|
| Body composition | |||
| Meredith-Jones et al. (2019)53 | Preschoolers | Ø | |
| Katzmarzyk & Staiano (2017)44 | Children/youth |  |
|
| Waist circumference | |||
| Leppänen et al. (2019)51 | Preschoolers |  |
|
| Carson et al. (2017)27 | Children/youth |  |
|
| Katzmarzyk & Staiano (2017)44 | Children/youth |  |
|
| Mental, social, and emotional health | |||
| Behavioral and emotional problems | Carson et al. (2019)35 | Preschoolers |  |
| Impulsivity | Guerrero et al. (2019)40 | Children |  |
| Psychological well-being | Lee et al. (2018)50 | Adolescents |  |
| Behavioral strengths and difficulties | Carson et al. (2017)27 | Children/youth |  |
| Emotional problems | Janssen et al. (2017)29 | Children/youth |  |
| Life satisfaction | Janssen et al. (2017)29 | Children/youth |  |
| Prosocial behavior | Janssen et al. (2017)29 | Children/youth |  |
| Cardiometabolic health | |||
| Systolic blood pressure | |||
| Carson et al. (2017)27 | Children/youth |  |
|
| Katzmarzyk & Staiano (2017)44 | Children/youth | Ø | |
| Diastolic blood pressure | |||
| Carson et al. (2017)27 | Children/youth | Ø | |
| Katzmarzyk & Staiano (2017)44 | Children/youth | Ø | |
| Triglycerides | |||
| Carson et al. (2017)27 | Children/youth |  |
|
| Katzmarzyk & Staiano (2017)44 | Children/youth |  |
|
| HDL-cholesterol | |||
| Carson et al. (2017)27 | Children/youth |  |
|
| Katzmarzyk & Staiano (2017)44 | Children/youth | Ø | |
| C-reactive protein | Carson et al. (2017)27 | Children/youth | Ø |
| Glucose | Katzmarzyk & Staiano (2017)44 | Children/youth |  |
| Insulin | Carson et al. (2017)27 | Children/youth |  |
| Cognitive development | |||
| Social-cognitive development | Cliff et al. (2017)38 | Preschoolers |  |
| Global cognition | Walsh et al. (2018)61 | Children |  |
| Perceived health-related quality of life | |||
| Chia et al. (2020)37 | Preschoolers |  |
|
| Sampasa-Kanyinga et al. (2017)58 | Children |  |
|
| Aerobic Fitness | Carson et al. (2017)27 | Children/youth |  |
| Dietary Patterns | Thivel et al. (2019)60 | Children |  |
Note:  Favorable association that was statistically significant; Ø null (nonsignificant) association. Abbreviations: BMI = body mass index; HDL = high-density lipoprotein.
Favorable association that was statistically significant; Ø null (nonsignificant) association. Abbreviations: BMI = body mass index; HDL = high-density lipoprotein.
3.4.2. Mental, social, and emotional health
The relationships between adherence to the 24-h movement guidelines and indicators of mental, social, and emotional health were examined in 5 studies27,29,35,40,50 of good quality (Table 6). One study35 examined the relationship between meeting the 24-h movement guidelines and behavioral and emotional problems in preschoolers and found that meeting more recommendations was associated with lower scores for total, externalizing, and internalizing problems. One study40 assessed the relationship between meeting the 24-h movement guidelines and dimensions of impulsivity in children and reported that adherence to all 3 recommendations was associated with lower positive urgency, negative urgency, and behavioral inhibition system scores, greater perseverance scores, and better scores on delay-discounting. One study50 examined the relationship between adherence to the 24-h movement guidelines and psychological well-being (happiness and stress) in adolescents and found that meeting all 3 recommendations was significantly associated with being happy and not feeling stressed. Furthermore, when the general combination of movement behaviors was considered, meeting more recommendations, compared to none, was significantly and incrementally associated with being happy. The relationships between adherence to 24-h movement guidelines and mental, social, and emotional health indicators in samples including children and youth were examined in 2 studies.27,29 Findings indicated that meeting all 3 recommendations was associated with better behavioral strengths and difficulties scores,27 lower emotional problem scores,29 and higher life satisfaction and prosocial behavior scores.29
3.4.3. Cardiometabolic health
Two studies27,44 examined the relationships between adherence to the 24-h movement guidelines and cardiometabolic biomarkers, both of which were conducted in a sample of children and youth (Table 6). The quality of evidence was fair in 1 study44 and good in another.27 Cardiometabolic health biomarkers included blood pressure, triglycerides, HDL-cholesterol, C-reactive protein, glucose, and insulin. Findings indicated that meeting all 3 recommendations was associated with lower insulin,27 lower triglyceride,27,44 and lower glucose levels.44 One study27 found favorable associations with blood pressure and HDL-cholesterol; however, the other study44 found no associations.
3.4.4. Cognitive development
The relationships between adherence to the 24-h movement guidelines and cognitive development were examined in 2 studies38,61 (Table 6). The quality of evidence was fair in 1 study61 and good in another.38 One study38 assessed the relationship between adherence to the 24-h movement guidelines and social-cognitive development in preschoolers and reported that meeting all 3 recommendations was associated with better performance on social cognition assessments. One study61 examined the relationship between adherence to the 24-h movement guidelines and global cognition in children and found that each additional recommendation met, as well as meeting all 3 recommendations, was positively associated with global cognition.
3.4.5. Perceived health
Two studies37,58 examined the relationships, in preschoolers37 and children,58 between adherence to the 24-h movement guidelines and perceived health-related quality of life (Table 6). The quality of evidence was poor in 1 study37 and good in another.58 Both studies reported that meeting all 3 24-h movement-guideline recommendations was associated with significantly better health-related quality of life when compared to meeting none of the recommendations. Interestingly, between-country differences were found for relationships between health-related quality of life and 24-h movement guidelines adherence among children.
3.4.6. Aerobic fitness
One study27 of good quality examined the relationship between adherence to the 24-h movement guidelines and fitness in children and youth and found that individuals who met all 3 recommendations had higher aerobic fitness than those meeting none, 1, and 2 recommendations (Table 6).
3.4.7. Dietary patterns
The relationships between adherence to the 24-h movement guidelines and dietary patterns were examined in 1 study60 of fair quality (Table 6). In a sample of children, it was found that a healthier dietary pattern was observed when more movement behavior recommendations were met.
3.4.8. Summary of evidence
Among toddlers, findings indicated that there is currently no evidence to support the claim that meeting the integrated guidelines is associated with lower adiposity.49,59 Among preschoolers, there was preliminary evidence that those who met the 24-h movement guidelines demonstrated better health-related quality of life,37 better social-cognitive development,38 and fewer behavioral and emotional problems.35 However, there was inconsistent evidence across studies as to whether meeting the 24-h movement guidelines was associated with favorable adiposity outcomes.28,34,51,53 For children and youth, there was consistent evidence that those who adhered to all three 24-h movement guidelines had lower adiposity and likelihood of obesity27,29,44,47,48,56 as well as favorable indicators for mental, social, and emotional health (e.g., impulsivity, psychological well-being, prosocial behavior).27,29,40,50 Meeting the integrated guidelines was also associated with higher aerobic fitness27 and favorable cardiometabolic health.27,44 Specific to children, there was preliminary evidence that those who met the guideline recommendations reported better global cognition,61 better health-related quality of life,58 and healthier dietary patterns.60
3.5. Compliance with 24-h movement guidelines
A total of 31 studies27, 28, 29,34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61 examined the proportion of individuals meeting specific (e.g., screen time only) and general combinations (e.g., all 3) of the 24-h movement guideline recommendations. A total of 12 studies28,34,35,37, 38, 39,42,46,49,51,53,59 examined the proportion of infants, toddlers, and preschoolers who met the 24-Hour Movement Guidelines for the Early Years (0–4 years old) and different recommendations within the guidelines. Only 1 study42 examined the prevalence of infants meeting the 24-h movement guidelines. It found that only 3.5% of infants met the combined guidelines (i.e., tummy time, time restrained, screen time, and sleep); furthermore, a significantly higher proportion of girls (5.7%) than boys (1.6%) met the combined guidelines. Two studies49,59 assessed compliance with the new 24-h movement guidelines in a sample of toddlers and found that only 8.9%–11.9% met the overall guidelines. Among preschool-aged children, the proportion that met all 3 recommendations ranged 5%–24% across 9 studies.28,34,35,37, 38, 39,46,51,53
A total of 19 studies27,29,36,40,41,43, 44, 45,47,48,50,52,54, 55, 56, 57, 58,60,61 examined the proportion of children and/or youth who met the 24-Hour Movement Guidelines for Children and Youth (5–17 years old), individually and in combination. Eight studies36,40,48,52,56,58,60,61 examined the prevalence of children meeting the 24-h movement guidelines, and the proportion that met all 3 recommendations ranged 4.8%–10.8%. Four studies45,47,50,54 examined the prevalence of youth meeting the 24-h movement guidelines, and the proportion that met all 3 recommendations ranged 1.6%–9.7%. Seven studies27,29,41,43,44,55,57 assessed compliance with the 24-h movement guidelines in a sample of children and youth, and the proportion that met all 3 recommendations ranged 2.6%–7.5%. Two studies found that children and youth with epilepsy57 and autism spectrum disorder41 showed lower adherence to the guidelines than their typically developing peers.
Because the first 24-h movement guidelines for adults and older adults will be released by Canada only in October of 2020, no studies were found that examined the proportion of adults or older adults meeting 24-h guidelines.
3.6. Correlates of meeting 24-h movement guidelines
Six studies36,42,45,46,52,54 examined correlates associated with adherence to the 24-h movement guidelines. Correlates examined included sociodemographic, lifestyle, and environmental factors, as well as infant, maternal, and family characteristics. Study samples included infants,42 preschoolers,46 children,36,52 and adolescents.45,54 Sex,42,45 age,45 race/ethnicity,45,46 poverty level,46 geographic location of school (urban vs. rural),52 BMI/obesity,45,54 outdoor time,52 marijuana use,45 alcohol use,45 and depressive symptoms,45,54 as well as parental education,52 maternal activity and television viewing,36 and household income,54 emerged as significant correlates of meeting the 24-h movement guidelines. One study67 found a significant relationship between the time-use composition of 24-h movement behaviors and active travel among individuals ≥ 16 years old, with those undertaking some active travel reporting more time spent in leisure MVPA and less time spent in leisure screen time and sleep than those reporting no active travel.
4. Discussion
This is the first review that has comprehensively examined the associations between the composition of 24-h movement behaviors, or adherence to 24-h movement guidelines, and multiple health indicators across all age groups. The number of studies using compositional analyses and/or assessing compliance with the 24-h movement guidelines to examine relationships with health is rapidly increasing. The most commonly studied health indicators in relation to 24-h time-use composition or 24-h movement guideline adherence were measures of adiposity, cardiometabolic, mental, social, and emotional health.
Compositional analyses have been recommended for properly analyzing movement behaviors (including PA, SB, and sleep) that together are constrained to, and fill, the 24-h period.16 Because none of the 24-h movement behaviors are independent of each other, and each of these behaviors has reciprocal effects on the others,20 it has been suggested that it is inappropriate to examine their associations with health in isolation. Compositional data-analysis techniques allow for overall 24-h time use among different movement behaviors to be considered. Compositional approaches address multicollinearity issues between movement variables, ensure that estimates are fully adjusted for all time use, and allow for the examination of combined and synergistic associations of the 24-h movement behaviors with health indicators.16 The findings of this review represent the current evidence concerning relationships between the daily composition of movement behaviors and health indicators.
Together, these findings suggest that the movement-behavior composition of the whole day is important for several indicators of health at all ages. The current evidence confirms that while MVPA remains a strong correlate of health indicators when the full 24-h movement behavior spectrum is considered, time spent in SB, sleep, and LPA may also have concomitant effects on health. These findings are consistent with the existing literature. For instance, in a review of 56 isotemporal substitution studies, Grgic and colleagues14 found that reallocations of time among MVPA, LPA, SB, and sleep were associated with a number of health outcomes; however, the strongest associations were observed when time was reallocated from SB to MVPA.
The development and release of evidence-informed 24-h movement guidelines by several countries21, 22, 23, 24, 25, 26 represents a new public health approach by providing specific recommendations for a healthy 24-h period, including time spent in PA, SB, sleep, and various trade-offs. These guidelines recognize that focusing on a single behavior has limitations and suggest that a combination of movement/nonmovement behaviors (PA, SB, and sleep) matters for health and healthy development. Our review of studies employing compositional data analysis techniques reaffirms this approach, across the lifespan. We extend these findings by examining whether adherence to these guidelines is associated with desirable health indicators.
Our findings highlight the potential health benefits of meeting the 24-h movement guidelines for the early years, as well as for children and youth. Currently, a larger and more consistent body of evidence exists surrounding the health associations of meeting the guidelines among children and youth, for whom disparities in health indicators are more evident. Our findings corroborate those of previous literature, which demonstrate the benefits of high PA, low screen time, and sufficient sleep, both separately and in combinations, for pediatric health.1,3,5,12 It is clear from the evidence that children and youth who meet the benchmarks for PA, screen time, and sleep recommended within the 24-h movement guidelines generally report better overall health than those who do not meet the benchmarks. The relationships between 24-h movement guideline adherence and a wide range of health indicators have been less studied for children who are in their early years. Furthermore, the current findings indicate primarily that meeting the 24-h movement guidelines does not appear to be associated with favorable adiposity outcomes among toddlers and preschoolers. Previous literature has also reported inconsistent findings as to whether PA, SB, screen time, and sleep, as well as specific combinations of these behaviors, are associated with adiposity, wherein the majority of observational studies have indicated null associations.2,4,6,11 The lack of evidence may be partly explained by the fact that these age groups are predominantly healthy and there is less of a differential on any given indicator for an association to arise. While the 24-h movement guidelines provide evidence-based benchmarks for the recommended time spent in PA, SB, and sleep, it is possible that more stringent thresholds are required to influence physical health indicators positively (e.g., adiposity) in the early years. It is also possible that comparing those meeting vs. not meeting the guidelines may lack the sensitivity required to detect associations between 24-h movement behaviors and health indicators, especially if the behavioral or health measures were not robust. Nonetheless, the potential relationships that may exist between meeting the 24-h movement guidelines and health indicators in the early years has only recently gained attention; hence, further investigation is warranted to ascertain whether compliance with these guideline recommendations is favorably associated with adiposity and several other health indicators in children during their early years.
Current evidence on the proportion of individuals who meet the 24-h movement guidelines suggest that adherence to the recommendations, in their entirety, is low. Moreover, the findings suggest that numerous sociodemographic, lifestyle, and environmental factors, as well as maternal and family characteristics, may be associated with guideline adherence. Among Australian infants, significant relationships between sex and compliance with the 24-h movement guidelines emerged, wherein a significantly higher proportion of girls (5.7%) than boys (1.6%) met the combined guidelines.42 For a sample of preschoolers in the United States, guidelines adherence varied by race and poverty level, wherein African American children and children who lived at or below the poverty level were less likely to meet all 3 guideline recommendations.46 Among children, greater maternal activity and less television viewing were associated with meeting all three 24-h movement guidelines in a sample of Singaporean children,36 while higher parental education and greater outdoor time were associated with meeting the 24-h guidelines in school children in Mozambique.52 Geographic location of the school was also associated with guideline adherence, in that more rural than urban children met the 24-h movement guidelines.52 In 2 large samples of adolescents from the United States and the United Kingdom, it was shown that Caucasian adolescents, younger adolescents (14 years and younger),45 boys,45 and those with a higher household income54 were more likely to meet all 3 guideline recommendations, whereas overweight and obese individuals,45,54 those with depressive symptoms,45,54 and those who reported marijuana and alcohol use45 were less likely to meet all 3 guidelines.
Based on the low levels of the population meeting the guidelines, it is clear that awareness, knowledge, and adoption of these guidelines by the general public needs to be improved. For instance, it has been found that the majority of parents have positive intentions to support child and youth health behaviors, yet many fail to enact this support.78 In the study, translation of intention into action was associated with attitudinal aspects, control over support, self-regulation skills, and parental habits and identity.78 The evidence provided in our study should alert health care professionals, researchers, educators, decision makers, advocacy groups, organizations, and parents to the low levels of adherence to the 24-h movement guideline recommendations and potential effects on health among children and youth. Latimer-Cheung et al.79 discussed the implications of these guidelines for professionals, practitioners, and organizations in PA, physical education, fitness, wellness, public health, and related fields, as well as potential strategies for dissemination and implementation. Several dissemination resources have been developed (e.g., scientific statements, Website content, promotional material); however, there is a need for novel and innovative dissemination and implementation strategies and activities, including effective social media and marketing efforts, educational initiatives, professional development and training, curriculum redesign, new programming, restructuring of the environment, policy change, advocacy resources, guideline endorsement, digital applications, and interprofessional collaboration. Our findings should encourage researchers and granting agencies to establish, fund, and implement interventions and public health promotion campaigns designed to improve awareness of, and adherence to, these guidelines in order to improve the health and well-being of our future generations. On-going surveillance of the proportion of the population meeting these targets and investigating associations between 24-h movement behaviors and health indicators are important in supporting efforts for guideline adoption and monitoring trends. Collectively, our findings support the importance of a healthy composition of PA, SB, and sleep and subsequently meeting the recommended 24-h movement behavior guidelines for disease prevention and health promotion across the lifespan.
4.1. Strengths and limitations
Based on the Downs and Black checklist31 for assessment of the methodological quality, the findings from the studies included in this systematic review come from reasonably high-quality studies (Table 1, Table 2, Table 3, Table 4). For instance, 31 of the 51 reported studies had overall quality scores ≥ 70%, and 47 of the 51 studies had overall quality scores ≥ 60%. We found slight differences between the average quality scores of studies examining adherence to 24-h movement guidelines (mean (M) = 70%) and those employing compositional analyses (M = 74%). Furthermore, studies that demonstrated an association between 24-h movement guideline adherence or the composition of 24-h movement behaviors and health indicators (n = 33; M = 73%) were of a quality similar to those studies that found no association between these constructs (n = 14; M = 74%). The 2 major weaknesses of the included studies were that only 8% of them employed prospective designs and measured the exposure variables prior to the assessment of health indicators, and only 8% reported a formal power calculation to inform their sample size. Because the majority of studies were cross-sectional, any causal inference is limited, and there may be several possible explanations for the estimated associations. Although the majority of studies accounted for potential covariates (e.g., socioeconomic factors), it is possible that the associations observed may be attributable to other factors (e.g., diet, health-compromising behaviors). Only studies published in English were considered, so ascertainment bias was possible. Furthermore, measures used to assess meeting the recommendations varied significantly across studies, so their respective validity and comparability cannot be assured. This calls for efforts to standardize, or at least harmonize, surveillance measures.
4.2. Areas for future research
A number of future research recommendations should be considered. Good-quality longitudinal and intervention studies are needed to examine a wide range of health indicators that are potentially associated with the composition of 24-h movement behaviors and adherence to the 24-h movement guidelines. It is important that future investigations utilize valid and reliable measures that are appropriate for the targeted age group. There is a need for the development of self-report instruments measuring screen time that accurately capture time spent on different screen-based devices across various platforms and activities.
With the exception of adiposity in children and youth, the evidence for most health indicators is limited by the number of studies across age groups, as well as variation in samples, instruments utilized, and specific indicator examined. These studies need to be replicated to confirm health associations with adherence to the 24-h movement guidelines and the 24-h movement behavior composition. The relationships between 24-h movement behaviors or guideline adherence and several health indicators have yet to be examined in specific age groups and populations. There is a need for additional research that examines the following:
-
•
Potential moderating effects of sex, age, race/ethnicity, socioeconomic status, and weight status on associations between the 24-h time-use composition of movement behaviors and adherence to the integrated guidelines and health indicators
-
•
Physical behaviors (e.g., active play, organized sport, physical education), individual characteristics (e.g., physical literacy, physical fitness), and government strategies and policies that may influence individuals’ daily composition of movement behaviors and subsequent adherence to the 24-h movement guideline recommendations
-
•
Household/family (e.g., parent-child dyads), school, and community and environment influences on 24-h time-use and guideline adherence
-
•
Spatial variation and temporal trends in the proportion of individuals meeting the 24-h movement guidelines
-
•
International and cross-cultural comparisons of the 24-h time-use distribution of movement behaviors and 24-h movement guideline compliance rates
-
•
24-h time-use composition and guideline adherence among clinical and at-risk populations.
The evidence to date suggests that adherence to the 24-h movement guidelines is poor in the early years and among children and youth; hence, implementation strategies and dissemination approaches to encourage uptake and adoption among stakeholders and the general public need to be encouraged and evaluated. Large-scale interventions and public health promotion efforts to encourage a healthy composition of daily movement behaviors and enhance compliance with the 24-h movement guidelines are necessary.
Upon the release of the Canadian 24-Hour Movement Guidelines for Adults and Older Adults in October 2020, investigations that are similar to those completed for children in their early years and for children and youth will need to be conducted in order to examine guideline adherence, correlates, and health associations among adult and older adult populations in Canada and abroad.
5. Conclusion
The findings from this review, based on moderate-quality evidence, indicate that the composition of movement behaviors within a 24-h period may have important implications for health at all ages and that meeting the current 24-h movement guidelines is associated with a number of desirable health indicators in children and youth. In summary, our findings demonstrate that school-aged children and youth who meet all of the 24-h movement guideline recommendations generally have more favorable measures of adiposity; mental, social, emotional, and cardiometabolic health; fitness; perceived health; and cognitive development and have healthier dietary patterns than those who do not meet the recommendations. Currently, evidence for toddlers and preschoolers is limited and equivocal. The evidence suggests that the time-use composition of PA, SB, and sleep during a 24-h period is associated with indicators of adiposity at all ages, as well as a number of other health indicators among specific age groups. Because the majority of studies were cross-sectional in design, there is a need for additional high-quality investigations employing longitudinal and experimental study designs using valid and reliable movement behavior (PA, SB, and sleep) measures and examining a wide array of health indicators across all age groups. Such studies would confirm the primarily cross-sectional evidence and further advance our understanding of the relationships among 24-h movement behaviors and health.
Authors’ contributions
SR was responsible for the initiation, conceptualization, and design of the systematic review, article screening process, data collection and extraction, risk of bias assessment, and analysis and interpretation of data, as well as being the primary author of the manuscript; OA contributed to data collection and extraction and the risk-of-bias assessment; MST contributed to the initiation, conceptualization, and design of the systematic review, as well as interpretation of data. All authors contributed to the manuscript writing and were responsible for revising the manuscript critically for important intellectual content. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2020.07.004.
Appendix. Supplementary materials
References
- 1.Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput JP. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: an update. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S240–S265. doi: 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- 2.Carson V, Lee EY, Hewitt L, Jennings C, Hunter S, Kuzik N. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(Suppl. 5):854. doi: 10.1186/s12889-017-4860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S266–S282. doi: 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- 4.Chaput JP, Gray CE, Poitras VJ, Carson V, Gruber R, Birken CS. Systematic review of the relationships between sleep duration and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(Suppl 5):855. doi: 10.1186/s12889-017-4850-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poitras VJ, Gray CE, Borghese MM, Carson V, Chaput JP, Janssen I. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S197–S239. doi: 10.1139/apnm-2015-0663. [DOI] [PubMed] [Google Scholar]
- 6.Poitras VJ, Gray CE, Janssen X, Aubert S, Carson V, Faulkner G. Systematic review of the relationships between sedentary behaviour and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(Suppl. 5):868. doi: 10.1186/s12889-017-4849-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katzmarzyk PT, Powell KE, Jakicic JM, Troiano RP, Piercy K, Tennant B. Sedentary behavior and health: update from the 2018 Physical Activity Guidelines Advisory Committee. Med Sci Sports Exerc. 2019;51:1227–1241. doi: 10.1249/MSS.0000000000001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med Sci Sports Exerc. 2019;51:1270–1281. doi: 10.1249/MSS.0000000000001939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin J, Jin X, Shan Z, Li S, Huang H, Li P. Relationship of sleep duration with all‐cause mortality and cardiovascular events: a systematic review and dose‐response meta‐analysis of prospective cohort studies. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.005947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ž Pedišić. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research—the focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology. 2014;46:135–146. [Google Scholar]
- 11.Kuzik N, Poitras VJ, Tremblay MS, Lee EY, Hunter S, Carson V. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(Suppl. 5):849. doi: 10.1186/s12889-017-4851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saunders TJ, Gray CE, Poitras VJ, Chaput JP, Janssen I, Katzmarzyk PT. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S283–S293. doi: 10.1139/apnm-2015-0626. [DOI] [PubMed] [Google Scholar]
- 13.Mekary RA, Willett WC, Hu FB, Ding EL. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol. 2009;170:519–527. doi: 10.1093/aje/kwp163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grgic J, Dumuid D, Bengoechea EG, Shrestha N, Bauman A, Olds T. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: a systematic scoping review of isotemporal substitution studies. Int J Behav Nutr Phys Act. 2018;15:69. doi: 10.1186/s12966-018-0691-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colley RC, Michaud I, Garriguet D. Reallocating time between sleep, sedentary and active behaviours: associations with obesity and health in Canadian adults. Health Rep. 2018;29:3–13. [PubMed] [Google Scholar]
- 16.Chastin SFM, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: a novel compositional data analysis approach. PloS One. 2015;10 doi: 10.1371/journal.pone.0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aitchison J. The statistical analysis of compositional data. J R Stat Soc Series B Stat Methodol. 1982;44:139–160. [Google Scholar]
- 18.Dumuid D, Stanford TE, Pedišić Ž, Maher C, Lewis LK, Martín-Fernández JA. Adiposity and the isotemporal substitution of physical activity, sedentary time and sleep among school-aged children: a compositional data analysis approach. BMC Public Health. 2018;18:311. doi: 10.1186/s12889-018-5207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carson V, Tremblay MS, Chaput JP, Chastin SFM. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S294–S302. doi: 10.1139/apnm-2016-0026. [DOI] [PubMed] [Google Scholar]
- 20.McGregor DE, Carson V, Palarea-Albaladejo J, Dall PM, Tremblay MS, Chastin SFM. Compositional analysis of the associations between 24-h movement behaviours and health indicators among adults and older adults from the Canadian health measure survey. Int J Environ Res Public Health. 2018;15:1779. doi: 10.3390/ijerph15081779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S311–S327. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- 22.Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17(Suppl.5):874. doi: 10.1186/s12889-017-4859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okely AD, Ghersi D, Hesketh KD, Santos R, Loughran SP, Cliff DP. A collaborative approach to adopting/adapting guidelines: the Australian 24-hour movement guidelines for the early years (birth to 5 years): an integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17(Suppl. 5):869. doi: 10.1186/s12889-017-4867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ministry of Health, Wellington, New Zealand. Sit less, move more, sleep well: active play guidelines for under-fives. Available at: https://www.health.govt.nz/publication/sit-less-move-more-sleep-well-active-play-guidelines-under-fives. [accessed 08.04.2020].
- 25.Draper CE, Tomaz SA, Biersteker L, Cook CJ, Couper J, de Milander M. The South African 24-hour movement guidelines for birth to 5 years: an integration of physical activity, sitting behaviour, screen time and sleep. J Phys Act Health. 2020;17:109–119. doi: 10.1123/jpah.2019-0187. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. WHO guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Available at: https://www.who.int/publications-detail/guidelines-on-physical-activity-sedentary-behaviour-and-sleep-for-children-under-5-years-of-age. [accessed 08.04.2020]. [PubMed]
- 27.Carson V, Chaput JP, Janssen I, Tremblay MS. Health associations with meeting new 24-hour movement guidelines for Canadian children and youth. Prev Med. 2017;95:7–13. doi: 10.1016/j.ypmed.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Chaput JP, Colley RC, Aubert S, Carson V, Janssen I, Roberts KC. Proportion of preschool-aged children meeting the Canadian 24-hour movement guidelines and associations with adiposity: results from the Canadian Health Measures Survey. BMC Public Health. 2017;17(Suppl. 5):829. doi: 10.1186/s12889-017-4854-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Janssen I, Roberts KC, Thompson W. Is adherence to the Canadian 24-hour movement behaviour guidelines for children and youth associated with improved indicators of physical, mental, and social health. Appl Physiol Nutr Metab. 2017;42:725–731. doi: 10.1139/apnm-2016-0681. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hooper P, Jutai JW, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol. 2008;43:180–187. doi: 10.3129/i08-001. [DOI] [PubMed] [Google Scholar]
- 33.Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction. Br J Sports Med. 2018;52:387–407. doi: 10.1136/bjsports-2016-097347. [DOI] [PubMed] [Google Scholar]
- 34.Berglind D, Ljung R, Tynelius P, Brooke HL. Cross-sectional and prospective associations of meeting 24-h movement guidelines with overweight and obesity in preschool children. Pediatr Obes. 2018;13:442–449. doi: 10.1111/ijpo.12265. [DOI] [PubMed] [Google Scholar]
- 35.Carson V, Ezeugwu VE, Tamana SK, Chikuma J, Lefebvre DL, Azad MB. Associations between meeting the Canadian 24-hour movement guidelines for the early years and behavioral and emotional problems among 3-year-olds. J Sci Med Sport. 2019;22:797–802. doi: 10.1016/j.jsams.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 36.Chen B, Bernard JY, Padmapriya N, Yao J, Goh C, Tan KH. Socio-demographic and maternal predictors of adherence to 24-hour movement guidelines in Singaporean children. Int J Behav Nutr Phys Act. 2019;16:70. doi: 10.1186/s12966-019-0834-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chia MYH, Tay LY, Chua TBK. Quality of life and meeting 24-h WHO guidelines among preschool children in Singapore. Early Child Educ J. 2020;48:313–323. [Google Scholar]
- 38.Cliff DP, McNeill J, Vella SA, Howard SJ, Santos R, Batterham M. Adherence to 24-hour movement guidelines for the early years and associations with social-cognitive development among Australian preschool children. BMC Public Health. 2017;17(Suppl. 5):857. doi: 10.1186/s12889-017-4858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Craemer M, McGregor D, Androutsos O, Manios Y, Cardon G. Compliance with 24-h movement behaviour guidelines among Belgian pre-school children: the ToyBox-Study. Int J Environ Res Public Health. 2018;15:2171. doi: 10.3390/ijerph15102171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guerrero MD, Barnes JD, Walsh JJ, Chaput JP, Tremblay MS, Goldfield GS. 24-hour movement behaviors and impulsivity. Pediatrics. 2019;144 doi: 10.1542/peds.2019-0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Healy S, Aigner CJ, Haegele JA, Patterson F. Meeting the 24-hr movement guidelines: an update on US youth with autism spectrum disorder from the 2016 National Survey of Children's Health. Autism Res. 2019;12:941–951. doi: 10.1002/aur.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hesketh KD, Downing KL, Campbell K, Crawford D, Salmon J, Hnatiuk JA. Proportion of infants meeting the Australian 24-hour movement guidelines for the early years: data from the Melbourne InFANT Program. BMC Public Health. 2017;17(Suppl. 5):856. doi: 10.1186/s12889-017-4856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Janssen I, Roberts KC, Thompson W. Adherence to the 24-hour movement guidelines among 10- to 17-year-old Canadians. Health Promot Chronic Dis Prev Can. 2017;37:369–375. doi: 10.24095/hpcdp.37.11.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katzmarzyk PT, Staiano AE. Relationship between meeting 24-hour movement guidelines and cardiometabolic risk factors in children. J Phys Act Health. 2017;14:779–784. doi: 10.1123/jpah.2017-0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Knell G, Durand CP, Kohl 3rd HW, Wu IHC, Gabriel KP. Prevalence and likelihood of meeting sleep, physical activity, and screen-time guidelines among US youth. JAMA Pediatr. 2019;173:387–389. doi: 10.1001/jamapediatrics.2018.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kracht CL, Webster EK, Staiano AE. Sociodemographic differences in young children meeting 24-hour movement guidelines. J Phys Act Health. 2019;16:908–915. doi: 10.1123/jpah.2019-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Laurson KR, Lee JA, Eisenmann JC. The cumulative impact of physical activity, sleep duration, and television time on adolescent obesity: 2011 Youth Risk Behavior Survey. J Phys Act Health. 2015;12:355–360. doi: 10.1123/jpah.2013-0402. [DOI] [PubMed] [Google Scholar]
- 48.Laurson KR, Lee JA, Gentile DA, Walsh DA, Eisenmann JC. Concurrent associations between physical activity, screen time, and sleep duration with childhood obesity. ISRN Obes. 2014;2014 doi: 10.1155/2014/204540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee EY, Hesketh KD, Hunter S, Kuzik N, Rhodes RE, Rinaldi CM. Meeting new Canadian 24-hour movement guidelines for the early years and associations with adiposity among toddlers living in Edmonton, Canada. BMC Public Health. 2017;17(Suppl.5):840. doi: 10.1186/s12889-017-4855-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee EY, Spence JC, Tremblay MS, Carson V. Meeting 24-hour movement guidelines for children and youth and associations with psychological well-being among South Korean adolescents. Ment Health Phys Act. 2018;14:66–73. [Google Scholar]
- 51.Leppänen MH, Ray C, Wennman H, Alexandrou C, Sääksjärvi K, Koivusilta L. Compliance with the 24-h movement guidelines and the relationship with anthropometry in Finnish preschoolers: the DAGIS study. BMC Public Health. 2019;19:1618. doi: 10.1186/s12889-019-7967-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Manyanga T, Barnes JD, Chaput JP, Katzmarzyk PT, Prista A, Tremblay MS. Prevalence and correlates of adherence to movement guidelines among urban and rural children in Mozambique: a cross-sectional study. Int J Behav Nutr Phys Act. 2019;16:94. doi: 10.1186/s12966-019-0861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meredith-Jones K, Galland B, Haszard J, Gray A, Sayers R, Hanna M. Do young children consistently meet 24-h sleep and activity guidelines? a longitudinal analysis using actigraphy. Int J Obes (Lond) 2019;43:2555–2564. doi: 10.1038/s41366-019-0432-y. [DOI] [PubMed] [Google Scholar]
- 54.Pearson N, Sherar LB, Hamer M. Prevalence and correlates of meeting sleep, screen-time, and physical activity guidelines among adolescents in the United Kingdom. JAMA Pediatr. 2019;173:993–994. doi: 10.1001/jamapediatrics.2019.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Roberts KC, Yao X, Carson V, Chaput JP, Janssen I, Tremblay MS. Meeting the Canadian 24-hour movement guidelines for children and youth. Health Rep. 2017;28:3–7. [PubMed] [Google Scholar]
- 56.Roman-Viñas B, Chaput JP, Katzmarzyk PT, Fogelholm M, Lambert EV, Maher C. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phys Act. 2016;13:123. doi: 10.1186/s12966-016-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ronen GM, Janssen I. Patterns of daily activity among young people with epilepsy. Dev Med Child Neurol. 2019;61:1386–1391. doi: 10.1111/dmcn.14223. [DOI] [PubMed] [Google Scholar]
- 58.Sampasa-Kanyinga H, Standage M, Tremblay MS, Katzmarzyk PT, Hu G, Kuriyan R. Associations between meeting combinations of 24-h movement guidelines and health-related quality of life in children from 12 countries. Public Health. 2017;153:16–24. doi: 10.1016/j.puhe.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 59.Santos R, Zhang Z, Pereira JR, Sousa-Sá E, Cliff DP, Okely AD. Compliance with the Australian 24-hour movement guidelines for the early years: associations with weight status. BMC Public Health. 2017;17(Suppl. 5):867. doi: 10.1186/s12889-017-4857-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thivel D, Tremblay MS, Katzmarzyk PT, Fogelholm M, Hu G, Maher C. Associations between meeting combinations of 24-hour movement recommendations and dietary patterns of children: a 12-country study. Prev Med. 2019;118:159–165. doi: 10.1016/j.ypmed.2018.10.025. [DOI] [PubMed] [Google Scholar]
- 61.Walsh JJ, Barnes JD, Cameron JD, Goldfield GS, Chaput JP, Gunnell KE. Associations between 24 hour movement behaviours and global cognition in US children: a cross-sectional observational study. Lancet Child Adolesc Health. 2018;2:783–791. doi: 10.1016/S2352-4642(18)30278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Carson V, Tremblay MS, Chastin SFM. Cross-sectional associations between sleep duration, sedentary time, physical activity, and adiposity indicators among Canadian preschool-aged children using compositional analyses. BMC Public Health. 2017;17(Suppl.5):848. doi: 10.1186/s12889-017-4852-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dumuid D, Lewis LK, Olds TS, Maher C, Bondarenko C, Norton L. Relationships between older adults’ use of time and cardio-respiratory fitness, obesity and cardio-metabolic risk: a compositional isotemporal substitution analysis. Maturitas. 2018;110:104–110. doi: 10.1016/j.maturitas.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 64.Dumuid D, Maher C, Lewis LK, Stanford TE, Martín Fernández JA. Human development index, children's health-related quality of life and movement behaviors: a compositional data analysis. Qual Life Res. 2018;27:1473–1482. doi: 10.1007/s11136-018-1791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dumuid D, Wake M, Clifford S, Burgner D, Carlin JB, Mensah FK. The association of the body composition of children with 24-hour activity composition. J Pediatr. 2019;208:43–49. doi: 10.1016/j.jpeds.2018.12.030. [DOI] [PubMed] [Google Scholar]
- 66.Fairclough SJ, Dumuid D, Taylor S, Curry W, McGrane B, Stratton G. Fitness, fatness and the reallocation of time between children's daily movement behaviours: an analysis of compositional data. Int J Behav Nutr Phys Act. 2017;14:64. doi: 10.1186/s12966-017-0521-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Foley L, Dumuid D, Atkin AJ, Olds T, Ogilvie D. Patterns of health behaviour associated with active travel: a compositional data analysis. Int J Behav Nutr Phys Act. 2018;15:26. doi: 10.1186/s12966-018-0662-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gupta N, Dumuid D, Korshøj M, Jørgensen MB, Søgaard K, Holtermann A. Is daily composition of movement behaviors related to blood pressure in working adults. Med Sci Sports Exerc. 2018;50:2150–2155. doi: 10.1249/MSS.0000000000001680. [DOI] [PubMed] [Google Scholar]
- 69.Gupta N, Hallman DM, Dumuid D, Vij A, Rasmussen CL, Jørgensen MB. Movement behavior profiles and obesity: a latent profile analysis of 24-h time-use composition among Danish workers. Int J Obes (Lond) 2019;44:409–417. doi: 10.1038/s41366-019-0419-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gupta N, Korshøj M, Dumuid D, Coenen P, Allesøe K, Holtermann A. Daily domain-specific time-use composition of physical behaviors and blood pressure. Int J Behav Nutr Phys Act. 2019;16:4. doi: 10.1186/s12966-018-0766-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lewthwaite H, Old T, Williams MT, Effing TW, Dumuid D. Use of time in chronic obstructive pulmonary disease: longitudinal associations with symptoms and quality of life using a compositional analysis approach. PloS One. 2019;14 doi: 10.1371/journal.pone.0214058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McGregor DE, Palarea-Albaladejo J, Dall PM, Del Pozo Cruz B, Chastin SFM. Compositional analysis of the association between mortality and 24-hour movement behaviour from NHANES. Eur J Prev Cardiol. 2019 doi: 10.1177/2047487319867783. [DOI] [PubMed] [Google Scholar]
- 73.Powell C, Browne LD, Carson BP, Dowd KP, Perry IJ, Kearney PM. Use of compositional data analysis to show estimated changes in cardiometabolic health by reallocating time to light-intensity physical activity in older adults. Sports Med. 2019;50:205–217. doi: 10.1007/s40279-019-01153-2. [DOI] [PubMed] [Google Scholar]
- 74.Ryan DJ, Wullems JA, Stebbings GK, Morse CI, Stewart CE, Onambele-Pearson GL. The difference in sleep, sedentary behaviour, and physical activity between older adults with “healthy” and “unhealthy” cardiometabolic profiles: a cross-sectional compositional data analysis approach. Eur Rev Aging Phys Act. 2019;16:25. doi: 10.1186/s11556-019-0231-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Talarico R, Janssen I. Compositional associations of time spent in sleep, sedentary behavior and physical activity with obesity measures in children. Int J Obes (Lond) 2018;42:1508–1514. doi: 10.1038/s41366-018-0053-x. [DOI] [PubMed] [Google Scholar]
- 76.Taylor RW, Haszard JJ, Farmer VL, Richards R, Te Morenga L, Meredith-Jones K. Do differences in compositional time use explain ethnic variation in the prevalence of obesity in children? Analyses using 24-hour accelerometry. Int J Obes (Lond) 2019;44:94–103. doi: 10.1038/s41366-019-0377-1. [DOI] [PubMed] [Google Scholar]
- 77.Taylor RW, Haszard JJ, Meredith-Jones KA, Galland BC, Heath ALM, Lawrence J. 24-h movement behaviors from infancy to preschool: cross-sectional and longitudinal relationships with body composition and bone health. Int J Behav Nutr Phys Act. 2018;15:118. doi: 10.1186/s12966-018-0753-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rhodes RE, Berry T, Faulkner G, Latimer-Cheung AE, O'Reilly N, Tremblay MS. Application of the multi‐process action control framework to understand parental support of child and youth physical activity, sleep, and screen time behaviours. Appl Psychol Health Well Being. 2019;11:223–239. doi: 10.1111/aphw.12150. [DOI] [PubMed] [Google Scholar]
- 79.Latimer-Cheung AE, Copeland JL, Fowles J, Zehr L, Duggan M, Tremblay MS. The Canadian 24-hour movement guidelines for children and youth: implications for practitioners, professionals, and organizations. Appl Physiol Nutr Metab. 2016;41(Suppl. 3):S328–S335. doi: 10.1139/apnm-2016-0086. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.