Sex differences in cardiovascular care are widespread. Women are less likely to receive statins for primary and secondary prevention, anticoagulation for atrial fibrillation, percutaneous coronary interventions for coronary disease, and heart replacement therapies like transplants and left ventricular assist devices for advanced heart failure. The list continues. Multiple research studies, educational efforts, professional campaigns, and guidelines have improved awareness and attempted interventions to reduce sex differences. However, more work needs to be done. The question remains: How do we provide high value care to women and reduce sex differences in care?
Contemporary shifts in health care delivery systems from fee-for-service to value-based payment models create challenges and opportunities to address treatment differences. Value-based systems aim to improve care and reduce costs. Critics of value-based payment models have focused on the concern that treatment differences and disparities in care will increase in such systems. Risk-adjustment may not appropriately account for all the social and environmental factors influencing care delivery and unfairly penalize health systems that serve high risk patients. Proponents of value-based models argue that systems with clearly defined quality metrics will raise standards of care for all patients and reduce health disparities.
In a Department of Health and Human Services report of social risk factors (ie, poverty, low-income housing, Black race, Hispanic ethnicity, disability, and rural residence) and federal payment systems, Medicare beneficiaries with social risk factors had worse outcomes on many quality measures, even after adjustment for provider difference.1 Further, providers who cared for a higher numbers of patients with social risk factors were more likely to have worse performance and face financial penalties. These findings are likely related to the negative impact of social and environment factors. Consequently, financial penalties can result in provider frustration and burnout. Thus, value-based systems may need to incentivize providers who care for a large number of high risk patients and subsidize special services that specifically address the social and environmental factors impacting patients in order to be successful. In other scenarios, value-based payment structures can potentially improve care by penalizing providers who provide disparate care and/or by providing incentives to providers who show significant improvements in care.
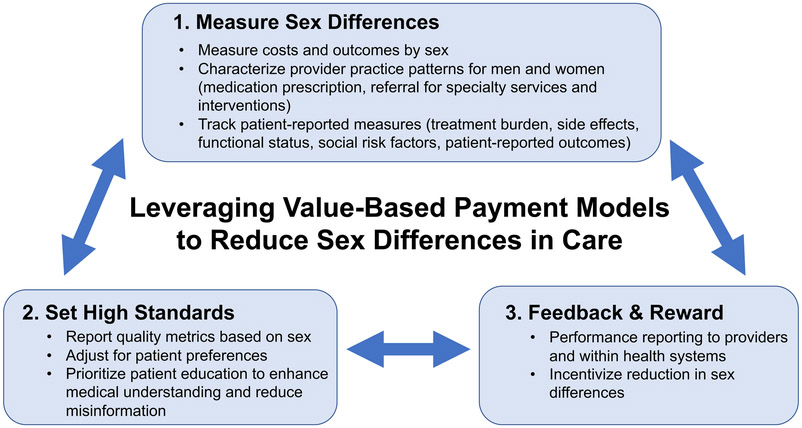
Value-based payment models may have a clearer path for success in reducing sex differences and disparities. Women comprise 50.5% of the U.S. population,3 span the gamut of social strata, and comprise the largest group of patients where treatment differences and disparities are a major health issue. Value-based payments may help address sex differences by directly targeting provider-related factors, rewarding performance improvement and honing in on patient-related factors like provider and treatment mistrust. To ensure appropriate understanding of the sex difference problem, providers and policymakers can extrapolate from the 3-step framework proposed for addressing social risk factors in the Medicare population,2 namely: 1) measuring and reporting quality based on sex, 2) setting explicit high quality standards for females and males, and 3) rewarding high quality when providers and systems reduce sex differences in care (Figure).
FIGURE:
Three Iterative Steps in Leveraging Value-Based Payment Models to Reduce Sex Differences in Care
Studies such as the Nanna et al article4 addressing sex differences in statin use in this issue of Circulation: Cardiovascular Quality and Outcomes help inform the first step in the process. This manuscript is an example of a new wave of studies that are uncovering reasons for care differences by measuring and reporting provider perceptions and practice patterns as well as patient perceptions, beliefs, and patient-centered outcomes. Similar to prior studies, this analysis found that females were less likely than males to receive guideline-recommended statin therapy for both primary and secondary prevention and were less likely to receive statins at guideline-recommended intensity. The analysis went on to assess the underlying causes of care differences and found that both patient and provider-related factors contributed. While some women did not receive statins due to mistrust of the therapy or discontinuation due to side effects, the majority of women did not receive statins because they were never offered the therapy by their provider. The next step is to use studies such as this to improve care delivery.
Policy makers and health systems can leverage value-based payment models to target sex differences in care. Health systems can explicitly measure sex differences in care within their own systems and prospectively monitor for any treatment differences. One example may be monitoring statin prescription among men and women using the electronic medical record based on guideline recommendations and risk status. It would require clear documentation that statin therapy is offered to all qualifying patients and if they choose not to pursue therapy. Further, measurement of patient-reported measures such as treatment burden and medication side effects, functional status, and social risk factors can also be included. Next, policy makers and health systems can directly address any sex differences by necessitating the reporting of quality metrics separately for men and women rather than as a combined measure. Systems can reward providers who deliver equitable care or demonstrate greater improvements in reducing treatment differences by sex. Interventions to improve issues like medication prescription may prove to be easier than processes of care like equitable referral of both women and men for cardiac interventions, but being cognizant of sex differences and the need to target these differences in care is paramount.
Prior interventions to reduce sex differences and disparities in care have failed at least partly because providers have not been incentivized to focus on these issues. Restructuring of the payment structure to reward performance in value-based payment models rather than fee-for-service stands a higher chance of success in targeting sex-based treatment differences and improving care for women.
Acknowledgments
Funding: Dr. Khazanie has institutional research grant support from National Institutes of Health (K23 HL145122) and the Center for Women’s Health Research, University of Colorado Anschutz Medical Campus. Dr. Ho is supported by grants from NHLBI and VA HSR&D.
Footnotes
Disclosures: Dr. Khazanie has no disclosures. Dr. Ho serves as the Deputy Editor for Circulation: Cardiovascular Quality and Outcomes.
Contributor Information
Prateeti Khazanie, Division of Cardiology, University of Colorado School of Medicine, Aurora, CO.
P. Michael Ho, Division of Cardiology and Data Science to Patient Value Program, University of Colorado School of Medicine, Aurora, CO; Rocky Mountain Regional VA Medical Center, Aurora, CO.
References
- 1.U.S. Department of Health & Human Services, Office of the Assistant Secretary for Planning and Evaluation. Report to Congress: Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing Programs. https://aspe.hhs.gov/pdf-report/report-congress-social-risk-factors-and-performance-under-medicares-value-based-purchasing-programs. Washington, DC: 2016. Accessed July 5, 2019. [Google Scholar]
- 2.Joynt KE, Zuckerman R and Epstein AM. Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing Programs. Circulation: Cardiovascular Quality and Outcomes. 2017;10:e003587. [DOI] [PubMed] [Google Scholar]
- 3.World Bank Data. Female Population. https://data.worldbank.org/indicato/sp.pop.totl.fe.zs Accessed July 18, 2019.
- 4.Nanna MG, Want TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, Virani SS, Wilson PWF, Louie MJ, Koren A, Li Z, Peterson ED, Navar AM. Sex Differences in the Use of Statins in Community Practice: The Patient and Provider Assessment of Lipid Management (PALM) Registry. Circulation: Cardiovascular Quality and Outcomes. 2019;12:e005562. [DOI] [PMC free article] [PubMed] [Google Scholar]