Abstract
This study examined the prevalence of multiple health risk behaviours, the clustering patterns of health risk behaviours, the association between socio-demographic characteristics, psychological distress and clusters and the relationship between number of health risk behaviours and psychological distress among adolescents in Ghana. Participants were senior high school (SHS) students aged 11–19 years who participated in the 2012 Global School-based Students Health Survey (n = 1763). Five health risk behaviours (smoking tobacco, inadequate fruit intake, inadequate vegetable intake, alcohol intake and physical inactivity) were measured. Participants were classified to be at risk if they indicated they smoked tobacco, did not eat fruit ≥ 2 times a day and vegetables ≥ 5 a day, drank alcohol during the past 30 days and did not engage in physical activity for ≥ 60 min per day during the past 7 days. Latent class analysis and latent regression were used to identify the clusters and factors associated with the clusters respectively. Multiple logistic regression was used to determine the relationship between number of health risk behaviours and psychological distress. The prevalence of multiple health risk behaviours (2 or more) was 94.8%. Two clusters emerged: Cluster 1 (“Poor nutrition, inactive, low substance use cluster”; 91%); Cluster 2 (“High Risk Cluster”; 9%). Using cluster 1 as a reference group, adolescents in the 11–15 years category had lower odds of belonging to cluster 2 (OR = 0.21 CI 0.05–0.91, ρ = 0.036) while those experiencing symptoms of depression had higher odds of belonging to cluster 2 (OR = 2.45 CI 1.45–4.14, ρ = 0.001). No significant relationship was found between number of health risk behaviour and psychological distress. Health risk behaviours cluster among adolescents with age and depression associated with the identified clusters. Early interventions that target these clusters are needed at the individual, school and community level to mitigate the burden of non-communicable diseases.
Keywords: Clustering, Multiple health risk behaviours, Psychological distress, Adolescence, Ghana
Highlights
-
•
Prevalence of multiple health risk behaviours among adolescents in Ghana is high.
-
•
Multiple health risk behaviours cluster among adolescents in Ghana.
-
•
Some demographic and psychological factors are associated with clusters among adolescents.
1. Introduction
Non-communicable diseases (NCDs) such as diabetes, stroke, cancer and cardiovascular diseases are the leading cause of death in the world and in Ghana (Loef and Walach, 2012, World Health Organization, 2018). Smoking tobacco, inadequate fruit intake, inadequate vegetable intake, alcohol intake and physical inactivity have consistently been identified as major health risk factors responsible for NCDs and mortality (Liu et al., 2012; Loef & Walach, 2012; Spring, Moller, & Coons, 2012).
Adolescence, a transitional period from childhood to adulthood is a critical period when young people begin to engage in health risk behaviours such as such as smoking tobacco, inadequate fruit consumption, inadequate vegetable consumption, alcohol consumption, and physical inactivity (Matias, Silva, Silva, Mello, & Salmon, 2018; Meader et al., 2016) and experience high level of psychological distress (Patton et al., 2014). According to the biopsychosocial model, biological/physiological factors (i.e. hormones, genetic predisposition, time of puberty and brain maturation), psychological factors (i.e. self-esteem, sensation seeking and affective states) and social/environmental factors (such as influences of peers and parents, influence of mass media and community norms) interact to explain why adolescents engage in health risk behaviours and how these behaviours cluster (Sales & Irwin, 2009, pp. 31–50).
Available data showed that 9.1% of adolescents aged 13–18 years in Ghana smoke tobacco (Doku, Koivusilta, Raisamo, & Rimpela, 2012), 56% and 48% are not meeting the recommended guideline for fruit and vegetable consumption respectively (Doku, Koivusilta, Raisamo, & Rimpela, 2013),12.6% reported drinking alcohol (Oppong Asante & Kugbey, 2019), 75% were physically inactive (Seidu et al., 2020), 16% reported experiencing symptoms of anxiety and 18.4% report experiencing symptoms of depression (Asante, Kugbey, Osafo, Quarshie, & Sarfo, 2017). These health risk behaviours do not only occur in isolation but they also tend to co-occur or cluster with individuals engaging in multiple health risk behaviours simultaneously (Leech & McNaughton, 2014; Meader et al., 2016). The health impact of clustering or co-occurrence of health risk behaviours is higher than the addictive effects of individual health risk behaviours (Kvaavik, Batty, Ursin, Huxley, & Gale, 2010; Nechuta et al., 2010).
Previous studies in developed countries have reported high prevalence of multiple health risk behaviours among adolescents (Boricic, Simic, & Eric, 2015; Dumith, Muniz, Tassitano, Hallal, & Menezes, 2012; Hale & Viner, 2016; Katon et al., 2010; Kipping, Smith, Heron, Hickman, & Campbell, 2015; Pearson, Atkin, Biddle, Gorely, & Edwardson, 2009; Sanchez et al., 2007). For example, a Brazilian study reported that 93.5% of adolescents engage in multiple health risk behaviours (i.e. smoking, inadequate fruit intake, alcohol intake and/or physical inactivity (Dumith et al., 2012), 80% in the United States (Sanchez et al., 2007), 19.3% in Serbia (Boricic et al., 2015) and 83.2% in a Malaysian study (Teh et al., 2019).
Engaging in these health risk behaviours during adolescence are usually carried into adulthood (Kwan, Cairney, Faulkner, & Pullenayegum, 2012) and has impact on health in later life (Liu et al., 2012). In addition to future risk of chronic diseases, engaging in multiple health risk behaviours is associated with psychological distress among adolescents (Arbour-Nicitopoulos, Faulkner, & Irving, 2012). Compared to their peers who do not engage in multiple health risk behaviour or who engage in single health risk behaviours, adolescents who engage in multiple health risk behaviours experience higher levels of depression and anxiety (Bannink, Broeren, Heydelberg, van't Klooster, & Raat, 2015; Yi et al., 2020). This suggest the need for early preventive health interventions that target multiple health risk behaviours and psychological distress instead of interventions that target multiple health risk behaviours or psychological distress seperately.
A systematic review of studies that examined clustering of health risk behaviours among adolescents in developed countries reported a mixed clustering pattern of physical activity and sedentary behaviour and healthy and unhealthy clusters of all three health risk behaviours (i.e. physical activity, sedentary behaviour and diet) (Leech & McNaughton, 2014). Being female, older age and lower socio-economic status (Leech & McNaughton, 2014) were associated with cluster membership. Another systematic review also reported a strong evidence of clustering for risky sexual behaviour and alcohol use, risky sexual behaviour and illicit use of drug and risky sexual behaviour and smoking among young adult population (Meader et al., 2016). Socio-economic status and gender were identified as some factors associated with the clusters in these studies (Meader et al., 2016).
Ghana, a developing country in Sub-Saharan Africa is currently burdened with NCDs which accounted for 43% of all deaths in 2016 and higher projected trends in the coming years (World Health Organization, 2018b). Although health risk behaviors have been studied among adolescents in Ghana, these studies focused on prevalence of single health risk behaviors and its related factors (Doku et al., 2012; Glozah, Oppong Asante, & Kugbey, 2018; Manyanga, El-Sayed, Doku, & Randall, 2014; Oppong Asante & Kugbey, 2019). No study has examined the prevalence of multiple health risk behaviours, the clustering patterns of health risk behaviours and factors associated with the clusters and the relationship between number of health risk behaviours and psychological distress among adolescents in Ghana. Changing a single health risk behaviour is good but the benefit associated with changing multiple health risk behaviours is more beneficial (Prochaska, Nigg, Spring, Velicer, & Prochaska, 2010). It is therefore important to examine the prevalence and clustering patterns of multiple health risk behaviour instead of examining them in isolation. Given that previous studies have reported psychological distress among adolescents in Ghana and how they are associated with health risk behaviours, an exploration of how multiple health risk behaviours are associated with psychological distress is also needed.
The present study aimed to examine the prevalence of five key multiple health risk behaviours (i.e. tobacco smoking, inadequate fruit intake, inadequate vegetable intake, alcohol consumption, and physical inactivity), clustering patterns of these health risk behaviours and whether socio-demographic factors (i.e. age, socio-economic status and sex) and psychological distress (i.e. depression and anxiety) are associated with identified clusters, and the association between number of health risk behaviours and psychological distress among adolescents in Ghana. These health risk behaviours were assessed because they are consistently associated with NCDs and mortality. The findings from this study will guide the development of health preventive interventions that target multiple health risk behaviours and psychological distress concurrently.
2. Methods
2.1. Study design and data
The cross-sectional design was used for this study. Data for this study was obtained from the 2012 Ghana Global School-Based Student Health Survey (GSHS) (World Health Organization, 2014a). GSHS is a school-based survey undertaken by the World Health Organization (WHO) in partnership with the Centre for Disease Control (CDC), Middle Tennessee State University and the Ghana Education Service (GES) (World Health Organization, 2014a). Participants’ health risk behaviours and other health information were collected using a closed ended questionnaire (World Health Organization, 2014b). Ethical approval was obtained from the Ministry of Education and relevant ethics committee. Written or verbal consents was sought from participants who were 18 years and above and for participants below 18 years, their parents or guardians were contacted to seek consent (World Health Organization, 2014b). Assent was obtained from the participants below 18 years before they participated in the study (World Health Organization, 2014b). Participation in this study was voluntary. Participants were assured of anonymity and confidentiality before data was collected. The student response rate for this study was 74% and the school response rate was 96% (World Health Organization, 2014b).
2.1.1. Sampling procedure and sample size
Participants in this study were sampled using a two-stage cluster sampling technique (World Health Organization, 2014b). Stage one involved the selection of schools from the 10 regions of Ghana and stage two involved the selection of schools taking into consideration the number of students enrolled in the school (World Health Organization, 2014b). This was followed by random selection of classes in selected schools. The random selection gave all students an equal chance of being selected to be part of the study. To adjust for non-response and for the different probabilities of selection, probability weighting was applied to each participant's response. In all, 1984 students participated in the survey (World Health Organization, 2014b).
2.2. Measures
2.2.1. Smoking tobacco
To assess participants smoking of tobacco, they were asked: “During the past 30 days, on how many days did you use any tobacco products other than cigarettes such as tawa snuff powder, chewing tobacco, paper rolled tobacco, dip, cigars, or pipe?"(World Health Organization, 2014b). Response options were: 0 days, 1 or 2 days, 3 to 5 days, 6 to 9 days, 10 to 19 days, 20 to 29 days and all 30 days. Responses were dichotomised for the purpose of analysis: those who selected 0 days were coded as 0 and those who selected 1 or 2 days and above were assigned the code 1 (Oppong Asante & Kugbey, 2019). The World Health Organization (WHO) recommends no smoking tobacco to maintain a good health hence all Participants who selected 0 days in response to the question were classified as non-smokers and those who chose 1 or 2 days and above were classified as smokers (World Health Organization, n.d.).
2.2.2. Fruit consumption
Fruit consumption was assessed by asking participants: “During the past 30 days how many times per day did you usually eat fruit such as oranges, pineapple, watermelon, banana, guava, pear, sweet apple, mangoes, or pawpaw?"(World Health Organization, 2014b) Response options varied from: I did not eat fruit during the past 30 days, less than one time per day, 1 time per day, 2 times per day, 3 times per day, 4 times per day, 5 or more times per day (World Health Organization, 2014b). Those who report eating fruits for ≤ 1 time per day were coded as 1 and those who report eating fruits for ≥2 times per day were coded as 0 for the purpose of analysis (Glozah et al., 2018). The World Health Organization recommends eating a minimum of 400 g of fruits per day (World Health Organization, 2005). The number of times in a day participant ate fruit was considered a proxy for the number of servings for fruits. Participants who had eaten fruits at least 2 times per day during the past 30 days were classified as adequate consumers of fruits and those who consumed fruits less than 2 times per day were classified as inadequate consumers of fruits (Teh et al., 2019).
2.2.3. Vegetable consumption
Participants vegetable consumption was assessed by asking them: “During the past 30 days how many times per day did you usually eat vegetables such as kontomire, garden eggs, lettuce, cabbage, okra, alefu, bira, ayoyo, or bean leaves?” Responses options were: I did not eat vegetables during the past 30 days, less than one time per day, 1 time per day, 2 times per day, 3 times per day, 4 times per day, 5 or more times per day (World Health Organization, 2014b). Participants responses were categorized as those who consumed vegetables for ≥ five times daily (coded 0) and those who consumed vegetables < five times a day were coded as 1 (Teh et al., 2019). The World Health Organization recommends eating at least 400 g vegetable each day to stay healthy (World Health Organization, 2005). The number of times participants ate vegetable was considered a proxy for the number of servings for vegetables. Participants who had eaten vegetables at least 5 times per day during the past 30 days were classified as adequate consumers of vegetables and those who consumed vegetables less than 5 times per day were classified as inadequate consumers of vegetables (Teh et al., 2019).
2.2.4. Alcohol consumption
Participants alcohol consumption was measured by asking the question: “During the past 30 days, on how many days did you have at least one drink containing alcohol?” The following response options were provided: 0 days, 1 or 2 days, 3 to 5 days, 6 to 9 days, 10 to 19 days, 20 to 29 days, and all 30 days (World Health Organization, 2014b). For the purpose of analysis, participant's responses were dichotomised as 0 for those who selected 0 days and those who selected 1 day to all 30 days were assigned the code 1 (Dumith et al., 2012). Participants who indicated they drank alcohol for 1 day and above were considered to be at risk because alcohol consumption among adolescents or underage teenagers is considered illegal and has health consequences (World Health Organization, 2019).
2.2.5. Physical activity
To measure respondents physical activity, they were asked: “During the past 7 days, on how many days were you physically active for a total of at least 60 minutes per day?” The following options were provided: 0 days, 1 day, 2 days, 3 days, 4 days, 5 days, 6 days, and 7 days (World Health Organization, 2014b).
Participants not meeting the WHO recommended guideline of ≥ 60 min per day of moderate PA on five or more days a week were categorized as 1 and those meeting the guidelines were categorized as 0 (Glozah et al., 2018; World Health Organization, 2010).
2.2.6. Body mass index (BMI)
Participants were asked to report their height in metres and weight in kg. Participants body mass index was calculated by dividing their weight by height in metres squared. Participants were classified as underweight, over-weight or obese (World Health Organization, 2014b).
2.2.7. Psychological distress
Participants level of psychological distress was measured by asking 2 questions: 1. Feeling worried (Anxiety) - “During the past 12 months how often have you been so worried about something that you could not sleep at night? Response options were: Never, Rarely, Sometimes, Most of the time, Always 2. Feeling lonely (Depression) “During the past 12 months how often have you felt lonely?” Response options were: Never, Rarely, Sometimes, Most of the time, Always (World Health Organization, 2014b). Responses were coded 0 if students selected never, rarely and sometimes and 1 for those who selected most of the time and always for the purpose of analysis (Glozah et al., 2018; Oppong Asante & Kugbey, 2019).
2.2.8. Socio-demographic characteristics
The following socio-demographic characteristics were assessed: age, sex, grade and socio-economic status (World Health Organization, 2014b). Table 1 below has the questions that were used to assess socio-demographic characteristics. Hunger status was used as a substitute measure of socio-economic status (Khan, Uddin, Lee, & Tremblay, 2019) because the GSHS did not directly measure socio-economic status.
Table 1.
Socio-demographic variables assessed.
| Socio-demographic variables | Questions | Recoding for regression analysis |
|---|---|---|
| Age | How old are you? |
|
| Sex | ‘What is your sex?’ |
|
| Socio-Economic Status (SES) | ‘During the past 30 days, how often did you go hungry because there was not enough food in your home?’ |
|
| Class | ‘In what grade are you?’ |
|
| ||
| ||
|
3. Ethical approval
The study was approved by the ethics committee of the Middle Tennessee State University. Ethical policies of the Ghana Education Service regarding the participation of students in research were strictly adhered to. Written permission was obtained from the Ghana Education Service (GES), participating schools, and teachers. Informed consent was obtained from the participants and parental consent was obtained from minors prior to data collection.
4. Statistical analysis
Latent class analysis (LCA) was used to identify clusters of participants with similar profiles of the five health risk behaviours (i.e. smoking tobacco, inadequate fruit intake, inadequate vegetable intake, alcohol consumption and physical inactivity). Each of the five health risk behaviours were coded as 1 indicating presence of risk and 0 indicating absence of risk. We summed them to generate a risk factor index of 0 (no risk factor) to 5 (presence of all risk factors).
LCA is a type of clustering analysis used to identify homogeneous, mutually exclusive classes in a heterogeneous population (Laska, Pasch, Lust, Story, & Ehlinger, 2009). Each latent class is made up of an estimated prevalence and probability of participants in the cluster who has each of the health risk behaviours (Noble et al., 2015). The latent regression model allows covariates to be included and this helps to identify how these covariates are associated with the latent clusters (Linzer & Lewis, 2011).
We used the Goodness of fit and interpretability of the clusters to determine the number of classes (Lanza, Collins, Lemmon, & Schafer, 2007). The LCA model was fit over three classes, the Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC) were generated for each (Lanza et al., 2007). The class with the smallest BIC and AIC was considered a good fit (Lanza et al., 2007). All analysis was performed using STATA 15 (Stata Corporation, College Station, TX, USA). Participants with missing values were not included in the analysis.
5. Results
5.1. Socio-demographic characteristics
A total of 1984 adolescents were recruited to participate in the study. However, 1763 provided complete data for the health risk behaviours in this study and those without complete data (n = 221) were excluded from the analysis. As shown in Table 2 below, A little above half were males (54.2%), majority were in the 16 and above age category (88%) and belonged to the high socio-economic status group (87%).
Table 2.
Socio-demographic characteristics of adolescents.
| Variables | Frequency | Percentage |
|---|---|---|
| Sex | ||
| Male | 955 | 54.2% |
| Female | 808 | 45.2% |
| Grade | ||
| SHS 1 | 524 | 29.7% |
| SHS 2 | 342 | 19.4% |
| SHS 3 | 554 | 31.4% |
| SHS 4 | 343 | 19.5% |
| Age in years | ||
| 11–15 years | 211 | 12% |
| 16 years and above | 1552 | 88% |
| Socio-economic Status | ||
| High | 1533 | 87% |
| Low | 230 | 13% |
SHS: Senior High School.
5.2. Prevalence of Health risk behaviours and psychological distress
Table 3 above is a summary of the prevalence of each of the health risk behaviours and psychological distress. The prevalence of smoking was 6.2%, 94.4% were not eating vegetables for five or more times per day, 78.1% were not eating fruits for two or more times in a day. The prevalence of alcohol consumption was 12.4% and 75.4% did not engage in physical activity for 60 or more minutes per day in the past 7 days. For BMI status, 7.7% and 0.9% were overweight and obese respectively. 18.1% reported they felt lonely for the past 12 months and 15.3% reported they were worried about something and could not sleep at night.
Table 3.
Prevalence of health risk behaviours and psychological distress among adolescents.
| Health Risk factors | Frequency | Percentage |
|---|---|---|
| Smoking | ||
| Yes | 110 | 6.2% |
| No | 1653 | 93.8% |
| Inadequate vegetable Intake | ||
| No | 99 | 5.6% |
| Yes | 1664 | 94.4% |
| Inadequate fruit intake | ||
| No | 386 | 21.9% |
| Yes | 1377 | 78.1% |
| Alcohol use for the past 30 days | ||
| Yes | 219 | 12.4% |
| No | 1544 | 87.6% |
| Physical inactivity | ||
| No | 434 | 24.6% |
| Yes | 1329 | 75.4% |
| Body Max Index (BMI) | ||
| Underweight | 59 | 3.3% |
| Overweight | 136 | 7.7% |
| Obesity | 16 | 0.9% |
| Depression | ||
| Yes | 319 | 18.1% |
| No | 1444 | 81.9% |
| Anxiety | ||
| Yes | 269 | 15.3% |
| No | 1494 | 84.7% |
5.3. Prevalence of multiple health risk behaviours (tobacco smoking, inadequate fruit intake, inadequate vegetable intake, alcohol use, physical activity)
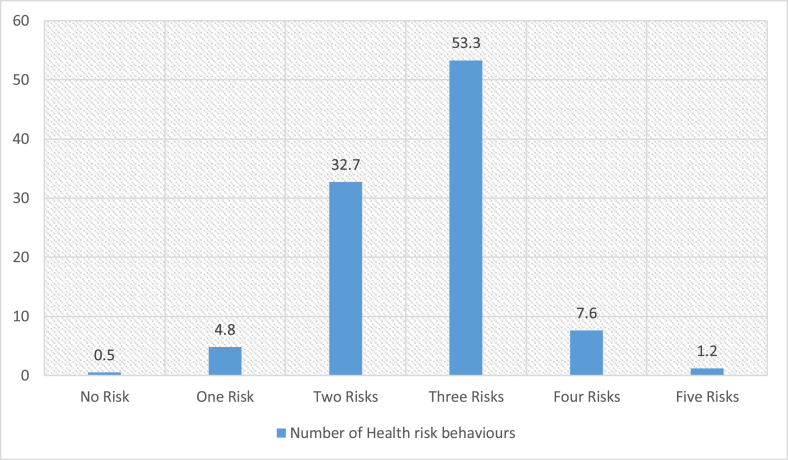
As presented in Fig. 1, 0.5% reported zero risk, 4.8% reported they engaged in one risk, 32.7% reported they engaged in two risks, 53.3% reported they engaged in three risks, 7.6% reported they engaged in four risks, 1.2% reported they engaged in all five risks. The overall prevalence of multiple health risk behaviours (i.e. 2 and more health risk behaviours) was 94.8%
Fig. 1.
Prevalence of multiple health heath risk behaviours.
5. 4. Cluster profiles
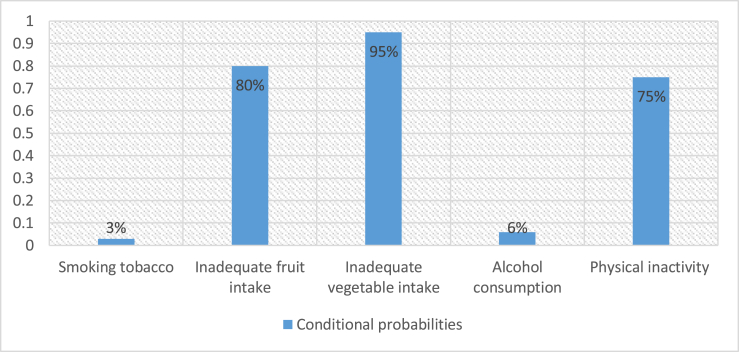
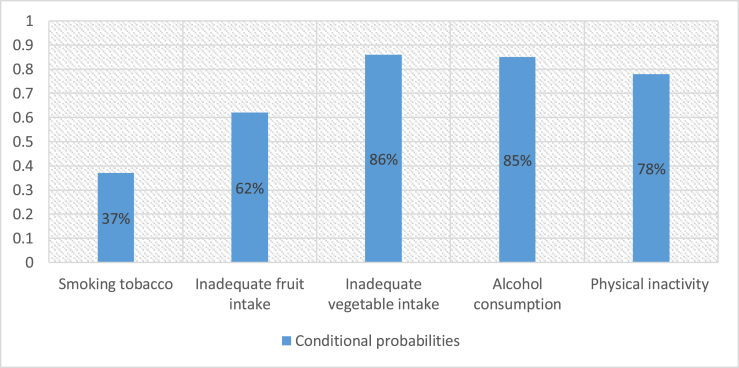
Models with one to three latent classes were fitted without predictor variables. The BIC and AIC of these classes were compared. The result from the Goodness of fit indicated that the 2-class model was the best fit with small AIC (6644.931) and BIC (6705.154). The conditional probabilities of the two clusters are presented in Fig. 2, Fig. 3 below.
Fig. 2.
Conditional probabilities of each health risk behaviour in cluster 1.
Fig. 3.
Conditional probabilities of each health risk behaviour in cluster 2.
Names were given to clusters based the health risk characteristics of each cluster. The two clusters are described as follows:
Cluster 1- “Poor nutrition, inactive, low substance use cluster” (91%): This cluster had the highest prevalence of poor nutrition characterised by inadequate vegetable intake, inadequate fruit intake and high prevalence of physical inactivity. Cluster 1 had the lowest prevalence of students who reported smoking tobacco and drinking alcohol.
Cluster 2- “High risk cluster” (9%): This cluster had the highest probability of students who report smoking tobacco and alcohol consumption compared to cluster 1. This cluster also had high prevalence of inadequate vegetable consumption, inadequate fruit intake and physical inactivity. However, the prevalence of inadequate fruit intake was higher in cluster 1 than this cluster.
5.5. Factors associated with cluster membership
Using cluster 1 as the reference group, the latent regression analysis result in Table 4 showed that adolescents in the 11–15 years category had lower odds of belonging to cluster 2 (OR = 0.21 CI 0.05–0.91, ρ = 0.036), those who reported experiencing a symptom of depression had higher odds of belonging to cluster 2 (OR = 2.45 CI 1.45–4.14, ρ = 0.001).
Table 4.
Odd Ratios, 95% confidence intervals and p-values of predictors of cluster membership.
| Variable |
Cluster 2 |
||
|---|---|---|---|
| AOR | 95% CI | p-value | |
| Sex | |||
| Female | 1 | ||
| Male | 1.27 | 0.74–2.16 | 0.376 |
| Age | |||
| 11–15years | 0.21 | 0.05–0.91 | 0.036 |
| 16 years and above | 1 | ||
| SES | |||
| Low | 1 | ||
| High | 1.20 | 0.58–2.46 | 0.620 |
| Depression | |||
| No | 1 | ||
| Yes | 2.45 | 1.45–4.14 | 0.001 |
| Anxiety | |||
| No | 1 | ||
| Yes | 1.52 | 0.86–2.67 | 0.148 |
Reference cluster = cluster 1; AOR = Adjusted Odd Ratios.
5.6. Relationship between number of health risk behaviours and depression
Table 5 below shows the relationship between number of health risk factors and depression using zero as the reference group. No significant association was found between number of health risk behaviours and depression. However, the adjusted odd ratios indicated that participants who reportedengaging in two or more health risk behaviours had higher odds of experiencing depression.
Table 5.
Logistic regression of number of health risk factors associated with depression.
| Number of Health risk factors | AOR | 95% CI | P-Value |
|---|---|---|---|
| Zero | 1 | ||
| One | 0.84 | 0.09–7.63 | 0.877 |
| Two | 1.42 | 0.17–11.65 | 0.745 |
| Three | 1.60 | 0.20–13.1 | 0.660 |
| Four | 2.20 | 0.26–18.5 | 0.470 |
| Five | 2.06 | 0.20–21.00 | 0.61 |
Reference group = Zero.
5.7. Relationship between number of health risk behaviours and anxiety
Table 6 below shows the relationship between number of health risk behaviours and anxiety using zero as the reference group. No significant association was found between number of health risk behavioursand anxiety. However, the adjusted odd ratios indicated that participants who reported engaging in three or more health risk behaviours had higher odds of experiencing anxiety.
Table 6.
Logistic regression of number of health risk factors associated with anxiety.
| Number of Health risk factors | Odd Ratios | 95% CI | P-Value |
|---|---|---|---|
| Zero | 1 | ||
| One | 1.17 | 0.13–10.35 | 0.890 |
| Two | 0.92 | 0.11–7.61 | 0.939 |
| Three | 1.32 | 0.16–10.81 | 0.796 |
| Four | 2.47 | 0.29–20.83 | 0.404 |
| Five | 2.06 | 0.20–20.96 | 0.542 |
Reference group = Zero.
6. Discussion
This is the first study in Ghana to examine the prevalence of five key multiple health risk behaviours (i.e. smoking tobacco, inadequate fruit intake, inadequate vegetable intake, alcohol consumption and physical inactivity) that are associated with NCDs and risk of mortality, the clustering patterns of these health risk behaviours and their association with socio-demographic characteristics (i.e. sex, age and SES) and psychological distress (i.e. depression and anxiety) and the relationship between number of health risk behaviours and psychological distress (i.e. anxiety and depression). Given that this is the first study in Ghana, a middle-income country in Sub-Saharan Africa, the findings of this study would be compared to similar studies conducted in developed countries. Although some of the findings in our current study are similar to what was reported by previous studies in developed countries, comparison and generalisation should be done bearing in mind the differences in culture norms, climate and other factors between Ghana and these developed countries.
The prevalence of multiple health risk behaviours among adolescents in this study was 94.8%. This is consistent with previous research conducted among adolescents in Malaysia, United States and Brazil which also reported high prevalence of multiple health risk behaviours among adolescents (Dumith et al., 2012; Sanchez et al., 2007; Teh et al., 2019).This finding show that adolescents in Ghana do not just engage in single health risk behaviours and it reinforces the need for interventions that address multiple health risk behaviours.
The present study also found health risk behaviours to cluster among the adolescents. The Latent Class Analysis generated two clusters namely: Cluster 1 (“Poor nutrition, inactive, low substance use cluster”). This is consistent with previous studies conducted in developed countries that reported low prevalence of smoking and alcohol among adolescent but high prevalence of inadequate fruit intake, high inadequate vegetable intake and high physical inactivity (Leech & McNaughton, 2014). Cluster 2 in our study had high prevalence of adolescents who smoke, drink alcohol and are physically inactive. This is also consistent with a previous study conducted among adolescents in Germany where being physically inactive clustered with smoking tobacco and drinking alcohol (Landsberg et al., 2010). Our study also showed that inadequate fruit intake, inadequate vegetable intake clustered with physical inactivity. This is also consistent with previous studies in developed countries that reported clustering of physical inactivity and poor nutrition characterised by inadequate fruit and vegetable intake (Leech & McNaughton, 2014; Loef & Walach, 2012). Given that the health risk behaviours adolescents engage in during adolescence are mostly carried into adulthood, the pattern of clustering identified in this study should inform the design of culturally effective interventions targeting these health risk behaviours concurrently at an early age which can then reduce the risk of non-communicable diseases in adulthood (Patton et al., 2016). All clusters were characterised by high prevalence of inadequate fruit intake, inadequate vegetable intake and physical inactivity. Again, this suggests the need for health interventions that target multiple health risk behaviours simultaneously instead of interventions that target behaviours in isolation (Prochaska et al., 2010). Targeting multiple health risk behaviours simultaneously instead of sequentially is cost-effective and efficient (Prochaska et al., 2010).
For characteristics associated with identified clusters, gender was not significantly associated with cluster 2. This is inconsistent with previous studies among adolescents that reported males to be more likely to belong to high risk clusters. (Dumith et al., 2012; Matias et al., 2018; Silva et al., 2014). However, the odd ratio shows that males were more likely to belong to cluster 2. Differences in characteristics of adolescents in previous studies from ours may explain why gender was not significantly associated with cluster 2. Consistent with previous studies, we found participants who were 16 years and above more likely to belong to the high risk cluster (Alamian and Paradis, 2009; Lawder et al., 2010; Nunes, Goncalves, Vieira, & Silva, 2016; Ottevaere et al., 2011). Adolescents who report experiencing a symptom of depression were also more likely to belong to the high-risk cluster. Again, this is consistent with previous studies that have reported co-occurnece between multiple health risk behaviours and depression among adolescents (Bannink et al., 2015). Past research suggests that poor diet is associated with psychological distress (Nguyen, Ding, & Mihrshahi, 2017), alcohol and drug use is associated with psychological distress (Teesson et al., 2005) and physical inactivity is also associated with poor mental health. Anxiety was not significantly associated with cluster 2 although the odd ratio showed that adolescents who reported they experienced a symptom of anxiety were more likely to belong to cluster 2. This findings reinforces the bidirectional relationship between health risk behaviours and psychological distress reported by a previous study (Schultchen et al., 2019) and calls for the design of health interventions that target health risk behaviours and psychological distress simultaneously. Contrary to previous studies among adolescents (Alamian and Paradis, 2009, Nunes et al., 2016), socio-economic status was not significantly associated with cluster 2 in our study although our analysis suggest that participants from low socio-economic background had higher odds of belonging to the high risk cluster. In this study, hunger status was used as a proxy for socio-economic status and that could be a reason why it was not significantly associated with the high risk cluster. Subsequent studies could use a more comprehensive measure to assess socio-economic status. Overall, these findings show which subgroups among adolescents in Ghana are more likely to engage in multiple health risk behaviours and are more likely to benefit from interventions targeting multiple health risk behaviours.
Contrary to a previous study (Arbour-Nicitopoulos et al., 2012) that found an association between number of health risk behaviours and psychological distress, we did not find a significant relationship between number of health risk behaviours and psychological distress. Although not statistically significant, the odd ratios from our analysis suggest that engaging in multiple health risk behaviours is related to experiencing a symptom of depression and anxiety. Screening for multiple health risk behaviours should also screen for psychological distress and vice versa because it is possible adolescents are engaging in these health behaviours as a coping mechanism for the psychological distress they are experiencing or engaging in these health risk behaviours results in psychological distress.
6.1. Strengths and limitations of the study
The current study has some strengths worth mentioning. Firstly, this is the first study to explore the clustering of health risk behaviours using LCA among adolescents in Ghana with a relatively large sample. Despite these strengths, the findings of this study should be interpreted bearing in mind these limitations. First, the study used a cross sectional design which demonstrates associations at one point in time and not causal links. Secondly, this study used self-report data and it is possible adolescents under or over reported their health risk behaviour. Future studies should consider using objective measures to measure a behaviour such as physical activity. Also, other health risk factors such as insufficient sleep, smoking of cigarettes and excessive screen time which cluster with the health risk behaviours we included in this study and have the potential to confound the clusters identified were not included in this study. These health risk behaviours were not measured by the GSHS team. Future studies should therefore include these health risk behaviours. Finally, although the study recruited large number of schools going adolescents using a sophisticated sampling method, the findings may not be generalizable to other adolescents who do not attend school.
6.2. Conclusion
In conclusion, the study indicated that adolescents engage in multiple health risk behaviours. Interventions targeting health risk behaviours should target multiple health risk behaviours instead of targeting risk behaviours in isolation. The clustering patterns of health risk behaviours and their associations with psychological distress should be taken into consideration when interventions are being designed and developed.
Funding
No funding was obtained for this study.
Availability of data
Data for this study was obtained from the World Health Organization (WHO) website and is freely available online and can be downloaded.
CRediT authorship contribution statement
Prince Atorkey: Conceptualization, Data curation, Methodology, Formal analysis, Writing - review & editing, Writing - original draft. Christiana Owiredua: Writing - original draft, Writing - review & editing.
Declaration of competing interest
None declared.
Acknowledgements
The authors wish to express their gratitude to the World Health Organization (WHO) and its partners for the data collected and for making the data freely available. We also thank the students for their participation in the study. Finally, we thank the teachers and Ghana Education Service (GES) for the assistance provided during the data collection.
References
- Alamian A., Paradis G. Clustering of chronic disease behavioral risk factors in Canadian children and adolescents. Preventive Medicine. 2009;48(5):493–499. doi: 10.1016/j.ypmed.2009.02.015. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19254742. [DOI] [PubMed] [Google Scholar]
- Arbour-Nicitopoulos K.P., Faulkner G.E., Irving H.M. Multiple health-risk behaviour and psychological distress in adolescence. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2012;21(3):171–178. https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/22876262/pdf/?tool=EBI Retrieved from. [PMC free article] [PubMed] [Google Scholar]
- Asante K.O., Kugbey N., Osafo J., Quarshie E.N.-B., Sarfo J.O. The prevalence and correlates of suicidal behaviours (ideation, plan and attempt) among adolescents in senior high schools in Ghana. SSM-population health. 2017;3:427–434. doi: 10.1016/j.ssmph.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bannink R., Broeren S., Heydelberg J., van't Klooster E., Raat H. Depressive symptoms and clustering of risk behaviours among adolescents and young adults attending vocational education: A cross-sectional study. BMC Public Health. 2015;15(396) doi: 10.1186/s12889-015-1692-7. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25896828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boricic K., Simic S., Eric J.M. Demographic and socio-economic factors associated with multiple health risk behaviours among adolescents in Serbia: A cross sectional study. BMC Public Health. 2015;15(157) doi: 10.1186/s12889-015-1509-8. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25884540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doku D., Koivusilta L., Raisamo S., Rimpela A. Tobacco use and exposure to tobacco promoting and restraining factors among adolescents in a developing country. Public Health. 2012;126(8):668–674. doi: 10.1016/j.puhe.2012.05.003. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22800958. [DOI] [PubMed] [Google Scholar]
- Doku D., Koivusilta L., Raisamo S., Rimpela A. Socio-economic differences in adolescents' breakfast eating, fruit and vegetable consumption and physical activity in Ghana. Public Health Nutrition. 2013;16(5):864–872. doi: 10.1017/S136898001100276X. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22030213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumith S.C., Muniz L.C., Tassitano R.M., Hallal P.C., Menezes A.M. Clustering of risk factors for chronic diseases among adolescents from Southern Brazil. Preventive Medicine. 2012;54(6):393–396. doi: 10.1016/j.ypmed.2012.03.014. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22484392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glozah F.N., Oppong Asante K., Kugbey N. Parental involvement could mitigate the effects of physical activity and dietary habits on mental distress in Ghanaian youth. PloS One. 2018;13(5):e0197551. doi: 10.1371/journal.pone.0197551. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29771990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale D.R., Viner R.M. The correlates and course of multiple health risk behaviour in adolescence. BMC Public Health. 2016;16(458) doi: 10.1186/s12889-016-3120-z. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27246600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W., Richardson L., Russo J., McCarty C.A., Rockhill C., McCauley E.…Grossman D.C. Depressive symptoms in adolescence: The association with multiple health risk behaviors. General Hospital Psychiatry. 2010;32(3):233–239. doi: 10.1016/j.genhosppsych.2010.01.008. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/20430225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A., Uddin R., Lee E.-Y., Tremblay M.S. Sitting time among adolescents across 26 asia–pacific countries: A population-based study. International Journal of Public Health. 2019;64(8):1129–1138. doi: 10.1007/s00038-019-01282-5. [DOI] [PubMed] [Google Scholar]
- Kipping R.R., Smith M., Heron J., Hickman M., Campbell R. Multiple risk behaviour in adolescence and socio-economic status: Findings from a UK birth cohort. The European Journal of Public Health. 2015;25(1):44–49. doi: 10.1093/eurpub/cku078. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/24963150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvaavik E., Batty G.D., Ursin G., Huxley R., Gale C.R. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom health and lifestyle survey. Archives of Internal Medicine. 2010;170(8):711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- Kwan M.Y., Cairney J., Faulkner G.E., Pullenayegum E.E. Physical activity and other health-risk behaviors during the transition into early adulthood: A longitudinal cohort study. American Journal of Preventive Medicine. 2012;42(1):14–20. doi: 10.1016/j.amepre.2011.08.026. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22176841. [DOI] [PubMed] [Google Scholar]
- Landsberg B., Plachta-Danielzik S., Lange D., Johannsen M., Seiberl J., Muller M.J. Clustering of lifestyle factors and association with overweight in adolescents of the Kiel Obesity Prevention Study. Public Health Nutrition. 2010;13(10A):1708–1715. doi: 10.1017/S1368980010002260. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/20883570. [DOI] [PubMed] [Google Scholar]
- Lanza S.T., Collins L.M., Lemmon D.R., Schafer J.L. Proc LCA: A SAS procedure for latent class Analysis. Structural Equation Modeling : A Multidisciplinary Journal. 2007;14(4):671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laska M.N., Pasch K.E., Lust K., Story M., Ehlinger E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prevention Science. 2009;10(4):376–386. doi: 10.1007/s11121-009-0140-2. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19499339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawder R., Harding O., Stockton D., Fischbacher C., Brewster D.H., Chalmers J.…Conway D.I. Is the scottish population living dangerously? Prevalence of multiple risk factors: The scottish health survey 2003. BMC Public Health. 2010;10(1):330. doi: 10.1186/1471-2458-10-330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leech R.M., McNaughton S.A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: A review. International Journal of Behavioral Nutrition and Physical Activity. 2014;11(1):1–9. doi: 10.1186/1479-5868-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linzer D.A., Lewis J.B. poLCA: An R package for polytomous variable latent class analysis. Journal of Statistical Software. 2011;42(10):1–29. [Google Scholar]
- Liu K., Daviglus M.L., Loria C.M., Colangelo L.A., Spring B., Moller A.C. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The coronary artery risk development in (young) adults (CARDIA) study. Circulation. 2012;125(8):996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22291127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loef M., Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: A systematic review and meta-analysis. Preventive Medicine. 2012;55(3):163–170. doi: 10.1016/j.ypmed.2012.06.017. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22735042. [DOI] [PubMed] [Google Scholar]
- Manyanga T., El-Sayed H., Doku D.T., Randall J.R. The prevalence of underweight, overweight, obesity and associated risk factors among school-going adolescents in seven African countries. BMC Public Health. 2014;14(887) doi: 10.1186/1471-2458-14-887. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25168589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matias T.S., Silva K.S., Silva J.A.D., Mello G.T., Salmon J. Clustering of diet, physical activity and sedentary behavior among Brazilian adolescents in the national school - based health survey (PeNSE 2015) BMC Public Health. 2018;18(1):1283. doi: 10.1186/s12889-018-6203-1. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/30463537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meader N., King K., Moe-Byrne T., Wright K., Graham H., Petticrew M.…Sowden A.J. A systematic review on the clustering and co-occurrence of multiple risk behaviours. BMC Public Health. 2016;16(657) doi: 10.1186/s12889-016-3373-6. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27473458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nechuta S.J., Shu X.O., Li H.L., Yang G., Xiang Y.B., Cai H.…Zheng W. Combined impact of lifestyle-related factors on total and cause-specific mortality among Chinese women: Prospective cohort study. PLoS Medicine. 2010;7(9) doi: 10.1371/journal.pmed.1000339. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/20856900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen B., Ding D., Mihrshahi S. Fruit and vegetable consumption and psychological distress: Cross-sectional and longitudinal analyses based on a large Australian sample. BMJ Open. 2017;7(3):e014201. doi: 10.1136/bmjopen-2016-014201. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28298322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noble N., Paul C.L., Turner N., Blunden S.V., Oldmeadow C., Turon H.E. A cross-sectional survey and latent class analysis of the prevalence and clustering of health risk factors among people attending an Aboriginal Community Controlled Health Service. BMC Public Health. 2015;15(666) doi: 10.1186/s12889-015-2015-8. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/26173908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes H.E., Goncalves E.C., Vieira J.A., Silva D.A. Clustering of risk factors for non-communicable diseases among adolescents from southern Brazil. PloS One. 2016;11(7):e0159037. doi: 10.1371/journal.pone.0159037. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27434023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppong Asante K., Kugbey N. Alcohol use by school-going adolescents in Ghana: Prevalence and correlates. Mental Health & Prevention. 2019;13:75–81. doi: 10.1016/j.mhp.2019.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottevaere C., Huybrechts I., Benser J., De Bourdeaudhuij I., Cuenca-Garcia M., Dallongeville J.…Group H.S. Clustering patterns of physical activity, sedentary and dietary behavior among European adolescents: The HELENA study. BMC Public Health. 2011;11(328) doi: 10.1186/1471-2458-11-328. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21586158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton G.C., Coffey C., Romaniuk H., Mackinnon A., Carlin J.B., Degenhardt L.…Moran P. The prognosis of common mental disorders in adolescents: A 14-year prospective cohort study. The Lancet. 2014;383(9926):1404–1411. doi: 10.1016/S0140-6736(13)62116-9. [DOI] [PubMed] [Google Scholar]
- Patton G.C., Sawyer S.M., Santelli J.S., Ross D.A., Afifi R., Allen N.B.…Bonell C. Our future: A lancet commission on adolescent health and wellbeing. The Lancet. 2016;387(10036):2423–2478. doi: 10.1016/S0140-6736(16)00579-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson N., Atkin A.J., Biddle S.J., Gorely T., Edwardson C. Patterns of adolescent physical activity and dietary behaviours. International Journal of Behavioral Nutrition and Physical Activity. 2009;6(45) doi: 10.1186/1479-5868-6-45. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19624822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J.J., Nigg C.R., Spring B., Velicer W.F., Prochaska J.O. The benefits and challenges of multiple health behavior change in research and in practice. Preventive Medicine. 2010;50(1–2):26–29. doi: 10.1016/j.ypmed.2009.11.009. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19948184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sales J.M., Irwin C.E., Jr. 2009. Theories of adolescent risk taking: The biopsychosocial model. Adolescent health: Understanding and preventing risk behaviors and adverse health outcomes. [Google Scholar]
- Sanchez A., Norman G.J., Sallis J.F., Calfas K.J., Cella J., Patrick K. Patterns and correlates of physical activity and nutrition behaviors in adolescents. American Journal of Preventive Medicine. 2007;32(2):124–130. doi: 10.1016/j.amepre.2006.10.012. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17197153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultchen D., Reichenberger J., Mittl T., Weh T.R.M., Smyth J.M., Blechert J. Bidirectional relationship of stress and affect with physical activity and healthy eating. British Journal of Health Psychology. 2019;24(2):315–333. doi: 10.1111/bjhp.12355. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/30672069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidu A.A., Ahinkorah B.O., Agbaglo E., Darteh E.K.M., Ameyaw E.K., Budu E. Are senior high school students in Ghana meeting WHO's recommended level of physical activity? Evidence from the 2012 global school-based student health survey data. PloS One. 2020;15(2):e0229012. doi: 10.1371/journal.pone.0229012. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/32050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva K.S., Barbosa Filho V.C., Del Duca G.F., de Anselmo Peres M.A., Mota J., Lopes Ada S. Gender differences in the clustering patterns of risk behaviours associated with non-communicable diseases in Brazilian adolescents. Preventive Medicine. 2014;65:77–81. doi: 10.1016/j.ypmed.2014.04.024. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/24814216. [DOI] [PubMed] [Google Scholar]
- Spring B., Moller A.C., Coons M.J. Multiple health behaviours: Overview and implications. Journal of Public Health. 2012;1(34 Suppl):i3–10. doi: 10.1093/pubmed/fdr111. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22363028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teesson M., Degenhardt L., Hall W., Lynskey M., Toumbourou J.W., Patton G. 2.3 substance use and mental health in longitudinal perspective. Preventing harmful substance use: The evidence base for policy and practice. 2005;43 [Google Scholar]
- Teh C.H., Teh M.W., Lim K.H., Kee C.C., Sumarni M.G., Heng P.P.…Fadzilah K. Clustering of lifestyle risk behaviours and its determinants among school-going adolescents in a middle-income country: A cross-sectional study. BMC Public Health. 2019;19(1):1177. doi: 10.1186/s12889-019-7516-4. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/31455283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Tobacco retrieved from. https://www.who.int/health-topics/tobacco#tab=tab_3 (n.d.)
- World Health Organization . FAO; 2005. Fruit and vegetables for health: Report of the Joint. [Google Scholar]
- World Health Organization . 2010. Global recommendations on physical activity for health. (Retrieved from) [PubMed] [Google Scholar]
- World Health Organization . 2014. Global school-based student health survey (GSHS)http://www.who.int/chp/gshs/en/ Retrieved from. [Google Scholar]
- World Health Organization . 2014. Global school-based student health survey (GSHS) purpose and methodology.http://www.who.int/chp/gshs/methodology/en/ Retrieved from. [Google Scholar]
- World Health Organization Noncommunicable diseases country profiles 2018. 2018. https://www.who.int/nmh/publications/ncd-profiles-2018/en/ Retrieved from.
- World Health Organization . World Health Organization; 2019. Global status report on alcohol and health 2018. [Google Scholar]
- Yi X., Liu Z., Qiao W., Xie X., Yi N., Dong X. Clustering effects of health risk behavior on mental health and physical activity in Chinese adolescents. Health and Quality of Life Outcomes. 2020;18(1):211. doi: 10.1186/s12955-020-01468-z. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/32620107. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data for this study was obtained from the World Health Organization (WHO) website and is freely available online and can be downloaded.