Abstract
Objectives
To evaluate the frequency and consequences of prescribing corticosteroids for pneumonia in a biomarker-concordant manner.
Patients and Methods
This was a single-center retrospective cohort study of adults with pneumonia admitted to the medical intensive care unit (ICU) at Mayo Clinic in Rochester, Minnesota, between January 1, 2009, and June 30, 2014. Steroid use was “biomarker concordant” if given when C-reactive protein (CRP) was ≥150 mg/L or withheld when CRP was <150 mg/L, and vice versa for biomarker discordant.
Results
Of 3481 ICU admissions with community-acquired pneumonia, 169 (4.9%) had CRPs measured within 48 hours of admission to the ICU. Steroid use in the ICU was biomarker concordant in 88 (52%) patients and biomarker discordant in 81 (48%) patients. Biomarker-concordant steroid use was associated with faster resolution of lung injury: median fraction of inspired oxygen on day 3 (0.4 [0.3, 0.5] vs 0.3 [0.21, 0.4], P=.005), day 4 (0.35 [0.3, 0.5] vs 0.28 [0.21, 0.38], P=<.001), and day 5 (0.30 [0.24, 0.45] vs 0.28 [0.21, 0.40], P=.03), and increased ICU (3.5; 95% CI, 0.5 to 6.4, P=.02), and hospital-free days (3.6; 95% CI, 0.4 to 6.8, P=.03) on multivariate analysis.
Conclusions
In critically ill patients with community-acquired pneumonia, steroid use is rarely biomarker informed and often discordant with inflammatory biomarker levels. Biomarker-concordant steroid use was associated with a faster recovery of hypoxemia and increased ICU- and hospital-free days. Future well-designed prospective studies are justified to test the potential value of biomarker-concordant steroid therapy.
Abbreviations and Acronyms: APACHE-III, Acute Physiology and Chronic Health Evaluation-III; CAP, community-acquired pneumonia; CRP, C-reactive protein; ICU, intensive care unit; FiO2, fraction of inspired oxygen
Pneumonia is a leading cause of hypoxemic respiratory failure in the intensive care unit (ICU) and is associated with increased hospital length of stay and mortality.1, 2, 3 Despite improvements in outcomes with early antimicrobial treatment and lung-protective mechanical ventilation strategies, the clinical consequences of pneumonia remains substantial.2
The role of adjunctive corticosteroid therapy has been established for infectious conditions such as Streptococcal spp. bacterial meningitis and Pneumocystis jirovecci pneumonia,4 in which excessive inflammation is a hallmark pathologic feature. Although inflammation is recognized as a core pathologic feature of pneumonia,5 our understanding of who benefits from adjunctive corticosteroid therapy remains limited, and the routine use of corticosteroids in this setting remains controversial.6,7
Recent meta-analyses have suggested that adjunctive corticosteroid use may reduce mortality, need for mechanical ventilation, and length of hospital stay.8, 9, 10, 11, 12 In a randomized trial of patients receiving adjuvant steroids for community-acquired pneumonia (CAP), administration of methylprednisolone reduced treatment failure (defined as a composite outcome of clinical deterioration, worsening respiratory failure, and radiographic progression) in those patients with C-reactive protein (CRP) levels >150 mg/L.13 Based on these and other such findings, recent Society of Critical Care Medicine (SCCM)/European Society of Intensive Care Medicine (ESICM) guidelines tentatively recommended adjunctive steroids in patients with CAP,6 However, equipoise remains, and guidelines published by the American Thoracic Society (ATS)/Infectious Disease Society (IDSA) recommends against routine use of corticosteroids.7 Importantly, the widespread acceptance of adjunctive steroids has been limited because of the relatively modest benefit seen with steroid use in clinical studies and methodological concerns about the underlying evidence.
A major barrier to the more precise and informed use of corticosteroids in both clinical practice and trials in patients with pneumonia is the inability to identify patients most likely to benefit from adjunctive anti-inflammatory treatment. To better understand the role of corticosteroid prescribing in pneumonia, we sought to evaluate the frequency and consequences of prescribing corticosteroids for pneumonia in a biomarker-concordant manner (used when CRP is elevated, not used when CRP is low) vs a biomarker-discordant manner (not used when CRP is elevated, used when CRP is low).
Materials and Methods
Design and Subjects
This was a single-center retrospective cohort study of adults (≥18 years of age) with pneumonia admitted to the medical ICU at Mayo Clinic in Rochester, Minnesota, between January 1, 2009, and June 30, 2014. Subjects were included if they had CRP measured within 48 hours of hospital admission based on the physician’s discretion (not used to explicitly inform steroid dosing). Patients who denied the use of their medical records for research purposes were excluded (0.5%). Mayo Clinic Institutional Review Board (IRB) approved this study before its initiation. The Strengthening the Reporting of Observational Studies in Epidemiology guidelines were followed in the design and reporting of this observational study.14
Data: Sources and Definitions
Data were extracted using customized, integrative relational research databases that contain a near real-time copy of clinical, administrative and environmental exposure data from the electronic medical record (the ICU Datamart and the OR Datamart). Manual chart review supplemented all electronic data retrieval. These retrieval strategies have been used and validated in previous studies by our group.15,16 Severity of illness was measured using Acute Physiology and Chronic Health Evaluation-III (APACHE-III ) and sequential organ failure assessment (SOFA) scores at admission.
Pneumonia was defined as an acute infection of the pulmonary parenchyma associated with 1 or more signs or symptoms of acute infection, accompanied by the presence of an acute infiltrate on a chest radiograph or auscultatory findings consistent with pneumonia.17 This was identified on admission by the International Classification of Diseases, 9th Edition (ICD 9), codes 481-486, and further verified by a clinical note search and manual chart review.
Predictor Variable: Biomarker Concordance
Steroid use was defined as either biomarker concordant: steroids given when CRP level is ≥150 mg/L or withheld when CRP level is <150 mg/L, or biomarker-discordant: steroids given when CRP level is <150 mg/L or withheld when CRP level is ≥150 mg/L.
Outcomes
The primary effectiveness outcome was evolution of respiratory failure measured by fraction of inspired oxygen (FiO2) at time of admission to the ICU, after 24 hours, after 48 hours, after 72 hours, after 96 hours, and after 120 hours (effectiveness). The primary safety outcome was possible adverse effects of steroid including hyperglycemia (random blood glucose ≥180 mg/dL) and delirium (measured by confusion-assessment method for the ICU [CAM-ICU]+). Secondary outcomes included hospital-free days and ICU-free days at day 28, defined as the days the patient was alive outside the hospital, from admission to 28 days, as well as in-hospital and ICU mortality.
Statistical Analysis
Continuous data are presented as median (interquartile range [IQR]), and categorical data are presented as counts (percentages). Wilcoxon rank sum, χ2, and Fisher exact tests were used to evaluate univariate continuous and categorical outcomes across concordant status. Associations between the primary outcome of ICU and hospital-free days—defined as the number of days the patient was alive outside the ICU or hospital within the first 28 days of admission to the ICU— and steroid concordance were analyzed using multivariable regression models. The models were adjusted for the effects of CRP level, steroid use, baseline APACHE-III score, and the presence of shock: all chosen a priori. Proportional hazards models were used for the multivariate analysis of hospital and ICU mortality, adjusted for the same covariates listed here. Time was defined as the number of days from ICU admission to the first of death within the ICU or hospital or discharged alive from the ICU or hospital. Statistical analyses were carried out with SAS version 9.4 (SAS Institute Inc., Cary, North Carolina). A 2-sided P value of <0.05 was determined to be significant. For the outcome of daily FiO2 measurements, we considered a P value <0.01 to be significant (0.05/5 using a Bonferonni adjustment for multiple comparisons).
Results
Of 3481 patients with pneumonia admitted to the ICU, 169 (4.9%) had CRP levels measured within 48 hours and were included in the study. The median time from ICU admission to CRP measurement was 3 hours (1.5, 10.7) and the median time from ICU admission to administration of steroids was 5.3 hours (2.6, 15.4), with only 11 (6.5%) patients receiving steroids before measurement of CRP levels (Supplemental Table 1, available online at http://www.mcpiqojournal.org). Steroid use in the ICU was concordant with biomarker level in 88 (52%) patients and discordant with biomarker level in 81 (48%) patients, and respectively (Figure).
Figure.
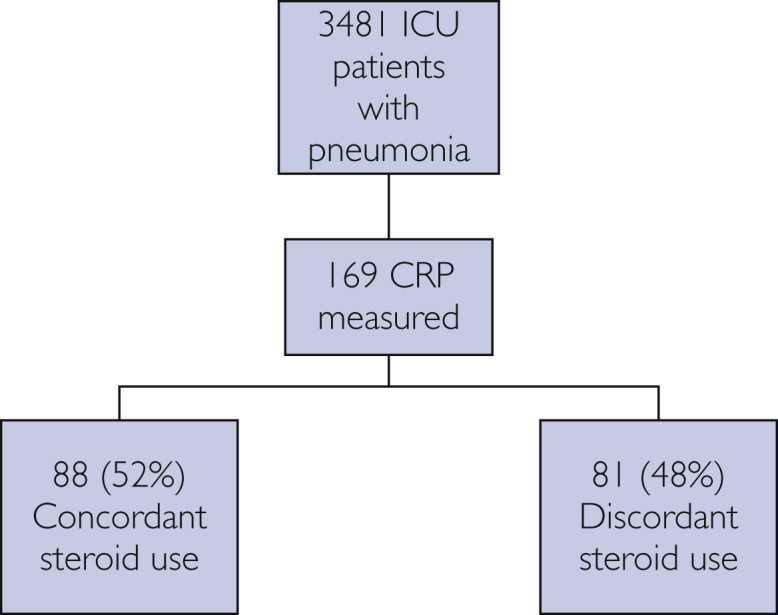
Study flow diagram. CRP = C-reactive protein; ICU = intensive care unit.
Baseline characteristics are shown in Table 1. Groups were similar, with the exception of a greater proportion of invasive ventilator use in the biomarker-discordant group vs the biomarker-concordant group (55.6% vs 39.8%, P=.04). Invasive ventilator days, noninvasive ventilator use, and noninvasive ventilator days were not significantly different between groups.
Table 1.
Patient Demographics and Clinical Characteristics By Concordance Status
| Characteristic | Discordant N=81 |
Concordant N=88 |
Total N=169 |
P value |
|---|---|---|---|---|
| Baseline demographics | ||||
| Age at ICU admission | 66 (48, 76)c | 64.5 (53.0, 79.5)c | 65 (51, 77)c | .57d |
| Male | 40 (49.4%)b | 47 (53.4%)b | 87 (51.5%)b | .60e |
| Weight (kg) | 80.0 (68.7, 97.8)c | 84.8 (69.8, 100.4)c | 83.9 (69.5, 99.0)c | .39d |
| White race | 70 (86.4%)b | 80 (90.9%)b | 150 (88.8%)b | .36e |
| Baseline APACHE IIIa | 43 (31, 54)c | 46.0 (33.0, 58.5)c | 44 (32, 55)c | .53d |
| SOFA at ICU admissiona | 6 (4, 8)c | 6 (3, 8)c | 6 (3, 8)c | .90d |
| Shock | 24 (29.6%)b | 28 (31.8%)b | 52 (30.8%)b | .76e |
| Charlson comorbidity index | 5 (2, 7)c | 5 (3, 9)c | 5 (3, 8)c | .12d |
| COPDa | 15 (18.5%)b | 17 (19.3%)b | 32 (18.9%)b | .89e |
| Asthma | 4 (4.9%)b | 10 (11.4%)b | 14 (8.3%)b | .17e |
| Ventilator use | ||||
| Invasive ventilator use | 45 (55.6%)b | 35 (39.8%)b | 80 (47.3%)b | .04e |
| Invasive ventilator days | 3.4 (0.9, 6.8)c | 3.2 (1.3, 5.0)c | 3.3 (1.1, 6.1)c | .60d |
| Noninvasive ventilator use | 35 (43.2%)b | 29 (33.0%)b | 64 (37.9%)b | .17e |
| Noninvasive ventilator days | 0.6 (0.2, 1.6)c | 0.7 (0.3, 1.6)c | 0.6 (0.2, 1.6)c | .78d |
| Both invasive and noninvasive vent | 19 (23.5%)b | 12 (13.6%)b | 31 (18.3%)b | .10e |
| Both invasive and noninvasive vent days | 0.2 (0.1, 1.0)c | 0.5 (0.2, 1.5)c | 0.3 (0.1, 1.2)c | .18d |
| Baseline measures | ||||
| Fi02 at ICU admissiona | 0.5 (0.4, 0.6)c | 0.4 (0.4, 0.6)c | 0.45 (0.4, 0.6)c | .57d |
| P02/Fi02 at ICU admissiona | 171.7 (130.0, 247.5)c | 209.6 (123.6, 300.5)c | 180 (130, 262)c | .24d |
| Sp02/Fi02 at ICU admissiona | 192.0 (156.7, 237.5)c | 204.1 (164.2, 248.8)c | 196.0 (158.3, 240.0)c | .16d |
| Delirium | 27 (33.3%)b | 23 (26.1%)b | 50 (29.6%)b | .31e |
| Hyperglycemia at ICU admission (glucose ≥180) | 18 (22.5%)b | 23 (26.7%)b | 41 (24.7%)b | .53e |
| Hyperglycemia after steroid | 20 (24.7%)b | 16 (18.2%)b | 36 (21.3%)b | .30e |
| FiO2 at ICU Admissiona | .45 (.32, .6)c | .36 (.28, .6)c | .4 (.3, .6)c | .16d |
| FiO2 Day 2a | .4 (.31, .5)c | .31 (.28, .5)c | .4 (.28, .5)c | .10d |
| FiO2 Day 3a | .4 (.3, .5)c | .3 (.21, .4)c | .35 (.28, .5)c | .005d |
| FiO2 Day 4a | .35 (.3, .5)c | .28 (.21, .38)c | .32 (.21, .4)c | <.001d |
| FiO2 Day 5a | .3 (.24, .45)c | .28 (.21, .4)c | .28 (.21, .4)c | .03d |
APACHE, Acute Physiology and Chronic Health Evaluation III; COPD, chronic obstructive pulmonary disease; FiO2, fraction of inspired oxygen; ICU, intensive care unit; PaO2, partial pressure of oxygen in arterial blood; SOFA, sequential organ failure; SpO2, oxygen saturation.
Numbers indicate N (%) unless otherwise noted.
Median (Q1, Q3).
Wilcoxon.
χ2.
Although there was no observed difference in mean FiO2, partial pressure of oxygen (PaO2)/FiO2, and oxygen saturation (SpO2)/FiO2 at admission to the ICU, resolution of lung injury was faster in the biomarker-concordant group. A significant difference was noted in the median FiO2 on day 3 (0.4 [0.3, 0.5] vs 0.3 [0.21, 0.4], P=.005), day 4 (0.35 [0.3, 0.5] vs 0.28 [0.21, 0.38], P=<.001) and day 5 (0.30 [0.24, 0.45] vs 0.28 [0.21, 0.40], P=.03) in favor of the concordant group (although the day 5 comparison was not significant after adjustment for multiple comparisons). The prevalence of hyperglycemia and delirium were also not different between groups.
Associations between concordance status and the secondary outcomes are provided in Table 2. Concordant patients had significantly more ICU free days (mean estimate=3.45; 95% confidence interval [CI], 0.52 to 6.38; P=0.02) and hospital-free days (mean estimate=3.58; 95% CI, 0.40 to 6.77; P=.03) when compared with discordant patients. Unsurprisingly, higher APACHE and presence of shock were significantly associated with decreased ICU- and hospital-free days.
Table 2.
Associations Between Concordance and ICU and Hospital-Free Days and ICU and Hospital Mortality Using Multivariable Linear Regression and Proportional Hazards Regression Models
| Outcome | Summary | Estimate | P value |
|---|---|---|---|
| ICU-free days | Mean (SD) | Mean estimate (95% CI) | P value |
| Concordance status | .02 | ||
| Discordant | 19.6 (10.1) | .00 (ref) | |
| Concordant | 22.2 (8.3) | 3.45 (.52, 6.38) | |
| CRP level | .03 | ||
| Low (<50) | 21.3 (9.5) | .00 (ref) | |
| Middle (50-149) | 19.5 (10.2) | –1.58 (–4.65, 1.49) | |
| High (150+) | 22.3 (7.5) | 2.91 (–.51, 6.33) | |
| Steroids | .20 | ||
| None | 22.7 (7.7) | .00 (ref) | |
| <.5 mg/kg per day | 18.7 (10.7) | –3.57 (–8.28, 1.14) | |
| ≥.5 mg/kg per day | 18.8 (10.6) | –2.04 (–5.05, .98) | |
| Baseline APACHE-III | .002 | ||
| Ordinal effect | 21.0 (9.2) | –.10 (–.17, –.04) | |
| Shock | .02 | ||
| No | 22.5 (8.1) | .00 (ref) | |
| Yes | 17.5 (10.7) | –3.55 (–6.47, –.63) | |
| Hospital-free days | Mean (SD) | Mean estimate (95% CI) | P value |
| Concordance status | .03 | ||
| Discordant | 12.0 (9.8) | .00 (ref) | |
| Concordant | 14.8 (9.8) | 3.58 (.40, 6.77) | |
| CRP level | .16 | ||
| Low (<50) | 15.0 (10.0) | .00 (ref) | |
| Middle (50-149) | 12.1 (10.2) | –2.53 (–5.88, .82) | |
| High (150+) | 13.4 (9.3) | 0.68 (–3.04, 4.41) | |
| Steroids | .57 | ||
| None | 14.5 (9.6) | .00 (ref) | |
| <.5 mg/kg per day | 11.4 (9.9) | –2.74 (–7.87, 2.39) | |
| ≥.5 mg/kg per day | 12.2 (10.3) | –.60 (–3.88, 2.67) | |
| Baseline APACHE-III | .006 | ||
| Ordinal effect | 13.4 (9.9) | –.10 (–.17, –.03) | |
| Shock | .009 | ||
| No | 15.1 (9.6) | .00 (ref) | |
| Yes | 9.6 (9.6) | –4.21 (–7.36, –1.06) | |
| ICU mortality | N deaths (%) | Hazard ratio (95% CI) | P value |
| Concordance status | .36 | ||
| Discordant | 13 (16.0%) | 1.00 (ref) | |
| Concordant | 5 (5.7%) | .53 (.14, 2.04) | |
| CRP level | .77 | ||
| Low (<50) | 7 (13.0%) | 1.00 (ref) | |
| Middle (50-149) | 7 (11.3%) | 1.34 (.40, 4.53) | |
| High (150+) | 4 (7.5%) | 0.82 (.17, 3.97) | |
| Steroids | .58 | ||
| None | 5 (5.3%) | 1.00 (ref) | |
| <0.5 mg/kg per day | 2 (14.3%) | 0.46 (.07, 3.18) | |
| ≥0.5 mg/kg per day | 11 (18.0%) | 1.28 (.30, 5.55) | |
| Baseline APACHE-III | .01 | ||
| Ordinal effect | 18 (10.7%) | 1.02 (1.01, 1.05) | |
| Shock | .15 | ||
| No | 8 (6.8%) | 1.00 (ref) | |
| Yes | 10 (19.2%) | 2.24 (.75, 6.70) | |
| Hospital mortality | N deaths (%) | Hazard ratio (95% CI) | P value |
| Concordance status | .09 | ||
| Discordant | 21 (25.9%) | 1.00 (ref) | |
| Concordant | 12 (13.6%) | 0.48 (0.21, 1.13) | |
| CRP level | .07 | ||
| Low (<50) | 9 (16.7%) | 1.00 (ref) | |
| Middle (50-149) | 16 (25.8%) | 1.76 (.71, 4.39) | |
| High (150+) | 8 (15.1%) | 0.61 (.21, 1.78) | |
| Steroids | .14 | ||
| None | 11 (11.7%) | 1.00 (ref) | |
| <0.5 mg/kg per day | 2 (14.3%) | 0.73 (.15, 3.45) | |
| ≥.5 mg/kg per day | 20 (32.8%) | 2.20 (.91, 5.34) | |
| Baseline APACHE-III | .001 | ||
| Ordinal effect | 33 (19.5%) | 1.03 (1.01, 1.04) | |
| Shock | .15 | ||
| No | 16 (13.7%) | 1.00 (ref) | |
| Yes | 17 (32.7%) | 1.73 (.82, 3.64) |
ICU- and hospital-free days were defined as the days the patient was alive outside the hospital minus within 28 days of ICU admission minus 28 days. For example, if the patient was discharged alive from the ICU 5 days after admission to the ICU, the ICU-free days was 23. If the patient died before discharge from the ICU , the ICU-free days was 0.
Time was defined as days from concordance within the hospital to death (event) or discharge (censor) in Cox proportional hazards regression models.The multivariable regression models included all variables listed in the Table.
APACHE = Acute Physiology and Chronic Health Evaluation III; CI = confidence interval; CRP = C-reactive protein; ICU = intensive care unit; SD = standard deviation.
A total of 18 ICU deaths were observed, with 5 in the concordant group (5.7%) and 13 (16.0%) in the discordant group. Concordant patients had a 47% lower rate (HR: 0.53; 95% CI, 0.14 to 2.04; P=.36) of death in the ICU compared with discordant patients, but this comparison did not reach statistical significance. Twelve (13.6%) and 21 (25.9%) concordant and discordant, respectively, patients died within the hospital. Concordant patients had lower rate of death in the hospital (HR: 0.48; 95% CI, 0.21 to 1.13; P=.09) compared with discordant patients, but this comparison did not reach statistical significance. Increased APACHE score was significantly associated with increased rates of ICU and hospital mortality.
Discussion
In this study, we attempted to outline the frequency and consequences of steroid-prescribing practices that are concordant with CRP levels compared with those that are not; CRP was obtained infrequently (<5% of ICU admissions with pneumonia). Steroid-prescribing practices were rarely biomarker informed and often discordant with CRP levels. The frequent discordance allowed us to establish 2 distinct groups—biomarker concordant and biomarker discordant—to test our hypothesis. We found that those patients whose steroid prescribing was biomarker concordant (ie, received steroids for high CRP levels or did not receive steroids when CRP levels were low) exhibited more rapid improvement in hypoxemia and shorter hospital and ICU length of stays than those patients who had biomarker-discordant steroids (ie, received steroids when CRP levels were low or did not receive steroids when CRP levels were high). These findings support further prospective clinical studies to identify patients likely to benefit from adjunctive corticosteroids in CAP.
Pneumonia is the most common cause of hypoxemic respiratory failure in the ICU associated with significant morbidity, mortality, and health care utilization.1,2,18 Despite almost 30 years of randomized clinical trials (RCTs) evaluating the role of steroids in pneumonia, our understanding of who benefits from adjunctive corticosteroids remains limited. Given the low yield of conventional clinical trials conducted in heterogeneous, unselected populations of patients with CAP, there is an urgent need for a predictive enrichment strategy that can best identify those patients who may benefit from adjunctive therapies, such as corticosteroids, and optimal dosing strategies. C-reactive protein is a widely available marker of inflammation with rapid turnaround, making it an attractive predictive enrichment tool.19,20 In addition to providing steroids to patients with CAP most likely to benefit, a biomarker-driven strategy will also reduce unnecessary steroid exposure in patients with hypoinflammatory CAP phenotype. C-reactive protein was recently evaluated in a RCT in which patients with high inflammatory response (pneumonia with an admitting CRP > 150 mg/L) benefitted from administration of modest-dose corticosteroids.13 Broadly, our data support the conclusions from this RCT. In our study, CRP was measured infrequently, which is not surprising, as the study preceded the publication of the Torres et al. RCT13 and the SCCM/ESICM guidelines supporting adjunctive steroid use in selected patients.6
Although recent guidelines support the use of steroids in CAP,6 these guidelines suggest a 1-size-fits-all approach to steroid prescribing in CAP, without regard for patient selection, steroid dosing, and steroid duration. As outlined here, although our data broadly support the use of CRP as a tool to identify those most likely to benefit from adjunctive steroids, future studies could also explore the use of CRP to guide steroid dose and duration. In this scenario, adjunctive steroid therapy would only be initiated for patients with CAP who have a CRP above a certain threshold level; CRP trajectory could be used to inform dose reduction and steroid cessation as CRP improves or dose augmentation in patients failing to respond.
This is the first observational study attempting to compare the effects of a biomarker-concordant vs discordant steroid therapy approach in CAP. We identified a potential predictive enrichment strategy to select patients who may most likely benefit from adjunctive corticosteroid therapy. This study provides key preliminary data to justify the next step in our investigation: the development and use of a biomarker-titrated steroid-dosing algorithm in patients hospitalized with CAP (ClinicalTrials.gov: NCT03852537).
Study Limitations
Our study has several limitations. The results are retrospective, and from a single academic center in which CRP measurements and steroid-prescribing practices in pneumonia are at the discretion of the clinician. This limits the overall generalizability of findings. The retrospective study design also creates selection bias, as the only patients included were those hospitalized with pneumonia with a CRP level measured (not used to explicitly inform steroid dosing). Importantly, only a minority of patients had CRP levels measured (therefore underpowered), and a CRP level >150 mg/L as an arbitrary threshold for hyperinflammatory phenotype was chosen based on a previous study.13 The observed difference in FiO2 requirement between both groups (the equivalent of 1 to 2 liters per minute of supplemental oxygen) may not reflect a clinically meaningful outcome for patients. Misclassification is also an important limitation, as pneumonia was identified by ICD 9 codes without consideration of specific risk factors for hospital-acquired or health care-associated pneumonia. A lack of microbiological data is also an important limitation. As with any retrospective study reliant on review of the medical record, there is a chance of errors with data abstraction, as well as missing data. However, to mitigate this, we used previously validated automated search strategies within our highly granular electronic medical record and supplemented automated data collection with manual chart review. As this study preceded the publication of guidelines supporting a CRP-stratified adjuvant steroid prescribing strategy, only a minority of patients had CRP levels measured. Finally, the presence of potential confounding factors, such as time-to-first antibiotic and previous treatment with corticosteroids, were not considered in this study.
Conclusions
In critically ill patients with CAP, steroid use is rarely biomarker informed and often discordant with inflammatory biomarker levels. Biomarker-concordant steroid use was associated with faster recovery of hypoxemia and increased ICU- and hospital-free days. Future well-designed prospective studies are justified to test the potential value of biomarker-concordant steroid therapy.
Footnotes
Drs Odeyemi and Herasevich are first authors. Drs Odeyemi, Herasevich, Chalmers, Barreto, Frank, Ognjen, and Yadav contributed to the design, data acquisition and analysis; writing of the manuscript; provided intellectual contributions to the content; and made critical revisions. All authors reviewed and approved the final version of the manuscript.
Grant Support: This study was funded by the Mayo Clinic Critical Care Independent Multidisciplinary Program (IMP) research grant (Institutional Departmental Grant), the 2018 Walter and Leonore Annenberg Career Development Award in Pulmonary Medicine, and the 2019 Transplant Scholarly Award (to Dr Yadav).
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at www.mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Restrepo M.I., Mortensen E.M., Velez J.A., Frei C., Anzueto A. A comparative study of community-acquired pneumonia patients admitted to the ward and the ICU. Chest. 2008;133(3):610–617. doi: 10.1378/chest.07-1456. [DOI] [PubMed] [Google Scholar]
- 2.Restrepo M.I., Anzueto A. Severe community-acquired pneumonia. Infect Dis Clin North Am. 2009;23(3):503–520. doi: 10.1016/j.idc.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 3.De Pascale G., Bello G., Tumbarello M., Antonelli M. Severe pneumonia in intensive care: cause, diagnosis, treatment and management: a review of the literature. Curr Opin Pulm Med. 2012;18(3):213–221. doi: 10.1097/MCP.0b013e328351f9bd. [DOI] [PubMed] [Google Scholar]
- 4.Pereira J.M., Lisboa T., Paiva J.A. Adjuvant therapies in critical care: steroids to treat infectious diseases. Intensive Care Med. 2018;44(8):1306–1309. doi: 10.1007/s00134-017-5020-9. [DOI] [PubMed] [Google Scholar]
- 5.Martinez R., Menendez R., Reyes S., et al. Factors associated with inflammatory cytokine patterns in community-acquired pneumonia. Eur Respir J. 2011;37(2):393–399. doi: 10.1183/09031936.00040710. [DOI] [PubMed] [Google Scholar]
- 6.Pastores S.M., Annane D., Rochwerg B. Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (Part II): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Crit Care Med. 2018;46(1):146–148. doi: 10.1097/CCM.0000000000002840. [DOI] [PubMed] [Google Scholar]
- 7.Metlay J.P., Waterer G.W., Long A.C., et al. Diagnosis and treatment of adults with community-acquired pneumonia. an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–e67. doi: 10.1164/rccm.201908-1581ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siemieniuk R.A., Meade M.O., Alonso-Coello P., et al. Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(7):519–528. doi: 10.7326/M15-0715. [DOI] [PubMed] [Google Scholar]
- 9.Horita N., Otsuka T., Haranaga S., et al. Adjunctive systemic corticosteroids for hospitalized community-acquired pneumonia: systematic review and meta-analysis 2015 update. Sci Rep. 2015;5:14061. doi: 10.1038/srep14061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang S., Liu T., Hu Y., et al. Efficacy and safety of glucocorticoids in the treatment of severe community-acquired pneumonia: a meta-analysis. Medicine (Baltimore) 2019;98(26):e16239. doi: 10.1097/MD.0000000000016239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Briel M., Spoorenberg S.M.C., Snijders D., et al. Corticosteroids in patients hospitalized with community-acquired pneumonia: systematic review and individual patient data metaanalysis. Clin Infect Dis. 2018;66(3):346–354. doi: 10.1093/cid/cix801. [DOI] [PubMed] [Google Scholar]
- 12.Chen L.P., Chen J.H., Chen Y., Wu C., Yang X.H. Efficacy and safety of glucocorticoids in the treatment of community-acquired pneumonia: a meta-analysis of randomized controlled trials. World J Emerg Med. 2015;6(3):172–178. doi: 10.5847/wjem.j.1920-8642.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torres A., Sibila O., Ferrer M., et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA. 2015;313(7):677–686. doi: 10.1001/jama.2015.88. [DOI] [PubMed] [Google Scholar]
- 14.Vandenbroucke J.P., von Elm E., Altman D.G., et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007;147(8):W163–W194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 15.Herasevich V., Pickering B.W., Dong Y., Peters S.G., Gajic O. Informatics infrastructure for syndrome surveillance, decision support, reporting, and modeling of critical illness. Mayo Clin Proc. 2010;85(3):247–254. doi: 10.4065/mcp.2009.0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh B., Singh A., Ahmed A., et al. Derivation and validation of automated electronic search strategies to extract Charlson comorbidities from electronic medical records. Mayo Clin Proc. 2012;87(9):817–824. doi: 10.1016/j.mayocp.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandell L.A., Wunderink R.G., Anzueto A., et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tong S., Amand C., Kieffer A., Kyaw M.H. Trends in healthcare utilization and costs associated with pneumonia in the United States during 2008–2014. BMC Health Services Res. 2018;18(1):715. doi: 10.1186/s12913-018-3529-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramírez P., Ferrer M., Martí V., et al. Inflammatory biomarkers and prediction for intensive care unit admission in severe community-acquired pneumonia. Crit Care Med. 2011;39(10):2211–2217. doi: 10.1097/CCM.0b013e3182257445. [DOI] [PubMed] [Google Scholar]
- 20.Menendez R., Martinez R., Reyes S., et al. Biomarkers improve mortality prediction by prognostic scales in community-acquired pneumonia. Thorax. 2009;64(7):587–591. doi: 10.1136/thx.2008.105312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


