Highlights
-
•
Moderate-to-vigorous and total physical activity are significantly positively associated with fundamental motor skills in the early years.
-
•
Only 1 longitudinal study has explored mediation and found that perceived motor competence did not mediate the association between motor competence and total or moderate-to-vigorous physical activity.
-
•
There is limited evidence from longitudinal studies to support or disprove the Stodden conceptual model that physical activity drives motor competence in early years and vice versa in later childhood.
Keywords: Early years, Fundamental motor skills, Physical activity
Abstract
Background
Physical activity (PA) in the early years is associated with a range of positive health outcomes. Fundamental motor skill (FMS) competence is associated with PA and is theorized to be driven by PA in the early years and vice versa in mid to late childhood. However, to date, no studies have meta-analyzed the association between PA and FMS in the early years.
Methods
Six electronic databases were searched for articles published up to April 2019. Cross-sectional and longitudinal studies were included if they targeted children (ages 3–6 year) as the population of the study and assessed the association between objectively measured PA and FMS. Total FMS, total physical activity (TPA), and moderate-to-vigorous physical activity (MVPA) data were meta-analyzed using a random effects model.
Results
We identified 24,815 titles and abstracts. In total, 19 studies met the inclusion criteria, including 14 cross-sectional and 4 longitudinal studies, as well as 1 study with cross-sectional and longitudinal analysis. There was a significant but small positive association between FMS and MVPA (r = 0.20, 95% confidence interval (CI): 0.13–0.26) and TPA (r = 0.20, 95%CI: 0.12–0.28). Findings from longitudinal studies revealed that PA drives FMS in early childhood. Mediation was explored in 1 study, which found that perceived motor competence did not mediate the association between FMS and PA.
Conclusion
Using a meta-analysis, this study is the first to show a positive association between FMS, MVPA, and TPA in the early years of childhood, suggesting that the association begins at an early age. Limited evidence from longitudinal studies supports the theory that PA drives FMS in the early years of childhood. More evidence is needed from large studies to track PA and FMS until mid to late childhood and to explore the mediators of this association.
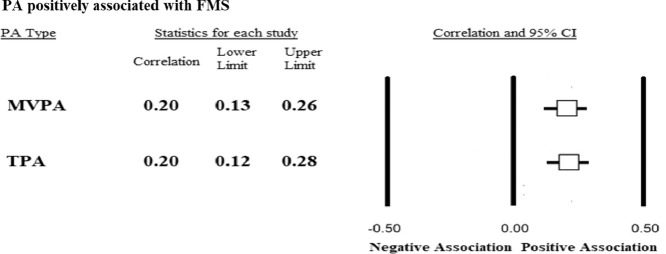
Graphical Abstract
1. Introduction
Engagement in physical activity (PA) in the early years of childhood brings a range of positive health outcomes, such as improvement in adiposity, cognitive development, and bone and skeletal, psychosocial, and cardiometabolic health.1 The PA guidelines in the UK recommend that preschool children should engage in at least 180 min of PA per day, with at least 60 min of this being moderate-to-vigorous physical activity (MVPA).2 Similar recommendations are provided in Canadian and Australian PA guidelines.3,4 However, compliance rates vary across the globe; studies have found that in Australia 93% of children meet the guidelines,5 whereas in Canada only 62% meet the recommendations when PA is assessed using accelerometry.6 A review of preschool PA levels found that the proportion of children meeting the recommendations varies from 27% to 100%.7
Understanding the mechanisms underlying participation in PA is important. Stodden et al.8 describe a conceptual model in which a number of health-related factors might influence PA engagement. One of these factors is motor competence, which encapsulates fundamental motor skills (FMS). FMS have been described as the initial building blocks of more complex, coordinated movements.9 Stodden et al.8 suggested that PA and FMS have a reciprocal and dynamic relationship in which, at a young age, PA could drive development of FMS which, in turn, drives engagement in PA at a later age. Establishing the relationship between PA and FMS in the early years of childhood, and seeing how this relationship changes over time, can help to test this premise.
Stodden et al.8 also hypothesized that mediators such as perceived motor competence might influence this association. In early years, when cognition is underdeveloped, there is likely to be a small correlation between perceived motor competence and actual motor competence. This is valuable because children may persist in activities in which they perceive themselves to be competent, which can drive skill acquisition. However, in later childhood, when children are more cognitively developed, the correlation between perceived and actual motor competence is stronger. Children who have low motor competence will have low perceived motor competence and engage in less PA. This, in turn, might affect the risk of conditions associated with physical inactivity such as obesity, which would ultimately provide feedback concerning their motor competence and subsequent PA levels. By examining what mediates the relationship between PA and FMS, we can determine the underlying mechanism by which one influences the other and highlight potential targets for intervention.
The relationship between FMS and PA across different age groups has been narratively synthesized in several systematic reviews.10, 11, 12 Logan et al.10 reported a low to moderate association between FMS and PA in early childhood from 4 studies, a low to high association in middle to late childhood from 7 studies, and a low to moderate association in adolescence from 2 studies. Lubans et al.11 explored the association between FMS and PA in children and adolescents across 21 cross-sectional studies and found strong evidence of a positive association; this was similar to the findings of another review of cross-sectional studies from Holfelder and Schott.12 Finally, a narrative review found that 8 of 11 studies of children 3–5 years old reported a significant relationship between motor skill competence and PA.13 Given the growing evidence demonstrating the association between PA and health outcomes that affect child development,14 such as obesity1 and cognitive outcomes, the establishment of the association between PA and FMS may have public health implications, which could lead to the further implementation of PA or FMS interventions in the early years.
A meta-analysis in this area is important because it tries to establish a statistical significance across studies in this area, thus increasing validity. This can provide public health and early-childhood practitioners with more reliable and valid information which, in turn, can guide practice and policies in the area. Likewise, the mediators of the association between FMS and PA, which might have important implications for the design of PA or FMS interventions, have never been synthesized. Therefore, the aim of this study was to synthesize and meta-analyze the evidence from cross-sectional and longitudinal studies to examine the association between FMS and PA in children 3–6 years old and to investigate the potential mediators of this association. To our knowledge, this is the first meta-analysis of the association between FMS and PA in preschool-aged children (3–6 years old).
2. Methods
This systematic review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria.15 The protocol for this systematic review has been registered at the International Prospective Register for Systematic Reviews (PROSPERO), registration number 2017: CRD42017062581.
2.1. Literature search
In April 2017, we carried out an online search of 6 databases (MEDLINE, EMBASE, PsycINFO, SPORTDiscus, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Education Resources Information Center (ERIC)); the search was repeated in April 2019 to update the review. The search strategy contained keywords, including “children”, “fundamental motor skills”, “physical activity”, and “association”. These keywords were arranged using Boolean operators to provide a sensitive and specific search strategy; an example of the search strategy (e.g., for MEDLINE) can be found in Supplementary File 1. No language or time barriers were placed on the search. Files were imported into Endnote reference management software (Version X7; Thomson Reuters, Toronto, ON, Canada), and duplicates were removed. The references of included articles identified in the search were hand searched for additional relevant publications.
2.2. Study inclusion and exclusion criteria
Studies were included if they met the following inclusion criteria: (1) participants in the study included children between 3 and 6 years of age at baseline and up to 11 years (average age) at follow-up; (2) the study was performed using normally developing children; (3) PA was measured objectively using an accelerometer or a pedometer; (4) the study reported a total or global FMS score assessed using validated methods; (5) the study reported the correlation between FMS and PA; and (6) the study used a cross-sectional or longitudinal design. Studies were excluded if: (1) the average age of the participants in the study at baseline or in a cross-sectional study was greater than 6 years old or the study did not report subgroup data for this age group; and (2) the study was performed using children who had developmental delays or physical impairments.
2.3. Study selection and data extraction
The first author (DJ) screened all titles and abstracts identified through the search against the study’s selection criteria. Another researcher (LBA) reviewed a random sample of 20% of the excluded titles. Those papers that met the inclusion criteria were reviewed in full and in duplicate by several pairs of researchers (DJ and LBA, DJ and ELG, DJ and AI, and DJ and EvS). Backward and forward reference searching of the included studies was carried out in May 2019.
A standardized data extraction form was used to collect methodologic and outcome variables from each included study. Data extracted included: study information (e.g., authors and publication year); population (e.g., age, sex, and number of participants); measurement tools (e.g., FMS tool and PA tool); outcome measures (baseline and follow-up (if longitudinal) of FMS and PA data); and analysis (PA data processing and correlation values between FMS and PA). All of the data were extracted by DJ and validated by LBA, ELG, AI, and EvS.
2.4. Study quality assessment
All studies were assessed using the observational studies tool from the Evidence for Policy and Practice Information Centre.16 This tool has 6 items for assessing internal and external validity, including type of study, number of participants, representation of general population, adjustment of the analysis, and objective measure of the outcome and exposure. Studies were classified as low, intermediate, or high, based on the number of criteria they met: (1) low < 3, (2) intermediate 3–5, and (3) high > 5. Quality assessment was performed by 2 reviewers independently (DJ and LBA); any disagreements were decided on by a third reviewer (AI).
2.5. Data synthesis and meta-analysis
Cross-sectional studies were meta-analyzed. Papers that reported total physical activity (TPA) using different units (e.g., min/h of PA, counts/min, total number of steps/day) were grouped in the same analysis. Papers that reported MVPA were grouped in a separate analysis. This included percent of MVPA/day or min of MVPA/day; these were grouped regardless of the cut-points used.
Authors were contacted if they had measured the association between FMS and PA using regression analyses but had not reported the Pearson correlation (r) values. Eight of the authors contacted17, 18, 19, 20, 21, 22, 23, 24 provided the information required. One author could not be contacted and was excluded from the analysis.
Meta-analyses were carried out for total FMS and MVPA and for total FMS and TPA. Analyses were performed using the statistical software Comprehensive Meta-Analysis (Version 3.0; Biostat, Englewood, NJ, USA). If studies reported correlation data separately for boys and girls, they were entered separately into the meta-analysis. In studies in which both univariate and multivariate correlations were available, only the univariate correlations were included in the meta-analysis because not all papers had included the same characteristics in the multivariate analysis. Correlation values (r) were pooled and entered into the software along with the sample size of the study. Correlation coefficients were transformed to Fisher z and then weighted and averaged and transformed back to a pooled r. Heterogeneity among the studies was measured using the tau statistic (τ), a standard deviation representing the typical variability of the mean between studies.25 Pooled correlation values (r) with 95% confidence intervals (CIs) were calculated for all studies included in the meta-analysis. A random effects model was used to derive a pooled estimate of the correlation values.26 To interpret the strength of correlation, we used Cohen cut-off points of 0.10, 0.30, and 0.50: cut-off r < 0.30 as small, 0.30 ≤ r < 0.50 as medium, and r ≥ 0.50 as large.27 A funnel plot was used to investigate publication bias.
Sensitivity analyses were performed to investigate the effect of combining studies reporting MVPA with studies reporting TPA because these variables are highly correlated.28 The first sensitivity analysis incorporated all studies that reported MVPA with studies that reported only TPA. The second sensitivity analysis incorporated all studies that reported TPA with studies that reported only MVPA. Sensitivity analyses exploring studies in which the same or similar motor skills tests (i.e., Test of Gross Motor Development-2 (TGMD-2), TGMD-3, and Children's Activity and Movement in Preschool Study Motor Skills Protocol (CMSP)) were applied. CMSP and TGMD-2 were combined in the analysis because the test procedures are identical. This analysis was performed for TPA and MVPA. A sensitivity analysis was performed in studies that had used only accelerometers to measure PA. Further sensitivity analyses were conducted to investigate the effect of using the adjusted models for each paper on the association between FMS with TPA and MVPA.
Included longitudinal studies presented a wide disparity in data-collection methods and analysis; for example, some studies measured PA at baseline and FMS at follow up, or vice versa. Furthermore, not all studies reported the change in PA or FMS over time. Therefore, a meta-analysis was deemed inappropriate, and these studies were synthesized narratively.
3. Results
3.1. Study selection
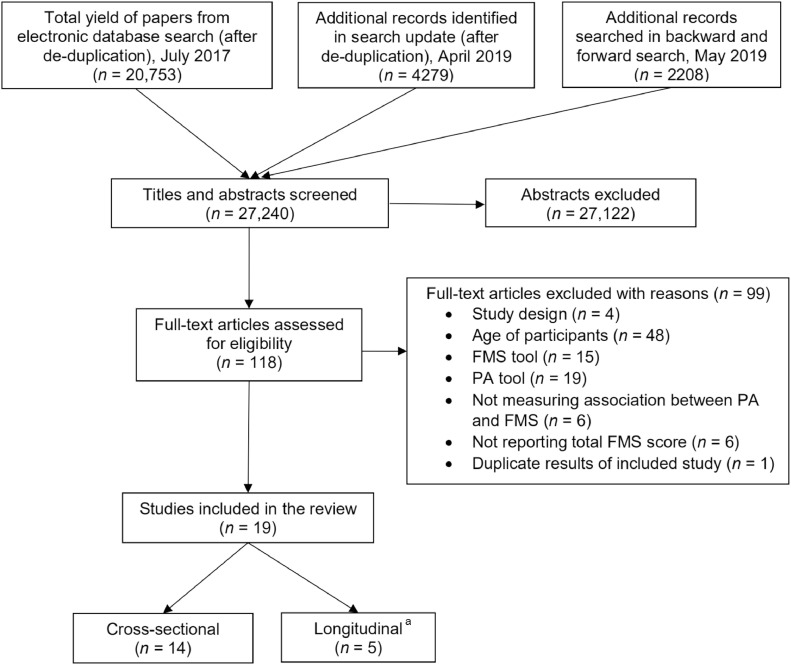
The 2 searches yielded a total of 37,094 citations; however, 9854 of these were duplicate citations and were, therefore, removed, leaving 27,240 papers in total. Nineteen papers17, 18, 19, 20, 21, 22, 23, 24,28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38 met the inclusion criteria and were included in the review. Fourteen cross-sectional studies18, 19, 20, 21, 22, 23, 24,28, 29, 30, 31, 32, 33, 34 were included in the meta-analyses, and 4 longitudinal studies35, 36, 37, 38 were included in the narrative synthesis. One study17 presented both cross-sectional and longitudinal data; the cross-sectional data were included in the meta-analysis, and the longitudinal data were included in the narrative analysis. Fig. 1 shows the PRISMA flowchart.
Fig. 1.
PRISMA flow diagram for the identification, screening, eligibility, and inclusion of studies. Databases included the following: MEDLINE, EMBASE, PsycINFO, SportDiscus, ERIC, and CINAHL. a one study contained both cross-sectional and longitudinal data. CINAHL = Cumulative Index to Nursing and Allied Health Literature; ERIC = Education Resources Information Center; FMS = fundamental motor skills; PA = physical activity; PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
3.2. Study characteristics
Table 1 summarizes the 19 studies included in the review. All studies were published in English between 2004 and 2018 and were conducted in 8 countries: UK (n = 4),20,23,28,32 USA (n = 5),24,29,33,36,37 Switzerland (n = 3),22,35,38 Greece (n = 1),31 Finland (n = 2),19,21 Australia (n = 2),17,30 South Africa (n = 1),34 and Denmark (n = 1).18 No studies were conducted on the continents of South America or Asia. Seventeen studies were conducted in preschool settings,18, 19, 20, 21, 22,24,28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38 1 study in a primary school setting,23 and 1 study did not state where the data collection was carried out.17 Overall, the cross-sectional studies included 2578 participants, and the longitudinal studies included 1239 participants. Hall et al.28 and Hall et al.23 were both cross-sectional studies based on the same original population but measured at different time points. Schmutz et al.35 was the follow-up to the longitudinal study by Schmutz et al.22
Table 1.
Included studies.
| First author and year | Country | Age (year) | Setting | Participants | FMS test | PA measurement | Correlation |
|---|---|---|---|---|---|---|---|
| Cross-sectional studies | |||||||
| Barnett et al., 201617 | Australia | 5 | Not stated | 127 | TGMD-2 | GT1M ActiGraph | FMS + MVPA; r = 0.163 |
| Cliff et al., 200930 | Australia | 3–6 | Preschool | 46 | TGMD-2 | 7164 ActiGraph | Boys FMS + mean cpm; r = 0.387 |
| Boys FMS + MVPA; r = 0.380 | |||||||
| Girls FMS + mean cpm; r = –0.199 | |||||||
| Girls FMS + MVPA; r = –0.456 | |||||||
| Cook et al., 201934 | South Africa | Mean age in months 50.73 | Preschool | 129 | TGMD-2 | GT3X ActiGraph | FMS + TPA; r = 0.150 |
| FMS + MVPA; r = 0.240 | |||||||
| Fisher et al., 200432 | UK | Mean age 4.2 | Preschool | 394 | MAB | CSA accelerometer | FMS + TPA; r = 0.100 |
| FMS + MVPA; r = 0.180 | |||||||
| Foweather et al., 201520,* | UK | 3–5 | Preschool | 99 | TGMD-2 | GT1M ActiGraph | FMS + TPA; r = 0.102 |
| FMS + MVPA; r = 0.114 | |||||||
| Guo et al., 201829 | USA | 3–5 | Preschool | 227 | CMSP | 7164 ActiGraph | FMS + TPA; r = 0.170 |
| Hall et al., 201828 | UK | Mean age 4.28 | Preschool | 166 | TGMD-2 | GENEActiv Accelerometer | FMS + TPA; r = 0.402 |
| FMS + MVPA; r = 0.376 | |||||||
| Hall et al., 201923,* | UK | Mean age 5.37 | School | 38 | TGMD-2 | GENEActiv accelerometer | FMS + TPA; r = –0.120 |
| FMS + MVPA; r = –0.170 | |||||||
| Iivonen et al., 201319,* | Finland | Mean age in months 49.14 | Preschool | 37 | APM Inventory | GT3X ActiGraph | FMS + TPA r = 0.402 |
| FMS + MVPA; r = 0.419 | |||||||
| Kambas et al., 201231 | Greece | 5–6 | Preschool | 232 | BOTMP-SF | OMRON pedometers | FMS + TPA; r = 0.368 |
| Wester et al., 201924,* | USA | 3.4 | Preschool | 88 | TGMD-3 | GT3X ActiGraph | FMS + TPA; r = 0.140 |
| FMS + MVPA; r = 0.290 | |||||||
| Laukkanen et al., 201421,* | Finland | 5–6 | Preschool | 53 | KTK | X6-1a accelerometer | Boys FMS + cpm; r = 0.448 |
| Girls FMS + cpm; r = 0.138 | |||||||
| Olesen et al., 201518,* | Denmark | 5–6 | Preschool | 350 | KTK | GT1M and GT3X ActiGraph | Boys FMS + MVPA; r = 0.279 |
| Girls FMS + MVPA; r = 0.127 | |||||||
| Schmutz et al., 201722,* | Switzerland | Mean age 3.9 | Preschool | 394 | ZNA | wGT3X-BT ActiGraph | FMS + TPA; r = 0.160 |
| FMS + MVPA; r = 0.170 | |||||||
| Williams et al., 200833 | USA | 3–4 | Preschool | 198 | CMSP | 7164 ActiGraph | FMS + MVPA; r = 0.200 |
| Longitudinal studies | |||||||
| Barnett et al., 201617 | Australia | 5 | Not stated | 127 | TGMD-2 | GT1M ActiGraph | MVPA at 3.5 years of age approached significance for predicting FMS at age 5. |
| Bürgi et al., 201138 | Switzerland | Baseline 5.2 (follow-up 9 months later) | Preschool | 217 | Balance and agility test | GT1M ActiGraph | Significant association between baseline TPA and changes in agility and balance at follow-up. |
| Gu 201636 | USA | Mean age 5.37 | Preschool | 256 | PE metrics | Actical accelerometers | FMS + MVPA; r = 0.260 |
| Gu et al., 201837 | USA | Mean age 5.37 | Preschool | 141 | PE metrics | Actical accelerometers | FMS + MVPA; r = 0.280 |
| Schmutz et al., 201835 | Switzerland | Baseline 3.9 (follow-up 1 year later) | Preschool | 498 | ZNA | wGT3X-BT ActiGraph | FMS and both TPA and MVPA were significantly positively associated at baseline. |
| FMS and both change in TPA and change in MVPA were not significantly associated. | |||||||
Abbreviations: BOTMP-SF = Bruininks-Oseretsky Test of Motor Proficiency-Short Form; CMSP = CHAMPS motor skills protocol; cpm = counts per min; FMS = fundamental motor skills; KTK = KörperKoördinations Test für Kinder; MAB = Movement Assessment Battery; MVPA = moderate-to-vigorous physical activity; PA = physical activity; PE = physical education; TGMD = Test of Gross Motor Development; TPA = total physical activity; ZNA = Zurich Neuromotor Assessment.
Denotes that the author was contacted to provide correlation data.
Fifteen cross-sectional studies were identified, of which 14 used accelerometers to measure PA,17, 18, 19, 20, 21, 22, 23, 24,28, 29, 30,32, 33, 34 whereas one used a pedometer.31 Thirteen studies used an ActiGraph model, with 1 study using 2 different ActiGraph models (7164: n = 3; GT1M: n = 4; GT3X: n = 4; wGT3X-BT: n = 2; CSA: n = 1) (ActiGraph, Pensacola, FL, USA).17, 18, 19, 20,22,24,29,30,32, 33, 34, 35,38 One study used an X6-1a accelerometer (Gulf Coast Data Concepts, Waveland, MS, USA),21 2 studies used a GENEActiv accelerometer (GeneActiv Activeinsights, Cambridge, UK),23,28 2 studies used Actical accelerometers (Mini-Mitter, Bend, OR, USA),36,37 and 1 study used Omron Pedometers (Omron, Kyoto, Japan).31
Measurement tools used to assess FMS varied widely. Ten different measurement tools were used; they included the CMSP (n = 2),29,33 which is based on the TGMD-2 (n = 6)17,20,23,28,30,34 and TGMD-3 (n = 1);24 the Körperkoordinations Test für Kinder (n = 2);18,21 the Bruininks-Oseretsky Test of Motor Proficiency-Short Form (n = 1);31 the APM Inventory (n = 1);19 the Movement Assessment Battery (MAB) (n = 1);32 the Zurich Neuromotor Assessment (ZNA) (n = 2);22,35 the PE Metrics (n = 2);36,37and the Balance and Agility Tests (n = 1).38 Accelerometer cut-points also varied among studies. The cut-points used to define MVPA ranged from 1680 counts/min20,22,24,33, 34, 35,38 to 3564 counts/min.30 Of the studies that reported cut-points, 7 different values were used to define MVPA. The most frequently used cut-point for MVPA was 1680 counts/min.
3.3. Quality assessment
Study quality ranged from intermediate to high. All of the longitudinal studies,35, 36, 37, 38 1 cross-sectional study,22 and the study including both cross-sectional and longitudinal data17 were deemed to be of high quality. Three studies did not analyze more than 50 participants.19,23,30 It was unclear for 10 of the included studies18,20,28,29,32, 33, 34,36, 37, 38 whether the author deemed the study sample to be representative of the general population. Fifteen of the included studies used adjusted or multivariate analysis17, 18, 19, 20,22, 23, 24,29,30,33, 34, 35, 36, 37, 38 as part of the inclusion criteria. All of the studies used objective measures of PA and a validated measure of FMS. A summary of the quality assessment scores for all included papers can be found in Supplementary Table 1.
3.4. Meta-analyses
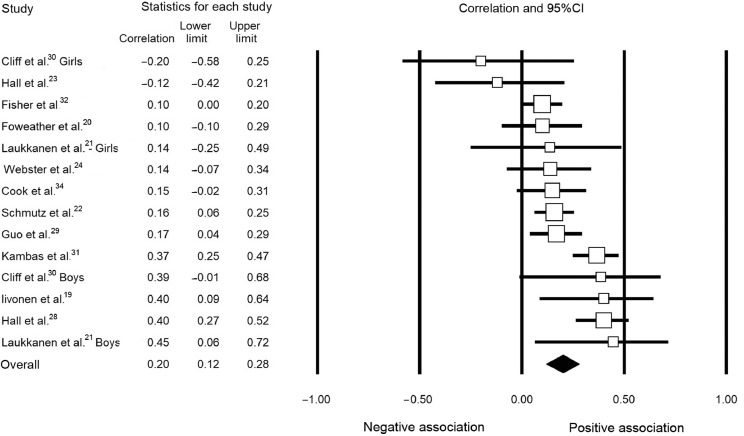
The correlation values for either (or both) total FMS and TPA or total FMS and MVPA were extracted (or provided by the authors of the 12 cross-sectional studies) and were included in the meta-analyses. The meta-analysis for total FMS and TPA included 12 studies.19, 20, 21, 22, 23, 24,28, 29, 30, 31, 32,34 Fig. 2 shows that the pooled correlation between total FMS and TPA was statistically significant but small: r = 0.20 (95%CI: 0.12–0.28). Heterogeneity was present in this analysis, with an τ value of ±0.113.
Fig. 2.
Forest plot of the correlation between total physical activity and fundamental motor skills. CI = confidence interval.
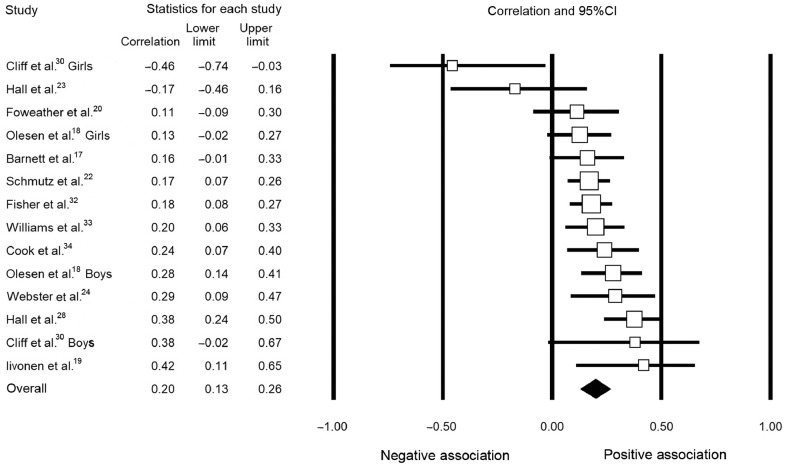
A meta-analysis of the association between MVPA and FMS is presented in Fig. 3. Twelve studies17, 18, 19, 20,22, 23, 24,28,30,32, 33, 34 were entered into this meta-analysis. There was a significant, but small, pooled correlation of r = 0.20 (95%CI: 0.13–0.26). Heterogeneity was present in this analysis, with an τ value of ±0.089.
Fig. 3.
Forest plot of the correlation between moderate-to-vigorous physical activity and fundamental motor skills. CI = confidence interval.
TPA and MVPA were combined in 2 separate meta-analyses. First, papers that reported TPA were pooled together with papers that reported only MVPA. The pool of 15 studies presented a significant, but small, correlation, with r = 0.20 (95%CI: 0.14–0.26, τ = ±0.091). Second, papers that reported MVPA were pooled together with papers reporting TPA only (n = 15). A similar and significant correlation was observed, with r = 0.21 (95%CI: 0.15–0.27, τ = ±0.092).
Sensitivity analyses were carried out by looking at studies that used the same FMS measurement tool (n = 9), the TGMD-2 and CMSP, and TPA and MVPA (TPA as preference). The correlation remained significant and positive (r = 0.18, 95%CI: 0.09–0.26, τ = ±0.096) but weaker compared with the analyses using all FMS measurement tools, as reported earlier (r = 0.20, 95%CI: 0.14–0.26, τ = ±0.091).
For studies using the same FMS measurement tools and reported associations of TPA and MVPA (MVPA as preference), the correlation also remained significantly positive (r = 0.18, 95%CI: 0.08–0.28, τ = ±0.121) but weaker when compared with all FMS tools together (r = 0.21, 95%CI: 0.15–0.27, τ = ±0.092).
Sensitivity analyses looking only at studies using accelerometers to measure MVPA or TPA (Kambas et al.31 was removed from the analyses because of pedometer use) found that the heterogeneity of the analysis decreased for all affected analyses, and pooled correlation remained significant: (1) TPA and MVPA (TPA as preference) (r = 0.18, 95%CI: 0.13–0.24, τ = ±0.073) and (2) TPA and MVPA (MVPA as preference) (r = 0.20, 95%CI: 0.14–0.26, τ = ±0.080). A final sensitivity analysis investigated the effect on the association between FMS and MVPA and TPA for studies that used an adjusted statistical model as part of their analysis. For both MVPA and TPA, the strength of the association decreased slightly (TPA: r = 0.19, MVPA: r = 0.18) but remained significant.
3.5. Longitudinal studies
A total of 5 longitudinal studies were included in the review. Two of these studies were conducted by the same research team36,37 with different populations of children. The teams measured FMS using PE Metrics in U.S. kindergarteners during autumn; PA was measured using Actical accelerometers the following spring. An Australian study17 measured children's MVPA using ActiGraph GT1M accelerometers at the following ages—19 months, 3.5 years, and 5 years—and children's FMS skills were measured using TGMD-2 at age 5. Bürgi et al.38 measured Swiss children's (mean age = 5.2 years) agility and dynamic balance as motor skills, and their PA was measured using ActiGraph GT1M accelerometers at baseline and 9 months later. Another Swiss study28 assessed FMS using the ZNA, and PA was measured using an ActiGraph wGT3X-BT accelerometer at baseline and 1 year later.
3.5.1. FMS as a predictor of PA
Findings from longitudinal studies revealed that FMS can act as a predictor of PA for some FMS domains, in particular object control and locomotor skills. Gu36 found a positive and significant association between total FMS (r = 0.26), object control skills (r = 0.21), and locomotor skills (r = 0.21) with MVPA at follow-up. The author also found that locomotor skills, but not object control skills, explained significant variance in MVPA after controlling for body mass index.
Gu et al.37 found a positive and significant association between MVPA and total FMS (r = 0.28), object control skills (r = 0.24), and locomotor skills (r = 0.24) at follow-up.
Similarly, Schmutz et al.35 identified gross motor skills at baseline as a determinant of TPA (p = 0.048) and MVPA (p = 0.023) at follow-up. However, despite the increase in PA over the period of the study, gross motor skills at baseline were not significantly associated with change in either TPA or MVPA from baseline to follow-up. Bürgi et al.38 also found that changes in agility (p ≥ 0.14) and balance (p ≥ 0.14) from baseline to follow-up did not significantly predict PA at follow-up.
3.5.2. PA as a predictor of FMS
Only 2 studies explored the longitudinal association of PA as a predictor of FMS, showing a positive association of PA for predicting some FMS domains (e.g., balance and locomotor skills) but no association or negative association for others (e.g., agility and object control).
Bürgi et al.38 found that baseline TPA was negatively associated with change in agility (p = 0.005) and positively associated with change in balance (p = 0.02) over 9 months. However, Barnett et al.17 found that MVPA in children at 3.5 years of age approached significance in positively predicting total skills score (p = 0.059) and positively predicting locomotor skills at age 5 (p = 0.033). However, MVPA among children at any age did not significantly predict object-control skills at age 5.
3.6. Mediators
Only 1 study included in this review investigated the mediators of the relationship between FMS and TPA. Hall et al.23 found that in the early childhood years, neither TPA nor MVPA was positively associated with an increase in motor competence as mediated by perceived motor competence.
4. Discussion
The aim of this review was to synthesize the evidence concerning the relationship between FMS and PA in the early childhood years, in studies that were both cross-sectional and longitudinal, while the secondary aim was to explore the mediators of this relationship. This review is the first to meta-analyze the cross-sectional association between FMS and PA in the early childhood years. We found that total FMS was positively associated with TPA (r = 0.20, 95%CI: 0.12–0.28) and MVPA (r = 0.20, 95%CI: 0.13–0.27), suggesting that the association between FMS and PA occurs at an early age.
This review also reports mixed findings from longitudinal studies. Of 5 longitudinal studies, 4 studies looked at FMS as a predictor of PA. In 2 studies,36,37 domains of FMS (i.e., object control and locomotor skills) predicted MVPA at follow-up. In another study,35 gross motor skills were identified as a determinant of PA at follow-up, but these were not associated with changes in PA from baseline to follow-up. Finally, 1 study38 found that agility and balance at baseline did not predict PA at follow-up. Similar to our findings, studies with older children have found that FMS skills can predict PA at a later age for some of the FMS domains. Barnett et al.39 found that object control skills at a mean age of 10 years predict PA levels in adolescence. This finding was echoed by Lopes et al.,40 who found that motor competence was an important predictor of PA between the ages of 6 and 10 years.
Conversely, 2 studies examined whether PA predicted FMS. One study38 found that changes in TPA were significantly associated with changes in agility and balance 9 months later, while another17 found that MVPA at 3.5 years of age approached significance for predicting FMS at age 5. The disparity between the data collection time points and the short follow-up period prevents firm conclusions’ being drawn about the direction of the relationship between FMS and PA. However, the findings from this review for FMS as a predictor of PA indicates that FMS does not drive changes in PA over a short time period in the early years, although changes in PA might predict changes in FMS in the early years.
The limited findings from longitudinal studies in our review cannot support or refute the theory developed by Stodden et al.8 that PA drives FMS in early childhood. It is important to test conceptual models to see whether they work in reality. Therefore, further studies should be conducted to explore the association between PA and FMS. In such studies, data collection would be performed in the early years and continue at regular follow-up intervals, including mid to late childhood, adolescence, and, potentially, adulthood. This would help to strengthen the evidence and clarify the direction of the association, thus enabling skill- and age-specific interventions to be developed.
Demonstrating the association between FMS and PA is important because it suggests that interventions in the early years could be of benefit for increasing FMS and PA in both the short and the long term. Several interventions have been designed to improve FMS in the early years; however, there is limited evidence from systematic reviews concerning the effect of FMS interventions in increasing PA. Van Capelle et al.41 found that FMS interventions do not significantly increase PA levels, attributing this finding to the discrepancies between studies in measuring PA. However, in a recent systematic review, Engel et al.42 found that teacher-led FMS interventions delivered at least 3 times a week can improve FMS proficiency, increase PA intensity, and reduce sedentary behavior in preschool children, suggesting that school-based interventions may be effective for increasing children's PA levels. Children may acquire rudimentary levels of some FMS through exploration, but to reach advanced levels of FMS requires instruction during childhood.43 This is evident from a number of early childhood interventions44, 45, 46 that have shown that simply providing children with free play time will not significantly improve their FMS, and it is only when children are instructed by trained specialists that significant improvements are made. These findings were confirmed in a narrative systematic review that supported the use of FMS interventions to improve children's FMS beyond free play.47 Concerning the effect of PA interventions on FMS, a systematic review of studies that examined the effect of PA interventions in the early years found that 80% of the included randomized control trials showed an improvement in motor skills.48 The authors concluded that PA interventions may be better at increasing PA and FMS during the early years as opposed to FMS interventions only, which may be a reason why PA drives FMS in the early years. However, this review did not find evidence to support or refute that theory. The authors also explored the association between PA and cognitive development and found a positive association for measures of academic achievement, learning, working memory, and language in 4 of 5 studies.48 This may have public health and educational implications because increasing PA in the early years could lead to better motor skills, health outcomes, and academic achievement. Given that motor competence and physical development are essential criteria for a child to be “school ready” in the early years,49 the dissemination of this evidence could be used to encourage schools and parents to increase the opportunities for children to engage in PA in their early years.
An important aspect of our study was the analysis of mediators of the association, which might support the design of an intervention. Stodden et al.8 theorized that perceived competence and physical fitness could mediate the relationship between PA and FMS, but it is likely to occur in middle childhood, when children have a better understanding of their competence and when their physical fitness is more important for engagement with PA and sport. The only study included in this review that explored mediators found that perceived motor competence did not mediate the relationship between motor competence and MVPA and TPA.23 This finding is similar to other research findings in which preschool children were the subjects. Crane et al.50 examined the individual domains of FMS, but not total FMS, and found that perceived motor competence did not mediate the relationship between object-control skill and MVPA in a small sample of preschool children. Although there is no evidence of mediation of motor competence and MVPA and TPA in the early years, 2 studies conducted in older children support Stodden et al.’s8 theory; these 2 studies demonstrate that perceived motor competence51,52 and physical fitness53,54 can mediate the association between motor competence and PA. However, there are no studies that explore physical fitness as a mediator in the early years. This is possibly due to the difficulty of measuring this outcome in the early years. Therefore, Stodden et al.8 may be accurate; the mediation effect of perceived competence and physical fitness on FMS and PA might be apparent only during middle childhood. However, more studies exploring mediators in early childhood with larger sample sizes are needed; current studies, including those by Hall et al.23 (n = 38) and Crane et al.50 (n = 116), were conducted with small numbers of participants.
This systematic review has not explored the individual domains of motor skills (object-control skills, locomotor skills, and balance) for cross-sectional studies. However, there is evidence to suggest that individual FMS domains might predict PA in the early years. Robinson et al.55 found that locomotor skill was a significant predictor of PA, but object-control skill was not. However, 2 studies50,56 found that object-control skill, but not locomotor skill, was significantly associated with PA. Further research is needed to explore whether these individual domains of motor skills develop naturally or as a result of structured practice or training and the rate at which these skills develop.
Our systematic review has several strengths, including a rigorous search-and-sifting methodology and the use of a meta-analysis. However, it is important to acknowledge the limitations of our review. In our study, only 20% of the excluded titles and abstracts were screened. Although this procedure has been used in many other systematic reviews57, 58, 59 in the field, future studies should consider double screening because, according to a recent methodologic systematic review, this could be a limitation.60 Another limitation is the inclusion of studies that used varying methodologies to assess motor skills. Although the skills measured were similar, the measurement tools or procedures used in various studies were different. For example, the Movement Assessment Battery Checklist includes a measure of fine motor skills, whereas TGMD-2 does not. Other tools measure all aspects of FMS, whereas the Körperkoordinations Test für Kinder does not assess object-control skill. However, the heterogeneity among the studies was not substantial, and previous meta-analyses have also pooled studies with different FMS assessment tools.61 Furthermore, sensitivity analyses revealed that the small positive association persisted, and heterogeneity was maintained when studies using the same assessment method were pooled. Due to the large magnitude of research into motor skills, we believe it is necessary to standardize a tool that can be used to measure motor skills across research internationally. This would increase the generalizability of studies as well as increase the likelihood of the study results’ being replicated. Another limitation to the meta-analysis is the varying cut-points and data-processing methods used to define objectively measured MVPA and TPA. Although these different methodologic procedures can be considered a limitation, in our study we investigated the correlation between the 2 variables (FMS and MVPA/TPA); thus, combining different measurement tools in the analysis had a minimum effect on our findings, and similar methods of analysis have been conducted in another meta-analysis.62 Nonetheless, the use of the same cut-points for MVPA would be useful for comparison across studies in the same age group.
Likewise, all but one31 of the studies included in this review used accelerometers to assess PA. Recent evidence suggests that accelerometery may not be the gold standard for measuring PA, and it may underestimate PA intensity in object projection skill performance.63 Therefore, the association between FMS and MVPA may be underestimated. Furthermore, many of the participants in these studies were required to remove the accelerometers for water-based activities, meaning that not all PA was captured.
5. Conclusion
This study is the first to meta-analyze the association between FMS and PA in the early years of childhood. A significant, but small, and positive association was found, which is consistent with narrative systematic reviews and studies in older children. The limited longitudinal findings cannot support or refute the Stodden conceptual model that PA drives FMS in early childhood. Additional longitudinal evidence is required to explore whether the association tracks into later life or whether FMS begins to drive PA. Finally, one study with a small sample (n = 38) examined a mediator of the relationship between FMS and PA and found that perceived motor competence did not mediate the relationship. More research is needed on this topic because mediators could potentially inform intervention components.
Acknowledgments
We are grateful for the contribution of Esther van Sluijs (EvS), who supported us on the conception of the study, sifting of the search results, and data extraction.
Authors’ contributions
DJ was involved in the conception of the study, the structured search, the sifting of search results, data extraction, quality assessment, analysis, and writing of the manuscript; AI, ELG, and LBA were involved in the conception of the study, sifting of search results, data extraction, quality assessment, and commenting on and editing of the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of the presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2020.03.001.
Appendix. Supplementary materials
References
- 1.Carson V., Lee E.Y., Hewitt L., Jennings C., Hunter S., Kuzik N. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(Suppl. 5):854. doi: 10.1186/s12889-017-4860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of Health and Social Care. UK Chief Medical Officers' Physical Activity Guidelines. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf. [accessed 04.10.2019].
- 3.Canadian Society for Exercise Physiology. Canadian 24 hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour and sleep. Available at: https://csepguidelines.ca/wp-content/themes/csep2017/pdf/PAR7972_24Hour_Guidelines_EY_En-4.pdf. [accessed 04.10.2019].
- 4.Australian Government Department of Health. Australian 24 hour movement guidelines for the early years (birth to 5 years). Available at: https://www1.health.gov.au/internet/main/publishing.nsf/Content/FCE78513DAC85E08CA257BF0001BAF95/$File/Birthto5years_24hrGuidelines_Brochure.pdf. [accessed 04.10.2019].
- 5.Cliff D.P., McNeill J., Vella S.A., Howard S.J., Santos R., Batterham M. Adherence to 24-Hour Movement Guidelines for the Early Years and associations with social-cognitive development among Australian preschool children. BMC Public Health. 2017;17(Suppl. 5):857. doi: 10.1186/s12889-017-4858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaput J.P., Colley R.C., Aubert S., Carson V., Janssen I., Roberts K.C. Proportion of preschool-aged children meeting the Canadian 24-h Movement Guidelines and associations with adiposity: results from the Canadian Health Measures Survey. BMC Public Health. 2017;17(Suppl. 5):829. doi: 10.1186/s12889-017-4854-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hnatiuk J.A., Salmon J., Hinkley T., Okely A.D., Trost S. A review of preschool children's physical activity and sedentary time using objective measures. Am J Prev Med. 2014;47:487–497. doi: 10.1016/j.amepre.2014.05.042. [DOI] [PubMed] [Google Scholar]
- 8.Stodden D.F., Langendorfer S.J., Goodway J.D., Roberton M.A., Rudisill M.E., Garcia C. A developmental perspective on the role of motor skill competence in physical activity: an emergent relationship. Quest. 2008;60:290–306. [Google Scholar]
- 9.Gallahue D.L., Ozmun J.C., Goodway J. McGraw-Hill; New York, NY: 2012. Understanding motor development: infants, children, adolescents, adults. [Google Scholar]
- 10.Logan S.W., Kipling E.W., Getchell N., Pfeiffer K.A., Robinson L.E. Relationship between fundamental motor skill competence and physical activity during childhood and adolescence: a systematic review. Kinesiol Rev. 2015;4:416–426. [Google Scholar]
- 11.Lubans D.R., Morgan P.J., Cliff D.P., Barnett L.M., Okely A.D. Fundamental movement skills in children and adolescents: review of associated health benefits. Sports Med. 2010;40:1019–1035. doi: 10.2165/11536850-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Holfelder B., Schott N. Relationship of fundamental movement skills and physical activity in children and adolescents: a systematic review. Psychol Sport Exerc. 2014;15:382–391. [Google Scholar]
- 13.Figueroa R., An R. Motor skill competence and physical activity in preschoolers: a review. Matern Child Health J. 2017;21:136–146. doi: 10.1007/s10995-016-2102-1. [DOI] [PubMed] [Google Scholar]
- 14.Carson V., Hunter S., Kuzik N., Wiebe S.A., Spence J.C., Friedman A. Systematic review of physical activity and cognitive development in early childhood. J Sci Med Sport. 2016;19:573–578. doi: 10.1016/j.jsams.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 15.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group PRISMA Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 16.Evidence for Policy and Practice Information and Coordinating (EPPI). Methods for conducting systematic reviews. Available at: https://www.betterevaluation.org/sites/default/files/Methods.pdf. [accessed 23.03.2017].
- 17.Barnett L.M., Salmon J., Hesketh K.D. More active pre-school children have better motor competence at school starting age: an observational cohort study. BMC Public Health. 2016;16:1068. doi: 10.1186/s12889-016-3742-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olesen L.G., Lund P.K., Korsholm L., Boye A.K., Froberg K. Correlates of objectively measured physical activity in 5-6-year-old preschool children. J Sport Med Phys Fit. 2015;55:513–526. [PubMed] [Google Scholar]
- 19.Iivonen K.S., Sääkslahti A.K., Mehtälä A., Villberg J.J., Tammelin T.H., Kulmala J.S. Relationship between fundamental motor skills and physical activity in 4-year-old preschool children. Percept Mot Skills. 2013;117:627–646. doi: 10.2466/10.06.PMS.117x22z7. [DOI] [PubMed] [Google Scholar]
- 20.Foweather L., Knowles Z., Ridgers N.D., O'Dwyer M.V., Foulkes J.D., Stratton G. Fundamental movement skills in relation to weekday and weekend physical activity in preschool children. J Sci Med Sport. 2015;18:691–696. doi: 10.1016/j.jsams.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 21.Laukkanen A., Pesola A., Havu M., Sääkslahti A., Finni T. Relationship between habitual physical activity and gross motor skills is multifaceted in 5- to 8-year-old children. Scand J Med Sci Sports. 2014;24:e102–e110. doi: 10.1111/sms.12116. [DOI] [PubMed] [Google Scholar]
- 22.Schmutz E.A., Leeger-Aschmann C.S., Radtke T., Muff S., Kakebeeke T.H., Zysset A.E. Correlates of preschool children's objectively measured physical activity and sedentary behavior: a cross-sectional analysis of the SPLASHY study. Int J Behav Nutr Phys Act. 2017;14:1. doi: 10.1186/s12966-016-0456-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall C.J.S., Eyre E.L.J., Oxford S.W., Duncan M.J. Does perception of motor competence mediate associations between motor competence and physical activity in early years children? Sports(Basel) 2019;7:E77. doi: 10.3390/sports7040077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webster E.K., Martin C.K., Staiano A.E. Fundamental motor skills, screen-time, and physical activity in preschoolers. J Sport Health Sci. 2019;8:114–121. doi: 10.1016/j.jshs.2018.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins J.P. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37:1158–1160. doi: 10.1093/ije/dyn204. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt F.L., Hunter J.E. SAGE Publications; Thousand Oaks, CA: 2014. Methods of meta-analysis: correcting error and bias in research findings. 3rd ed. [Google Scholar]
- 27.Cohen J. Lawrence Earlbaum Associates; Hillsdale, NJ: 1988. Statistical power analysis for the behavioral sciences. [Google Scholar]
- 28.Hall C.J.S., Eyre E.L.J., Oxford S.W., Duncan M.J. Relationships between motor competence, physical activity, and obesity in British preschool aged children. J Funct Morphol Kinesiol. 2018;3:57. doi: 10.3390/jfmk3040057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guo H., Schenkelberg M.A., O'Neill J.R., Dowda M., Pate R.R. How does the relationship between motor skill performance and body mass index impact physical activity in preschool children. Pediatr Exerc Sci. 2018;30:266–272. doi: 10.1123/pes.2017-0074. [DOI] [PubMed] [Google Scholar]
- 30.Cliff D.P., Okely A.D., Smith L.M., McKeen K. Relationships between fundamental movement skills and objectively measured physical activity in preschool children. Pediatr Exerc Sci. 2009;21:436–449. doi: 10.1123/pes.21.4.436. [DOI] [PubMed] [Google Scholar]
- 31.Kambas A., Michalopoulou M., Fatouros I.G., Christoforidis C., Manthou E., Giannakidou D. The relationship between motor proficiency and pedometer-determined physical activity in young children. Pediatr Exerc Sci. 2012;24:34–44. doi: 10.1123/pes.24.1.34. [DOI] [PubMed] [Google Scholar]
- 32.Fisher A., Reilly J.J., Kelly L.A., Montgomery C., Williamson A., Paton J.Y. Fundamental movement skills and habitual physical activity in young children. Med Sci Sports Exerc. 2005;37:684–688. doi: 10.1249/01.mss.0000159138.48107.7d. [DOI] [PubMed] [Google Scholar]
- 33.Williams H.G., Pfeiffer K.A., O'Neill J.R., Dowda M., McIver K.L., Brown W.H. Motor skill performance and physical activity in preschool children. Obesity. 2008;16:1421–1426. doi: 10.1038/oby.2008.214. [DOI] [PubMed] [Google Scholar]
- 34.Cook C.J., Howard S.J., Scerif G., Twine R., Kahn K., Norris S.A. Associations of physical activity and gross motor skills with executive function in preschool children from low-income South African settings. Dev Sci. 2019;22:e12820. doi: 10.1111/desc.12820. [DOI] [PubMed] [Google Scholar]
- 35.Schmutz E.A., Haile S.R., Leeger-Aschmann C.S., Kakebeeke T.H., Zysset A.E., Messerli-Bürgy N. Physical activity and sedentary behavior in preschoolers: a longitudinal assessment of trajectories and determinants. Int J Behav Nutr Phys Act. 2018;15:35. doi: 10.1186/s12966-018-0670-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gu X. Fundamental motor skill, physical activity, and sedentary behavior in socioeconomically disadvantaged kindergarteners. Psychol Health Med. 2016;21:871–881. doi: 10.1080/13548506.2015.1125007. [DOI] [PubMed] [Google Scholar]
- 37.Gu X., Keller M.J., Weiller-Abels K.H., Zhang T. The roles of physical activity and sedentary behavior on Hispanic children's mental health: a motor skill perspective. Qual Life Res. 2018;27:185–193. doi: 10.1007/s11136-017-1687-1. [DOI] [PubMed] [Google Scholar]
- 38.Bürgi F., Meyer U., Granacher U., Schindler C., Marques-Vidal P., Kriemler S. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross-sectional and longitudinal study (Ballabeina) Int J Obes(Lond) 2011;35:937–944. doi: 10.1038/ijo.2011.54. [DOI] [PubMed] [Google Scholar]
- 39.Barnett L.M., van Beurden E., Morgan P.J., Brooks L.O., Beard J.R. Childhood motor skill proficiency as a predictor of adolescent physical activity. J Adolesc Health. 2009;44:252–259. doi: 10.1016/j.jadohealth.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 40.Lopes V.P., Rodrigues L.P., Maia J.A., Malina R.M. Motor coordination as predictor of physical activity in childhood. Scand J Med Sci Sports. 2011;21:663–669. doi: 10.1111/j.1600-0838.2009.01027.x. [DOI] [PubMed] [Google Scholar]
- 41.Van Capelle A., Broderick C.R., van Doorn N., E Ward R., Parmenter B.J. Interventions to improve fundamental motor skills in pre-school aged children: a systematic review and meta-analysis. J Sci Med Sport. 2017;20:658–666. doi: 10.1016/j.jsams.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 42.Engel A.C., Broderick C.R., van Doorn N., Hardy L.L., Parmenter B.J. Exploring the relationship between fundamental motor skill interventions and physical activity levels in children: a systematic review and meta-analysis. Sports Med. 2018;48:1845–1857. doi: 10.1007/s40279-018-0923-3. [DOI] [PubMed] [Google Scholar]
- 43.Barnett L.M., Stodden D., Cohen K.E., Smith J.J., Lubans D.R., Lenoir M. Fundamental movement skills: an important focus. J Teach Phys Educ. 2016;35:219–225. [Google Scholar]
- 44.Goodway J.D., Branta C.F. Influence of a motor skill intervention on fundamental motor skill development of disadvantaged preschool children. Res Q Exerc Sport. 2003;74:36–46. doi: 10.1080/02701367.2003.10609062. [DOI] [PubMed] [Google Scholar]
- 45.Goodway J.D., Robinson L.E., Crowe H. Gender differences in fundamental motor skill development in disadvantaged preschoolers from two geographical regions. Res Q Exerc Sport. 2010;81:17–24. doi: 10.1080/02701367.2010.10599624. [DOI] [PubMed] [Google Scholar]
- 46.Foulkes J.D., Knowles Z., Fairclough S.J., Stratton G., O'Dwyer M., Ridgers N.D. Effect of a 6-week active play intervention on fundamental movement skill competence of preschool children: a cluster randomized controlled trial. Pecept Mot Skills. 2017;124:393–412. doi: 10.1177/0031512516685200. [DOI] [PubMed] [Google Scholar]
- 47.Logan S.W., Robinson L.E., Wilson A.E., Lucas W.A. Getting the fundamentals of movement: a meta-analysis of the effectiveness of motor skill interventions in children. Child Care Health Dev. 2012;38:305–315. doi: 10.1111/j.1365-2214.2011.01307.x. [DOI] [PubMed] [Google Scholar]
- 48.Zeng N., Ayyub M., Sun H., Wen X., Xiang P., Gao Z. Effects of physical activity on motor skills and cognitive development in early childhood: a systematic review. Biomed Res Int. 2017;2017 doi: 10.1155/2017/2760716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Standards & Testing Agency. Early Years Foundation Stage Profile 2019 Handbook. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/790580/EYFSP_Handbook_2019.pdf. [accessed 17.05.2019].
- 50.Crane J.R., Naylor P.J., Cook R., Temple V.A. Do perceptions of competence mediate the relationship between fundamental motor skill proficiency and physical activity levels of children in kindergarten? J Phys Act Health. 2015;12:954–961. doi: 10.1123/jpah.2013-0398. [DOI] [PubMed] [Google Scholar]
- 51.Barnett L.M., Morgan P.J., van Beurden E., Beard J.R. Perceived sports competence mediates the relationship between childhood motor skill proficiency and adolescent physical activity and fitness: a longitudinal assessment. Int J Behav Nutr Phys Act. 2008;5:40. doi: 10.1186/1479-5868-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barnett L.M., Morgan P.J., Van Beurden E., Ball K., Lubans D.R. A reverse pathway? Actual and perceived skill proficiency and physical activity. Med Sci Sports Exerc. 2011;43:898–904. doi: 10.1249/MSS.0b013e3181fdfadd. [DOI] [PubMed] [Google Scholar]
- 53.Khodaverdi Z., Bahram A., Stodden D., Kazemnejad A. The relationship between actual motor competence and physical activity in children: mediating roles of perceived motor competence and health-related physical fitness. J Sports Sci. 2016;34:1523–1529. doi: 10.1080/02640414.2015.1122202. [DOI] [PubMed] [Google Scholar]
- 54.Lima R.A., Pfeiffer K., Larsen L.R., Bugge A., Moller N.C., Anderson L.B. Physical activity and motor competence present a positive reciprocal longitudinal relationship across childhood and early adolescence. J Phys Act Health. 2017;14:440–447. doi: 10.1123/jpah.2016-0473. [DOI] [PubMed] [Google Scholar]
- 55.Robinson L.E. The relationship between perceived physical competence and fundamental motor skills in preschool children. Child Care Health Dev. 2011;37:589–596. doi: 10.1111/j.1365-2214.2010.01187.x. [DOI] [PubMed] [Google Scholar]
- 56.Barnett L., Hinkley T., Okely A.D., Salmon J. Child, family, and environmental correlates of children's motor skill proficiency. J Sci Med Sport. 2013;16:332–336. doi: 10.1016/j.jsams.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 57.Azevedo L.B., van Sluijs E.M.F., Moore H.J., Hesketh K. Determinants of change in accelerometer‐assessed sedentary behaviour in children 0 to 6 years of age: a systematic review. Obes Rev. 2019;20:1441–1464. doi: 10.1111/obr.12882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barnett I., van Sluijs E.M., Ogilvie D. Physical activity and transitioning to retirement: a systematic review. Am J Prev Med. 2012;43:329–336. doi: 10.1016/j.amepre.2012.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Craggs C., Corder K., van Sluijs E.M., Griffin S.J. Determinants of change in physical activity in children and adolescents: a systematic review. Am J Prev Med. 2011;40:645–658. doi: 10.1016/j.amepre.2011.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Waffenschmidt S., Knelangen M., Sieben W., Bühn S., Pieper D. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Methodol. 2019;19:132. doi: 10.1186/s12874-019-0782-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Morgan P.J., Barnett L.M., Cliff D.P., Okely A.D., Scott H.A., Cohen K.E. Fundamental movement skill interventions in youth: a systematic review and meta-analysis. Pediatrics. 2013;132:e1361–e1383. doi: 10.1542/peds.2013-1167. [DOI] [PubMed] [Google Scholar]
- 62.Hollis J.L., Sutherland R., Williams A.J., Campbell E., Nathan N., Wolfenden L. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in secondary school physical education lessons. Int J Behav Nutr Phys Act. 2017;14:52. doi: 10.1186/s12966-017-0504-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sacko R.S., Brazendale K., Brian A., McIver K., Nesbitt D., Pfeifer C. Comparison of indirect calorimetry-and accelerometry-based energy expenditure during object project skill performance. Meas Phys Educ Exerc Sci. 2019;23:148–158. doi: 10.1080/02701367.2019.1642440. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.