Significance
Mortality among young adults (age 25 to 44) is rising due in part to preventable, self-inflicted deaths from suicide, alcohol-related liver disease, and drug overdose. This study finds that a comprehensive childhood intervention (Fast Track) designed to reduce conduct problems in at-risk children also reduces the probability of exhibiting adolescent and young adulthood behaviors that precede these deaths, including suicidal ideation and hazardous drinking as well as opioid use in young adulthood. Intervention-driven improvements in children’s interpersonal, intrapersonal, and academic skills in elementary and middle school partially mediate the direct intervention effect on adolescent and young adult behaviors of despair with a strong indirect pathway through earlier acquisition of interpersonal skills.
Keywords: prevention, suicide, opioids, alcohol misuse
Abstract
How to mitigate the dramatic increase in the number of self-inflicted deaths from suicide, alcohol-related liver disease, and drug overdose among young adults has become a critical public health question. A promising area of study looks at interventions designed to address risk factors for the behaviors that precede these —often denoted—“deaths of despair.” This paper examines whether a childhood intervention can have persistent positive effects by reducing adolescent and young adulthood (age 25) behaviors that precede these deaths, including suicidal ideation, suicide attempts, hazardous drinking, and opioid use. These analyses test the impact and mechanisms of action of Fast Track (FT), a comprehensive childhood intervention designed to decrease aggression and delinquency in at-risk kindergarteners. We find that random assignment to FT significantly decreases the probability of exhibiting any behavior of despair in adolescence and young adulthood. In addition, the intervention decreases the probability of suicidal ideation and hazardous drinking in adolescence and young adulthood as well as opioid use in young adulthood. Additional analyses indicate that FT’s improvements to children’s interpersonal (e.g., prosocial behavior, authority acceptance), intrapersonal (e.g., emotional recognition and regulation, social problem solving), and academic skills in elementary and middle school partially mediate the intervention effect on adolescent and young adult behaviors of despair and self-destruction. FT’s improvements to interpersonal skills emerge as the strongest indirect pathway to reduce these harmful behaviors. This study provides evidence that childhood interventions designed to improve these skills can decrease the behaviors associated with premature mortality.
Premature mortality rates are rising among midlife Americans across racial/ethnic groups (1). Suicide, drug overdoses, and alcohol-related liver disease primarily drive these premature deaths and have been coined “deaths of despair” because they coincide with the decades-long overall economic downturn and its consequences (2). Alarmingly, premature mortality has now also increased among younger Americans aged 25 to 44 (3). Among this age group, suicide has become the second leading cause of death, drug overdoses have risen sharply, and liver disease remains the sixth leading cause of death (4, 5). This premature mortality crisis raises the urgent question of how we can decrease the prevalence of the deadly behaviors driving these self-inflicted causes of death.
To reduce deaths of despair, we must prevent the behaviors that often lead to these deaths. Suicide is typically preceded by suicidal ideation, planning, and attempts (6). Death from alcoholic liver disease is preceded by problematic alcohol consumption, such as binge drinking and excessive weekly drinking (7). Drug overdose deaths are largely driven by nonmedical opioid use (8).
What preventable factors lead to these harmful “behaviors of despair and self-destruction?” Extant research has identified a multitude of causes grouped into four general categories (9–14): genetic/epigenetic, psychopathological, personality traits, and social/environmental. The coining of the premature mortality crisis as deaths of despair implies that despair is a critical precursor. Many of these underlying causes (e.g., genetic predispositions, environmental shocks, and some psychological disorders) are clearly neither the result of despair nor preventable using standard intervention pathways. The literature surrounding deaths of despair suggests, however, that a second set of underlying causes is composed of psychopathological, social, and environmental factors that lead to depression, hopelessness, and poor interpersonal/intrapersonal skills such as impulsivity and underdeveloped coping strategies (15). Prior research has identified these negative emotional states and paucity of critical skill sets as precursors to the behaviors of despair leading to deaths of despair (16–21). Could some of these precursors be addressed in their childhood developmental origins? If so, could premature mortality be prevented in childhood, long before deadly despair and its self-destructive behaviors occur?
Developmental models and empirical evidence have identified child/adolescent conduct problems (e.g., aggression, destructiveness, stealing) as a shared and key pathway to suicidal behavior (22, 23), excessive/hazardous drinking (24, 25), and illicit drug/opioid misuse (26, 27). Thus, reducing conduct problems in childhood could be a key pathway for preventing later behaviors and deaths of despair.
Extant work on this topic is often correlational in nature and not comprehensively focused on the three categories of behaviors of despair. Indeed, the effectiveness of conduct problem interventions on mitigating behaviors of despair has yet to be established. Doing so requires an intervention specifically designed to address child and adolescent conduct problems and also, rich longitudinal follow-up data to assess the intervention’s long-term outcomes. Here, we leverage data from one such intervention, Fast Track (FT) (28). FT was designed to decrease life-course antisocial and delinquent behaviors by improving the emotional awareness and regulation as well as interpersonal skills of children at high risk for aggression by both intervening with the children themselves as well as creating more supportive conditions at home and school. The intervention began when participants were in first grade and continued for 10 y. Longitudinal follow-up has continued since then. Participants are currently reaching their mid- to late thirties, the ages at increased risk for premature mortality from deaths of despair.
Intervention Procedures
The FT intervention took a bioecological approach to addressing childhood risk factors for conduct problems (29) based on previous empirical evidence. The first set, child factors, includes poor executive function, impulsivity, and social–cognitive skills related to effective peer relationships (30). A second set, parenting factors, includes harsh and inconsistent discipline (31), lack of parental monitoring and involvement (32), and aversive parent–child interactions (33). A final set includes struggles to keep up with academic demands (34). With these risk factors in mind, FT targeted children’s intrapersonal, interpersonal, and academic skills and their parents’ parenting skills and behaviors through two intervention phases: elementary (grades 1 to 5) and secondary (grades 6 to 10) school (details are provided in ref. 28).
Evaluations of the program to date show that throughout elementary school, random assignment to FT decreased aggressive and disruptive behaviors at home and school (29, 35–37). The positive impacts from intervention diminished during middle school (38) but reemerged during high school and into adulthood (39–42). The intervention proved effective at reducing conduct problems, including antisocial behavior, juvenile arrests, delinquency, and adult convictions. These results, in conjunction with research connecting conduct problems with the suicide-related behaviors, alcohol misuse, and illicit drug use, suggest that the FT intervention may reduce behaviors of despair.
Research Questions
This paper examines whether FT reduces adolescent and young adult behaviors of despair. Given the importance of conduct problems in the development of these despair behaviors and FT’s significant impact reducing life-course conduct problems, we hypothesize that FT reduces the probability of exhibiting these behaviors, and this impact does not vary by sex or race. This paper also explores whether FT’s impact of these behaviors of despair is mediated by the intervention’s positive impact on interpersonal, intrapersonal, and academic skills in elementary and middle school.
Results
Intervention Effects.
Any behavior of despair.
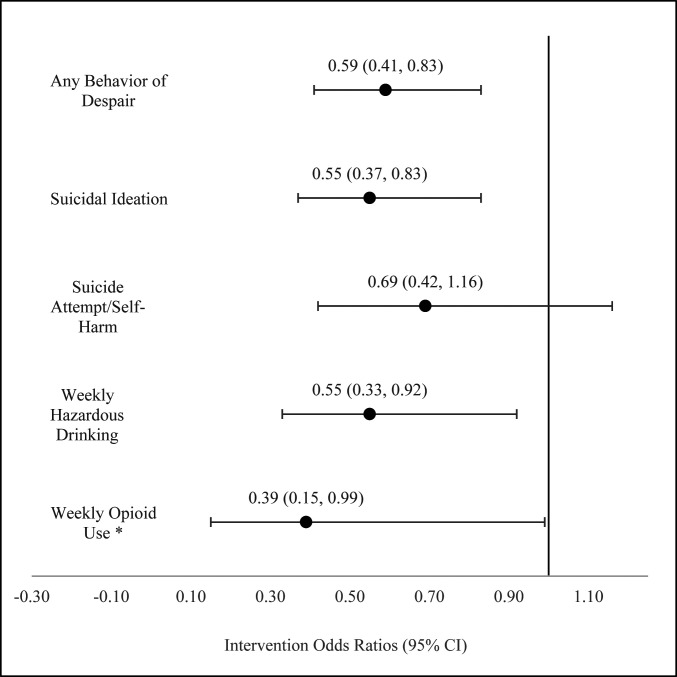
As seen in Fig. 1, 34.3% of the control participants reported a behavior of despair from ages 15 to 25, compared with only 24.6% among intervention participants. Controlling for demographics and other preintervention covariates, random assignment to intervention significantly decreased the probability of exhibiting any behavior of despair from adolescence through young adulthood by 41.5% (Fig. 2) (odds ratio [OR] = 0.585; CI = 0.413, 0.828). SI Appendix provides the complete set of results (SI Appendix, Table S1).
Fig. 1.
Prevalence of behaviors of despair, adolescence through young adulthood (ages 15 to 20 and 25). *Weekly opioid use is based on data collected at ages 19, 20, and 25 only.
Fig. 2.
FT intervention effect on behaviors of despair in adolescence to young adulthood (ages 15 to 20 and 25) from full-information maximum likelihood (FIML) models (n = 891). *Weekly opioid use is based on data collected at ages 19, 20, and 25 only.
Suicidal ideation.
From ages 15 to 25, 24.3% of the control youth reported suicidal ideation, compared with only 16.3% of the intervention youth. Intervention significantly decreased the probability of suicidal ideation by 45.1% (OR = 0.549; CI = 0.365, 0.828).
Suicide attempts and self-harm.
Throughout adolescence and young adulthood, 11.8% of control participants attempted suicide/self-harm in the past 12 mo, whereas only 8.6% of the intervention participants attempted suicide/self-harm. After controlling for covariates, the intervention effect was not statistically significant (OR = 0.693; CI = 0.415, 1.157). Excluding the age 25 data that combine suicide attempts and self-harm yields similar results.
Hazardous drinking.
Among control participants, 14.9% reported hazardous drinking between ages 15 and 25, whereas only 8.9% of intervention youth reported such behavior. Intervention significantly decreased the probability of hazardous drinking by 45.3% (OR = 0.547; CI = 0.327, 0.916).
Opioid use.
During young adulthood (ages 19 to 25), 4.1% of control participants reported weekly use of opioids in the past 12 mo, whereas only 1.7% of intervention participants reported such use. Intervention significantly decreased the probability of opioid use by 61.2% (OR = 0.388; CI = 0.153, 0.982).
Moderation of Intervention Effects by Race and Sex.
There was no evidence of moderation by race across outcomes. In addition, the interaction between intervention and sex was only significant for one of the five outcomes—suicide attempt/self-harm. Among male participants from ages 15 to 25, 11.1% of control participants attempted suicide/self-harm, whereas only 5.1% of the intervention participants attempted suicide/self-harm. Intervention decreased the probability of attempting suicide/self-harm from adolescence through young adulthood among males by 64.2% (OR = 0.358; CI = 0.179, 0.713). Among female participants from age 15 to 25, however, 13.3% of control participants attempted suicide/self-harm, whereas 16.7% of the intervention participants attempted suicide/self-harm. The intervention effect was not significantly significant (OR = 1.612; CI = 0.747, 3.478). SI Appendix provides the complete set of results (SI Appendix, Tables S2 and S3).
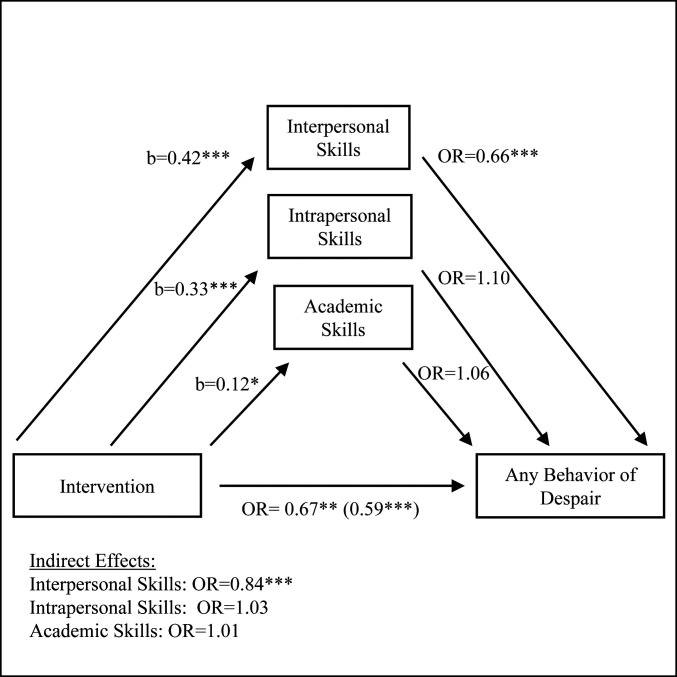
Mediation of Intervention Effects through Elementary and Middle School Skills.
When the potential mediators capturing interpersonal, intrapersonal, and academic skills in elementary and middle school are added to the model estimating any behavior of despair, the magnitude of the intervention effect decreases but remains significant (Fig. 3) (OR = 0.668; CI = 0.436, 0.978). Interpersonal, intrapersonal, and academic skills acquired earlier in life partially mediate the intervention effect by decreasing the direct effect of intervention on the probability of any behavior of despair by 33.2% rather than 41.5% (thus, accounting for 20% of the intervention impact). While intervention increases the level of interpersonal and intrapersonal skills exhibited in elementary and middle school (b = 0.416; CI = 0.278, 0.549 and b = 0.331; CI = 0.214, 0.460, respectively), only interpersonal skills significantly decrease the probability of exhibiting a behavior of despair (OR = 0.656; CI = 0.518, 0.807). Intervention, through increases in interpersonal skills in elementary and middle school, indirectly decreases the probability of exhibiting any behavior of despair in adolescence and young adulthood by 16.1% (OR = 0.839; CI = 0.743, 0.923).
Fig. 3.
Mediation of FT intervention effect on any behavior of despair in adolescence to young adulthood (ages 15 to 20 and 25). The intervention OR in parentheses corresponds to the intervention effect when elementary and middle school skills are not included in the model. *P < 0.10; **P < 0.05; ***P < 0.01.
Elementary and middle school skills partially mediate the direct effect of intervention on suicidal ideation and weekly opioid use as demonstrated by the decrease in the magnitude of the direct effect of intervention after the mediators are added.* Intervention indirectly decreases the probability of suicidal ideation through improvements in interpersonal skills, but this indirect effect is not significant for opioid use. While the direct effect of intervention on suicide attempt/self-harm is not significant in either model, there is evidence that FT’s improvements to interpersonal skills indirectly decreases the probability of suicide attempts/self-harm in adolescence and young adulthood (P < 0.10). For hazardous drinking, there is little evidence that these three types of skills acquired in elementary and middle school mediate the direct effect of intervention, but the indirect effect of intervention through intrapersonal skills increases the probability of hazardous drinking. SI Appendix provides the complete set of results (SI Appendix, Table S4).
Discussion
Deaths of despair and the premature mortality crisis have captured the attention of American society and scientists alike. What are the developmental origins of this crisis? Our study provides causal evidence that mitigating a broad range of intrapersonal, interpersonal, academic, and parenting risk factors for childhood conduct problems in at-risk children reduces behaviors of despair in adolescence and young adulthood. The intervention was particularly effective for reducing suicidal ideation, hazardous drinking, and opioid use. Importantly, the magnitude of positive impact of FT on behaviors of despair (e.g., decreasing suicidal ideation by 45%, hazardous drinking by 46%, and weekly opioid use by 61%) strongly suggests that childhood interventions can be particularly effective at preventing some of the most dangerous precursors to self-inflicted mortality.
Identifying why the FT intervention was so successful at decreasing behaviors of despair is critical to replicating its success with other at-risk populations. First, its efficacy likely stems from the early age at which the intervention began with children at high risk. Recent research has confirmed that childhood intervention not only improved the proximal- and medium-term outcomes for at-risk children but also, has had profound impacts on adult well-being and prevented costly adult outcomes (43–45). Second, the intervention lasted 10 y, which enabled different skills to be addressed at different ages, skill development to be reinforced over time, and fade-out to be avoided. Third, the intervention took a comprehensive/holistic approach, targeting multiple domains of children’s lives: intrapersonal skills (e.g., emotional recognition, emotional regulation, social problem solving); interpersonal skills (e.g., prosocial behavior, improving relationships with peers and adults); academic skills; and parenting skills that govern child and parent communication and parental monitoring. These interventions were not restricted to the children—FT’s innovative design paired direct child and parent instruction with supervised practicing of those newly learned skills between children and parents as well as children and peers.
In addition to the direct effects of the FT intervention, we examine the intermediate pathways by which FT affects behaviors of despair. Previous research demonstrates that the positive impacts of FT on social information processing skills in elementary school partially mediate FT’s direct effect on antisocial behavior in adolescence (46). Similarly, FT’s improvement to childhood interpersonal, intrapersonal, and cognitive competences accounts for significant portions of antisocial, delinquency, and health outcomes in early adulthood (47). This study extends that work by investigating the pathways through which FT affects behaviors of despair. FT’s positive impact on behaviors of despair is partially mediated by the intervention’s improvement to interpersonal, intrapersonal, and academic skills in elementary and middle school. Interpersonal skills emerge as the strongest indirect pathway.
The complex interplay among these competencies is imperfectly understood, but together, the skills learned may strengthen children’s capacity to weather life’s challenges, including those that lead many others in their age group to consider suicide and substance misuse. The strength of our results, both direct and mediated, strongly argues for similarly holistic approaches in future interventions. Future research should use the longitudinal nature of the FT study to further refine our understanding of the dynamics among different pathways over time. Additional research should also explore the more refined components of intrapersonal skills by distinguishing between the different types of social information processing abilities. This research is particularly important for understanding FT’s positive impact on hazardous drinking given that the composite measure of intrapersonal skills analyzed here was unexpectedly associated with an increase in probability of misuse.
These results must be evaluated in light of several limitations. First, although the sample represented both urban and rural populations recruited from low-income and high-crime areas of the country, the sample was not nationally representative. Consequently, we cannot draw conclusions regarding the potential impact of FT on behaviors of despair for the general population. However, we can draw conclusions about its impact on young adults who exhibited high aggressive/delinquent behavior at age 5 and were raised in at-risk communities. Second, the items capturing both suicidal ideation and self-harm/suicide attempts at age 25 are not precisely worded and include ambiguous response options (not true, sometimes true, often true) instead of yes/no responses. Different findings might emerge with different wordings. In addition, this study only examined opioid use rather than capturing nonmedically prescribed use and misuse of prescription drugs more broadly. Finally, the study cannot address other known risk factors associated with these behaviors of despair such as genetic predisposition.
In conclusion, our findings suggest that prevention programs aimed at facilitating the solid acquisition of key social, behavioral, and academic skills in children at risk for conduct problems could be one way to reverse the alarming rise in early and midlife mortality due to deaths of despair. The breadth and magnitude of the positive impacts make a clear case for the value of early holistic, developmentally informed psychological interventions that involve the child, family, and school in mitigating preventable self-inflicted mortality.
Materials and Methods
Participants.
High-risk elementary schools (n = 55) were selected for study participation based on neighborhood crime and poverty rates in four geographic areas: Durham, NC; Nashville, TN; rural Pennsylvania; and Seattle, WA. Within site, schools were matched on demographics and randomly assigned to intervention or control conditions. Three consecutive cohorts (1991 to 1993) of high-risk kindergarten children were identified using a two-step screening procedure (48). First, teachers completed the Authority Acceptance scale of the Teacher Observation of Classroom Adjustment–Revised (49) measure on all kindergarteners (n = 9,594), yielding an aggressive behavior sum score. Then, parents of children scoring in the top 40% within cohort and site were solicited to complete a 22-item instrument based on the Child Behavior Checklist (50) to capture behavior problems at home. Standardized teacher and parent scores were combined to create a severity-of-risk screen score (28).
Children within cohort and site were rank ordered based on this screen score, and study children were recruited starting with the highest risk until designated sample sizes were reached within sites, cohorts, and conditions. Ninety-one percent of recruited families consented, yielding a sample of 891 children, with randomization based on their school (intervention n = 445; control n = 446). In the first year of the study, the average child age was 6.58 y (SD = 0.48). Sixty-nine percent of the sample was male, 51% was Black (47% White and 2% other ethnicity), 58% had single parents, 35% of families were in the lowest socioeconomic (SES) class (51), and 29% of parents had not completed high school. No robust statistically significant differences between the intervention and control samples have been found across variables capturing child behaviors, cognitive and noncognitive attributes, parenting behaviors including warmth and harsh parenting, and family SES (29, 37–39).
The Institutional Review Boards (IRBs) of Duke University, Penn State University, Vanderbilt University, and the University of Washington approved all project procedures. Parents completed written informed consent, and children provided oral assent. Parents (and children after grade 5) were compensated for completing interviews, and parents from the intervention sample received payment for program participation. Initial program participation was extremely high, with 96% of parents and 98% of children attending at least one group session during first grade. Among participating families, 79% of parents and 90% of children completed 50% or more of the group sessions provided. While participation declined over time, due largely to residential moves, at least 80% of youths continued to participate during the adolescent phase of the intervention.
This study includes seven waves of data collection as youths were followed after completing the intervention from ages 15 to 20 and age 25; 78% of living study participants completed at least 50% of the surveys (n = 693). By age 25, 12 intervention and 7 control participants had passed away. Participation did not vary by intervention status (control n = 335; intervention n = 358). Comparing means for interviewed and noninterviewed participants, 3 of the 20 preintervention characteristics (42) differed significantly. Among interviewed participants, the means for the intervention and control groups differed significantly on 4 of the 20 variables. Given the low number of significant differences among these tests, we concluded that attrition did not systematically alter the representativeness of the samples. However, the 20 preintervention variables were included in the statistical models to control for any existing differences.
Measures.
Suicidal ideation and attempts.
Suicidal ideation was captured using a self-reported item indicating whether during the past 12 mo the participant “ever seriously thought about committing suicide.” This item was part of the National Institute of Mental Health Diagnostic Interview Schedule for Children/Young Adults (52) at ages 15, 18, and 20, while at ages 16 and 17, it was part of a suicide module from the National Longitudinal Study of Adolescent and Adult Health (53). At age 25, participants completed the Adult Self Report (ASR) (54), yielding an indicator for suicidal ideation coded as one if the participant reported “I think about killing myself” as sometimes or often true over the past 6 mo. These same measures also contained an item capturing whether the participant attempted suicide in the past 12 mo at each of ages 15 to 20. At age 25, an indicator for self-harm/suicide attempt was created if the participant reported sometimes or often true to the ASR item “I have deliberately tried to hurt or kill myself.”
Hazardous drinking.
Hazardous drinking was defined by the World Health Organization in 1981 as use that “will probably lead to harmful consequences,” where harmful consequences include tissue damage or mental illness (55). Following previous research (56) and using data from the Tobacco, Alcohol, and Drugs (TAD) (57) at ages 15 to 20 and 25, hazardous drinking for men was defined as 21 or more drinks per week or having four or more binge drinking sessions per week. For women, the definition included having 14 or more drinks per week or having four or more binge drinking sessions per week. For both men and women, binge drinking was defined as five or more drinks on a single occasion.
Opioid use.
Participants also reported the frequency (never, less than once a month, one to four times every month, one to six times every week, every day) of opioid use (including methadone, morphine, codeine, Percodan, Darvon, Dilaudid, and Demerol) and Oxycontin in the past year in the TAD at ages 19, 20, and 25. Weekly opioid use was coded one if participants reported using either type of drug weekly over the past year.
Mediators.
Three broad indices of interpersonal, intrapersonal, and academic skills during elementary and middle school were constructed using outcomes from previously published FT intervention research. Outcomes for which intervention significantly improved skills at a minimum of 0.06 significance level were used (29, 35, 37, 38), yielding a set of mediators that overlap closely with previous FT mediation analyses (46, 47). Scales were coded such that higher values indicate greater skill level, and for each set of skills, an average was calculated across the standardized scores. Interpersonal skills included 15 scores: teacher-reported authority acceptance (reverse coded) in grades 1 and 3, parent- and teacher-reported positive child behavior changes in grades 1 and 3, interviewer-rated positive peer interactions in grade 1, peer social preference and peer-nominated prosocial behavior in grade 1, parent report of oppositional and aggressive behavior (reverse coded) in grade 3, indicator for lack of home and community problems and lack of deviant peer problems in grades 4 and 5, self-reported index offenses in grade 7, parent-reported hyperactivity in grade 7, and reverse-coded deviant activity of best friend in grade 8. Intrapersonal skills included seven child-reported scores: competent social problem solving in grades 1 and 3, emotional recognition in grade 1, emotion coping skills in grade 1, reversed-coded endorsement of aggressive retaliation in grade 1, hostile attributions in grade 3, and indicator for lack of social cognition and competence problems in grades 4 and 5. Academic skills included four scores: language arts grades, Spache diagnostic reading subscale, minutes of special education services (reversed) in first grade, and the absence of special education diagnosis in third grade.
Analysis Plan.
For each behavior of despair (suicidal ideation, suicide attempt, hazardous drinking, and weekly opioid use), we created an indicator for ever exhibiting the behavior across all available interview waves from adolescence through young adulthood. We also examined a global indicator capturing any behavior of despair from adolescence through young adulthood (age 15 to 25).
The impact of the FT intervention on behaviors of despair was estimated using full-information maximum likelihood logistic regression models that included covariates for site, cohort, race, sex, and 20 preintervention covariates that have historically been included in intervention analyses (42). SEs were clustered by first-grade school because random assignment into FT intervention was completed at the school level. Additional analyses examined whether intervention varied by sex and race by including the interaction between the indicator for intervention and the potential moderator. Mediation models were constructed by adding the three elementary and middle school skills variables (interpersonal, intrapersonal, and academic) as predictors of the outcome and simultaneously estimating the three skills variables as a function of intervention, site, cohort, race, sex, and the 20 preintervention covariates.
Supplementary Material
Acknowledgments
The members of the Conduct Problems Prevention Research Group (CPPRG) are Karen L. Bierman (Pennsylvania State University); John D. Coie (Duke University); Daniel M. Crowley (Pennsylvania State University); Kenneth A. Dodge (Duke University); Mark T. Greenberg (Pennsylvania State University); John E. Lochman (The University of Alabama); Robert J. McMahon (Simon Fraser University and the B.C. Children’s Hospital Research Institute); and Ellen E. Pinderhughes (Tufts University). The FT project has been supported by National Institute of Mental Health (NIMH) Grants R18 MH48043, R18 MH50951, R18 MH50952, R18 MH50953, K05MH00797, and K05MH01027; National Institute on Drug Abuse (NIDA) Grants DA016903, K05DA15226, RC1DA028248, and P30DA023026; National Institute of Child Health and Human Development Grant R01 HD093651; and Department of Education Grant S184U30002. The Center for Substance Abuse Prevention also provided support through a memorandum of agreement with the NIMH. Additional support for this study was provided by a B. C. Children’s Hospital Research Institute Investigator Grant Award and a Canada Foundation for Innovation award (to Robert J. McMahon). The research reported in this publication was supported by NIMH Grant R01MH117559 and NIDA Grants R01DA036523 and R01DA11301.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
2A complete list of the Conduct Problems Prevention Research Group can be found in the Acknowledgments.
* The mediation model for weekly opioid use did not converge properly likely due to the low prevalence rate of weekly opioid use in the sample and the increased complexity of the model. An alternative model was estimated that excluded all preintervention covariates except the initial screen score. Those results are presented here. SI Appendix provides the FIML results for all models estimating weekly opioid use with the reduced number of covariates (SI Appendix, Table S5). The main effects of intervention and the moderation results are consistent with the fully specified results.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2016234117/-/DCSupplemental.
Contributor Information
Collaborators: Karen L. Bierman, John D. Coie, Daniel M. Crowley, Kenneth A. Dodge, Mark T. Greenberg, John E. Lochman, Robert J. McMahon, and Ellen E. Pinderhughes
Data Availability.
Researchers with IRB-approval can request the Fast Track data and code used in these analyses by submitting a short application (https://fasttrackproject.org/request-use-data.php).
References
- 1.Woolf S. H., et al. , Changes in midlife death rates across racial and ethnic groups in the United States: Systematic analysis of vital statistics. BMJ 362, k3096 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Case A., Deaton A., Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U.S.A. 112, 15078–15083 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curtin S. C., Arias E., “Mortality trends by race and ethnicity among adults aged 25 and over, 2000–2017” (NCHS Data Brief 342, National Center for Health Statistics, Hyattsville, MD, 2019). [PubMed] [Google Scholar]
- 4.NCHS , 2018 Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Web-Based Injury Statistics Query and Reporting System (WISQARS) (2020). https://www.cdc.gov/injury/wisqars/. Accessed 20 May 2020.
- 5.Hedegaard H., Miniño A. M., Warner M., “Drug overdose deaths in the United States, 1999–2017” (NCHS Data Brief 329, National Center for Health Statistics, Hyattsville, MD, 2018). [Google Scholar]
- 6.Cooper J., et al. , Suicide after deliberate self-harm: A 4-year cohort study. Am. J. Psychiatry 162, 297–303 (2005). [DOI] [PubMed] [Google Scholar]
- 7.Stahre M., Roeber J., Kanny D., Brewer R. D., Zhang X., Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev. Chronic Dis. 11, E109 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohnert A. S. B., et al. , Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 305, 1315–1321 (2011). [DOI] [PubMed] [Google Scholar]
- 9.Maciejewski D. F., et al. , Overlapping genetic and environmental influences on nonsuicidal self-injury and suicidal ideation: Different outcomes, same etiology? JAMA Psychiatry 71, 699–705 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heath A. C., et al. , Genetic and environmental contributions to alcohol dependence risk in a national twin sample: Consistency of findings in women and men. Psychol. Med. 27, 1381–1396 (1997). [DOI] [PubMed] [Google Scholar]
- 11.Wang J. C., Kapoor M., Goate A. M., The genetics of substance dependence. Annu. Rev. Genomics Hum. Genet. 13, 241–261 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bridge J. A., Goldstein T. R., Brent D. A., Adolescent suicide and suicidal behavior. J. Child Psychol. Psychiatry 47, 372–394 (2006). [DOI] [PubMed] [Google Scholar]
- 13.Whelan R. et al.; IMAGEN Consortium , Neuropsychosocial profiles of current and future adolescent alcohol misusers. Nature 512, 185–189 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cragg A., et al. , Risk factors for misuse of prescribed opioids: A systematic review and meta-analysis. Ann. Emerg. Med. 74, 634–646 (2019). [DOI] [PubMed] [Google Scholar]
- 15.Shanahan L., et al. , Does despair really kill? A roadmap for an evidence-based answer. Am. J. Public Health 109, 854–858 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kashden J., Fremouw W. J., Callahan T. S., Franzen M. D., Impulsivity in suicidal and nonsuicidal adolescents. J. Abnorm. Child Psychol. 21, 339–353 (1993). [DOI] [PubMed] [Google Scholar]
- 17.Moeller F., Dougherty D., Impulsivity and substance abuse: What is the connection? Addict. Disord. Their Treat. 1, 3–10 (2002). [Google Scholar]
- 18.Horwitz A. G., Hill R. M., King C. A., Specific coping behaviors in relation to adolescent depression and suicidal ideation. J. Adolesc. 34, 1077–1085 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner E. F., Myers M. G., McIninch J. L., Stress-coping and temptation-coping as predictors of adolescent substance use. Addict. Behav. 24, 769–779 (1999). [DOI] [PubMed] [Google Scholar]
- 20.Brown G. K., Beck A. T., Steer R. A., Grisham J. R., Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. J. Consult. Clin. Psychol. 68, 371–377 (2000). [PubMed] [Google Scholar]
- 21.Krank M., et al. , Structural, concurrent, and predictive validity of the substance use risk profile scale in early adolescence. Addict. Behav. 36, 37–46 (2011). [DOI] [PubMed] [Google Scholar]
- 22.Capaldi D., Co-occurrence of conduct problems and depressive symptoms in early adolescent boys. II. A 2-year follow-up at grade 8. Dev. Psychopathol. 4, 125–144 (1992). [DOI] [PubMed] [Google Scholar]
- 23.Thompson M. P., Ho C. H., Kingree J. B., Prospective associations between delinquency and suicidal behaviors in a nationally representative sample. J. Adolesc. Health 40, 232–237 (2007). [DOI] [PubMed] [Google Scholar]
- 24.Kosterman R., et al. , Young adult social development as a mediator of alcohol use disorder symptoms from age 21 to 30. Psychol. Addict. Behav. 28, 348–358 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lynskey M. T., Fergusson D. M., Childhood conduct problems, attention deficit behaviors, and adolescent alcohol, tobacco, and illicit drug use. J. Abnorm. Child Psychol. 23, 281–302 (1995). [DOI] [PubMed] [Google Scholar]
- 26.Dodge K. A., et al. , A dynamic cascade model of the development of substance-use onset. Monogr. Soc. Res. Child Dev. 74, vii-119 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Capaldi D. M., Kerr D. C. R., Tiberio S. S., Owen L. D., Men’s misuse of prescription opioids from early to middle adulthood: An examination of developmental and concurrent prediction models. J. Consult. Clin. Psychol. 87, 893–903 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Conduct Problems Prevention Research Group , The Fast Track Program for Children at Risk: Preventing Antisocial Behavior (Guilford, 2019). [Google Scholar]
- 29.Conduct Problems Prevention Research Group , Initial impact of the Fast Track prevention trial for conduct problems. I. The high-risk sample. Conduct problems prevention research group. J. Consult. Clin. Psychol. 67, 631–647 (1999). [PMC free article] [PubMed] [Google Scholar]
- 30.Moffitt T. E., Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychol. Rev. 100, 674–701 (1993). [PubMed] [Google Scholar]
- 31.Patterson G. R., Reid J. B., Dishion T. J., Antisocial Boys (Castalia, 1992). [Google Scholar]
- 32.Chamberlain P., Reid J. B., Ray J., Capaldi D. M., Fisher P., “Parent inadequate discipline (PID)” in DSM–IV Sourcebook, Widiger T. A., Frances A. J., Pincus H. A., First M. B., Ross R., Davis W. W., Eds. (American Psychiatric Association, Washington, DC, ed. 1, 1997), pp. 569–629. [Google Scholar]
- 33.Dodge K. A., Bates J. E., Pettit G. S., Mechanisms in the cycle of violence. Science 250, 1678–1683 (1990). [DOI] [PubMed] [Google Scholar]
- 34.Coie J. D., Dodge K. A., “Aggression and antisocial behavior” in Handbook of Child Psychology: Social, Emotional, and Personality Development, Damon W., Eisenberg N., Eds. (John Wiley & Sons Inc., Hoboken, NJ, 1998), pp. 779–862. [Google Scholar]
- 35.Bierman K., Evaluation of the first 3 years of the Fast Track prevention trial with children at high risk for adolescent conduct problems. J. Abnorm. Child Psychol. 30, 19–35 (2002). [DOI] [PubMed] [Google Scholar]
- 36.Bierman K. L. et al.; Conduct Problems Prevention Research Group , Using the Fast Track randomized prevention trial to test the early-starter model of the development of serious conduct problems. Dev. Psychopathol. 14, 925–943 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bierman K. L. et al.; Conduct Problems Prevention Research Group , The effects of the Fast Track program on serious problem outcomes at the end of elementary school. J. Clin. Child Adolesc. Psychol. 33, 650–661 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Conduct Problems Prevention Research Group , The difficulty of maintaining positive intervention effects: A look at disruptive behavior, deviant peer relations, and social skills during the middle school years. J. Early Adolesc. 30, 593–624 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dodge K. A.; CONDUCT PROBLEMS PREVENTION RESEARCH GROUP , Fast Track randomized controlled trial to prevent externalizing psychiatric disorders: Findings from grades 3 to 9. J. Am. Acad. Child Adolesc. Psychiatry 46, 1250–1262 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Conduct Problems Prevention Research Group , Fast Track intervention effects on youth arrests and delinquency. J. Exp. Criminol. 6, 131–157 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Conduct Problems Prevention Research Group , The effects of the Fast Track preventive intervention on the development of conduct disorder across childhood. Child Dev. 82, 331–345 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dodge K. A. et al.; Conduct Problems Prevention Research Group , Impact of early intervention on psychopathology, crime, and well-being at age 25. Am. J. Psychiatry 172, 59–70 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barnett W. S., Lives in the Balance: Age-27 Benefit-Cost Analysis of the High/Scope Perry Preschool Program (High/Scope Press, 1996). [Google Scholar]
- 44.Heckman J., Policies to foster human capital. Res. Econ. 54, 3–56 (2000). [Google Scholar]
- 45.Reynolds A. J., et al. , Effects of a school-based, early childhood intervention on adult health and well-being: A 19-year follow-up of low-income families. Arch. Pediatr. Adolesc. Med. 161, 730–739 (2007). [DOI] [PubMed] [Google Scholar]
- 46.Dodge K. A., Godwin J.; Conduct Problems Prevention Research Group , Social-information-processing patterns mediate the impact of preventive intervention on adolescent antisocial behavior. Psychol. Sci. 24, 456–465 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sorensen L. C., Dodge K. A.; Conduct Problems Prevention Research Group , How does the Fast Track intervention prevent adverse outcomes in young adulthood? Child Dev. 87, 429–445 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lochman J. E., Screening of child behavior problems for prevention programs at school entry. The Conduct Problems Prevention Research Group. J. Consult. Clin. Psychol. 63, 549–559 (1995). [DOI] [PubMed] [Google Scholar]
- 49.Werthamer-Larsson L., Kellam S., Wheeler L., Effect of first-grade classroom environment on shy behavior, aggressive behavior, and concentration problems. Am. J. Community Psychol. 19, 585–602 (1991). [DOI] [PubMed] [Google Scholar]
- 50.Achenbach T. M., Manual for the Child Behavior Checklist/4-18 and 1991 Profile (University of Vermont, Department of Psychiatry, 1991). [Google Scholar]
- 51.Bierman K., Predictor variables associated with positive Fast Track outcomes at the end of third grade. J. Abnorm. Child Psychol. 30, 37–52 (2002). [PMC free article] [PubMed] [Google Scholar]
- 52.Shaffer D., Fisher P., Lucas C. P., Dulcan M. K., Schwab-Stone M. E., NIMH diagnostic interview Schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 39, 28–38 (2000). [DOI] [PubMed] [Google Scholar]
- 53.Harris K. M., et al. , The National Longitudinal Study of Adolescent to Adult Health: Research Design (2009). https://addhealth.cpc.unc.edu/documentation/study-design/. Accessed 11 November 2019.
- 54.Achenbach T. M., Rescorla L. A., Manual for the ASEBA Adult Forms & Profiles (University of Vermont, Research Center for Children, Youth, & Families, Burlington, VT, 2003). [Google Scholar]
- 55.Edwards G., Arif A., Hadgson R., Nomenclature and classification of drug- and alcohol-related problems: A WHO memorandum. Bull. World Health Organ. 59, 225–242 (1981). [PMC free article] [PubMed] [Google Scholar]
- 56.Reid M. C., Fiellin D. A., O’Connor P. G., Hazardous and harmful alcohol consumption in primary care. Arch. Intern. Med. 159, 1681–1689 (1999). [DOI] [PubMed] [Google Scholar]
- 57.Bureau of Labor Statistics, US Department of Labor , National Longitudinal Survey of Youth 1997 Cohort, 1997-2001 (National Opinion Research Center, the University of Chicago, 2002). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Researchers with IRB-approval can request the Fast Track data and code used in these analyses by submitting a short application (https://fasttrackproject.org/request-use-data.php).