Abstract
Objectives
Ecuador is among the worst-hit countries in the world by the coronavirus disease 2019 (COVID-19) pandemic. In terms of confirmed deaths per million inhabitants, as of October 22, Ecuador ranks fourth in the Americas and ninth worldwide according to data from the World Health Organization. In this report, we estimate excess deaths due to any cause in Ecuador since the start of the lockdown measures on March 17, 2020 until October 22, 2020.
Methods
Estimates of excess deaths were calculated as the difference between the number of observed deaths from all causes and estimates of expected deaths from all causes. Expected deaths were estimated for the period March 17–October 22, 2020 from forecasts of an ARIMA model of order (3,0,1) with drift which was applied to daily mortality data for the period from January 1, 2014 to March 16, 2020.
Results
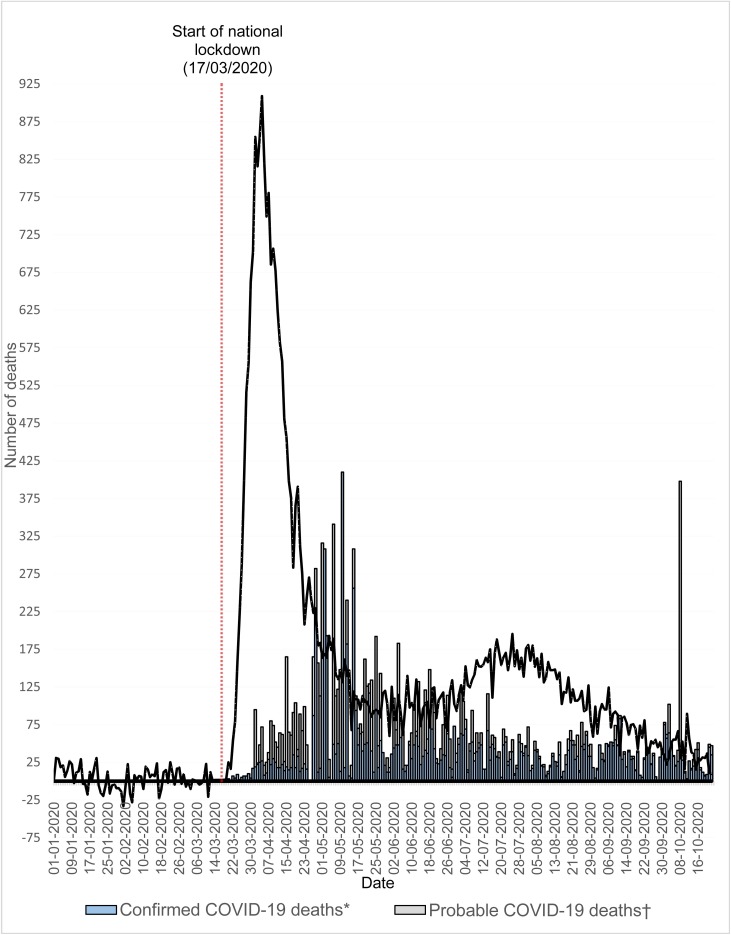
The number of all-cause excess deaths in Ecuador was estimated to be 36,922 (95% bootstrap confidence interval: 32,314–42,696) during the study period. The peak in all-cause excess mortality in Ecuador may have occurred on April 4, 2020, with 909 excess deaths.
Conclusions
Our results suggest that the real impact of the pandemic in Ecuador was much worse than that indicated by reports from national institutions. Estimates of excess mortality might provide a better approximation of the true COVID-19 death toll. These estimates might capture not only deaths directly attributable to the COVID-19 pandemic but also deaths from other diseases that resulted from indirect effects of the pandemic.
Keywords: COVID-19, Ecuador, Mortality, Excess deaths
On December 31, 2019, the Wuhan Municipal Health Commission reported a cluster of cases of atypical pneumonia in Wuhan, China. A new type of coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was identified as the source. This virus causes the coronavirus disease 2019 (COVID-19). On March 11, 2020, the World Health Organization declared the COVID-19 outbreak a pandemic (World Health Organization, 2020a). SARS-CoV-2 has rapidly spread worldwide, infecting 41,200,511 people and causing 1,130,914 confirmed deaths as of October 22 (World Health Organization, 2020b). Ecuador is among the worst-hit countries in the world. As of October 22, Ecuador reported 8,195 confirmed deaths and 4,305 probable deaths from COVID-19 (Servicio Nacional de Gestión de Riesgos y Emergencias, 2020). In terms of confirmed deaths per million inhabitants, as of October 22, Ecuador ranks fourth in the Americas and ninth worldwide (World Health Organization, 2020b). However, the real impact of the pandemic in Ecuador may be worse as the existence of underreporting of COVID-19-associated deaths cannot be disregarded. Underreporting may occur, for instance, due to delays in death registrations, a lack of enough test kits nationwide, false-negative test results, or misattribution of deaths from COVID-19 to other causes. The purpose of this study is to estimate excess deaths due to any cause in Ecuador from March 17, 2020 (when the national lockdown began) to October 22, 2020. Estimates of excess deaths might capture deaths caused directly or indirectly by COVID-19 and could thus provide a better assessment of the impact of the COVID-19 outbreak (Olson et al., 2020). For this analysis, daily mortality data from the National Institute of Statistics and Census (Instituto Nacional de Estadística y Censos, 2020), the National Civil Registry (Dirección General del Registro Civil, Identificación y Cedulación, 2020), and the National Risk and Emergency Management Service (Servicio Nacional de Gestión de Riesgos y Emergencias, 2020) of Ecuador were used. All-cause excess deaths for any day were estimated as the difference between the number of observed deaths from all causes and the estimate of expected deaths from all causes obtained for that day from historical data. To obtain estimates of expected deaths from all causes from March 17 to October 22, 2020, we used forecasts from a statistical model built on daily mortality data from the period January 1, 2014 to March 16, 2020. This is a similar approach to that used by Blanton et al. (2007) and Olson et al. (2020). Different models of exponential smoothing, cubic smoothing splines, simple moving average, and ARIMA were considered for this study. These methods have been used in similar studies (see e.g., Adair et al., 2020, Rossen et al., 2020, Vieira et al., 2020). To compare the forecast performance of these models we used out-of-sample (OOS) testing with rolling windows (Tashman, 2000) on the model-building dataset. In particular, the fit period was successively set to start on March 17 and end on March 16 of the following year to produce forecasts for the subsequent test period from March 17 to October 22. Because mortality data were available from January 1, 2014 onwards, the first fit period was set from January 1, 2014 to March 16, 2015. Five fit-test periods were generated in total in the model-building dataset. Note that this evaluation procedure emulates the forecast problem of this study. We used as a measure of performance the root mean squared error (RMSE) computed from the observed and forecasted values in the five testing periods considered. For each method, only the model with the lowest RMSE estimate in the OOS evaluation is displayed in Table 1 . As shown in Table 1, the ARIMA model of order (3,0,1) with drift shows the best forecast performance and was therefore selected for the analysis. Figure 1 shows the estimated curve of excess mortality based on this model and compares it with the daily number of confirmed and probable COVID-19 deaths in the period January 1–October 22, 2020. Note that the sequence of bars for the daily number of confirmed and probable COVID-19 deaths shows a pattern similar to the curve of excess mortality, except for being shifted to the right, which may reflect reporting delays by national institutions during the pandemic. Note also that the levels of estimated excess mortality in general exceed those of the number of confirmed and probable COVID-19 deaths. This difference may represent deaths directly attributable to COVID-19 that were not officially reported but also deaths from other diseases that resulted from indirect effects of the pandemic, such as the fear of being treated in hospitals overwhelmed with COVID-19 patients or a shortage of medication, physicians, intensive care unit beds, ventilators, or a general lack of access to healthcare services. These results suggest that the real impact of the pandemic in Ecuador was much worse than that indicated by reports from national institutions. Estimates of all-cause excess mortality might provide a better approximation of the true COVID-19 death toll. From March 17 to October 22, 2020, a total of 80,108 deaths from all causes were registered in Ecuador, of which 36,922 (95% bootstrap confidence interval: 32,314–42,696) were estimated to be in excess of expected levels. As shown in Figure 1, the peak in all-cause excess mortality in Ecuador may have occurred on April 4, 2020, with 909 excess deaths.
Table 1.
RMSE estimates of the best models for each of the methods considered in this study based on the OOS evaluation.
| Models | RMSE |
|---|---|
| Simple exponential smoothing with multiplicative errors – ETS (M,N,N) | 24.37 |
| Cubic smoothing spline with 5 degrees of freedom (complexity parameter) | 54.56 |
| Moving average model of order q = 28 days | 25.81 |
| ARIMA (3,0,1) with drift | 22.02 |
Figure 1.
Estimates of excess deaths from all causes based on an ARIMA (3,0,1) model with drift, number of confirmed COVID-19 deaths, and number of probable COVID-19 deaths in Ecuador between January 1 and October 22, 2020. Data on confirmed and probable COVID-19 deaths were obtained from the National Risk and Emergency Management Service of Ecuador (Servicio Nacional de Gestión de Riesgos y Emergencias, 2020).
*The National Risk and Emergency Management Service of Ecuador defines a confirmed COVID-19 death as a case that had laboratory confirmation of SARS-CoV-2 infection before death.
†A probable COVID-19 death is defined by the National Risk and Emergency Management Service of Ecuador as a case that exhibited known COVID-19 symptoms but did not have laboratory confirmation of SARS-CoV-2 infection before death.
Notes:
- The website of the National Institute of Statistics and Census (Instituto Nacional de Estadística y Censos, 2020) reports all-cause mortality data until December 31, 2019. For the period from January 1, 2020 to October 22, 2020 all-cause mortality data were obtained from the website of the National Civil Registry (Dirección General del Registro Civil, Identificación y Cedulación, 2020).
- Levels of all-cause mortality from December 24, 2019 to December 31, 2019 were on average lower than those registered on previous days. Deaths not registered on these vacation days were probably only registered on January 1, 2020, and as a result excess mortality was estimated to be much higher than 0 for that day. Levels of deaths in the period from March 13, 2020 to March 19, 2020 were also unusually low and as a result negative estimates of excess deaths were obtained in a systematic way for those days. These results were obtained in a first analysis with the ARIMA (3,0,1) model with drift, which showed the best performance with the OOS evaluation. To improve the fit of the model, we fitted a simple exponential smoothing model with multiplicative errors (ETS(M,N,N)) on the time series data preceding each of these periods and used the corresponding forecasts to replace the actual values of these days. ETS(M,N,N) produced the lowest RMSE in a last block evaluation for each of these 2 periods when compared with other models of exponential smoothing, cubic smoothing splines, simple moving average, and ARIMA. Reported results in Figure 1 and Table 1 are based on these modified data.
- Data on confirmed and probable COVID-19 deaths from the National Risk and Emergency Management Service of Ecuador were negative for some days. We set those values to 0 in the plot shown in Figure 1.
- A number of 362 probable COVID-19 deaths on October 8, 2020 appears to be an outlier with respect to levels of COVID-19 deaths around that period of time. Many of them may represent deaths that possibly occurred at an earlier point in time and that were only registered on October 8.
Ethical approval
None.
Conflict of interest
We declare no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Adair T., Lopez A.D., Hudson S. Bloomberg Philanthropies Data for Health Initiative, Civil Registration and Vital Statistics Improvement, University of Melbourne; Melbourne, Australia: 2020. Approaches and methods for estimating excess deaths due to COVID-19. CRVS best-practice and advocacy. [Google Scholar]
- Blanton L., Brammer L., Budd A., Wallis T., Shay D., Bresee J. Update: influenza activity—United States and worldwide, 2006-07 season, and composition of the 2007-08 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2007;56(31):789–794. [PubMed] [Google Scholar]
- Dirección General del Registro Civil, Identificación y Cedulación . 2020. Cifras Defunciones.https://www.registrocivil.gob.ec/cifras/ [Google Scholar]
- Instituto Nacional de Estadística y Censos . 2020. Nacimientos y Defunciones — Información Histórica.https://www.ecuadorencifras.gob.ec/nacimientos-y-defunciones-informacion-historica/ [Google Scholar]
- Olson D.R., Huynh M., Fine A., Baumgartner J., Castro A., Chan H.T. Preliminary estimate of excess mortality during the COVID-19 outbreak — New York City, March 11–May 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(19):603–605. doi: 10.15585/mmwr.mm6919e5. [DOI] [PubMed] [Google Scholar]
- Rossen L.M., Branum A.M., Ahmad F.B., Sutton P., Anderson R.N. Excess deaths associated with COVID-19, by age and race and ethnicity — United States, January 26–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1522–1527. doi: 10.15585/mmwr.mm6942e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servicio Nacional de Gestión de Riesgos y Emergencias . 2020. Informes de Situación e Infografías — COVID 19 — desde el 29 de Febrero del 2020.https://www.gestionderiesgos.gob.ec/informes-de-situacion-covid-19-desde-el-13-de-marzo-del-2020/ [Google Scholar]
- Tashman L.J. Out-of-sample tests of forecasting accuracy: an analysis and review. Int J Forecast. 2000;16(4):437–450. [Google Scholar]
- Vieira A., Peixoto V.R., Aguiar P., Abrantes A. Rapid estimation of excess mortality during the COVID-19 pandemic in Portugal—beyond reported deaths. J Epidemiol Glob Health. 2020;10(3):209–213. doi: 10.2991/jegh.k.200628.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19 — 11 March 2020.https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020/ [Google Scholar]
- World Health Organization . 2020. WHO coronavirus disease (COVID-19) dashboard.https://covid19.who.int/ [Google Scholar]