Abstract
OBJECTIVE:
To evaluate the orthodontic treatment outcome among patients with non-syndromic unilateral cleft lip and palate using the Peer Assessment Rating (PAR) index.
MATERIALS AND METHODS:
The retrospective study comprised a sample of 80 patients with unilateral cleft lip and palate (39 males and 41 females) with complete pretreatment and posttreatment orthodontic records. The patients were divided into two groups according to the treatment modalities. Group 1 (n = 55), nonsurgical (consisted of patients treated with comprehensive orthodontics) and Group 2 (n = 25), surgical (with presurgical orthodontics followed by maxillary advancement orthognathic surgery). PAR score was evaluated on pretreatment and posttreatment study models for both groups.
RESULTS:
The mean percentage change for the weighted PAR score of Group 1 and Group 2 was 76.79 ± 20.27% and 82.37 ± 11.38%, respectively. Out of the total sample of 80 cases; 62 (77.5%) cases were “greatly improved,” 16 (20%) cases were “improved,” and 2 (2.5%) showed “worse/no improvement.” Nearly 72.5% of cases in Group 1 and 88% in Group 2 were greatly improved.
CONCLUSIONS:
The reduction in PAR score in both groups was satisfactory as more than 70% of the patients were in the greatly improved category. The results of the PAR index revealed a high occlusal outcome of orthodontic treatment rendered by the department for patients with unilateral cleft lip and palate.
Keywords: Cleft, orthodontic treatment outcome, Peer Assessment Rating index, unilateral cleft lip and palate
Introduction
Cleft lip and/or palate are one of the commonest craniofacial anomalies. It has a prevalence of approximately 1 in 700 live births ranging from 2.2–11.7 per 10,000 varying with a specific type of cleft, geographic location, ethnic group, and socioeconomic conditions.[1] Its incidence in the Asian population is reported to be around 2.0/1000 live births or higher.[2] The management of patients with cleft lip and/or palate begins from birth and requires a balance between growth, esthetics, function, and psychosocial development.[3] The common complication associated with these patients is maxillary growth retardation due to surgical repair of palatal processes that lead to Skeletal Class III malocclusion.[4] The effect of early surgical treatment has been commonly assessed using GOSLON (Great Ormond Street, London, and Oslo) yardstick[5] and 5-year-olds' index,[6] however, there are few studies in the literature to assess occlusal treatment outcome in patients with cleft lip and palate. The dental malocclusions, rotations, crowding, anomalous incisor, and skeletal discrepancies are commonly associated with patients having a cleft lip and/or palate and require immediate orthodontic interventions.[7] ICON,[8] ABO (American Board of Orthodontists) model grading system,[9] and Peer Assessment Rating Index (PAR) index[10] are the most commonly used indices for evaluation of treatment outcomes in orthodontic patients. The PAR was developed by Richmond et al.[10] specifically for the assessment of occlusal treatment outcome in orthodontics. The utility and validation of the PAR index in non-cleft and non-syndromic patients are well-documented in the literature.[11,12,13,14,15,16,17,18,19,20,21,22] The treatment outcome using the PAR index in the cleft patients has earlier been documented by Deacon et al.[23] and Manosudprasit et al.[24] A national project was conducted in the UK by Deacon et al.[23] to assess the occlusal outcomes for patients with unilateral cleft lip and palate (UCLP) using the PAR index. Manosudprasit et al.[24] also evaluated treatment outcomes among patients with cleft lip and/or palate who had undergone orthodontic treatment alone and with orthognathic surgery using the PAR index. Mano et al.[25] in a collaborative survey of 25 centers in Japan treating UCLP patients assessed the occlusion of anterior and posterior teeth with various parameters and concluded that final occlusion after orthodontic treatment was satisfactory in most cases.
At our center, significantly large numbers of patients with cleft lip and palate are managed comprehensively with orthodontics and combined orthognathic and surgical treatment. The literature regarding the objective assessment of occlusal treatment outcome is scanty from other cleft care centers. Hence, the proposed study was conducted to evaluate the orthodontic treatment outcome among patients with UCLP treated with comprehensive orthodontic and/or orthognathic surgery using the PAR index.
The null hypothesis for the study was “a high standard orthodontics treatment with excellent to good occlusal outcome is rendered at the institute to the patients with cleft lip and palate.”
Material and Methods
The present retrospective study was based on pretreatment and posttreatment records obtained from the orthodontic archives of the institution to assess the orthodontic treatment outcome using the PAR index in patients with UCLP. The present study was approved by the Institute ethics committee with approval reference number MK/2900/MDS dated 19-11-2016. After the initial screening of orthodontic archives; the treatment of 140 patients with complete unilateral cleft lip and palate was found to be initiated in the department from 2005 to 2018. The records of 80 debonded (39 males and 41 females) non-syndromic patients with UCLP with orthodontic treatment with or without functional jaw orthopedics, surgical maxillary advancement (LeFort 1 osteotomy), and complete pretreatment and posttreatment records were enrolled for the study. Alveolar bone grafting was done in few patients in Group 1 but was not considered for further evaluation during the study. No attempt was made to select the patient based on the malocclusion type, gender, or extraction pattern. All the debonded patients were included in the evaluation. Remaining 60 patients are still under various stages of orthodontic treatment and not yet debonded. Patients with cleft lip only, cleft palate only, and bilateral cleft and palate were excluded from the study.
The patients selected for this study were divided into two groups based on treatment modalities as per the record files.
Group 1: Nonsurgical Group (Comprehensive Orthodontics); (n = 55).
Group 2: Surgical Group (Orthodontics + Conventional Orthognathic Surgery; (n = 25).
PAR index[10] is a reliable method for assessing orthodontic treatment outcome. It was used in the present study for subjective evaluation of the pretreatment and posttreatment plaster models of patients with UCLP using the PAR ruler [Figure 1]. The scoring was done by the same examiner for the following 11 components of the PAR index: “Upper right segment, Upper anterior segment, Upper left segment, Lower right segment, Lower anterior segment, Lower left segment, Right buccal occlusion, Left buccal occlusion, Overjet, Overbite, and Centerline” [Figures 2-5]. Each set of models occluded in maximum intercuspation to assign the values to each component based on criteria outlined by Richmond et al.[10] The unweighted scores for each of the 11 components were multiplied by the British weightage as suggested by Richmond et al. to obtain a weighted PAR score [Figure 6]. Richmond et al.[10] using UK weightage had stated that to demonstrate a high standard of treatment for a practitioner, the mean percentage reduction in weighted PAR score should be greater than 70% for “greatly improved” category, more than 30% for “improved” category and the number of cases in the “worse or no improvement” category should be negligible or less change. Richmond et al.[10] considered a PAR score of 10 or less to be acceptable alignment and occlusion and a PAR score of five or less to be an almost ideal occlusion.
Figure 1.
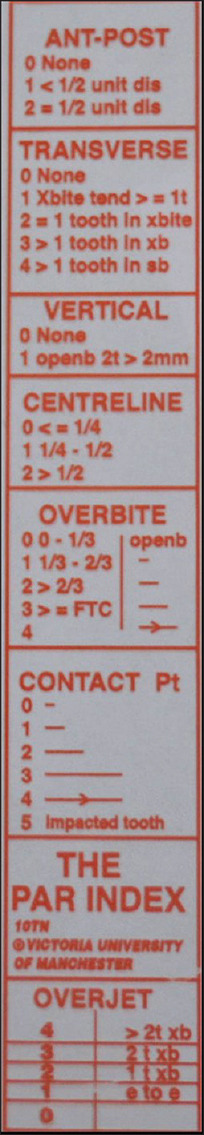
Peer Assessment Rating (PAR) index ruler
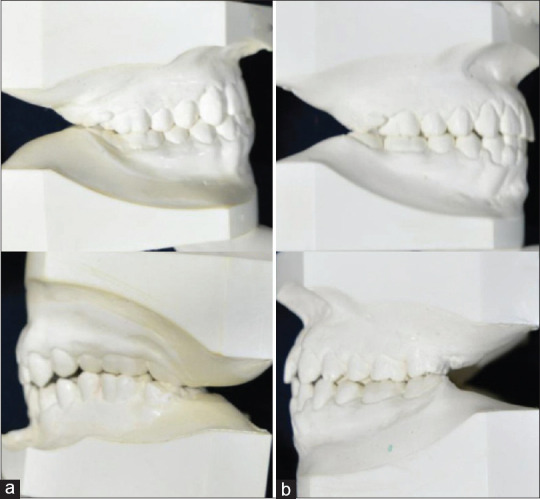
Figure 2.
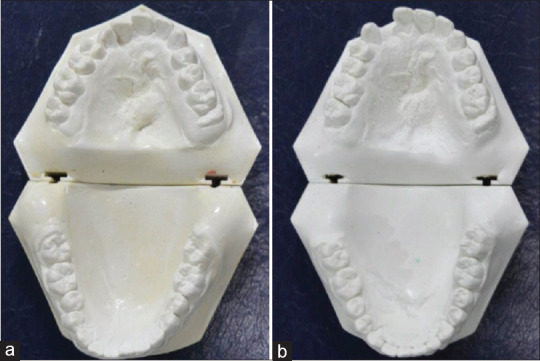
Study Models (a) Pretreatment (b) Posttreatment
Figure 5.
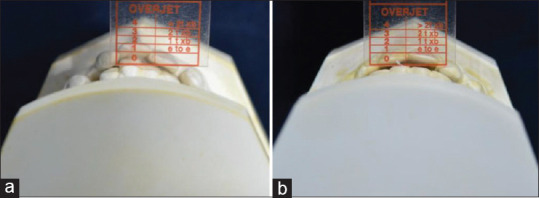
Measurement of an overjet component of PAR index with PAR ruler (a) Pretreatment model (b) Posttreatment model
Figure 6.
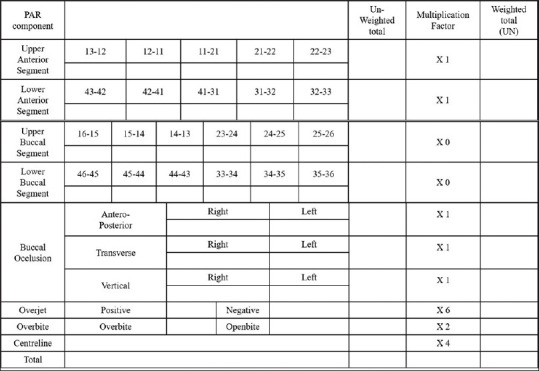
Peer Assessment Rating (PAR) index scoring sheet
Figure 3.

Measurement of displacement of contact points with PAR ruler between the central incisors on study models (a) Pretreatment model (b) Posttreatment model
Figure 4.
Measurement of right and left buccal segment component of PAR index (a) Pretreatment model (b) Posttreatment model
The intra-examiner reliability was determined for various parameters of the PAR index by repeating the measurements of 10 randomly selected study models by the same examiner at an interval of 3 weeks using Pearson's correlation coefficient and good intra-examiner reliability was found with a value of 0.864 to 1.000.
Statistical analysis
The analysis was conducted using the SPSS software (SPSS, version 22.0, IBM, Chicago, IL). Discrete categorical data were presented as n (%); continuous data were given as Mean ± SD. The normality of quantitative data was checked by measures of the Shapiro-Wilk test. Inferential statistics included the Mann-Whitney test, the Wilcoxon Signed-Rank test, and Fischer's exact test. Mann-Whitney test was used to compare the mean difference between the two groups. For the time-related variable, the Wilcoxon Signed-Rank test was applied. The distribution between the groups was compared using Fisher's exact test. All statistical tests were two-sided and performed at a significance level of α = 0.05.
Results and Observations
Table 1 shows the mean values of pretreatment, posttreatment PAR score, the mean point and percentage change for unweighted and weighted PAR scores of Group 1 and Group 2. The mean pretreatment weighted PAR score was 25.09 ± 12.32 for Group 1 (nonsurgical group) and 38.33 ± 9.91 for Group 2 (surgical group). The mean posttreatment weighted PAR score was 4.95 ± 3.85 for Group 1 (nonsurgical group) and 6.83 ± 4.62 for Group 2 (surgical group). The mean values of the weighted PAR score for the two groups decreased significantly from pretreatment to posttreatment. A reduction of more than 70% in the PAR score was observed in both groups. Group 1 and Group 2 showed a mean percentage reduction of 76.79% and 82.37% in the PAR score, respectively. Table 2 shows a significant difference between pretreatment weighted PAR scores of Group 1 compared to Group 2. Table 3 shows the distribution of the total sample into the three categories according to the percentage change in the PAR score. Around 77.5% of the patients out of the total sample of 80 were in the “greatly improved” category, 16 (20%) cases were in the “improved” category, and 2 (2.5%) cases showed “worse/no improvement.” In Group 1 (n = 55); 40 (72.7%) cases were categorized as “greatly improved,” 13 (23.6%) cases were in “improved” category and 2 (3.6%) cases showed “worse/no improvement.” In Group 2 (n = 25); 22 (88%) cases were categorized as “greatly improved,” 3 (12%) cases were in the “improved” category and none of the cases showed “worse/no improvement.”
Table 1.
Mean values of pretreatment, posttreatment, point and percentage change in Unweighted and Weighted PAR scores for the total sample (n=80) based upon various treatment modality groups
| Unweighted PAR score | Weighted PAR score | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment Mean±SD | Posttreatment Mean±SD | Point change mean±SD | Percentage change Mean±SD | P | Pretreatment Mean±SD | Posttreatment Mean±SD | Point change mean±SD | Percentage change mean±SD | P | |
| Group 1 (n=55) | 17.14±8.38 | 3.23±2.39 | 13.91±8.40 | 77.83±19.24 | 0.000** | 25.09±12.32 | 4.95±3.85 | 20.14±12.40 | 76.79±20.27 | 0.000** |
| Group 2 (n=25) | 22.50±6.22 | 4.67±2.80 | 17.36±5.03 | 79.36±9.87 | 0.028* | 38.33±9.91 | 6.83±4.62 | 31.33±9.07 | 82.37±11.38 | 0.028* |
P<0.05*, P<0.001**
Table 2.
Comparison between pre-treatment unweighted and weighted PAR scores for the total sample (n=80) based upon various treatment modality groups
| Unweighted PAR score Pretreatment P | Weighted PAR score Pretreatment P | |
|---|---|---|
| Group 1 vs Group 2 | 0.001** | 0.000** |
P<0.05*, P<0.001**
Table 3.
The outcome of treatment in different treatment modality groups and the total number of cases in each category for the weighted PAR score
| Category | Group 1 (n=55) | Group 2 (n=25) | Total (n=80) | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Greatly improved | 40 | 72.7% | 22 | 88% | 62 | 77.5% |
| Improved | 13 | 23.6% | 3 | 12% | 16 | 20% |
| Worse/no improvement | 2 | 3.6% | 0 | 0% | 2 | 2.5% |
Discussion
The results of the study led to the acceptance of the null hypothesis that “a high standard orthodontics treatment with excellent to good occlusal outcome is rendered at the institute to the patients with cleft lip and palate.” The inter-comparison of the surgical and nonsurgical groups was not possible because of the significant difference in the severity of pretreatment malocclusion in the surgical and nonsurgical groups as shown in Table 2. The present study showed a higher mean pretreatment weighted PAR score of 38.33 ± 9.91 for Group 2. The study by Manosudprasit et al.[24] with a sample size of 27 patients in orthodontic alone group and 7 patients in the orthognathic group showed the mean pretreatment weighted PAR score for orthodontics alone group (32.26 ± 7.96) in patients with UCLP was comparable to Group 1 (25.09 ± 12.32) of our study and the PAR score in the orthognathic group (39.86 ± 9.35) was comparable with Group 2 (38.33 ± 9.91) of the present study. According to Manosudprasit et al.[24] the mean posttreatment PAR scores were 2.67 ± 2.27 and 2.43 ± 1.51 for the orthodontic and orthognathic group, respectively which were lesser than the posttreatment scores of 4.95 ± 3.85 and 6.83 ± 4.62 observed in the present study for the similar groups. Deacon et al.[23] assessed a total of 128 cases from different centers and reported a mean pretreatment weighted PAR score of 41 ± 11 for consecutively treated UCLP cases treated without orthognathic surgery. Deacon et al.[23] who reported a posttreatment score of 12 ± 9 for UCLP cases is greater than the nonsurgical group in the present study. The results can be explained by the fact that the pretreatment scores were higher and comparable to the surgical group though the patients were treated nonsurgically. According to Manosudprasit et al.[24] the mean point reduction of weighted PAR scores was 29.59 ± 8.79 and 37.43 ± 8.79 for the orthodontic and orthognathic group, respectively which was comparatively higher than the present study with a mean point reduction of weighted PAR score of 20.14 ± 12.40 and 31.33 ± 9.07. The results of the study by Manosudprasit et al.[24] reported 100% of the cases treated with orthognathic surgery in the “greatly improved” category whereas the present study showed 88% of the cases in the greatly improved category. In the study by Manosudprasit et al.,[24]92.59% cases treated by comprehensive orthodontic treatment alone were in the greatly improved category which is higher than the present study but the sample of our study was more thus, the results are more reliable.
Ponduri et al.[26] compared the treatment outcomes of 40 consecutively treated orthodontic patients and 40 orthognathic patients to evaluate the standard of care using the PAR index in non-cleft patients. PAR scores of orthodontic and orthognathic patients improved by 77% and 74%, respectively, after treatment indicating that excellent to good occlusal results were achieved for both groups. Thus, surgical and nonsurgical treatment of UCLP patients at our center showed results comparable to occlusal outcomes in non-cleft individuals. A high-quality occlusal outcome is important for all patients as good intercuspation at the end of treatment is thought to improve stability.
The PAR index used in the study also has some limitations. Centerline and molar relation in cleft cases with missing lateral incisors or sometimes more missing teeth and a large defect and difficult to correct. This leads to increased posttreatment PAR scores. Deacon et al.[23] recommended 69.2% as a landmark for comparison of fixed orthodontic treatment outcome in cleft lip and palate patients. The results show greater PAR scores for patients in both groups in the study. A new landmark of a mean percentage reduction of 76.79% and 82.37% in PAR score in nonsurgical and surgical cases should be used for appraisal of treatment outcome at cleft centers.
The limitation of the present study was a retrospective design and prospective study in the future can provide high-quality evidence. Moreover, other factors such as age at which orthodontic treatment was commenced, the extent of cleft, alveolar bone grafting, and missing teeth which can affect the outcome were not taken into consideration.
Conclusions
The pretreatment PAR scores were higher for Group 2 due to the severity of the malocclusion. The posttreatment PAR scores were lower for Group 2 and reduction in score was also greater for Group 2. Since 70% of the cases in both the groups were greatly improved it can be concluded that excellent to good occlusal results were achieved for both the groups. The results of the PAR index revealed a high occlusal outcome for all the cleft cases treated at the center.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Brito LA, Meira JGC, Kobayashi GS, Passos-Bueno MR. Genetics and management of the patient with orofacial cleft? Plast Surg Int. 2012;2012:782821. doi: 10.1155/2012/782821. doi: 10.1155/2012/782821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray J. Gene/environment causes of cleft lip and/or palate: Gene/environment causes of cleft lip and palate. Clin Genet. 2002;61:248–56. doi: 10.1034/j.1399-0004.2002.610402.x. [DOI] [PubMed] [Google Scholar]
- 3.Cobourne MT. The complex genetics of cleft lip and palate. Eur J Orthod. 2004;26:7–16. doi: 10.1093/ejo/26.1.7. [DOI] [PubMed] [Google Scholar]
- 4.Liao Y-F, Mars M. Hard palate repair timing and facial growth in cleft lip and palate: A systematic review. Cleft Palate Craniofac J. 2006;43:563–70. doi: 10.1597/05-058. [DOI] [PubMed] [Google Scholar]
- 5.Mars M, Plint D, Houston WJB, Bergland O, Semb G. The Goslon Yardstick: A new system of assessing dental arch relationships in children with unilateral clefts of the lip and palate. Cleft Palate J. 1987;24:314–22. [PubMed] [Google Scholar]
- 6.Atack N, Hathorn I, Mars M, Sandy J. Study models of 5-year-old children as predictors of surgical outcome in unilateral cleft lip and palate. Eur J Orthod. 1997;19:165–70. doi: 10.1093/ejo/19.2.165. [DOI] [PubMed] [Google Scholar]
- 7.Honda Y, Suzuki A, Ohishi M, Tashiro H. Longitudinal study on the changes of maxillary arch dimensions in Japanese children with cleft lip and/or palate: Infancy to 4 years of age. Cleft Palate Craniofac J. 1995;32:149–55. doi: 10.1597/1545-1569_1995_032_0149_lsotco_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 8.Daniels C, Richmond S. The development of the index of complexity, outcome, and need (ICON) J Orthod. 2000;27:149–62. doi: 10.1093/ortho/27.2.149. [DOI] [PubMed] [Google Scholar]
- 9.Casko JS, Vaden JL, Kokich VG, Damone J, James RD, Cangialosi TJ, et al. Objective grading system for dental casts and panoramic radiographs. Am J Orthod Dentofacial Orthop. 1998;114:589–99. doi: 10.1016/s0889-5406(98)70179-9. [DOI] [PubMed] [Google Scholar]
- 10.Richmond S, Shaw WC, O'Brien KD, Buchanan IB, Jones R, Stephens CD, et al. The development of the PAR Index (Peer Assessment Rating): Reliability and validity. Eur J Orthod. 1992;14:125–39. doi: 10.1093/ejo/14.2.125. [DOI] [PubMed] [Google Scholar]
- 11.Buchanan IB, Shaw WC, Richmond S, O'Brien KD, Andrews M. A comparison of the reliability and validity of the PAR Index and Summers' Occlusal Index. Eur J Orthod. 1993;15:27–31. doi: 10.1093/ejo/15.1.27. [DOI] [PubMed] [Google Scholar]
- 12.Richmond S, Andrews M. Orthodontic treatment standards in Norway. Eur J Orthod. 1993;15:7–15. doi: 10.1093/ejo/15.1.7. [DOI] [PubMed] [Google Scholar]
- 13.DeGuzman L, Bahiraei D, Vig KWL, Vig PS, Weyant RJ, O'Brien K. The validation of the Peer Assessment Rating index for malocclusion severity and treatment difficulty. Am J Orthod Dentofacial Orthop. 1995;107:172–6. doi: 10.1016/s0889-5406(95)70133-8. [DOI] [PubMed] [Google Scholar]
- 14.Birkeland K, Furevik J, Boe OE, Wisth PJ. Evaluation of treatment and post-treatment changes by the PAR Index. Eur J Orthod. 1997;19:279–88. doi: 10.1093/ejo/19.3.279. [DOI] [PubMed] [Google Scholar]
- 15.Al Yami EA, Kuijpers-Jagtman AM, van 't Hof MA. Stability of orthodontic treatment outcome: Follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999;115:300–4. doi: 10.1016/s0889-5406(99)70333-1. [DOI] [PubMed] [Google Scholar]
- 16.McKnight MM, Daniels CP, Johnston LE. A retrospective study of two-stage treatment outcomes assessed with two modified PAR indices. Angle Orthod. 1998;68:521–6. doi: 10.1043/0003-3219(1998)068<0521:ARSOTS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Hamdan A. An appraisal of the peer assessment rating (PAR) index and a suggested new weighting system. Eur J Orthod. 1999;21:181–92. doi: 10.1093/ejo/21.2.181. [DOI] [PubMed] [Google Scholar]
- 18.Dyken RA, Sadowsky PL, Hurst D. Orthodontic outcomes assessment using the Peer Assessment Rating Index. Angle Orthod. 2001;71:164–9. doi: 10.1043/0003-3219(2001)071<0164:OOAUTP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Fox NA, Daniels C, Gilgrass T. A comparison of the index of complexity outcome and need (ICON) with the peer assessment rating (PAR) and the index of orthodontic treatment need (IOTN) Br Dent J. 2002;193:225–30. doi: 10.1038/sj.bdj.4801530. [DOI] [PubMed] [Google Scholar]
- 20.Freitas KMS, Freitas DS, Valarelli FP, Freitas MR, Janson G. PAR evaluation of treated Class I extraction patients. Angle Orthod. 2008;78:270–4. doi: 10.2319/042307-206.1. [DOI] [PubMed] [Google Scholar]
- 21.O'Brien K, Wright J, Conboy F, Appelbe P, Bearn D, Caldwell S, et al. Prospective, multi-center study of the effectiveness of orthodontic/orthognathic surgery care in the United Kingdom. Am J Orthod Dentofacial Orthop. 2009;135:709–14. doi: 10.1016/j.ajodo.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 22.Onyeaso CO, BeGole EA. Orthodontic treatment—improvement and standards using the Peer Assessment Rating index. Angle Orthod. 2006;76:260–4. doi: 10.1043/0003-3219(2006)076[0260:OTASUT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Deacon S, Bessant P, Russell JI, Hathorn I. What are the occlusal outcomes for unilateral cleft lip and palate patients.A national project in the UK? Br Dent J. 2007;203:E18. doi: 10.1038/bdj.2007.807. [DOI] [PubMed] [Google Scholar]
- 24.Manosudprasit M, Wangsrimongkol T, Danthumrongkul S. The final orthodontic treatment outcome evaluation in patients with cleft lip and palate at Khon Kaen University cleft lip and palate center: A pilot study. J Med Assoc Thai. 2011;94:S21–6. [PubMed] [Google Scholar]
- 25.Mano M, Ishiwata Y, Asahito T, Sakamoto T, Morishita T, Oonishi YY, et al. A collaborative survey on occlusion after orthodontic treatment in patients with unilateral cleft lip and palate in Japan. Orthod Waves. 2018;77:101–10. [Google Scholar]
- 26.Ponduri S, Pringle A, Illing H, Brennan PA. Peer assessment rating (PAR) index outcomes for orthodontic and orthognathic surgery patients. Br J Oral Maxillofac Surg. 2011;49:217–20. doi: 10.1016/j.bjoms.2010.03.009. [DOI] [PubMed] [Google Scholar]


