Abstract
As the world navigates the coronavirus disease 2019 (COVID-19) pandemic, there is a growing need to assess its impact in patients with autoimmune rheumatic diseases, such as systemic lupus erythematosus (SLE). Patients with SLE are a unique population when considering the risk of contracting COVID-19 and infection outcomes. The use of systemic glucocorticoids and immunosuppressants, and underlying organ damage from SLE are potential susceptibility factors. Most patients with SLE have evidence of high type I interferon activity, which may theoretically act as an antiviral line of defense or contribute to the development of a deleterious hyperinflammatory response in COVID-19. Other immunopathogenic mechanisms of SLE may overlap with those described in COVID-19, thus, studies in SLE could provide some insight into immune responses occurring in severe cases of the viral infection. We reviewed the literature to date on COVID-19 in patients with SLE and provide an in-depth review of current research in the area, including immune pathway activation, epidemiology, clinical features, outcomes, and the psychosocial impact of the pandemic in those with autoimmune disease.
Abbreviations: Act-1, Adaptor protein NF-κ activator; ACE2, Angiotensin-converting enzyme 2; AZA, Azathioprine; C5aR1, C5a receptor; COVID-19, Coronavirus disease 2019; C-19-GRA, COVID-19 Global Rheumatology Alliance; CYC, Cyclophosphamide; EBV, Epstein-Barr virus; HCQ, Hydroxychloroquine; ICU, Intensive care unit; IFN, Interferon; IRF, Interferon regulatory factor; ISG, Interferon-stimulated gene; IFNAR, Interferon-α/β receptor; IL, Interleukin; JAK, Janus kinase; LOF, Loss-of-function; MASP-2, Manna-binding lectin associated serine protease-2; mTOR, Mechanistic (mammalian) target of rapamycin; MMF, Mycophenolate mofetil; MyD88, Myeloid differentiation primary response 88; NAC, N-Acetylcisteine; NET, Neutrophil extracellular trap; NYC, New York City; pDC, Plasmacytoid dendritic cell; PI3K, Phosphatidylinositol 3-kinase; Treg, Regulatory T cell; RT-PCR, Reverse transcription polymerase chain reaction; pS6, Ribosomal protein 6; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; STAT, Signal Transducer and Activator of Transcription; SDH, Social determinants of health; sGC, Systemic glucocorticoids; SLE, Systemic Lupus Erythematosus; Th17, T helper 17; TBK1, TANK-binding kinase 1; TLR, Toll-like receptor; TNF, Tumor necrosis factor; TRAF, Tumor necrosis factor receptor-associated factor; TRIF, TIRdomain-containing adapter-inducing interferon-β
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causal agent of coronavirus disease 2019 (COVID-19), has infected millions of people worldwide. The mortality of the virus is likely underestimated in official counts, as we have observed a 20% increase in deaths over the average expected number between March 1 and August 1, 2020 in the United States.1 It is clear that outcomes following COVID-19 infection vary considerably between people, and some populations are at particularly high risk. Thus, there has been a need to assess the impact of COVID-19 in patients with autoimmune disease, including those with systemic lupus erythematosus (SLE).
Patients with SLE are a unique population when considering the risk of contracting COVID-19 and the outcomes of the infection. The underlying organ damage from SLE and the use of systemic glucocorticoids (sGC) and immunosuppressants could be risk factors for the development of severe COVID-19.2 SLE is more prevalent and severe in ancestrally African and Hispanic patients, which overlaps with high-risk groups associated with poor outcomes of COVID-19, although the association with the latter may be mediated more by social determinants of health (SDH) as opposed to biologic factors.3, 4, 5, 6 In contrast, SLE is a female-predominant disease which may represent a protective factor, as COVID-19 has been shown to affect males more severely.3 , 7, 8, 9, 10 One interesting feature is that inflammation in SLE is often characterized by elevation of type I interferon (IFN), which has antiviral properties and could potentially be protective. This is not known, however, and even if true, it could be offset by other sociodemographic, biologic, and clinical aspects of the disease and its management. In addition, excessive complement activation with consequent development of thrombotic microangiopathy has been identified in many patients with COVID-19 and seems to at least partially mediate organ dysfunction in severe cases, resembling a complement-mediated thrombotic microangiopathy.11 , 12 Although complement consumption is a classic feature of SLE, the classical pathway is often the main target of activation by immune complexes in SLE, whereas the alternative and lectin-based complement pathways seem to play a greater role in COVID-19 pathogenesis.13 , 14
There have been substantial scientific efforts around the world to elucidate COVID-19 pathogenesis, risk factors, optimal management, and prevention strategies. Similarly, data on the impact of the pandemic in patients with SLE has grown significantly in recent months. Accordingly, we provide an overview of the susceptibility factors to viral infections in patients with SLE and potential immunologic and pathologic overlaps between COVID-19 and SLE, as well as data regarding the epidemiology, clinical features, outcomes, and psychosocial impact of COVID-19 in SLE patients.
RELATIONSHIP BETWEEN SLE AND RISK OF VIRAL INFECTIONS
SARS-CoV-2, a single-stranded RNA virus and the causal agent of COVID-19, has infected millions of people worldwide. The virus enters the cells by binding to the angiotensin-converting enzyme 2 (ACE2) receptor, which determines viral tropism. The type 2 transmembrane serine protease is also required to complete the fusion process by cleaving the ACE2 molecules and activating the SARS-CoV-2 S protein.15 The clinical spectrum of COVID-19 is broad, ranging from asymptomatic infection to life-threatening cytokine storm, acute respiratory distress syndrome, and multiorgan dysfunction.16
SLE is a chronic multisystem autoimmune disease characterized by dysregulated type I IFN responses and defective immune tolerance mechanisms.17 Patients with SLE have an increased risk of mortality that is 2–5 times the rate of the general population.18 Bacterial, viral, and opportunistic infections are common in SLE and account for the second leading cause of death in this group in developed countries, ranging from 25% to 50% of mortality cases.19, 20, 21 Infections in patients with SLE tend to be more frequent during the initial 5 years after diagnosis, which could reflect underlying disease pathogenesis or aggressive immunosuppressive therapy at the outset of disease.18 , 22
Functional abnormalities in the immune system due to intrinsic factors and the use of immunosuppressive therapies both contribute to infection risk in patients with SLE.20 , 23 , 24, 25, 26, 27 Immune cells are affected in SLE in both number and function. Lymphopenia and neutropenia can occur either due to active inflammation in SLE with increased apoptosis of immune cells or as a side effect of immunosuppressants.28 CD8 T cell responses are impaired in SLE patients, including defects in phagocytosis and chemotaxis.20 , 29 , 30 Interestingly, Katsuyama et al recently reported the presence of CD8+T cells highly expressing CD38 in a subset of patients with SLE and high incidence of infections, independent of disease activity, organ damage and disease flares. These CD8CD38highT cells exhibited decreased cytotoxic capacity, degranulation, and expression of perforin and granzymes, providing a mechanism by which abnormalities in cellular immunity may lead to an increased susceptibility to infections in patients with SLE.29 Complement dysregulation is common in SLE and worsens with disease activity. Hypocomplementemia has been identified as an independent predictor of infection in SLE patients.24 Interestingly, genetic deficiencies in complement components can predispose to SLE, as well as other primary immunodeficiency disorders.31 Furthermore, low immunoglobulin (Ig) levels, particularly IgG subclasses and IgM, have been identified in patients with SLE, which may also contribute to the increased susceptibility to infections.28 , 32 , 33
Herpes zoster is frequent in SLE, occurring in up to 40% of patients.19 Certain SLE-specific factors have been associated with herpes zoster, including lymphopenia and anti-Ro antibodies. As expected, the use of sGC and immunosuppressants such as cyclophosphamide (CYC) are also associated with a greater risk of herpes zoster and other viral infections.24 , 34 , 35 Cytomegalovirus and upper respiratory tract viral infections are common in the SLE population, and may present with severe and atypical manifestations that mimic SLE flares.28 , 36
Respiratory infections are one of the most common causes of hospitalization and early mortality in patients with SLE.22 Elderly individuals (≥65 years of age) with rheumatic conditions are at greater risk of influenza and influenza-related complications.37 Influenza pneumonia often precedes bacterial infections, which may lead to prolonged hospitalizations and overall worse outcomes.38 , 39 In patients with SLE, viral infections can also trigger SLE flares after the virus is cleared.39 , 40 In comparison, Influenza A infection in lupus-prone Faslpr mice is cleared effectively and is not associated with worsening autoimmune features in the acute setting, although these mice can subsequently develop severe pulmonary inflammation weeks after viral clearance.41 Notably, annual vaccination against influenza is associated with decreased hospitalization and intensive care unit (ICU) admissions in patients with SLE; hence this practice is highly encouraged.42
In addition to the increased susceptibility to certain viral infections in SLE, the role of exogenous viruses in triggering autoimmunity has also been proposed. Epstein-Barr virus (EBV) is a potential environmental factor involved in SLE pathogenesis.43 Although most acute EBV infections occur during childhood, EBV remains latent in B cells and can subsequently reactivate. EBV stimulates the proliferation of autoreactive B cells, acts as a superantigen in T cells, and stimulates IFN-α production by plasmacytoid dendritic cells (pDCs).44 Additionally, studies have demonstrated evidence of molecular mimicry between EBV proteins and nuclear antigens, and the EBV nuclear antigen 2 protein can bind to several SLE risk alleles, suggesting important mechanisms by which EBV can trigger autoimmunity.44, 45, 46 The role of other viruses such as cytomegalovirus in the pathogenesis of SLE is less clear.
CONVERGENT IMMUNOPATHOGENIC MECHANISMS OF COVID-19 AND SLE
Type I interferons
Various lines of evidence have suggested a crucial role of type I IFNs in the course of disease and outcomes of COVID-19. The antiviral properties of type I IFNs are well known and many viruses have developed strategies to escape their inhibitory effects.47 , 48 Furthermore, most patients with SLE have evidence of elevated circulating type I IFN or show overexpression of type I IFN genes in circulating immune cells49, 50, 51; therefore, it is conceivable that IFNs are a critical point of convergence between SLE and COVID-19.
Previous murine studies on SARS-CoV had demonstrated that exuberant viral replication coupled with delayed type I IFN responses are associated with decreased survival.52 In vivo and in vitro models of SARS-CoV-2 infection have shown evidence of inappropriate antiviral and dysregulated inflammatory responses, characterized by low levels of type I and type III IFNs, high levels of multiple chemokines and IL-6.53 Consistent with these observations, a more recent study found that patients with severe and critical COVID-19 displayed significant impairment in the type I IFN response, with lack of IFN-β, low IFN-ɑ activity and plasma levels, as well as a higher SARS-Co-2 viral load, and increased tumor necrosis factor (TNF)-α and IL-6.54 As certain conditions such as obesity, cancer and aging may be associated with decreased type I IFN signaling, it is also possible that these conditions contribute to a dysfunctional IFN response in COVID-19.55, 56, 57 In addition, pDC depletion and functional impairment have also been identified in patients with COVID-19, with decreased production of IFN-α by these cells in vitro.58 , 59 A single-cell gene expression study of peripheral immune cells showed upregulation of several IFN-stimulated genes (ISGs) in CD14+ monocytes, although the IFN signature was heterogeneous among COVID-19 patients and cell types.58 Another study evaluating cells obtained from the respiratory tract of patients with COVID-19 via bronchoalveolar lavage showed marked expression of “proinflammatory” ISGs compared to cells from patients with community-acquired pneumonia and SARS-CoV infection. The ISG expression presumably decreased over time in COVID-19 patients who survived when comparing cells collected from different patients ranging from days 4 to 15 from the onset of symptoms. In contrast, cells from the deceased patient showed robust ISG expression, despite being obtained at day 12 after symptom onset.48 Although the small sample size and lack of longitudinal data for each patient are potential limitations of this study, these findings could suggest that a persistent and/or delayed type I IFN response may be associated with worse outcomes. Results from a recent study also suggest a temporal shift in the cytokine response in patients with COVID-19, ranging from an early type I IFN-predominant response to a proinflammatory response in later stages of the disease.59 Interestingly, this study also found an impaired type I IFN response and marked reduction in proinflammatory cytokine production by circulating monocytes and myeloid dendritic cells, despite elevated levels of these cytokines in plasma, suggesting the source is likely to be the lungs rather than peripheral blood cells.59
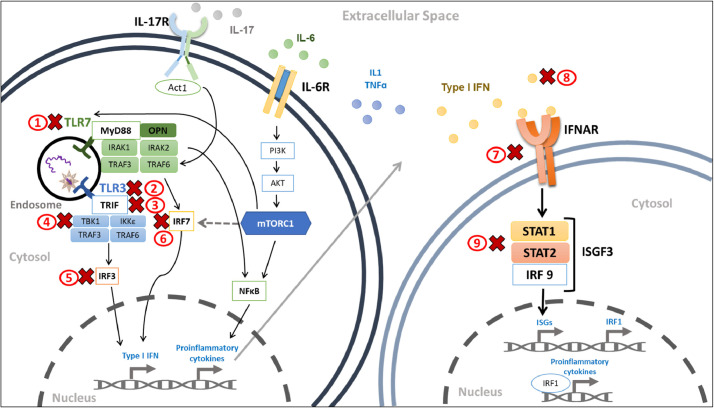
Several inborn errors that directly or indirectly involve type I and type III IFN pathways are also associated with life-threatening viral infections secondary to the influenza virus, live-attenuated vaccines, and other viruses. These include genetic defects in the IFN-α/β receptor-1 and -2 (IFNAR-1 and IFNAR-2), IRF3, IRF7, IRF9, IFIH1, TLR3, TBK1, TICAM1/TRIF, STAT1 and STAT2.60, 61, 62 TLR3 and IFIH1 (also known as MDA5) are pattern recognition receptors that bind viral RNA. TLR3 and TLR7 induce type I IFN production via activation of IRF-3 (mediated by TBK1 and TICAM1/TRIM) and IRF7, respectively. IRF9, STAT1 and STAT2 are components of the IFN-stimulated factor gene 3 (ISFG3) complex, which is part of the intracellular downstream pathway activated by type I IFN (Fig 1 ).63 Interestingly, the structural SARS-CoV-2 N protein has also been shown to antagonize IFN signaling by suppressing phosphorylation and translocation of STAT1 and STAT2, representing a potential viral mechanism to evade the innate immune response.64 GATA2 deficiency, a pleiotropic syndromic disorder, is also associated with increased susceptibility to viral infections, at least partially due to the absence of pDCs in this disorder, a major cell type in producing type I IFN.65
Fig 1.
Convergent type I interferon and proinflammatory cytokine pathways shared between SLE and COVID-19. Binding of viral RNA to toll-like receptor (TLR)3 and TLR7 induces activation of interferon regulatory factor (IRF)3 and IRF7, respectively, which is mediated by several adaptor proteins. Once active, IRF3 and IRF7 translocate to the nucleus and induce transcription of interferon (IFN)-α or IFN-β. TLR7 (and TLR8) activation also leads to nuclear translocation of NF-κB and induction of proinflammatory cytokines such as interleukin-1 (IL-1), IL-6, and tumor necrosis factor-α (TNF-α). Binding of IL-17, secreted by Th17 cells, to its receptor (IL-17R) activates the adaptor protein NF-κ activator (Act1) and TRAF6, inducing the nuclear translocation of NF-κB. IL-6 binding to its receptor (IL-6R) activates the phosphatidylinositol 3-kinase (PI3K)-Akt pathway, in turn activating the mechanistic target of rapamycin complex 1 (mTORC1). mTORC1 mediates phosphorylation of S6K (not shown), which promotes the formation of the TLR-MyD88 complex and IRF7-mediated production of type I IFN. Activated mTORC1 also stimulates transcription of IRF7 mRNA by a 4E-BP phosphorylation-dependent mechanism (dashed arrow), and induces NF-κB activity. Type I IFNs, secreted in an autocrine and paracrine matter, bind to the IFN-α/-β receptor (IFNAR), leading to assembly and translocation to the nucleus of the interferon-stimulated gene factor 3 (ISGF3), which is composed of STAT1, STAT2 and IRF9. Once in the nucleus, ISGF3 binds to promoters of IFN-stimulated genes (ISG), stimulating their transcription. IRF1 is also induced in response to type I IFN, which activates the transcription of proinflammatory cytokines. A red X mark is located next to each component of the pathway that is impaired by loss-of-function genetic variants (1–7), autoantibodies against type I IFN (8), or SARS-CoV-2 proteins. Act1, adaptor protein NF-κ activator; IFN, interferon; IFNAR, IFN-α/-β receptor; IRF, interferon regulatory factor; ISG, IFN-stimulated genes; ISGF3, interferon-stimulated gene factor 3; mTORC1, mechanistic target of rapamycin complex 1; MyD88, myeloid differentiation primary response 88; PI3K, phosphatidylinositol 3-kinase; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; STAT, signal transducer and activator of transcription; TBK1, TANK-binding kinase 1; TLR, toll-like receptor; TNF-α, tumor necrosis factor-α; TRAF, tumor necrosis factor receptor-associated factor; TRIF, TIR-domain-containing adapter-inducing interferon-β. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
In agreement with the antiviral role of type I IFN, a case series identified rare missense and nonsense putative loss-of-function (LOF) variants involving TLR7 in 4 young previously healthy males with critical COVID-19; these variants were associated with impaired type I and type II IFN response in these patients.66 A recent study showed that rare LOF variants involving TLR3- and IRF7-mediated type I IFN response were enriched in patients with life-threatening COVID-19 when compared to subjects with mild or asymptomatic SARS-CoV-2 infection. Genetic defects at 8 loci (TLR3, UNC93B1, TICAM1/TRIF, TBK1, IRF3, IRF7, IFNAR 1, and IFNAR2) involved in type I IFN signaling were identified in 3.5% of patients. Interestingly, prior to COVID-19, these patients had not had any life-threatening viral infections, which may relate to the increased virulence of SARS-CoV-2 compared to influenza and other common respiratory viruses (Fig 1). Some of the autosomal dominant genetic disorders were newly identified, including UNC93B1 (a chaperone that regulates endosomal TLR stability), IRF7, IFNAR1, and IFNAR2 deficiencies.67 Conversely, several risk genes linked to type I IFN have been associated with SLE, many of which are gain-of-function variants.68 One of such examples is the IFIH1 rs1990760 gene variant, which is associated with the presence of anti-double-stranded DNA antibodies and increased sensitivity to IFN-α in SLE.69 Interestingly, other IFIH1 polymorphisms have been associated with increased risk or protection for the development of type 1 diabetes mellitus,70 , 71 suggesting a spectrum of immunomodulatory roles of type I IFN-related molecules that span from the development of autoimmunity to susceptibility to life-threatening viral infections.
The presence of neutralizing autoantibodies to certain type I IFNs, mainly IFN-α2 and IFN-ω, was recently demonstrated in 101 out of 987 (10%) patients with severe outcomes of COVID-19, including death, who were predominantly male (94%).72 Interestingly, in 5 of these patients, the authors were able to demonstrate that the autoantibodies preceded the development of COVID-19, suggesting their development is a cause rather than a consequence of the viral infection. Furthermore, none of the patients with asymptomatic or mild COVID-19, and only 4 of 1227 healthy individuals had detectable type I IFN autoantibodies.72 In addition, none of the patients with LOF mutations affecting IFN pathways had neutralizing antibodies against type I IFN, strongly suggesting there seem to be at least 2 independent mechanisms by which dysfunctional IFN signaling leads to an increased susceptibility to life-threatening COVID-19.67 Previous studies have found that approximately 25% of patients with SLE have anti-IFN antibodies.73, 74, 75, 76, 77 The most common type I IFN autoantibodies in SLE are against IFN-α2 and IFN-ω, as seen in severe COVID-19.77 In addition, some of these anti-IFN antibodies were shown to be effective at neutralizing type I IFN activity in vitro, and patients with neutralizing antibodies tended to have lower SLE disease activity.76 Whether patients with SLE and anti-IFN antibodies are more susceptible to contracting COVID-19 or experience worse outcomes remains to be elucidated.
Given the evidence that the lack of an appropriate type I IFN response is associated with worse outcomes and retrospective data suggesting improved inflammatory markers and a shorter duration of detectable virus in COVID-19 patients treated with IFN-α2b,78 various clinical trials assessing the efficacy of type I IFN therapy in COVID-19 are ongoing. A recent phase 2 trial of nebulized IFN-β1a met its primary outcome of clinical improvement in COVID-19.79 In contrast, interim results of the World Health Organization Solidarity trial suggest IFN-β-1a was not effective at improving COVID-19 overall mortality, initiation of mechanical ventilation, or duration of hospital stay.80 However, it is possible that the timing of administration is crucial to ensure the benefit of exogenous type I IFN administration in COVID-19, as an early IFN surge may be needed to achieve optimal antiviral effects, whereas a delayed response could contribute to the deleterious hyperinflammatory response.81, 82, 83 This hypothesis may help explain some of the contradictory findings with respect to type I IFN in COVID-19, and inconsistent definitions of severe COVID-19 likely also contributes to the dissimilar observations.84 It may be that type I or type III IFN pathway-enhancing agents are beneficial in the early stages of SARS-CoV-2 infection, while immunosuppressive drugs, such as Janus kinase (JAK) inhibitors, anti-IL1 drugs, or sGC would provide the most benefit at treating the excessive and deleterious inflammatory response (ie, cytokine storm) that ensues in later phases of COVID-19 course.85, 86, 87, 88, 89, 90, 91
SARS-CoV-2 enters the host cells by binding to ACE2 in the cell membrane, hence the viral tropism depends on the level of ACE2 expression in each cell type. For instance, ACE2 expression is abundant in type II pneumocytes, enterocytes, and nasal goblet secretory cells. Interestingly, ACE2 has been postulated as an ISG, as IFN-α drives ACE2 expression in human upper airway basal cells, which would suggest potential deleterious effects of type I IFN by eliciting an increased risk of SARS-CoV-2 infection and viral dissemination.92 However, this issue is not settled as a recent study suggested that the ACE2 isoform that is induced by IFN-α, designated by the investigators as dACE2, corresponds to a novel truncated version that does not confer tropism for SARS-CoV-2.93 Although not yet corroborated, it has also been proposed that as a consequence of the epigenetic dysregulation present in patients with SLE, demethylation of ACE2 can lead to overexpression and increased susceptibility to SARS-CoV-2, while demethylation of IFN-regulated genes and other genes related to cytokine expression may lead to the development of a cytokine storm in the setting of COVID-19.94
Finally, most studies evaluating the risk of viral infections in patients with SLE are observational and confounded by long-term sGC and immunosuppressant use.28 However, it is possible that the baseline increased IFN activity in SLE exerts a protective role against contracting or developing worse outcomes of COVID-19; hence, this concept should be investigated further.
Neutrophil extracellular traps
Neutrophil extracellular traps (NETs) are web-like chromatin fibers with microbicidal proteins and granule enzymes released by neutrophils as a host defense mechanism against microbes. NETs are of high relevance in SLE, as they can enhance inflammation and type I IFN responses.95 NETs are also thought to potentiate thrombosis in antiphospholipid syndrome.96 , 97 Recent studies have suggested a key role of dysregulated NETs in COVID-19. Zuo et al identified that circulating NET-specific markers were significantly elevated in COVID-19 patients compared to healthy controls and in patients with critical COVID-19 on mechanical ventilation compared to those with milder disease; in addition, sera from patients with COVID-19 can trigger NET formation when exposed to control neutrophils in vitro.98 Similarly, Middleton et al demonstrated a correlation between plasma NETs and severity of respiratory manifestations of COVID-19.99 NETs are also abundant in respiratory secretions and lung tissue from patients with COVID-19, a process that may be driven by SARS-CoV-2-induced neutrophil activation and NET release. This inflammatory reaction could contribute to microthrombi formation in the lungs in COVID-19.99, 100, 101 Therapeutic interventions to dissolve NETs or prevent their release may be beneficial in managing severe COVID-19. A clinical trial evaluating dipyridamole, an antiplatelet agent and adenosine A2A receptor agonist with NET-suppressing properties,102 is ongoing (NCT04391179).
Antiphospholipid antibodies and thrombosis
Various observational studies have identified a high prevalence of antiphospholipid antibodies in hospitalized patients with COVID-19. Lupus anticoagulant positivity has been commonly found in patients with COVID-19, ranging from 42% to 83% in severe and critical COVID-19, although the prevalence may be lower when patients with milder forms are included.103, 104, 105, 106 The presence of IgG or IgM anti-cardiolipin and anti-beta2-glycoprotein I antibodies in patients with COVID-19 seems to be less prevalent and more variable across different studies, ranging from 0% to 13%.104 , 105 , 107 , 108
Interestingly, there has been conflicting evidence on how well the presence of antiphospholipid antibodies correlate with clinically significant thrombotic episodes, with various initial studies suggesting that these represent innocent bystanders instead of pathogenic antibodies.103, 104, 105 , 107, 108, 109, 110, 111 However, a recent study has demonstrated a potential pathogenic role of antiphospholipid antibodies in severe COVID-19. This cross-sectional study showed that 50% of hospitalized patients with COVID-19 had antiphospholipid antibodies, and higher titers were associated with elevated circulating NET markers and a more severe COVID-19 course.112 In addition, IgG fractions of antiphospholipid antibodies promoted NET release in vitro and induced accelerated venous thrombosis in mice.112 Nonetheless, there is still a lack of longitudinal studies assessing the persistence of antiphospholipid antibodies several weeks after COVID-19 diagnosis,108 and it is possible that this represents a transient event as it has been demonstrated in the setting of other infections.113, 114, 115
Dysregulation of the complement system
Complement dysregulation is a classic feature of SLE, and hypocomplementemia is a marker of disease activity.14 Complement activation has been associated with the excessive inflammatory response seen in patients with severe COVID-19, and the presence of a complement-mediated microvascular injury syndrome has been proposed based on the observed pattern of tissue damage.11, 12, 13
SARS-CoV-2 is thought to predominantly trigger the lectin and alternative complement pathways, although the classical complement pathway could also be activated in this setting by immune complexes.116 The C3a and C5a anaphylatoxins are potent inflammatory mediators and chemoattractants. C5a plasma levels were shown to rise proportionally to COVID-19 severity, suggesting sustained complement activation, likely triggered by SARS-CoV-2 antibodies and high levels of C-reactive protein.117 Additionally, COVID-19 patients have a large number of monocytes and neutrophils in bronchoalveolar lavage expressing the C5a receptor (C5aR1), suggesting a role of C5a in cell recruitment to the inflamed tissues.117 C5a may help generate thrombogenic NETs, promoting a complement and/or NET-driven cycle that leads to immunothrombosis.116
Disorders of the complement system can be genetic or acquired. Age-related macular degeneration, in which the complement system is overactive, is associated with worse COVID-19 outcomes. In addition, genetic variants previously reported in association with age-related macular degeneration were found to also predispose to hospitalization for COVID-19. Variants affecting the C3 gene were protective, whereas complement decay-accelerating factor (CD55) variants were associated with adverse outcomes of COVID-19.118 Conversely, patients with complement deficiency disorders may have a milder disease course.118
Together, these findings suggest a detrimental role of hyperactive complement. Therefore, a role of complement inhibitors to target thromboinflammation in COVID-19 has been suggested, and clinical trials assessing various agents are ongoing.119, 120, 121 Results from a small single-arm study of narsoplimab, a mannan-binding lectin associated serine protease-2 (MASP-2) blocker, are encouraging.122 Similarly, although data remain limited, eculizumab therapy also seems to improve clinical outcomes and biomarkers of inflammation and coagulation in patients with severe COVID-19.123 , 124
The mechanistic (mammalian) target of rapamycin pathway
Mechanistic (mammalian) target of rapamycin (mTOR) is a ubiquitous kinase and nutrient sensor that modulates cell differentiation, growth, proliferation, and survival. The mTOR pathway has been shown to regulate T‑cell and macrophage differentiation, and is thought to play a critical role in the pathogenesis of autoimmune and inflammatory diseases such as SLE.125 Accordingly, phase 1/2 trials of agents blocking the mTOR pathway, including N-Acetylcysteine (NAC) and rapamycin, have demonstrated potential benefits in SLE.126 , 127 Interestingly, a role of mTOR in the dysregulated inflammatory response in COVID-19 has been postulated.59 , 128 For instance, mTOR signaling has been shown to be decreased in pDCs from COVID-19 patients, on the basis of reduced ribosomal protein S6 (pS6) expression, translating into impaired IFN-α production by these cells which may negatively impact the host antiviral response (Fig 1).59
Conversely, it has been hypothesized that mTOR pathway hyperactivation in certain conditions such as obesity may enhance SARS-CoV-2 replication, providing at least a partial explanation for worse COVID-19 outcomes in obese patients.129 Therefore, targeting the mTOR pathway may reduce SARS-CoV-2 replication and inhibit the deleterious immune hyperactivation by reducing hyper-reactive T cells, while maintaining regulatory T (Treg) cell number and function in COVID-19.130 In agreement with this hypothesis, hospitalized patients with critical COVID-19 treated with NAC showed significant clinical improvement and reduction of inflammation markers, suggesting a beneficial effect of NAC in COVID-19, possibly mediated by mTOR inhibition.131 Limited observational studies of patients with tuberous sclerosis complex and/or lymphangioleiomyomatosis on long-term mTOR inhibitors (sirolimus or everolimus) have not identified an increased risk of COVID-19 or poor outcomes of the infection132 , 133 and clinical trials of mTOR inhibitors in COVID-19 are ongoing. However, whether activation of the mTOR pathway plays a role in SARS-CoV-2-infected patients with SLE remains to be elucidated.
Dysregulated adaptive immune responses
Lymphopenia is a common feature of SLE, thought to be due to complement-mediated or antibody-dependent cytotoxicity, excess apoptosis, and decreased lymphopoiesis.134 In addition, T cell function is also impaired in SLE, which may predispose these patients to infections (see the previous section on Relationship between SLE and risk of viral infections). Reversible lymphopenia has been observed in patients with COVID-19, especially those with severe disease.135 Although transient lymphopenia is common in the setting of viral infections, COVID-19-associated peripheral lymphopenia may persist for longer and be more severe than in other viral illnesses.136 Among the potential mechanisms that contribute to lymphocyte depletion in COVID-19 are infection of lymphocytes by SARS-CoV-2, exhaustion, and induction of apoptosis by cell hyperactivation and/or an increase in proinflammatory cytokines and pro-apoptotic signals.135, 136, 137 Although more pronounced in CD8+ T cells, lymphopenia has also been shown to affect CD4+ T cells.136 , 137
Various studies have also identified functional impairment or alterations in the differentiation status of T cells, with marked heterogeneity in immune cell responses. T cells in COVID-19 may range from an exhausted to an overactive phenotype.59 , 136, 137, 138 It has been proposed that a more severe disease course could be associated with a reduced CD8+ T cell pool and less activated T cells, with increased expression of co-inhibitory signals including PD1, TIM3, CTLA4, and CD38.136 , 139 However, differentiating between an exhausted phenotype and hyperactive T cells represents a challenge as they both demonstrate increased expression of inhibitory receptors. A recent multi-omics study identified that certain CD8+ subpopulations correlated with COVID-19 severity, with an increase of naïve clusters and lower activated effector T cells identified in severe cases when compared to patients with moderate disease.140 Another study using high-dimensional flow cytometry identified distinct immunotypes related to disease severity in hospitalized patients with COVID-19. Interestingly, the immunotype characterized by robust CD4+ T cell activation, a paucity of circulating T follicular helper cells, and highly activated or exhausted CD8+ T cells was associated with more severe disease.137
A potential role for T helper 17 (Th17) cells in COVID-19 has also been suggested, and significant skewing towards a Th17 functional phenotype with decreased Treg levels have been described.136 , 138 , 141 , 142 Similarly, patients with SLE have impaired Treg cells, greater numbers of Th17 cells and increased production of IL-17, which seems to correlate with disease activity.143 , 144
A central immunopathogenic role of dysregulated B cell responses in COVID-19 is also likely. A stronger B-cell immune response in patients with severe COVID-19 compared to milder disease has been described.145 Poor COVID-19 outcomes are associated with suppression of germinal centers, extrafollicular B cell activation, and a large expansion of the antibody-secreting cell compartment, similar to what is seen in SLE.59 , 137 , 140 , 146 , 147 However, whether infection-induced autoreactive B cell responses persist after the acute phase of COVID-19 or if they contribute to long-lasting symptoms experienced by some patients with COVID-19, the so-called “long-haulers”, remain to be determined. Moreover, the effect of B-cell depleting therapy on COVID-19 outcomes needs to be addressed, although very limited data to date have suggested the potential for detrimental effects.148, 149, 150
Overall, the findings of pathogenic adaptive immune responses in COVID-19 further support the notion that the timely implementation of immunomodulatory therapy in selected patients may be beneficial.
COMMONLY USED DRUGS IN SLE AND PREDISPOSITION TO VIRAL INFECTIONS
SLE management involves the use of multiple therapeutic strategies to treat the specific manifestations, lower disease activity, and prevent irreversible organ dysfunction.151 General standard treatment strategies involve the use of antimalarials, non-biologic and biologic immunosuppressive agents, and sGC, if necessary. sGC are generally considered a first-line treatment in the management of organ- and life-threatening manifestations of SLE. Although sGC are effective in decreasing disease activity, their undesirable side effect profile has led to widely accepted recommendations to limit the dose and duration of treatment as much as possible.2 , 152, 153, 154 Multiple studies to date have reported significantly increased risk of serious infections in patients on sGC, with doses as low as 10 mg prednisone-equivalent, although this mostly corresponds to bacterial infections.28 , 155, 156, 157, 158, 159, 160
Hydroxychloroquine (HCQ) use is recommended in most patients with SLE, owing to multiple health benefits in patients with SLE and overall safety.161, 162, 163, 164 Various observational studies have indicated a protective effect of HCQ against serious infections in SLE.165, 166, 167, 168 In vitro studies have also suggested potential anti-viral effects of HCQ by means of increasing lysosomal pH and preventing post-translational modification of synthesized proteins that are crucial for replication and dissemination of viruses.165 , 167 , 169 However, human studies have failed to identify any benefit of HCQ in preventing or managing viral infections, including dengue, chikungunya, and SARS-CoV-2.170 , 171
Azathioprine (AZA), mycophenolate mofetil (MMF), and CYC are commonly used in SLE to manage moderate to severe manifestations. In a retrospective study from France, exposure to CYC led to an increased incidence of herpes zoster in patients with SLE during the first year after initiating therapy.172 A systematic review and meta-analysis identified a higher incidence of infections in the CYC compared to the MMF group.173 However, a large propensity-score matched study showed no significant differences in rates of infection or mortality between Medicaid patients with SLE using CYC vs MMF after 6 months of initiation of therapy.174 A study from the Hopkins Lupus Cohort that followed 214 patients after MMF initiation reported an increased risk of developing bacterial infections but no change in the risk of viral infection.175 Furthermore, a recent review did not find sufficient evidence to conclude that AZA, MMF, or CYC increased the risk of acute respiratory viral adverse events in patients with SLE or other rheumatic diseases.156 Tacrolimus, a calcineurin inhibitor used as a single agent or in combination with MMF in SLE, has been associated with a relatively low incidence of severe infections in various reports, although data are scarce.156 , 176 , 177 A comparison between SLE patients on sGC and tacrolimus vs those on sGC and CYC showed a similar incidence rate of herpes zoster and varicella between the 2 groups.178
Belimumab, a B lymphocyte stimulator inhibitor, is currently the only biologic approved for use in SLE.179 Based on data from randomized controlled trials and open-label extensions, there is no suggestion of a significantly increased risk of severe respiratory viral infections with Belimumab use.156 Rituximab (RTX), a B-cell depleting agent, has been associated with progressive multifocal leukoencephalopathy arising from John Cunningham virus reactivation.159 , 180 Additionally, hepatitis B (HB) reactivation is a potentially life-threatening complication from RTX therapy in patients with positive HB surface antigen or HB anticore antibody.181 Although data on other viral infections with RTX use are scarce, the frequency of upper respiratory tract infections is variable among trials but generally similar to the placebo arms.156 , 182 , 183 Recently, 2 small studies reported high rates of severe COVID-19 and mortality in patients on RTX for various indications.148 , 149 However, larger studies and longer follow-up are needed to confirm these observations.
Anifrolumab, a type I IFN blocking agent, is awaiting FDA approval for use in SLE.184 Overall, in the randomized controlled trials, there were increased rates of herpes zoster, upper respiratory tract infections, nasopharyngitis, bronchitis, and influenza in the anifrolumab group, although the differences were not statistically significant.156 , 185 , 186 Further longitudinal studies are needed to assess the risk of viral infection in anifrolumab-receiving patients with SLE; however, considering its mechanism of action, an increased risk of viral infections with the use of anifrolumab is biologically plausible.
EPIDEMIOLOGY AND OUTCOMES OF COVID-19 IN PATIENTS WITH SLE
As COVID-19 was increasingly recognized as a rapidly spreading global threat, the urgent need to describe the characteristics and outcomes of patients with rheumatic diseases became evident. Early reports suggesting a potential beneficial role of chloroquine and HCQ, which are commonly used in patients with rheumatic diseases, also drove the need to evaluate this population closely. The first studies on patients with SLE and COVID-19 emerged from the heaviest hit regions in the early phases of the pandemic and consisted of mostly case reports or small case series (Table Ⅰ ).
Table Ⅰ.
Main published studies by October 31, 2020 including patients with SLE and presumptive or confirmed COVID-19
| Reference and country/region | Study timeline* | Number of SLE patients included and COVID-19 status | Age (years) and gender (% female patients) | % Medication use | Hospitalizations and deaths due to COVID-19 | Main findings |
|---|---|---|---|---|---|---|
| Chen et al230 Wuhan, China |
Feb 29 | N = 101 (LN only) Confirmed: 2 |
Median age: 42 Gender: F: 89 (88%) |
HCQ: 52 (51%) ISx: aggregate data NA sGC: 95 (94%) |
Hospitalization: 2/2 (100%) Death: 0 |
Low prevalence of confirmed COVID-19 in lupus nephritis patients during the Wuhan peak |
| Singer et al191 USA |
Jan 20 to Jul 13 | N = 35 Confirmed: NA Presumptive: NA | NA for SLE subgroup | NA for SLE subgroup | NA for SLE subgroup | HCQ did not prevent COVID-19 in patients with SLE |
| Huang et al251 Wuhan, China |
Jan 29 to Mar 8 | N = 3 Confirmed: 3 |
NA for SLE subgroup | NA for SLE subgroup | Hospitalization: 3/3 (100%) Death: 1/3 (67%) |
Age, male gender and comorbidities are risk factors for severe COVID-19 |
| Holubar et al189 Montpellier, France |
Feb 1 to Apr 24 | N = 120 Confirmed: 0 Presumptive: 30 |
Age: On HCQ: 42 ± 12 Not on HCQ: 52 ± 12 Gender: F: 110 (92%) |
HCQ: 72 (60%) sGC: 50 (42%) |
Hospitalization: 0 Death: 0 |
No severe forms of COVID-19 were identified |
| Gendebien et al193Liège, Belgium | Feb 4 to Jun 6† | N = 225 Confirmed: 5 Presumptive: 13 |
Mean age ± SD: 52 years ± 14.9 Gender: F: 209 (93%) |
HCQ: 151 (68%) ISx: 28 (31%) sGC: 23 (25%) |
Hospitalization: 2/18 (11%) Death: 0 |
sGC dose was associated with COVID-19 diagnosis and hospitalization |
| Bozzalla Cassione et al194 Northern Italy |
Feb 15 to Apr 29† | N = 165 Confirmed: 4 Presumptive: 8 |
Mean age, range: 53, 25–81 Gender: F: 112 (84%) |
HCQ use: 127 (77%) ISx: 53 (32%) sGC: 93 (56%) |
Hospitalization: NA‡ Death: 0 |
No protective effect of HCQ against COVID-19 in SLE patients |
| Fredi et al196 Brescia, Italy |
Feb 24 to May 1 | N = 12 (10% of 117 patients with rheumatic diseases) Confirmed: 5 Presumptive: 7 |
NA for SLE subgroup | NA for SLE subgroup | NA for SLE subgroup | Poor outcomes of COVID-19 were associated with older age and the presence of comorbidities |
| Favalli et al210 Lombardy, Italy |
Feb 25 to Apr 10 | N = 62 Confirmed: 0 Presumptive: 8 |
Mean age: 44 Gender: F: 56 (91%) |
HCQ: 30 (48%) ISx: 52 (84%) sGC 46 (75%) |
Hospitalization: 0 Death: 0 |
Very low impact of COVID-19 in SLE patients |
| D'Silva et al206 Massachusetts, USA |
Mar 1 to Apr 8 | N = 10 Confirmed: 10 |
NA for SLE subgroup | NA for SLE subgroup | NA for SLE subgroup | COVID-19 outcomes similar between patients with and without rheumatic diseases, except for ICU/MV |
| Wallace et al205 Michigan, USA |
Mar 1 to Apr 20 | N = 5 Confirmed: 5 |
Mean age, range: 54, 26–67 Gender: F: 5 (100%) |
HCQ: 4 (80%) ISx: 3 (60%) sGC: 4 (80%) |
Hospitalization: 4/5 (80%) Death: 1/5 (20%) |
Patients with quiescent SLE may develop severe COVID-19 |
| Santos et al200 León, Spain |
Mar 1 to Jun 1 | N = 5 (13% of 38 patients with rheumatic diseases). Confirmed: 5 |
NA for SLE subgroup | NA for SLE subgroup | Hospitalization: 5 (100%) Death: 1 (20%) |
Comorbidities, rheumatic disease activity and laboratory abnormalities were associated with mortality |
| Gentry et al190 USA |
Mar 1 to Jun 30 | N = 7117 (22% of 32,109 patients with rheumatic diseases) Confirmed: 23 |
NA for SLE subgroup | HCQ: 2642 (37%) ISx and sGC: NA for SLE subgroup |
NA for SLE subgroup | HCQ was not associated with COVID-19 prevention or improvement in outcomes of the infection |
| Montero et al195 Madrid, Spain |
Mar 4 to Apr 24 | N = 9 (15% of 62 patients with various autoimmune/ inflammatory diseases) Confirmed: 9 |
NA for SLE subgroup | NA for SLE subgroup | Hospitalized: 6/9 (67%) Death: 2 (22%) |
Factors associated with COVID-19 hospitalization: Baseline sGC use, male sex, preexisting lung disease |
| Emmi et al252 Tuscany, Italy |
Apr 1 to Apr 14 | N = 117 Confirmed: 0 Presumptive: 4 |
NA for SLE subgroup | NA for SLE subgroup | Hospitalized: 0 Death: 0 |
No clear evidence of increased risk of COVID-19 in patients with SLE |
| Konig et al188 Worldwide (C-19-GRA) |
Apr 17 | N = 80 Confirmed/ presumptive status: NA |
Age ≤65: 69 (86%) Gender F: 72 (90%) |
HCQ/CQ: 51 (64%) ISx and sGC: NA for SLE subgroup |
Hospitalization: 45/80 (56%) Death: 0 |
No difference in the frequency of COVID-19 hospitalizations based on HCQ use |
| Gianfrancesco et al203 Worldwide (C-19-GRA) |
Mar 24 to Apr 20 | N = 85 (14% of 600 patients with rheumatic diseases) Confirmed: 80 Presumptive: 5 |
NA for SLE subgroup | NA for SLE subgroup | Hospitalized: 48/85 (56%) Death: NA for SLE subgroup |
Age, comorbidities and sGC use are associated with increased odds of hospitalization |
| Mathian et al187 France |
Mar 29 to Apr 6 | N = 17§ Confirmed:17 |
Mean age, range: 54 (27–69) Gender: F: 13 (76%) |
HCQ: 17 (100%) ISx: 7 (41%) sGC: 12 (71%) |
Hospitalization: 14/17 (82%) Death: 2/14 (14%) |
No role of HCQ preventing severe COVID-19 in patients with SLE |
| Gartshteyn et al204 New York, USA |
Apr 26 | N = 18 Confirmed: 10 Presumptive:: 8 |
Mean age ± SD: 41 ± 11 Gender: F: 16 (89%) |
HCQ: 13 (72%) ISx: 15 (83%) sGC: 7 (39%) |
Hospitalization: 7/18 (39%) Death: 0 |
COVID-19 severity was not affected by SLE medication use. |
| Zen et al253 Padua, Italy |
Apr 9 to Apr 25 | N = 397 Confirmed: 1 Presumptive:14 |
Mean age ± SD: 48 ± 13 Gender: F: 340 (86%) |
HCQ: NA ISx: aggregate data NA sGC: 42 (11%) |
Hospitalization: 1/1 (100%) Death: 0 |
COVID-19 incidence was comparable to the general population |
| Fernandez-Ruiz et al192 New York, USA |
Apr 13 to Jun 1 | N = 226 Confirmed: 41 Presumptive: 42 |
Confirmed: Mean age ± SD: 47 ± 17 Gender: F: 38 (93%) Presumptive: Mean age ± SD: 41 ± 13 Gender: F: 39 (93%) |
Confirmed: HCQ: 32 (78%) ISx: 24 (59%) sGC: 18 (44%) Presumptive: HCQ: 33 (79%) ISx: 24 (57%) sGC: 5 (12%) |
Confirmed only: Hospitalization: 24/41 (59%) Death: 4/41 (10%) |
Predictors of hospitalization in confirmed COVID-19 patients: non-white race, the presence of ≥1 comorbidities and BMI per increase in kg/m2 |
| Marques et al197 Brazil |
May 19 to Jun 16 | N = NA for SLE subgroup | NA for SLE subgroup | NA for SLE subgroup | Hospitalized: NA for SLE subgroup Death: 4 |
No rheumatic disease-specific factors were associated with death from COVID-19. High frequency of comorbidities in deceased patients. |
| Cho et al199 Asia Pacific Region |
Jun 3║ | N = 3375 Confirmed: 3 |
Confirmed: Mean age: 40 ± 16 Gender: F: 3 (100%) |
Confirmed: HCQ: 2 (67%) ISx: 2 (67%) sGC: 3 (100%) |
Hospitalized: 3/3 (100%) Death: 1/3 (33%) |
Only 3 COVID-19 cases were identified in a cohort of 3375 SLE patients. All patients required escalation of SLE therapy around the time of COVID-19 diagnosis |
| Pablos et al208 Spain |
NA | N =2253 Confirmed: 17 |
Confirmed: Mean age, IQR: 51 (42–66) Gender: F: 77% |
NA for SLE subgroup | NA for SLE subgroup | Low prevalence of confirmed COVID-19 in SLE patients compared to most systemic autoimmune diseases |
Abbreviations: BMI, body mass index; COVID-19, coronavirus disease 2019; F, female; HCQ, hydroxychloroquine; ICU, intensive care unit; IQR, interquartile range; ISx, immunosuppressants; LN, lupus nephritis; MV, mechanical ventilation; NA, not available; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; sGC, systemic glucocorticoids; SLE, systemic lupus erythematosus.
Confirmed: patients who had positive diagnostic testing for SARS-CoV-2.
Presumptive: patients with symptoms suggestive of COVID-19 (at the authors’ discretion) who did not undergo diagnostic testing for SARS-CoV-2.
Unless otherwise specified, if the start date of the observation period is not reported in the article, the end of observation date is presented in the table.
Latest date the article was received by the journal.
One patient was admitted to the intensive care unit. Other patients had a milder course but it is unclear if they were hospitalized.
Sixteen patients met the classification criteria for systemic lupus erythematosus (SLE) and one patient had antiphospholipid syndrome with additional features of SLE.
Date survey was sent.
Mathian et al described 17 patients with SLE who were diagnosed with COVID-19 in France between March 29 and April 6, most of whom were on long-term HCQ and had therapeutic levels of the drug.187 Seven (41%) patients required admission to an intensive care unit, and 2 out of 14 hospitalized patients died of COVID-19; notably, comorbidities were highly prevalent in these SLE patients, as was use of sGC (71%) and immunosuppressants (41%), and most patients had clinically quiescent SLE. This study represented one of the first to note that patients with SLE on HCQ were not protected against COVID-19.187 Several other groups have now also suggested the lack of benefit of HCQ against contracting or developing severe COVID-19 in patients with SLE and other rheumatic diseases.188, 189, 190, 191, 192, 193, 194
A retrospective study from Spain included 62 patients with several different rheumatic or autoimmune diseases, nine of which had SLE. They found no statistically significant between-group differences for rheumatologic diagnosis or baseline use of immunosuppressive therapy except for sGC use, which was more frequent in hospitalized patients. SLE was not a risk factor for severe COVID-19 requiring hospitalization, but male sex, previous lung disease, and sGC use (> 5 mg/day of prednisone) were significantly associated with hospital admission.195 Similarly, a study from Belgium which included 18 patients with confirmed or suspected COVID-19 did not find differences in the proportion of patients who developed COVID-19 between patients on immunosuppressants and those not on these medications. However, sGC dose was found to be positively associated with a positive reverse transcription polymerase chain reaction (RT-PCR) test for COVID-19, hospitalization, and various COVID-19 symptoms.193 Several other studies from Spain, Italy, France, and Brazil have also suggested that the main risk factors for poor COVID-19 outcomes are similar to those previously reported in the general population, including age and the presence of comorbidities.189 , 196, 197, 198 Additional potential risk factors suggested by studies of SLE and other autoimmune diagnoses included the presence of interstitial lung disease, moderate or high rheumatic disease activity (or flare preceding the COVID-19 diagnosis), history of neuropsychiatric lupus, and known exposure to a confirmed COVID-19 case.199, 200, 201 However, the small sample size, lack of confirmatory testing for many of the included patients, selection biases, insufficient identification and adjustments for confounders, and several other limitations from these observational data preclude from making definitive statements about these observations.
In response to the scarcity of data on the impact of COVID-19 in patients with immune-mediated diseases, a number of registries were established to better characterize these patients and assess their outcomes. The largest of these registries addressing rheumatic diseases is the COVID-19 Global Rheumatology Alliance (C-19-GRA). The C-19-GRA was formed over the course of a few days in response to an urgent need for information, as the rheumatology community gathered in social media.202 The largest C-19-GRA publication to date reported on the first 600 patients entered to the registry, including 85 patients with SLE, of whom 55% were hospitalized.203 This study found that a prednisone dose ≥10 mg/day was associated with higher odds of hospitalization in patients across all rheumatic diseases. Immunosuppressant use was not found to be associated with hospital admission for COVID-19, with the exception of tumor necrosis factor inhibitor users, in whom the odds of hospitalization were lower.203
As New York City (NYC) was the initial epicenter of the pandemic in the United States, many patients living with rheumatic diseases were affected by COVID-19. Gartshteyn et al published the first case series describing patients with SLE and COVID-19 in NYC. The study included 10 patients with real-time RT-PCR confirmed COVID-19 and 8 with suspected infection; 7 of these patients were hospitalized. Most patients (83%) in this case series were taking immunosuppressants, 39% were on sGC, and 61% had lupus nephritis. Although limited by the small number of cases, the study did not find significant differences in immunosuppressant use in patients with mild vs severe COVID-19.204 As COVID-19 rapidly extended to other regions of the United States, other groups published on the outcomes of patients with rheumatic diseases and COVID-19. Wallace et al described their COVID-19 experience at a tertiary care academic center in Michigan, reporting 5 patients with SLE, of whom 4 were hospitalized, 3 required invasive ventilation, and 1 died of COVID-19. Overall, when compared to 31 patients with various rheumatic diseases, patients with SLE and COVID-19 seemed to have worse outcomes in this study; however, SLE patients were noted to have a high prevalence of comorbidities, sGC use, and more likely to be African-American, which are all known risk factors for hospitalization and mortality in COVID-19.205
To further close the information gaps concerning the impact of COVID-19 in patients with immune-mediated diseases in one of the heaviest hit regions in the world by the initial phases of the pandemic, our NYC-based institution established a prospective cohort of patients with immune-mediated diseases, the Web‐based Assessment of Autoimmune, Immune‐Mediated, and Rheumatic Patients during the COVID‐19 Pandemic (WARCOV). An initial report on patients with various immune-mediated diseases from the WARCOV cohort, which did not include any patients with SLE, identified sGC use as one of the main factors associated with higher odds of hospitalization.157 We later reported the characteristics and COVID-19 outcomes of patients with SLE, including 41 confirmed and 42 suspected cases of COVID-19, as well as 19 patients who were tested for COVID-19 and were negative, and 124 patients with SLE from our lupus registry who did not develop COVID-19 symptoms on prospective follow-up.192 Out of the 41 patients with RT-PCR confirmed COVID-19, 24 patients with SLE required hospitalization. Notably, no SLE-specific factors, such as immunosuppressant use, were noted to increase the odds of hospitalization. However, there was a higher proportion of patients on sGC in the hospitalized (54.2%) compared to the ambulatory group (29.4%), although the difference was not statistically significant. Non-white race, having 1 or more comorbidities, and body mass index were identified as independent predictors of hospitalization in our patients with SLE and COVID-19, similar to the general population.192 These findings were in agreement with smaller studies assessing outcomes of COVID-19 in patients with SLE, as previously discussed.
Several studies have compared patients with and without rheumatic/autoimmune diseases to investigate differences in risk of contracting SARS-CoV-2 and experiencing poor outcomes of the disease. In a matched study of 52 patients with various rheumatic diseases, including 10 patients with SLE, compared to 104 without rheumatic diseases, D'Silva et al found that the proportion of patients who were hospitalized for COVID-19 and mortality from the disease were similar between the 2 groups; however, patients with rheumatic diseases had significantly higher odds of requiring mechanical ventilation or admission to the intensive care unit ventilation compared to patients without rheumatic diseases.206
Various studies have addressed the question of whether patients with autoimmune diseases, including SLE, increase the risk of contracting COVID-19. A recent large study from Milan, Italy, comparing 20,364 SARS-CoV-2 test-positive and 34,697 test-negative subjects, did not find an association between having an autoimmune disease (in aggregate), including SLE, and having a positive test for COVID-19.207 A study from 7 hospitals in Spain also suggested patients with SLE were not at a higher risk of testing positive for COVID-19 in the hospital setting compared to a reference population of 2.9 million people.208 In contrast with these observations, a meta-analysis of 7 case-control studies of patients with autoimmune diseases and COVID-19 showed 2-fold higher odds of contracting COVID-19 in this population compared to controls.209 On meta-regression analysis, sGC use was significantly associated with the risk of COVID-19. Furthermore, patients with SLE, Sjogren's syndrome, and systemic sclerosis, in aggregate, had a higher prevalence of hospitalization when compared with the other disease groups. Notably, sGC was highly prevalent in this group (60%).209
Overall, studies seem to suggest that most patients with SLE may not be at an increased risk of contracting COVID-19. However, patients with SLE have likely implemented more strict protective behaviors to avoid exposure to SARS-CoV-2 out of fear of having worse outcomes, so this element should be factored in when considering risk for developing COVID-19 in patients with SLE.201 , 210 Other than sGC use, there is no clear evidence to suggest that the SLE population is at risk of worse COVID-19 outcomes due to specific factors related to their underlying autoimmune disease. Although studies to date have significantly improved our understanding of the associations and outcomes of COVID-19 in the SLE population, it is important to note that there are several limitations to these observational data and the results should be interpreted with caution.
ASSOCIATION OF COVID-19 WITH SLE FLARES AND de novo SLE
There have been reports in the literature of COVID-19 shortly preceding a de novo diagnosis of SLE, presenting concomitantly or mimicking SLE, raising the possibility of SARS-CoV-2 being a trigger of autoimmunity, as it has been postulated for other viruses.19 , 111 , 211 However, we need to use caution when making a diagnosis of SLE in patients with COVID-19 for various reasons. Certain clinical diagnostic criteria of SLE overlap with COVID-19 symptoms. Also, autoantibodies can occur in response to infections, and these are usually transient and of unclear significance in this setting.113 , 114 , 212 Hence, longitudinal evaluation of these patients is required to offer insights into the association between COVID-19 and de novo SLE.
Similarly, various reports have indicated that COVID-19 may worsen SLE manifestations.213, 214, 215 However, attributing SLE flares to a biologic mechanism is challenging because many of these patients have had greater difficulty accessing health care during the pandemic and may suffer worsened disease control due to lack of medical care or difficulty continuing their SLE medications, in addition to the psychosocial stressors of the pandemic. Therefore, it is currently unclear whether COVID-19 could predispose to SLE or cause a flare of disease in SLE patients. Long-term longitudinal studies are needed to ascertain these associations.
ANCESTRAL BACKGROUND, SOCIOECONOMIC FACTORS AND INDIRECT CONSEQUENCES OF THE COVID-19 PANDEMIC IN PATIENTS WITH SLE: CHALLENGES IN ACCESS TO HEALTH CARE, MEDICATION SHORTAGES, AND PSYCHOSOCIAL FACTORS
It is well established that SLE is more prevalent and severe in ancestrally African and Hispanic patients.3 In addition, patients with SLE from minority racial and ethnic groups are known to experience substantial inequities in care and are much less likely to enroll in clinical trials when compared to white patients, owing to structural racism, implicit bias, previous experiences of discrimination and injustices.2 , 216 The COVID-19 pandemic has magnified the impact of health disparities and barriers to health care experienced by marginalized populations around the world. Consequently, COVID-19 has disproportionately affected Indigenous communities, Black and Hispanic populations4 , 6 , 217, 218, 219, comparable to what has been identified in patients with SLE and COVID-19.192 , 220 Interestingly, a recent study suggested African ancestry populations showed a genetic predisposition for lower expression of both ACE2 and type 2 transmembrane serine protease, suggesting decreased susceptibility to contracting SARS-CoV-2 in this population221. Although these findings suggest genetic determinants of COVID-19 transmissibility and severity across populations exist, SDH are more likely responsible for the different outcomes in racial and ethnic minorities, as it has been suggested by a recent retrospective cohort study from New York.222 Therefore, assessing the impact of SDH on severity and mortality related to COVID-19 in patients with rheumatic diseases is essential.223, 224, 225, 226
Although telemedicine has played a significant role in securing continuity of care for patients with SLE and other rheumatic diseases during the pandemic-related lockdowns194 , 227 , 228, concerns have been raised about specific situations where a virtual consultation may be insufficient.229 For instance, patients with SLE require routine monitoring of laboratory parameters. New patients or those with urgent concerns may require a more thorough evaluation than what is feasible by telemedicine. Furthermore, special consideration should be given to those patients who lack reliable internet connection or access to smartphones or other devices suitable for telemedicine.
Even when imperfect, telemedicine has allowed patients with SLE to be evaluated by health care professionals, preventing major gaps in medical attention during the pandemic, which may lead to discontinuation of SLE therapies and subsequent flares. This concept was exemplified in a study from Wuhan, China, where 60% of 101 respondents with lupus nephritis had been unable to attend their rheumatology appointments. In addition, 25% of patients discontinued their medications, mostly due to limited access to health care, and 5% experienced a disease flare. Interestingly, only 2 patients in this study contracted SARS-CoV-2 and both had a mild COVID-19 course.230 Similarly, in a study of 1040 patients with SLE in India, over 50% of patients had missed their follow-up appointments, 37% were unable to perform routine laboratory exams, 40% needed to change their medications due to lack of availability, and 25% presented financial difficulties during the lockdown period,231 suggesting additional sources of stressors experienced by these patients.
HCQ is a mainstay of treatment in SLE, as it is associated with multiple health benefits in this population, including reducing the risk of flares and organ damage.163 , 232 In the early phases of the COVID-19 pandemic, limited data including in vitro and small observational studies suggested a potential benefit of HCQ in COVID-19.233 , 234 Multiple recent studies, including observational data from patients with immune-mediated diseases on long-term HCQ as well as large randomized clinical trials, have consistently demonstrated the lack of efficacy of HCQ in preventing the viral infection or improving any COVID-19-related outcomes.171 , 190 , 235, 236, 237, 238 However, for several weeks after the preclinical studies and limited observational data came to light, HCQ shortages ensued in many countries as its use was redirected toward prophylaxis or management of COVID-19, leading to inadequate supplies of the drug for many patients with SLE worldwide.239 , 240
An electronic survey distributed to the SLE International Collaborating Clinics members with SLE-affiliated centers aimed to evaluate physicians’ experiences with HCQ shortages during the pandemic.241 Out of 31 responses, 55% reported HCQ shortages among patients with SLE. Most respondents (65%) in this study had been contacted by patients and pharmacies regarding difficulties accessing HCQ.241 Similarly, a national survey to Canadian rheumatologists in April, 2020 found that 50-94% of respondents, depending on the region, had been contacted by pharmacies or patients regarding difficulties accessing HCQ.242 In a patient-centered study in Germany, 70% of 369 respondents expressed concerns about being unable to receive HCQ prescriptions, and 9% had already reduced their HCQ dose in an attempt to overcome potential drug supply issues.243
One of the main concerns that HCQ shortages prompted was the risk of SLE flares, which are known to occur as soon as 2 weeks after drug discontinuation for most patients with SLE, especially in the younger SLE population.163 , 244 In addition, due to fears of contracting SARS-CoV-2, many patients fail to seek prompt medical attention in emergent and urgent situations.245 , 246 A report from Malaysia found a 65.4% decline in hospitalizations in patients with SLE during the lockdown period compared to 2019 rates. However, the patients with SLE who presented to the hospital in 2020 were significantly sicker when compared to those admitted in 2019 with respect to SLE Disease Activity Index, intensive care unit requirement, and mortality. Strikingly, only 1 death was attributed to COVID-19.247 These findings are likely multifactorial; while patients with SLE may have avoided presenting to the hospital due to fear of contracting COVID-19 until it was inevitable, it is also possible that different factors such as lack of close monitoring of clinical or laboratory parameters, issues with access or self-adjustments of the doses of SLE medications, have also contributed to higher severity and mortality rates in this population.
Finally, it is evident that the COVID-19 pandemic has had a profound psychosocial impact in patients with SLE. Multiple factors inherent to the pandemic have acted as stressors in the general population, potentially increasing the risk of mental health disorders; these include disinformation, uncertainty, collective fear, in addition to the declared states of emergency and lockdowns, resulting in financial concerns and social isolation.248 Patients with SLE have faced numerous additional challenges during the pandemic. The fears of worse outcomes if contracting COVID-19, as well as the aforementioned concerns about access to health care and medication availability in this population, may affect the emotional and mental health of patients with SLE even further. Accordingly, a study from Poland showed a higher risk of anxiety, depression, and sleep disorders in SLE patients when compared to non-SLE patients during the COVID-19 pandemic.249 In addition, in a cohort of patients with rheumatoid arthritis and SLE in the Philippines, a considerable proportion of patients were experiencing moderate to severe stress (12%), moderate to extremely severe anxiety (39%), and depression (28%).250
CONCLUSION
Many of the immune system pathways important to COVID-19 infection are active in SLE, providing a valuable comparison and lessons to be learned in instances when the two conditions co-exist. It seems that besides sGC use, most risk factors for worse outcomes of COVID-19 in patients with SLE are similar to those identified in the general population. However, the impact of additional factors, including those related to SDH, requires further study. It is possible that some of the factors in SLE offset one another, such as any potential protective effect from type I IFN being offset by immunosuppressive agents, for example. These complexities hold promise for a greater understanding of COVID-19 immunopathogenesis in the broader population, and lessons learned through years of human SLE research seem highly relevant to challenges presented by this new viral pathogen.
Acknowledgments
Conflict of interest: All authors have read the journal's authorship agreement and policy on disclosure of potential conflicts of interest. All authors have disclosed potential conflicts of interest.
TBN: Grants from the Colton Center for Autoimmunity, NIH (AR060861, AR057781, AR065964, AI071651), the Lupus Research Foundation, and the Lupus Research Alliance. TBN has received research grants from EMD Serono and Janssen, Inc., and has consulted for Thermo Fisher and Inova, all unrelated to the current manuscript. RFR and JP have nothing to disclose.
We would like to thank Drs. Bruce N. Cronstein, Arthur H. Fierman, and Mark Schwartz for revising some sections of the manuscript and improve readability.
References
- 1.Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L, Taylor DDH. Excess deaths from COVID-19 and other causes. Jama. 2020;324:1562–1564. doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruce IN, O'Keeffe AG, Farewell V, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the systemic lupus international collaborating clinics (SLICC) inception cohort. Ann Rheum Dis. 2015;74:1706–1713. doi: 10.1136/annrheumdis-2013-205171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Izmirly PM, Wan I, Sahl S, et al. The incidence and prevalence of systemic lupus erythematosus in New York County (Manhattan), New York: the Manhattan Lupus Surveillance Program. Arthritis Rheumatol. 2017;69:2006–2017. doi: 10.1002/art.40192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Millett GA, Honermann B, Jones A, et al. white counties stand apart: the primacy of residential segregation in COVID-19 and HIV diagnoses. AIDS Patient Care STDS. 2020;34:417–424. doi: 10.1089/apc.2020.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khazanchi R, Evans CT, Marcelin JR. Racism, not race, drives inequity across the COVID-19 continuum. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19933. [DOI] [PubMed] [Google Scholar]
- 7.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 8.Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. Jama. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jin JM, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11:6317. doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holter JC, Pischke SE, de Boer E, et al. Systemic complement activation is associated with respiratory failure in COVID-19 hospitalized patients. Proc Natl Acad Sci U S A. 2020;117:25018–25025. doi: 10.1073/pnas.2010540117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merrill JT, Erkan D, Winakur J, James JA. Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat Rev Rheumatol. 2020;16:581–589. doi: 10.1038/s41584-020-0474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahajan A, Herrmann M, Muñoz LE. Clearance deficiency and cell death pathways: a model for the pathogenesis of SLE. Front Immunol. 2016;7:35. doi: 10.3389/fimmu.2016.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bourgonje AR, Abdulle AE, Timens W, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19) J Pathol. 2020;251:228–248. doi: 10.1002/path.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. Jama. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 17.Tsokos GC. Systemic lupus erythematosus. N Engl J Med. 2011;365:2110–2121. doi: 10.1056/NEJMra1100359. [DOI] [PubMed] [Google Scholar]
- 18.Fors Nieves CE, Izmirly PM. Mortality in systemic lupus erythematosus: an updated review. Curr Rheumatol Rep. 2016;18:21. doi: 10.1007/s11926-016-0571-2. [DOI] [PubMed] [Google Scholar]
- 19.Jung JY, Suh CH. Infection in systemic lupus erythematosus, similarities, and differences with lupus flare. Korean J Intern Med. 2017;32:429–438. doi: 10.3904/kjim.2016.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doria A, Canova M, Tonon M, et al. Infections as triggers and complications of systemic lupus erythematosus. Autoimmun Rev. 2008;8:24–28. doi: 10.1016/j.autrev.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 21.Ocampo-Piraquive V, Nieto-Aristizábal I, Cañas CA, Tobón GJ. Mortality in systemic lupus erythematosus: causes, predictors and interventions. Expert Rev Clin Immunol. 2018;14:1043–1053. doi: 10.1080/1744666x.2018.1538789. [DOI] [PubMed] [Google Scholar]
- 22.Cervera R, Khamashta MA, Font J, et al. Morbidity and mortality in systemic lupus erythematosus during a 10-year period: a comparison of early and late manifestations in a cohort of 1,000 patients. Medicine (Baltimore) 2003;82:299–308. doi: 10.1097/01.md.0000091181.93122.55. [DOI] [PubMed] [Google Scholar]
- 23.Fessler BJ. Infectious diseases in systemic lupus erythematosus: risk factors, management and prophylaxis. Best Pract Res Clin Rheumatol. 2002;16:281–291. doi: 10.1053/berh.2001.0226. [DOI] [PubMed] [Google Scholar]
- 24.Bosch X, Guilabert A, Pallarés L, et al. Infections in systemic lupus erythematosus: a prospective and controlled study of 110 patients. Lupus. 2006;15:584–589. doi: 10.1177/0961203306071919. [DOI] [PubMed] [Google Scholar]
- 25.Lim CC, Liu PY, Tan HZ, et al. Severe infections in patients with lupus nephritis treated with immunosuppressants: a retrospective cohort study. Nephrology. 2017;22:478–484. doi: 10.1111/nep.12809. [DOI] [PubMed] [Google Scholar]
- 26.Zonana-Nacach A, Camargo-Coronel A, Yañez P, Sánchez L, Jimenez-Balderas FJ, Fraga A. Infections in outpatients with systemic lupus erythematosus: a prospective study. Lupus. 2001;10:505–510. doi: 10.1191/096120301678416088. [DOI] [PubMed] [Google Scholar]
- 27.Torres-Ruiz J, Mejía-Domínguez NR, Zentella-Dehesa A, et al. The systemic lupus erythematosus infection predictive index (LIPI): a clinical-immunological tool to predict infections in lupus patients. Front Immunol. 2018;9:3144. doi: 10.3389/fimmu.2018.03144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Danza A, Ruiz-Irastorza G. Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus. 2013;22:1286–1294. doi: 10.1177/0961203313493032. [DOI] [PubMed] [Google Scholar]
- 29.Katsuyama E, Suarez-Fueyo A, Bradley SJ, et al. The CD38/NAD/SIRTUIN1/EZH2 axis mitigates cytotoxic CD8 T cell function and identifies patients with SLE prone to infections. Cell Rep. 2020;30:112–123.e4. doi: 10.1016/j.celrep.2019.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kis-Toth K, Comte D, Karampetsou MP, et al. Selective loss of signaling lymphocytic activation molecule family member 4-positive CD8+ T cells contributes to the decreased cytotoxic cell activity in systemic lupus erythematosus. Arthritis Rheumatol. 2016;68:164–173. doi: 10.1002/art.39410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sawada T, Fujimori D, Yamamoto Y. Systemic lupus erythematosus and immunodeficiency. Immunol Med. 2019;42:1–9. doi: 10.1080/25785826.2019.1628466. [DOI] [PubMed] [Google Scholar]
- 32.Saiki O, Saeki Y, Tanaka T, et al. Development of selective IgM deficiency in systemic lupus erythematosus patients with disease of long duration. Arthritis Rheum. 1987;30:1289–1292. doi: 10.1002/art.1780301112. [DOI] [PubMed] [Google Scholar]
- 33.Perazzio SF, Granados Á, Salomão R, Silva NP, Carneiro-Sampaio M, Andrade LE. High frequency of immunodeficiency-like states in systemic lupus erythematosus: a cross-sectional study in 300 consecutive patients. Rheumatology (Oxford) 2016;55:1647–1655. doi: 10.1093/rheumatology/kew227. [DOI] [PubMed] [Google Scholar]
- 34.Koh JWH, Ng CH, Tay SH. Biologics targeting type I interferons in SLE: a meta-analysis and systematic review of randomised controlled trials. Lupus. 2020 doi: 10.1177/0961203320959702. [DOI] [PubMed] [Google Scholar]
- 35.Hu SC, Lin CL, Lu YW, et al. Lymphopaenia, anti-Ro/anti-RNP autoantibodies, renal involvement and cyclophosphamide use correlate with increased risk of herpes zoster in patients with systemic lupus erythematosus. Acta Derm Venereol. 2013;93:314–318. doi: 10.2340/00015555-1454. [DOI] [PubMed] [Google Scholar]
- 36.Qin L, Qiu Z, Hsieh E, et al. Association between lymphocyte subsets and cytomegalovirus infection status among patients with systemic lupus erythematosus: a pilot study. Medicine. 2019;98:e16997. doi: 10.1097/md.0000000000016997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Furer V, Rondaan C, Heijstek M, et al. Incidence and prevalence of vaccine preventable infections in adult patients with autoimmune inflammatory rheumatic diseases (AIIRD): a systemic literature review informing the 2019 update of the EULAR recommendations for vaccination in adult patients with AIIRD. RMD open. 2019;5 doi: 10.1136/rmdopen-2019-001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mathian A, Pha M, Amoura Z. Lupus and vaccinations. Curr Opin Rheumatol. 2018;30:465–470. doi: 10.1097/bor.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 39.Tselios K, Tsioka R, Sarantopoulos A, Mouloudi E, Boura P. Influenza A/H1N1 septic shock in a patient with systemic lupus erythematosus. A case report. BMC Infect Dis. 2011;11:358. doi: 10.1186/1471-2334-11-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun F, Chen Y, Wu W, et al. Varicella zoster virus infections increase the risk of disease flares in patients with SLE: a matched cohort study. Lupus Sci Med. 2019;6 doi: 10.1136/lupus-2019-000339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Slight-Webb SR, Bagavant H, Crowe SR, James JA. Influenza A (H1N1) virus infection triggers severe pulmonary inflammation in lupus-prone mice following viral clearance. J Autoimmun. 2015;57:66–76. doi: 10.1016/j.jaut.2014.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang CC, Chang YS, Chen WS, Chen YH, Chen JH. Effects of annual influenza vaccination on morbidity and mortality in patients with systemic lupus erythematosus: a nationwide cohort study. Sci Reps. 2016;6:37817. doi: 10.1038/srep37817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.James JA, Robertson JM. Lupus and Epstein-Barr. Curr Opin Rheumatol. 2012;24:383–388. doi: 10.1097/BOR.0b013e3283535801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Illescas-Montes R, Corona-Castro CC, Melguizo-Rodríguez L, Ruiz C, Costela-Ruiz VJ. Infectious processes and systemic lupus erythematosus. Immunology. 2019;158:153–160. doi: 10.1111/imm.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pisetsky DS. Role of Epstein-Barr virus infection in SLE: gene-environment interactions at the molecular level. Ann Rheum Dis. 2018;77:1249–1250. doi: 10.1136/annrheumdis-2018-213783. [DOI] [PubMed] [Google Scholar]
- 46.Harley JB, Chen X, Pujato M, et al. Transcription factors operate across disease loci, with EBNA2 implicated in autoimmunity. Nat Genet. 2018;50:699–707. doi: 10.1038/s41588-018-0102-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Müller U, Steinhoff U, Reis LF, et al. Functional role of type I and type II interferons in antiviral defense. Science. 1994;264:1918–1921. doi: 10.1126/science.8009221. [DOI] [PubMed] [Google Scholar]
- 48.Zhou Z, Ren L, Zhang L, et al. Heightened innate immune responses in the respiratory tract of COVID-19 patients. Cell Host Microbe. 2020;27:883–890.e2. doi: 10.1016/j.chom.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weckerle CE, Franek BS, Kelly JA, et al. Network analysis of associations between serum interferon-α activity, autoantibodies, and clinical features in systemic lupus erythematosus. Arthritis Rheum. 2011;63:1044–1053. doi: 10.1002/art.30187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baechler EC, Batliwalla FM, Karypis G, et al. Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc Natl Acad Sci U S A. 2003;100:2610–2615. doi: 10.1073/pnas.0337679100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Niewold TB. Interferon alpha as a primary pathogenic factor in human lupus. J Interferon Cytokine Res. 2011;31:887–892. doi: 10.1089/jir.2011.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Channappanavar R, Fehr AR, Vijay R, et al. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-Infected Mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blanco-Melo D, Nilsson-Payant BE, Liu WC, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181:1036–1045. doi: 10.1016/j.cell.2020.04.026. .e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369:718–724. doi: 10.1126/science.abc6027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Terán-Cabanillas E, Hernández J. Role of leptin and SOCS3 in inhibiting the type I interferon response during obesity. Inflammation. 2017;40:58–67. doi: 10.1007/s10753-016-0452-x. [DOI] [PubMed] [Google Scholar]
- 56.Li G, Ju J, Weyand CM, Goronzy JJ. Age-associated failure to adjust type I IFN receptor signaling thresholds after T cell activation. J Immunol. 2015;195:865–874. doi: 10.4049/jimmunol.1402389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Critchley-Thorne RJ, Simons DL, Yan N, et al. Impaired interferon signaling is a common immune defect in human cancer. Proc Natl Acad Sci U S A. 2009;106:9010–9015. doi: 10.1073/pnas.0901329106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wilk AJ, Rustagi A, Zhao NQ, et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat Med. 2020;26:1070–1076. doi: 10.1038/s41591-020-0944-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arunachalam PS, Wimmers F, Mok CKP, et al. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science. 2020;369:1210–1220. doi: 10.1126/science.abc6261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang Q. Human genetics of life-threatening influenza pneumonitis. Hum Genet. 2020;139:941–948. doi: 10.1007/s00439-019-02108-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Asgari S, Schlapbach LJ, Anchisi S, et al. Severe viral respiratory infections in children with IFIH1 loss-of-function mutations. Proc Natl Acad Sci U S A. 2017;114:8342–8347. doi: 10.1073/pnas.1704259114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sancho-Shimizu V, Pérez de Diego R, Lorenzo L, et al. Herpes simplex encephalitis in children with autosomal recessive and dominant TRIF deficiency. J Clin Invest. 2011;121:4889–4902. doi: 10.1172/jci59259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Postal M, Vivaldo JF, Fernandez-Ruiz R. Type I Interferon in the pathogenesis of systemic lupus erythematosus. Curr Opin Immunol. 2020;67:87–94. doi: 10.1016/j.coi.2020.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mu J, Fang Y, Yang Q, et al. SARS-CoV-2 N protein antagonizes type I interferon signaling by suppressing phosphorylation and nuclear translocation of STAT1 and STAT2. Cell Discov. 2020;6:65. doi: 10.1038/s41421-020-00208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Reizis B. Plasmacytoid dendritic cells: development, regulation, and function. Immunity. 2019;50:37–50. doi: 10.1016/j.immuni.2018.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.van der Made CI, Simons A, Schuurs-Hoeijmakers J, et al. Presence of genetic variants among young men with severe COVID-19. Jama. 2020;324:1–11. doi: 10.1001/jama.2020.13719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang Q, Bastard P, Liu Z, et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370 doi: 10.1126/science.abd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Niewold TB. Advances in lupus genetics. Curr Opin Rheumatol. Sep 2015;27(5):440–447. doi: 10.1097/bor.0000000000000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oliveira L, Sinicato NA, Postal M, Appenzeller S, Niewold TB. Dysregulation of antiviral helicase pathways in systemic lupus erythematosus. Front Genet. 2014;5:418. doi: 10.3389/fgene.2014.00418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smyth DJ, Cooper JD, Bailey R, et al. A genome-wide association study of nonsynonymous SNPs identifies a type 1 diabetes locus in the interferon-induced helicase (IFIH1) region. Nat Genet. 2006;38:617–619. doi: 10.1038/ng1800. [DOI] [PubMed] [Google Scholar]
- 71.Nejentsev S, Walker N, Riches D, Egholm M, Todd JA. Rare variants of IFIH1, a gene implicated in antiviral responses, protect against type 1 diabetes. Science. 2009;324:387–389. doi: 10.1126/number/science.1167728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bastard P, Rosen LB, Zhang Q, et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020;370 doi: 10.1126/science.abd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Panem S, Check IJ, Henriksen D, Vilcek J. Antibodies to alpha-interferon in a patient with systemic lupus erythematosus. J Immunol. 1982;129:1–3. [PubMed] [Google Scholar]
- 74.Harris BD, Kuruganti S, Deshpande A, Goepfert PA, Chatham WW, Walter MR. Characterization of Type-I IFN subtype autoantibodies and activity in SLE serum and urine. Lupus. 2020;29:1095–1105. doi: 10.1177/0961203320935976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Howe HS, Leung BPL. Anti-cytokine autoantibodies in systemic lupus erythematosus. Cells. 2019;9 doi: 10.3390/cells9010072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Morimoto AM, Flesher DT, Yang J, et al. Association of endogenous anti-interferon-α autoantibodies with decreased interferon-pathway and disease activity in patients with systemic lupus erythematosus. Arthritis Rheum. 2011;63:2407–2415. doi: 10.1002/art.30399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Slavikova M, Schmeisser H, Kontsekova E, Mateicka F, Borecky L, Kontsek P. Incidence of autoantibodies against type I and type II interferons in a cohort of systemic lupus erythematosus patients in Slovakia. J Interferon Cytokine Res. 2003;23:143–147. doi: 10.1089/107999003321532475. [DOI] [PubMed] [Google Scholar]
- 78.Zhou Q, Chen V, Shannon CP, et al. Interferon-α2b treatment for COVID-19. Front Immunol. 2020;11:1061. doi: 10.3389/fimmu.2020.01061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Monk PD, Marsden RJ, Tear VJ, et al. Safety and efficacy of inhaled nebulised interferon beta-1a (SNG001) for treatment of SARS-CoV-2 infection: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Respir Med. 2020 doi: 10.1016/s2213-2600(20)30511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pan H, Peto R, Henao-Restrepo AM, et al. Repurposed antiviral drugs for COVID-19 - interim WHO solidarity trial results. N Engl J Med. 2020 doi: 10.1056/NEJMoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang N, Zhan Y, Zhu L, et al. Retrospective multicenter cohort study shows early interferon therapy is associated with favorable clinical responses in COVID-19 patients. Cell Host Microbe. 2020;28:455–464.e2. doi: 10.1016/j.chom.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Trouillet-Assant S, Viel S, Gaymard A, et al. Type I IFN immunoprofiling in COVID-19 patients. J Allergy Clin Immunol. 2020;146:206–208.e2. doi: 10.1016/j.jaci.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Channappanavar R, Fehr AR, Zheng J, et al. IFN-I response timing relative to virus replication determines MERS coronavirus infection outcomes. J Clin Invest. 2019;129:3625–3639. doi: 10.1172/jci126363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee JS, Shin EC. The type I interferon response in COVID-19: implications for treatment. Nat Rev Immunol. 2020;20:585–586. doi: 10.1038/s41577-020-00429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Luo W, Li YX, Jiang LJ, Chen Q, Wang T, Ye DW. Targeting JAK-STAT signaling to control cytokine release syndrome in COVID-19. Trends Pharmacol Sci. 2020;41:531–543. doi: 10.1016/j.tips.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rodriguez-Garcia JL, Sanchez-Nievas G, Arevalo-Serrano J, Garcia-Gomez C, Jimenez-Vizuete JM, Martinez-Alfaro E. Baricitinib improves respiratory function in patients treated with corticosteroids for SARS-CoV-2 pneumonia: an observational cohort study. Rheumatology (Oxford) 2020 doi: 10.1093/rheumatology/keaa587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huet T, Beaussier H, Voisin O, et al. Anakinra for severe forms of COVID-19: a cohort study. Lancet Rheumatol. 2020;2:e393–e400. doi: 10.1016/S2665-9913(20)30164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with covid-19 - preliminary report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dequin PF, Heming N, Meziani F, et al. Effect of hydrocortisone on 21-day mortality or respiratory support among critically ill patients with COVID-19: a randomized clinical trial. Jama. 2020;324:1–9. doi: 10.1001/jama.2020.16761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tomazini BM, Maia IS, Cavalcanti AB, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. Jama. 2020;324:1–11. doi: 10.1001/jama.2020.17021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sterne JAC, Murthy S, Diaz JV, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. Jama. 2020;324:1–13. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ziegler CGK, Allon SJ, Nyquist SK, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181:1016–1035.e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Onabajo OO, Banday AR, Stanifer ML, et al. Interferons and viruses induce a novel truncated ACE2 isoform and not the full-length SARS-CoV-2 receptor. Nat Genet. 2020 doi: 10.1038/s41588-020-00731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sawalha AH, Zhao M, Coit P, Lu Q. Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. Clin Immunol. 2020;215 doi: 10.1016/j.clim.2020.108410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Papayannopoulos V. Neutrophil extracellular traps in immunity and disease. Nat Rev Immunol. 2018;18:134–147. doi: 10.1038/nri.2017.105. [DOI] [PubMed] [Google Scholar]
- 96.Tambralli A, Gockman K, Knight JS. NETs in APS: current knowledge and future perspectives. [DOI] [PubMed]
- 97.Meng H, Yalavarthi S, Kanthi Y, et al. In vivo role of neutrophil extracellular traps in antiphospholipid antibody-mediated venous thrombosis. Arthritis Rheumatol. 2017;69:655–667. doi: 10.1002/art.39938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020;5 doi: 10.1172/jci.insight.138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Middleton EA, He XY, Denorme F, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Veras FP, Pontelli MC, Silva CM, et al. SARS-CoV-2–triggered neutrophil extracellular traps mediate COVID-19 pathology. J Exp Med. 2020;217 doi: 10.1084/jem.20201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Radermecker C, Detrembleur N, Guiot J, et al. Neutrophil extracellular traps infiltrate the lung airway, interstitial, and vascular compartments in severe COVID-19. J Exp Med. 2020;217 doi: 10.1084/jem.20201012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ali RA, Gandhi AA, Meng H, et al. Adenosine receptor agonism protects against NETosis and thrombosis in antiphospholipid syndrome. Nat Commun. 2019;10:1916. doi: 10.1038/s41467-019-09801-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Devreese KMJ, Linskens EA, Benoit D, Peperstraete H. Antiphospholipid antibodies in patients with COVID-19: a relevant observation? J Thromb Haemost. 2020 doi: 10.1111/jth.14994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Siguret V, Voicu S, Neuwirth M, et al. Are antiphospholipid antibodies associated with thrombotic complications in critically ill COVID-19 patients? Thromb Res. 2020;195:74–76. doi: 10.1016/j.thromres.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gatto M, Perricone C, Tonello M, et al. Frequency and clinical correlates of antiphospholipid antibodies arising in patients with SARS-CoV-2 infection: findings from a multicentre study on 122 cases. Clin Exp Rheumatol. 2020;38:754–759. [PubMed] [Google Scholar]
- 106.Ferrari E, Sartre B, Squara F, et al. High prevalence of acquired thrombophilia without prognosis value in Covid-19 patients. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.017773. Epub 2020 Sep 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tvito A, Ben-Chetrit E, Zimmerman FS, Asher E, Helviz Y. Lupus anticoagulant in patients with COVID-19. Int J Lab Hematol. 2020 doi: 10.1111/ijlh.13334. [DOI] [PubMed] [Google Scholar]
- 108.Gkrouzman E, Barbhaiya M, Erkan D, Lockshin MD. A reality check on antiphospholipid antibodies in COVID-19-associated coagulopathy. Arthritis Rheumatol. 2020 doi: 10.1002/art.41472. [DOI] [PubMed] [Google Scholar]
- 109.Bowles L, Platton S, Yartey N, et al. Lupus anticoagulant and abnormal coagulation tests in patients with covid-19. N Engl J Med. 2020;3:288–290. doi: 10.1056/NEJMc2013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Reyes Gil M, Barouqa M, Szymanski J, Gonzalez-Lugo JD, Rahman S, Billett HH. Assessment of lupus anticoagulant positivity in patients with coronavirus disease 2019 (COVID-19) JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.17539. [DOI] [PubMed] [Google Scholar]
- 111.Mantovani Cardoso E, Hundal J, Feterman D, Magaldi J. Concomitant new diagnosis of systemic lupus erythematosus and COVID-19 with possible antiphospholipid syndrome. Just a coincidence? A case report and review of intertwining pathophysiology. Clin Rheumatol. 2020;39:2811–2815. doi: 10.1007/s10067-020-05310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zuo Y, Estes SK, Ali RA, et al. Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci Transl Med. 2020 doi: 10.1126/scitranslmed.abd3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Martirosyan A, Aminov R, Manukyan G. Environmental triggers of autoreactive responses: induction of antiphospholipid antibody formation. Front Immunol. 2019;10:1609. doi: 10.3389/fimmu.2019.01609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Uthman IW, Gharavi AE. Viral infections and antiphospholipid antibodies. Semin Arthritis Rheum. 2002;31:256–263. doi: 10.1053/sarh.2002.28303. [DOI] [PubMed] [Google Scholar]
- 115.Abdel-Wahab N, Lopez-Olivo MA, Pinto-Patarroyo GP, Suarez-Almazor ME. Systematic review of case reports of antiphospholipid syndrome following infection. Lupus. 2016;25:1520–1531. doi: 10.1177/0961203316640912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Skendros P, Mitsios A, Chrysanthopoulou A, et al. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J Clin Invest. 2020 doi: 10.1172/jci141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Carvelli J, Demaria O, Vély F, et al. Association of COVID-19 inflammation with activation of the C5a-C5aR1 axis. Nature. 2020 doi: 10.1038/s41586-020-2600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ramlall V, Thangaraj PM, Meydan C, et al. Immune complement and coagulation dysfunction in adverse outcomes of SARS-CoV-2 infection. Nat Med. 2020;26:1609–1615. doi: 10.1038/s41591-020-1021-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mastellos DC, Pires da Silva BGP, Fonseca BAL, et al. Complement C3 vs C5 inhibition in severe COVID-19: early clinical findings reveal differential biological efficacy. Clin Immunol. 2020;220 doi: 10.1016/j.clim.2020.108598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mastaglio S, Ruggeri A, Risitano AM, et al. The first case of COVID-19 treated with the complement C3 inhibitor AMY-101. Clin Immunol. 2020;215 doi: 10.1016/j.clim.2020.108450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Smith K, Pace A, Ortiz S, Kazani S, Rottinghaus S. A phase 3 open-label, randomized, controlled study to evaluate the efficacy and safety of intravenously administered ravulizumab compared with best supportive care in patients with COVID-19 severe pneumonia, acute lung injury, or acute respiratory distress syndrome: a structured summary of a study protocol for a randomised controlled trial. Trials. 2020;1:639. doi: 10.1186/s13063-020-04548-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rambaldi A, Gritti G, Micò MC, et al. Endothelial injury and thrombotic microangiopathy in COVID-19: Treatment with the lectin-pathway inhibitor narsoplimab. Immunobiology. 2020 doi: 10.1016/j.imbio.2020.152001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Diurno F, Numis FG, Porta G, et al. Eculizumab treatment in patients with COVID-19: preliminary results from real life ASL Napoli 2 Nord experience. Eur Rev Med Pharmacol Sci. 2020;24:4040–4047. doi: 10.26355/eurrev_202004_20875. [DOI] [PubMed] [Google Scholar]
- 124.Laurence J, Mulvey JJ, Seshadri M, et al. Anti-complement C5 therapy with eculizumab in three cases of critical COVID-19. Clin Immunol. 2020;219 doi: 10.1016/j.clim.2020.108555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Perl A. Activation of mTOR (mechanistic target of rapamycin) in rheumatic diseases. Nat Rev Rheumatol. 2016;12:169–182. doi: 10.1038/nrrheum.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lai ZW, Hanczko R, Bonilla E, et al. N-acetylcysteine reduces disease activity by blocking mammalian target of rapamycin in T cells from systemic lupus erythematosus patients: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2012;64:2937–2946. doi: 10.1002/art.34502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lai ZW, Kelly R, Winans T, et al. Sirolimus in patients with clinically active systemic lupus erythematosus resistant to, or intolerant of, conventional medications: a single-arm, open-label, phase 1/2 trial. Lancet. 2018;391:1186–1196. doi: 10.1016/s0140-6736(18)30485-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Maiese K. The mechanistic target of rapamycin (mTOR): novel considerations as an antiviral treatment. Curr Neurovasc Res. 2020;17:332–337. doi: 10.2174/1567202617666200425205122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bolourian A, Mojtahedi Z. Obesity and COVID-19: the mTOR pathway as a possible culprit. Obes Rev. 2020;21:e13084. doi: 10.1111/obr.13084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Terrazzano G, Rubino V, Palatucci AT, Giovazzino A, Carriero F, Ruggiero G. An open question: is it rational to inhibit the mTor-dependent pathway as COVID-19 therapy? Front Pharmacol. 2020;11:856. doi: 10.3389/fphar.2020.00856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ibrahim H, Perl A, Smith D, et al. Therapeutic blockade of inflammation in severe COVID-19 infection with intravenous N-acetylcysteine. Clin Immunol. 2020;219 doi: 10.1016/j.clim.2020.108544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Baldi BG, Amaral AF, de Figueiredo Braga Colares P, Kairalla RA, de Oliveira MR, Carvalho CRR. COVID-19 and lymphangioleiomyomatosis: Experience at a reference center and the potential impact of the use of mTOR inhibitors. Am J Med Genet A. 2020;12:3068–3070. doi: 10.1002/ajmg.a.61877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Peron A, La Briola F, Bruschi F, et al. Tuberous sclerosis complex (TSC), lymphangioleiomyomatosis, and COVID-19: the experience of a TSC clinic in Italy. Am J Med Genet A. 2020;182:2479–2485. doi: 10.1002/ajmg.a.61810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Spihlman AP, Gadi N, Wu SC, Moulton VR. COVID-19 and systemic lupus erythematosus: focus on immune response and therapeutics. Front Immunol. 2020;11 doi: 10.3389/fimmu.2020.589474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tan L, Wang Q, Zhang D, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;1:33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chen Z, John Wherry E. T cell responses in patients with COVID-19. Nat Rev Immunol. 2020;20:529–536. doi: 10.1038/s41577-020-0402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mathew D, Giles JR, Baxter AE, et al. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science. 2020;369 doi: 10.1126/science.abc8511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Wang F, Hou H, Luo Y, et al. The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight. 2020;5 doi: 10.1172/jci.insight.137799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Diao B, Wang C, Tan Y, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) Front Immunol. 2020;11:827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Su Y, Chen D, Yuan D, et al. Multi-omics resolves a sharp disease-state shift between mild and moderate COVID-19. Cell. 2020 doi: 10.1016/j.cell.2020.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/s2213-2600(20)30076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.De Biasi S, Meschiari M, Gibellini L, et al. Marked T cell activation, senescence, exhaustion and skewing towards TH17 in patients with COVID-19 pneumonia. Nat Commun. 2020;11:3434. doi: 10.1038/s41467-020-17292-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yang XY, Wang HY, Zhao XY, Wang LJ, Lv QH, Wang QQ. Th22, but not Th17 might be a good index to predict the tissue involvement of systemic lupus erythematosus. J Clin Immunol. 2013;33:767–774. doi: 10.1007/s10875-013-9878-1. [DOI] [PubMed] [Google Scholar]
- 144.Katsuyama T, Tsokos GC, Moulton VR. Aberrant T cell signaling and subsets in systemic lupus erythematosus. Front Immunol. 2018;9:1088. doi: 10.3389/fimmu.2018.01088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang F, Gan R, Zhen Z, et al. Adaptive immune responses to SARS-CoV-2 infection in severe versus mild individuals. Signal Transduct Target Ther. 2020;5:156. doi: 10.1038/s41392-020-00263-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Woodruff MC, Ramonell RP, Nguyen DC, et al. Extrafollicular B cell responses correlate with neutralizing antibodies and morbidity in COVID-19. Nat Immunol. 2020;21:1506–1516. doi: 10.1038/s41590-020-00814-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kaneko N, Kuo HH, Boucau J, et al. Loss of Bcl-6-expressing T follicular helper cells and germinal centers in COVID-19. Cell. 2020;183:143–157.e13. doi: 10.1016/j.cell.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Notz Q, Meybohm P, Kranke P, Weismann D, Lotz C, Schmalzing M. Antirheumatic drugs, B cell depletion and critical COVID-19: correspondence on 'Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine' by Mathian et al. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218778. [DOI] [PubMed] [Google Scholar]
- 149.Loarce-Martos J, García-Fernández A, López-Gutiérrez F, et al. High rates of severe disease and death due to SARS-CoV-2 infection in rheumatic disease patients treated with rituximab: a descriptive study. Rheumatol Int. 2020:1–7. doi: 10.1007/s00296-020-04699-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kos I, Balensiefer B, Roth S, et al. Prolonged course of COVID-19-associated pneumonia in a B-cell depleted patient after rituximab. Front Oncol. 2020;10:1578. doi: 10.3389/fonc.2020.01578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Durcan L, O'Dwyer T, Petri M. Management strategies and future directions for systemic lupus erythematosus in adults. Lancet (London, England) 2019;393:2332–2343. doi: 10.1016/s0140-6736(19)30237-5. [DOI] [PubMed] [Google Scholar]
- 152.Ugarte A, Danza A, Ruiz-Irastorza G. Glucocorticoids and antimalarials in systemic lupus erythematosus: an update and future directions. Curr Opin Rheumatol. 2018;30:482–489. doi: 10.1097/bor.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 153.van Vollenhoven RF, Mosca M, Bertsias G, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis. 2014;73:958–967. doi: 10.1136/annrheumdis-2013-205139. [DOI] [PubMed] [Google Scholar]
- 154.Petri M, Magder LS. Comparison of remission and lupus low disease activity state in damage prevention in a United States systemic lupus erythematosus cohort. Arthritis Rheumatol. 2018;70:1790–1795. doi: 10.1002/art.40571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Atzeni F, Bendtzen K, Bobbio-Pallavicini F, et al. Infections and treatment of patients with rheumatic diseases. Clin Exp Rheumatol. 2008;26(1 Suppl 48):S67–S73. [PubMed] [Google Scholar]
- 156.Kilian A, Chock YP, Huang IJ, et al. Acute respiratory viral adverse events during use of antirheumatic disease therapies: a scoping review. Semin Arthritis Rheum. 2020;50:1191–1201. doi: 10.1016/j.semarthrit.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Haberman R, Axelrad J, Chen A, et al. Covid-19 in immune-mediated inflammatory diseases — case series from New York. N Engl J Med. 2020 doi: 10.1056/NEJMc2009567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Haberman RH, Castillo R, Chen A, et al. COVID-19 in patients with inflammatory arthritis: a prospective study on the effects of comorbidities and DMARDs on clinical outcomes. Arthritis Rheumatol. 2020 doi: 10.1002/art.41456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Barber MRW, Clarke AE. Systemic lupus erythematosus and risk of infection. Exp Rev Clin Immunol. 2020;16:527–538. doi: 10.1080/1744666x.2020.1763793. [DOI] [PubMed] [Google Scholar]
- 160.Peng L, Wang Y, Zhao L, Chen T, Huang A. Severe pneumonia in Chinese patients with systemic lupus erythematosus. Lupus. 2020;29:735–742. doi: 10.1177/0961203320922609. [DOI] [PubMed] [Google Scholar]
- 161.Alarcon GS, McGwin G, Bertoli AM, et al. Effect of hydroxychloroquine on the survival of patients with systemic lupus erythematosus: data from LUMINA, a multiethnic US cohort (LUMINA L) Ann Rheum Dis. 2007;66:1168–1172. doi: 10.1136/ard.2006.068676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Izmirly P, Kim M, Friedman DM, et al. Hydroxychloroquine to prevent recurrent congenital heart block in fetuses of anti-SSA/Ro-positive mothers. J Am Coll Cardiol. 2020;76:292–302. doi: 10.1016/j.jacc.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.A randomized study of the effect of withdrawing hydroxychloroquine sulfate in systemic lupus erythematosus. N Engl J Med. 1991;324:150–154. doi: 10.1056/nejm199101173240303. [DOI] [PubMed] [Google Scholar]
- 164.Ruiz-Irastorza G, Ramos-Casals M, Brito-Zeron P, Khamashta MA. Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: a systematic review. Ann Rheum Dis. 2010;69:20–28. doi: 10.1136/ard.2008.101766. [DOI] [PubMed] [Google Scholar]
- 165.Dörner T. Therapy: hydroxychloroquine in SLE: old drug, new perspectives. Nat Rev Rheumatol. 2010;6:10–11. doi: 10.1038/nrrheum.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Stojan G, Petri M. The risk benefit ratio of glucocorticoids in SLE: have things changed over the past 40 years? Curr Treatm Opt Rheumatol. 2017;3:164–172. doi: 10.1007/s40674-017-0069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ruiz-Irastorza G, Olivares N, Ruiz-Arruza I, Martinez-Berriotxoa A, Egurbide MV, Aguirre C. Predictors of major infections in systemic lupus erythematosus. Arthritis Res Ther. 2009;11:R109. doi: 10.1186/ar2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Sakai R, Honda S, Tanaka E, et al. The risk of hospitalized infection in patients with systemic lupus erythematosus treated with hydroxychloroquine. Lupus. 2020 doi: 10.1177/0961203320952853. [DOI] [PubMed] [Google Scholar]
- 169.Rolain JM, Colson P, Raoult D. Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int J Antimicrob Agents. 2007;30:297–308. doi: 10.1016/j.ijantimicag.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Rodrigo C, Fernando SD, Rajapakse S. Clinical evidence for repurposing chloroquine and hydroxychloroquine as antiviral agents: a systematic review. Clin Microb Infect. 2020;26:979–987. doi: 10.1016/j.cmi.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Horby P, Mafham M, Linsell L, et al. Effect of hydroxychloroquine in hospitalized patients with covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2022926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Garnier C, Ribes D, Chauveau D, et al. Zoster after cyclophosphamide for systemic lupus erythematosus or vasculitis: incidence, risk factors, and effect of antiviral prophylaxis. J Rheumatol. 2018;45:1541–1548. doi: 10.3899/jrheum.180310. [DOI] [PubMed] [Google Scholar]
- 173.Jiang YP, Zhao XX, Chen RR, Xu ZH, Wen CP, Yu J. Comparative efficacy and safety of mycophenolate mofetil and cyclophosphamide in the induction treatment of lupus nephritis: a systematic review and meta-analysis. Medicine. 2020;99:e22328. doi: 10.1097/md.0000000000022328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Feldman CH, Marty FM, Winkelmayer WC, et al. Comparative rates of serious infections among patients with systemic lupus erythematosus receiving immunosuppressive medications. Arthritis Rheumatol. 2017;69:387–397. doi: 10.1002/art.39849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Subedi A, Magder LS, Petri M. Effect of mycophenolate mofetil on the white blood cell count and the frequency of infection in systemic lupus erythematosus. Rheumatol Int. 2015;35:1687–1692. doi: 10.1007/s00296-015-3265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Tani C, Elefante E, Martin-Cascón M, et al. Tacrolimus in non-Asian patients with SLE: a real-life experience from three European centres. Lupus Sci Med. 2018;5 doi: 10.1136/lupus-2018-000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Singh JA, Hossain A, Kotb A, Wells G. Risk of serious infections with immunosuppressive drugs and glucocorticoids for lupus nephritis: a systematic review and network meta-analysis. BMC Med. 2016;14:137. doi: 10.1186/s12916-016-0673-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zhou T, Lin S, Yang S, Lin W. Efficacy and safety of tacrolimus in induction therapy of patients with lupus nephritis. Drug Des Devel Ther. 2019;13:857–869. doi: 10.2147/dddt.S189156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Furie R, Petri M, Zamani O, et al. A phase III, randomized, placebo-controlled study of belimumab, a monoclonal antibody that inhibits B lymphocyte stimulator, in patients with systemic lupus erythematosus. Arthritis Rheum. 2011;63:3918–3930. doi: 10.1002/art.30613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Henegar CE, Eudy AM, Kharat V, Hill DD, Bennett D, Haight B. Progressive multifocal leukoencephalopathy in patients with systemic lupus erythematosus: a systematic literature review. Lupus. 2016;25:617–626. doi: 10.1177/0961203315622819. [DOI] [PubMed] [Google Scholar]
- 181.Masse V, Al Jijakli A, Genet P, et al. Screening and management of hepatitis B virus before the first rituximab infusion: we must do better! Blood. 2014;124:2754. doi: 10.1182/blood.V124.21.2754.2754. -2754. [DOI] [Google Scholar]
- 182.Witt M, Grunke M, Proft F, et al. Clinical outcomes and safety of rituximab treatment for patients with systemic lupus erythematosus (SLE) - results from a nationwide cohort in Germany (GRAID) Lupus. 2013;22:1142–1149. doi: 10.1177/0961203313503912. [DOI] [PubMed] [Google Scholar]
- 183.Iwata S, Saito K, Hirata S, et al. Efficacy and safety of anti-CD20 antibody rituximab for patients with refractory systemic lupus erythematosus. Lupus. 2018;27:802–811. doi: 10.1177/0961203317749047. [DOI] [PubMed] [Google Scholar]
- 184.Paredes JL, Niewold TB. Type I interferon antagonists in clinical development for lupus. Expert Opin Investig Drugs. 2020;29:1025–1041. doi: 10.1080/13543784.2020.1797677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Furie R, Khamashta M, Merrill JT, et al. Anifrolumab, an anti-interferon-α receptor monoclonal antibody, in moderate-to-severe systemic lupus erythematosus. Arthritis Rheumatol. 2017;69:376–386. doi: 10.1002/art.39962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Morand EF, Furie R, Tanaka Y, et al. Trial of anifrolumab in active systemic lupus erythematosus. N Engl J Med. 2020;382:211–221. doi: 10.1056/NEJMoa1912196. [DOI] [PubMed] [Google Scholar]
- 187.Mathian A, Mahevas M, Rohmer J, et al. Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine. Ann Rheum Dis. 2020;6:837–839. doi: 10.1136/annrheumdis-2020-217566. [DOI] [PubMed] [Google Scholar]
- 188.Konig MF, Kim AH, Scheetz MH, et al. Baseline use of hydroxychloroquine in systemic lupus erythematosus does not preclude SARS-CoV-2 infection and severe COVID-19. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Holubar J, Le Quintrec M, Letaief H, Faillie JL, Pers YM, Jorgensen C. Monitoring of patients with systemic lupus erythematosus during the COVID-19 outbreak. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217919. [DOI] [PubMed] [Google Scholar]
- 190.Gentry CA, Humphrey MB, Thind SK, Hendrickson SC, Kurdgelashvili G, Williams RJ., 2nd Long-term hydroxychloroquine use in patients with rheumatic conditions and development of SARS-CoV-2 infection: a retrospective cohort study. Lancet Rheumatol. 2020;2:e689–e697. doi: 10.1016/s2665-9913(20)30305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Singer ME, Kaelber DC, Antonelli MJ. Hydroxychloroquine ineffective for COVID-19 prophylaxis in lupus and rheumatoid arthritis. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218500. [DOI] [PubMed] [Google Scholar]
- 192.Fernandez-Ruiz R, Masson M, Kim MY, et al. Leveraging the United States epicenter to provide insights on COVID-19 in patients with systemic lupus erythematosus. Arthritis Rheumatol. 2020 doi: 10.1002/art.41450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Gendebien Z, von Frenckell C, Ribbens C, et al. Systematic analysis of COVID-19 infection and symptoms in a systemic lupus erythematosus population: correlation with disease characteristics, hydroxychloroquine use and immunosuppressive treatments. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218244. [DOI] [PubMed] [Google Scholar]
- 194.Bozzalla Cassione E, Zanframundo G, Biglia A, Codullo V, Montecucco C, Cavagna L. COVID-19 infection in a northern-Italian cohort of systemic lupus erythematosus assessed by telemedicine. Ann Rheum Dis. 2020;10:1382–1383. doi: 10.1136/annrheumdis-2020-217717. [DOI] [PubMed] [Google Scholar]
- 195.Montero F, Martínez-Barrio J, Serrano-Benavente B, et al. Coronavirus disease 2019 (COVID-19) in autoimmune and inflammatory conditions: clinical characteristics of poor outcomes. Rheumatol Int. 2020;40:1593–1598. doi: 10.1007/s00296-020-04676-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Fredi M, Cavazzana I, Moschetti L, Andreoli L, Franceschini F. COVID-19 in patients with rheumatic diseases in northern Italy: a single-centre observational and case-control study. Lancet Rheumatol. 2020;2:e549–e556. doi: 10.1016/s2665-9913(20)30169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Marques C, Pinheiro MM, Reis Neto ET, Dantas AT, Ribeiro FM, Melo AKG. COVID-19 in patients with rheumatic diseases: what is the real mortality risk? Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218388. [DOI] [PubMed] [Google Scholar]
- 198.Ramirez GA, Moroni L, Della-Torre E, et al. Systemic lupus erythematosus and COVID-19: what we know so far. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218601. [DOI] [PubMed] [Google Scholar]
- 199.Cho J, Kandane-Rathnayake R, Louthrenoo W, et al. COVID-19 infection in patients with systemic lupus erythematosus: data from the Asia Pacific Lupus Collaboration. Int J Rheum Dis. 2020;9:1255–1257. doi: 10.1111/1756-185X.13937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Santos CS, Morales CM, Álvarez ED, Castro C, Robles AL, Sandoval TP. Determinants of COVID-19 disease severity in patients with underlying rheumatic disease. Clin Rheumatol. 2020;39:2789–2796. doi: 10.1007/s10067-020-05301-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ramirez GA, Gerosa M, Beretta L, et al. COVID-19 in systemic lupus erythematosus: data from a survey on 417 patients. Semin Arthritis Rheum. 2020;50:1150–1157. doi: 10.1016/j.semarthrit.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Robinson PC, Yazdany J. The COVID-19 Global Rheumatology Alliance: collecting data in a pandemic. Nat Rev Rheumatol. 2020;16:293–294. doi: 10.1038/s41584-020-0418-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gianfrancesco M, Hyrich KL, Al-Adely S, et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Gartshteyn Y, Askanase AD, Schmidt NM, et al. COVID-19 and systemic lupus erythematosus: a case series. Lancet Rheumatol. 2020;2:e452–e454. doi: 10.1016/s2665-9913(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wallace B, Washer L, Marder W, Kahlenberg JM. Patients with lupus with COVID-19: University of Michigan experience. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217794. [DOI] [PubMed] [Google Scholar]
- 206.D'Silva KM, Serling-Boyd N, Wallwork R, et al. Clinical characteristics and outcomes of patients with coronavirus disease 2019 (COVID-19) and rheumatic disease: a comparative cohort study from a US 'hot spot'. Ann Rheum Dis. 2020;79:1156–1162. doi: 10.1136/annrheumdis-2020-217888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Murtas R, Andreano A, Gervasi F, et al. Association between autoimmune diseases and COVID-19 as assessed in both a test-negative case-control and population case-control design. Auto Immun Highlights. 2020;11:15. doi: 10.1186/s13317-020-00141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Pablos JL, Abasolo L, Alvaro-Gracia JM, et al. Prevalence of hospital PCR-confirmed COVID-19 cases in patients with chronic inflammatory and autoimmune rheumatic diseases. Ann Rheum Dis. 2020;79:1170–1173. doi: 10.1136/annrheumdis-2020-217763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Akiyama S, Hamdeh S, Micic D, Sakuraba A. Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: a systematic review and meta-analysis. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218946. [DOI] [PubMed] [Google Scholar]
- 210.Favalli EG, Gerosa M, Murgo A, Caporali R. Are patients with systemic lupus erythematosus at increased risk for COVID-19? Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217787. [DOI] [PubMed] [Google Scholar]
- 211.El Aoud S, Morin C, Lorriaux P, et al. SARS CoV-2 presenting as lupus erythematosus-like syndrome. Disaster Med Public Health Prep. 2020:1–9. doi: 10.1017/dmp.2020.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Doaty S, Agrawal H, Bauer E, Furst DE. Infection and lupus: which causes which? Curr Rheumatol Rep. 2016;18:13. doi: 10.1007/s11926-016-0561-4. [DOI] [PubMed] [Google Scholar]
- 213.Raghavan S, Gonakoti S, Asemota IR, Mba B. A case of systemic lupus erythematosus flare triggered by severe coronavirus disease 2019. J Clin Rheumatol. 2020;26:234–235. doi: 10.1097/rhu.0000000000001531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kondo Y, Kaneko Y, Oshige T, et al. Exacerbation of immune thrombocytopaenia triggered by COVID-19 in patients with systemic lupus erythematosus. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218157. [DOI] [PubMed] [Google Scholar]
- 215.Hayden A, Vyas-Lahar A, Rella V, Rudinskaya A. Severe refractory thrombocytopenia in a woman positive for coronavirus disease 2019 with lupus and antiphospholipid syndrome. Lupus. 2020;29:1472–1474. doi: 10.1177/0961203320940389. [DOI] [PubMed] [Google Scholar]
- 216.Lima K, Phillip CR, Williams J, Peterson J, Feldman CH, Ramsey-Goldman R. Factors associated with participation in rheumatic disease-related research among underrepresented populations: a qualitative systematic review. Arthritis Care Res (Hoboken) 2020;72:1481–1489. doi: 10.1002/acr.24036. [DOI] [PubMed] [Google Scholar]
- 217.Golestaneh L, Neugarten J, Fisher M, et al. The association of race and COVID-19 mortality. EClinicalMedicine. 2020;25 doi: 10.1016/j.eclinm.2020.100455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with covid-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Hatcher S, Agnew-Brune C, Anderson M, et al. COVID-19 among American Indian and Alaska Native persons - 23 States, January 31-July 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1166–1169. doi: 10.15585/mmwr.mm6934e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Gianfrancesco MA, Leykina LA, Izadi Z, et al. Race/ethnicity association with COVID-19 outcomes in rheumatic disease: data from the COVID-19 Global Rheumatology Alliance Physician Registry. Arthritis Rheumatol. 2020 doi: 10.1002/art.41567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Ortiz-Fernández L, Sawalha AH. Genetic variability in the expression of the SARS-CoV-2 host cell entry factors across populations. Genes Immun. 2020;21:269–272. doi: 10.1038/s41435-020-0107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Ogedegbe G, Ravenell J, Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York city. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.26881. -e2026881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Feldman CH, Ramsey-Goldman R. Widening disparities among patients with rheumatic diseases in the COVID-19 era: an urgent call to action. Arthritis Rheumatol. 2020 doi: 10.1002/art.41306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. 2020;8:659–661. doi: 10.1016/s2213-2600(20)30234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Sirotich E, Hausmann JS. Removing barriers and disparities in health: lessons from the COVID-19 pandemic. Nat Rev Rheumatol. 2020:1–2. doi: 10.1038/s41584-020-00524-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Blazer A, Fernandez-Ruiz R, Masson M, et al. Neighborhood deprivation and race/ethnicity affects COVID-19 risk and severity in SLE [abstract] Arthritis Rheumatol. 2020;72 https://acrabstracts.org/abstract/neighborhood-deprivation-and-race-ethnicity-affects-covid-19-risk-and-severity-in-sle/ [Google Scholar]
- 227.Perniola S, Alivernini S, Varriano V, et al. Telemedicine will not keep us apart in COVID-19 pandemic. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218022. [DOI] [PubMed] [Google Scholar]
- 228.López-Medina C, Escudero A, Collantes-Estevez E. COVID-19 pandemic: an opportunity to assess the utility of telemedicine in patients with rheumatic diseases. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218008. [DOI] [PubMed] [Google Scholar]
- 229.Mathian A, Amoura Z. Response to ‘Impact of COVID-19 pandemic on hospitalisation of patients with systemic lupus erythematosus (SLE): report from a tertiary hospital during the peak of the pandemic’ by Chuah <em>et al</em>. Ann Rheum Dise. 2020 doi: 10.1136/annrheumdis-2020-218487. [DOI] [PubMed] [Google Scholar]
- 230.Chen C, Yao B, Yan M, Su KE, Wang H, Xu C. The plight of patients with lupus nephritis during the outbreak of COVID-19 in Wuhan, China. J Rheumatol. 2020;9:1452. doi: 10.3899/jrheum.200452. [DOI] [PubMed] [Google Scholar]
- 231.Rathi M, Singh P, Bi HP, et al. Impact of the COVID-19 pandemic on patients with systemic lupus erythematosus: observations from an Indian inception cohort. Lupus. 2020 doi: 10.1177/0961203320962855. [DOI] [PubMed] [Google Scholar]
- 232.Fessler BJ, Alarcon GS, McGwin G, Jr., et al. Systemic lupus erythematosus in three ethnic groups: XVI. Association of hydroxychloroquine use with reduced risk of damage accrual. Arthritis Rheum. 2005;52:1473–1480. doi: 10.1002/art.21039. [DOI] [PubMed] [Google Scholar]
- 233.Gautret P, Lagier JC, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56 doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Liu J, Cao R, Xu M, et al. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discov. 2020;6:16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Lyngbakken MN, Berdal JE, Eskesen A, et al. A pragmatic randomized controlled trial reports lack of efficacy of hydroxychloroquine on coronavirus disease 2019 viral kinetics. Nat Commun. 2020;11:5284. doi: 10.1038/s41467-020-19056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Abella BS, Jolkovsky EL, Biney BT, et al. Efficacy and safety of hydroxychloroquine vs placebo for pre-exposure SARS-CoV-2 prophylaxis among health care workers: a randomized clinical trial. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.6319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Skipper CP, Pastick KA, Engen NW, et al. Hydroxychloroquine in nonhospitalized adults with early COVID-19: a randomized trial. Ann Intern Med. 2020;173:623–631. doi: 10.7326/m20-4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Boulware DR, Pullen MF, Bangdiwala AS, et al. A randomized trial of hydroxychloroquine as postexposure prophylaxis for covid-19. N Engl J Med. 2020;383:517–525. doi: 10.1056/NEJMoa2016638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Kim AHJ, Sparks JA, Liew JW, et al. A rush to judgment? rapid reporting and dissemination of results and its consequences regarding the use of hydroxychloroquine for COVID-19. Ann Intern Med. 2020;12:819–821. doi: 10.7326/M20-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Yazdany J, Kim AHJ. Use of hydroxychloroquine and chloroquine during the COVID-19 pandemic: what every clinician should know. Ann Intern Med. 2020;11:754–755. doi: 10.7326/M20-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Mendel A, Bernatsky S, Askanase A, et al. Hydroxychloroquine shortages among patients with systemic lupus erythematosus during the COVID-19 pandemic: experience of the Systemic Lupus International Collaborating Clinics. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218164. [DOI] [PubMed] [Google Scholar]
- 242.Mendel A, Bernatsky S, Thorne JC, Lacaille D, Johnson SR, Vinet É. Hydroxychloroquine shortages during the COVID-19 pandemic. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217835. [DOI] [PubMed] [Google Scholar]
- 243.Plüß M, Chehab G, Korsten P. Concerns and needs of patients with systemic lupus erythematosus regarding hydroxychloroquine supplies during the COVID-19 pandemic: results from a patient-centred survey. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-217967. [DOI] [PubMed] [Google Scholar]
- 244.Fernandez-Ruiz R, Bornkamp N, Kim MY, et al. Discontinuation of hydroxychloroquine in older patients with systemic lupus erythematosus: a multicenter retrospective study. Arthritis Res Ther. 2020;22:191. doi: 10.1186/s13075-020-02282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Pessoa-Amorim G, Camm CF, Gajendragadkar P, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6:210–216. doi: 10.1093/ehjqcco/qcaa046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Nagamine M, Chow DS, Chang PD, Boden-Albala B, Yu W, Soun JE. Impact of COVID-19 on acute stroke presentation at a comprehensive stroke Center. Front Neurol. 2020;11:850. doi: 10.3389/fneur.2020.00850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Chuah SL, Teh CL, Wan Mohd Akbar SA, Cheong YK, Sachdev Manjit Singh B. Impact of COVID-19 pandemic on hospitalisation of patients with systemic lupus erythematosus (SLE): report from a tertiary hospital during the peak of the pandemic. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218475. [DOI] [PubMed] [Google Scholar]
- 248.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020:1–10. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- 249.Wańkowicz P, Szylińska A, Rotter I. Evaluation of mental health factors among people with systemic lupus erythematosus during the SARS-CoV-2 pandemic. J Clin Med. 2020;9 doi: 10.3390/jcm9092872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Tee CA, Salido EO, Reyes PWC, Ho RC, Tee ML. Psychological state and associated factors during the 2019 coronavirus disease (COVID-19) pandemic among filipinos with rheumatoid arthritis or systemic lupus erythematosus. Open Access Rheumatol. 2020;12:215–222. doi: 10.2147/oarrr.s269889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Huang Y, Chen Z, Wang Y, et al. Clinical characteristics of 17 patients with COVID-19 and systemic autoimmune diseases: a retrospective study. Ann Rheum Dis. 2020;7:1163–1169. doi: 10.1136/annrheumdis-2020-217425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Emmi G, Bettiol A, Mattioli I, et al. SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimmun Rev. 2020;19 doi: 10.1016/j.autrev.2020.102575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Zen M, Fuzzi E, Astorri D, et al. SARS-CoV-2 infection in patients with autoimmune rheumatic diseases in northeast Italy: a cross-sectional study on 916 patients. J Autoimmun. 2020;112 doi: 10.1016/j.jaut.2020.102502. [DOI] [PMC free article] [PubMed] [Google Scholar]