Abstract
Background
In total knee arthroplasty (TKA), advances in posterior-stabilized (PS) knee implant designs address patellofemoral mechanics and cam–post engagement in an effort to reduce patellofemoral pain and improve knee kinematics. Such modifications may include improved femoral rollback, improved femoral dislocation resistance, minimized wear, and improved longevity.
Questions/Purposes
In this study, we compared a newer PS knee design that incorporates a left and right specific femoral component and smoother trochlear groove to improve patellofemoral mechanics with an older PS design in order to assess patellofemoral pain, manipulation rates, and revision rates.
Methods
Using an institutional database, we retrospectively identified TKAs performed by the same surgeon using the Logic® PS knee system and the older Optetrak PS knee system (Exactech Inc., Gainesville, FL, USA), with a minimum 2-year follow-up. Clinical outcomes for each cohort were measured using the Knee Society Clinical Rating System, University of California Los Angeles Activity Scale, pain visual analog scale (VAS), Veterans Rand 12-Item Health Survey, and Western Ontario and McMaster Universities Osteoarthritis Index. In addition, rates of anterior knee pain, manipulation, and revision were compared between the two knee systems, and a Kaplan–Meier survivorship curve defining failure as need for revision was calculated to allow comparison between the cohorts.
Results
From 2000 to 2018, there were 1482 TKAs performed using the Logic PS (not counting 12 patients who had died) and 445 in the Optetrak PS group (not counting 20 patients who had died). In the Logic PS and Optetrak PS groups, respectively, the average age at operation was 66.7 years and 68.6 years and the average body mass index was 30.8 and 31.2. Pain VAS scores were significantly lower in the Logic PS group than in the Optetrak group (1.72 vs. 2.75 out of 10, respectively). There was also a significant difference in the percentages of patients reporting anterior knee pain in the Logic group, as compared with the Optetrak group (5.6% vs. 11.8%, respectively). In addition, manipulation rates differed significantly between the Logic and Optetrak groups (0.34% vs. 10.70%, respectively). The revision rates were 1.15% for the Logic group and 2.0% for the Optetrak group. However, there was a significant difference in rates of revision performed because of osteolysis, favoring the Logic group (0.07% vs. 0.6%). The Kaplan–Meier survivorship curve shows a significant difference in time until revision between the Logic and Optetrak groups.
Conclusion
Design modifications to improve patellofemoral mechanics demonstrated significant improvements in overall pain and patellofemoral pain and reduced manipulation rates post-operatively.
Keywords: total knee replacement, patellofemoral pain, range of motion, clinical outcomes, manipulation, revision
Introduction
Total knee arthroplasty (TKA) is recognized as an effective treatment for relieving pain and restoring joint function in arthritic knees. However, only 43% of patients report being pain free 2 years after a primary TKA procedure [5]. Anterior knee pain is also observed following TKA, and patellofemoral issues are a common source of knee complaints. While posterior-stabilized (PS) knee systems rely on a cam-and-post articulation, the patellofemoral mechanics are quite complicated and a function of the design of the femoral component, the depth of the trochlear groove, the retinacular tension, and other surgical factors such as component size, stability, and alignment [3].
Design engineers strive to optimize patellofemoral mechanics in PS knee systems in order to make the TKA procedure easier, faster, and more consistent and with improved patient satisfaction. The focus on a reduction in anterior knee pain can reveal the extent to which these changes were implemented [6]. The Logic® PS knee system (Exactech Inc., Gainesville, FL, USA) was designed as an advancement to its predecessor, the Optetrak PS system, in reducing patellofemoral pain and improving knee kinematics by offering a redesigned patellofemoral articulation with a left and right specific femoral component and a redesigned trochlear region. Particularly, the left and right specific femoral component and use of half sizes increase the femoral congruency from 0.94 to 0.96, which acts to reduce contact stress by 20% [1]. This change also assists with patellar engagement and patellar tracking and reduces changes of medial overhang of the femoral component proximally on the anterior flange. In addition, the redesigned trochlear region requires less bone removal and simplifies the notch preparation to reduce stress concentrations. Together, these changes have the potential to reduce anterior knee pain in a clinical setting. All other aspects of the design, including the use of net compression molded, non-highly cross-linked polyethylene for the tibial insert and patella, were identical.
We sought to compare the newer Logic PS knee system to the Optetrak PS design in order to assess whether the newer Logic PS knee system resulted in reduced pain, particularly in the anterior knee, as well as other patient-reported outcome measures (PROMs) evaluated in a clinical setting. Outcomes were measured using two questionnaires for a clinical evaluation of function and self-reported function, respectively: the Knee Society Clinical Rating System (KSCRS) and the McMaster Universities Osteoarthritis Index (WOMAC), a questionnaire of self-reported overall health. The Veterans Rand 12-Item Health Survey (VR-12) and a questionnaire of physical activity levels, the University of California Los Angeles Activity Scale (UCLA), were also used.
Methods
We retrospectively reviewed our institutional registry for all TKAs performed using the Logic PS system by a single surgeon with a minimum 2-year follow-up. For comparison, we retrospectively reviewed our institutional registry for all TKAs performed using a previous version of the knee design, the Optetrak PS, performed by the same surgeon with a minimum 2-year follow-up. The study consisted of 1482 Logic PS TKAs and 445 Optetrak PS TKAs from 2000 to 2018, not counting 12 patients in the Logic PS group and 20 in the Optetrak PS group who were deceased. The average follow-up in the Logic PS group was 2.64 years (range 2–9 years) and in the Optetrak PS group was 4.62 years (range 2–19 years).
Patient demographics in both groups were similar (Table 1). Females represented 60% of the Logic PS group and 62% of the Optetrak PS group. The average body mass index (BMI) was 30.76 in the Logic PS group and 31.20 in the Optetrak PS group.
Table 1.
Demographic breakdown between the two cohorts
| Logic | Optetrak | p | |
|---|---|---|---|
| Total knees | 1494 | 475 | NA |
| Knees available for analysis | 1482 | 445 | NA |
| Male/female | 596/886 | 169/276 | 0.40 |
| Age (years), mean | 66.74 | 68.64 | 0.32 |
| Body mass index, mean | 30.76 | 31.20 | 0.64 |
| Average follow-up (years) | 2.64 | 4.62 | < 0.001 |
Compared with the Optetrak PS, the Logic PS has a high-flexion cam-and-post design that allows 145° of motion, a more “patellofemoral friendly” design with a deeper trochlear groove, and a reduction of metal on either side of the trochlear groove to allow less retinacular tension (Fig. 1). The left and right specific femoral components and the use of half sizes reduce bony overhang anteriorly.
Fig. 1.
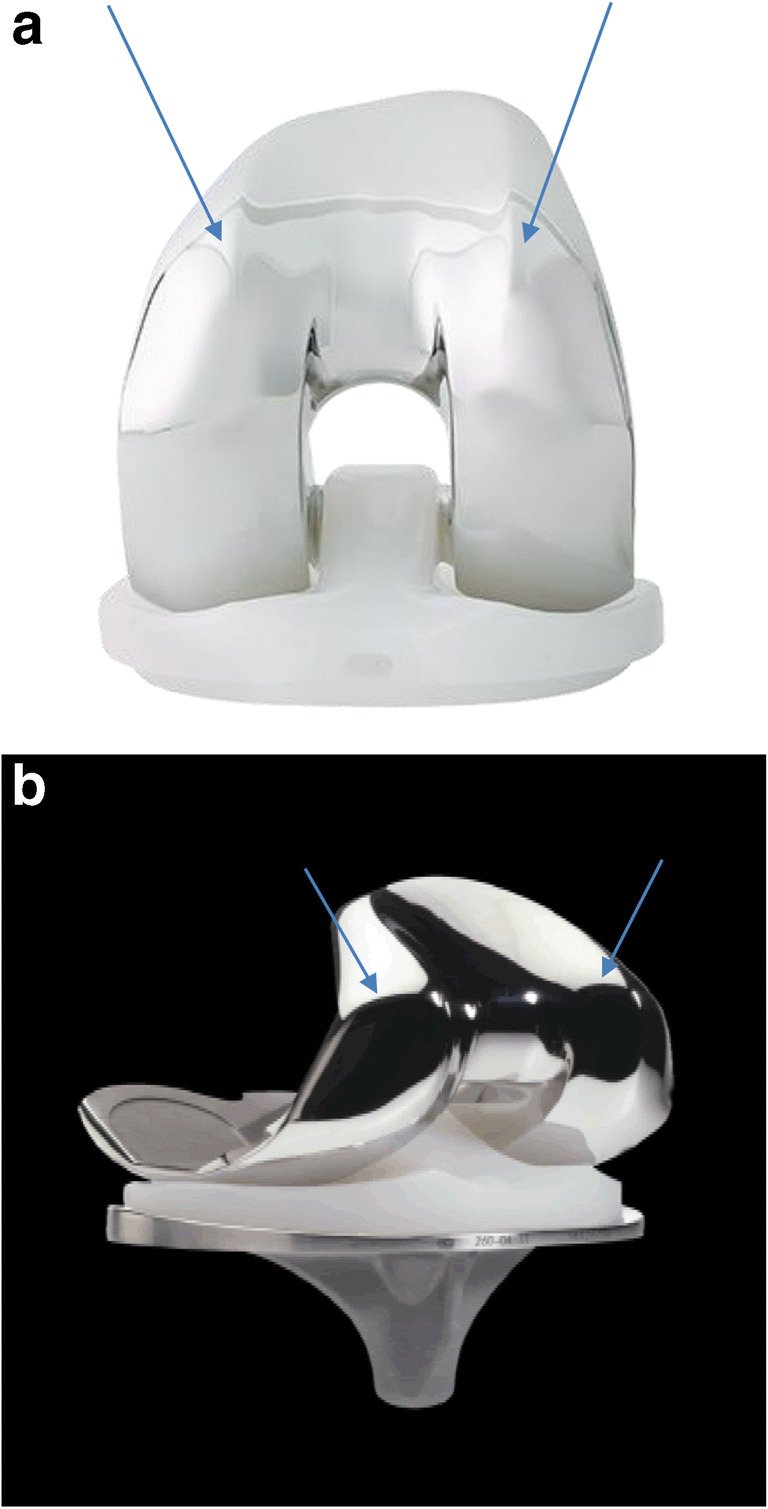
a The Logic PS implant shows a reduction in metal on either side of the trochlear groove, which allows for less retinacular tension (arrows). In addition, the bony overhang is anteriorly reduced by the left and right specific femoral component and the use of half sizes. b The Optetrak PS implant has noticeably more metal on either side of the trochlear groove (arrows) and is less smooth than the Logic PS. In addition, the bony overhang is greater due to the lack of femoral-specific components.
Clinical data were collected from the latest post-operative visits included in our institutional database. Data collected and measured by the attending orthopedic surgeon (G.H.W.) at the patients’ follow-up appointments included range of motion (ROM), the KSCRS, the UCLA, the pain VAS (visual analog scale), the VR-12 for self-reported global health, the WOMAC, and anterior knee pain (yes/no). Survey forms were collected on paper and verified by a research assistant prior to entry in our institutional database. Revision rates and manipulation rates were compared for each cohort. Manipulation of the knee took place if the patient had less than 90° ROM 6 or more weeks post-surgery and after physical therapy had not improved ROM. Incidence of and reason for revision were identified and analyzed as well. In addition, the Kaplan-Meier survivorship curve, defining failure as need for revision, was calculated to allow comparison between the cohorts. Statistical analysis was performed by our biostatisticians to compare any differences between the two systems; p values for outcome scores of KSCRS, UCLA, VR-12, WOMAC, anterior knee pain, manipulation rate, and revision rate were obtained with a two-sample t test comparing the two groups. We used a p value of < 0.05 as a value of significance in this analysis.
Results
The Logic PS knee system cohort had less overall pain, with a reduced average pain VAS score (1.72 vs. 2.75 on a scale of 0 to 10, p < 0.001), less anterior knee pain (5.6% vs. 11.8% of patients, p < 0.001), and a lower manipulation rate (0.34% vs. 10.70% of patients, p < 0.001) at their latest follow-up (Table 2). There were no differences in the recorded ROM or in KSCRS, UCLA, VR-12, and WOMAC scores between the Logic PS and Optetrak PS cohorts (Table 2).
Table 2.
Patient-reported outcome measures (PROMs) and complications between the two cohorts
| Logic | Optetrak | p | |
|---|---|---|---|
| Post-op, mean | Post-op, mean | ||
| ROM—degrees | 112.62 | 107.03 | 0.11 |
| UCLA score—on a scale of 1 to 10, 10 being the best | 4.80 | 4.85 | 0.78 |
| WOMAC score—out of 96, 96 being the worst | 74.02 | 75.74 | 0.36 |
| Pain VAS—on a scale of 0 to 10, 10 being the worst | 1.72 | 2.75 | < 0.001 |
| VR-12 score, lower being worse | 40.35 | 38.74 | 0.10 |
| Anterior knee pain—% of patients | 5.6% | 11.8% | < 0.001 |
ROM range of motion, UCLA University of California Los Angeles Activity Scale, WOMAC Western Ontario and McMaster Universities Osteoarthritis Index, VAS visual analog scale, VR-12 Veterans Rand 12-Item Health Survey
The causes of revision were comparable, except for osteolysis, which was less common with the Logic PS design (p = 0.01) (Table 3). There was a low revision rate in each cohort: 1.15% in the Logic PS cohort and 2.0% in the Optetrak PS cohort (p = 0.16).
Table 3.
Cause of revision in each cohort
| Logic (n = 1482) | Optetrak (n = 445) | p | |
|---|---|---|---|
| % follow-up group (n) | % follow-up group (n) | ||
| Revisions | |||
| All causes | 1.15% (17) | 2.0% (9) | 0.16 |
| Infection | 0.1% (2) | 0.4% (2) | 0.93 |
| Aseptic loosening | 0.7% (11) | 0.2% (1) | 0.22 |
| Instability | 0.2% (3) | 0.6% (3) | 0.11 |
| Osteolysis | 0.07% (1) | 0.6% (3) | 0.01 |
| Periprosthetic fracture | 0% (0) | 0% (0) | NA |
| Manipulation | 0.34% (5) | 10.70% (48) | < 0.001 |
The Kaplan–Meier survivorship curve revealed a difference in terms of longevity: the average time to revision was 14.89 months in the Logic group and 13.75 months in the Optetrak group. This difference was not statistically significant. At 48 months, the survival rate was 94% (95% confidence interval [CI] 93–95%) for the Logic PS and 82% (95% CI 78–86%) for the Optetrak.
Discussion
The purpose of this study was to compare the Logic PS knee design to an earlier version, the Optetrak PS design. We assessed PROMs, ROM, overall pain, patellofemoral pain, and incidence of manipulation and revision in both cohorts. We found a lower incidence of overall pain and patellofemoral pain in the Logic PS group. These results support our hypothesis that changes in the design would result in improved patient outcomes, particularly anterior knee pain.
We acknowledge limitations in the study. We decided not to match the groups for BMI and sex so that we could include a much larger number of patients and an extended follow-up period for the Logic PS group. However, our statistician noted that there were no significant differences between the groups in BMI, age, or sex. Also, the use of one surgeon (G.H.W.) in a nonblinded fashion is a potential source of bias, but the uniformity in the protocol (strict adherence to 90° ROM) at a high-volume practice helped to mitigate the potential for bias in the rate of manipulation. Since the Optetrak PS implants pre-date the Logic PS implants, it is possible that surgical technique and the type of cement used could have more impact on outcomes than design modifications. However, the uniformity in surgical procedure by the same surgeon reduces this concern. Finally, the significant difference in the latest follow-up (Fig. 2) revealed improved longevity until revision of the Logic PS implant, as compared with the Optetrak PS implant. The follow-up differences are mitigated by the large patient population, similarity in patient demographics, and Kaplan–Meier survivorship curve. In addition, we hope to continue to examine the relationship between design changes and contact patterns and articular surface damage in the future.
Fig. 2.
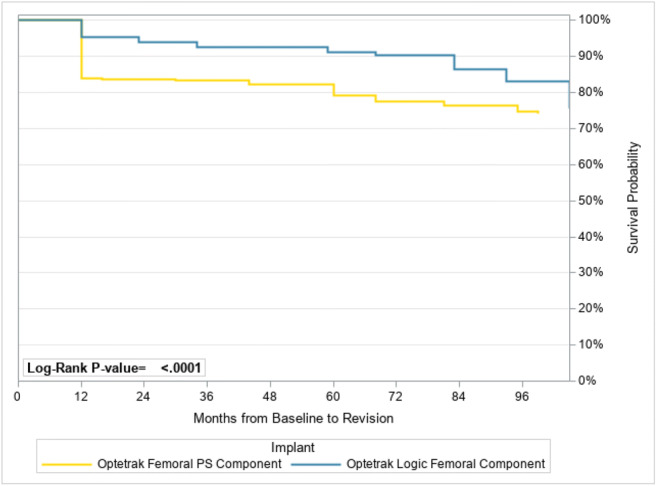
Kaplan–Meier survival curve.
Ruel et al. conducted a much smaller matched-pair study comparing the Logic PS and the Optetrak PS [9]. Results indicated that the Logic PS reduced anterior knee pain, reduced bone resection in the femoral box, and improved ROM. They also noted a reduction in pain and patellar clunk that were observed in earlier designs. However, they did not examine anterior knee pain directly, using only the Knee Society Score as a proxy for it. We found no significant difference in WOMAC scores between the groups (Table 1) but did find a reduction in anterior knee pain, which suggests the relationship between design modifications and anterior knee pain can be established. Our findings suggest that the increased femoral congruency, reduction in contact stress, and reduction in bone play a direct role in reducing anterior knee pain.
Gilbert et al. confirmed the impact of the Logic PS modifications to the anterior face of the tibial post and corresponding anterior articulating surface of the femoral component [4]. This design change reduced edge loading on the polyethylene post. In addition to the reduction of stresses from a rounded contact geometry of the tibial post, the redesign led to a reduction in deformation and surface damage on the tibial post.
Ehrhardt et al. demonstrated improved clinical outcomes of the Optetrak PS, with improvement in Knee Society pain scores from 5.3 pre-operatively to 44.6 post-operatively and ROM from 105° pre-operatively to 120° post-operatively over an average 7-year follow-up [2]. The authors suggested that the deepened patellar sulcus and truncation of the patellar flange may account for the reduction in pain scores and improvement in ROM, but as did Ruel et al., they used the Knee Society Score as a proxy for anterior knee pain.
An additional study by Robinson found a survivorship rate of 97% in 66 Optetrak knees with a minimum of 5 years of follow-up [7]. In this study, 90% of patients rated “good” or “excellent” on the internal outcome scores, the HSS Knee Score and the Knee Society Score. The negative correlation that they suggested exists between BMI and Knee Society Score was addressed by having similar patient populations with regard to BMI. This is consistent with the low revision rates in our current study for Logic PS (1.15%) and Optetrak PS (2.0%).
In terms of manipulation rates, our finding of 0.34% for the Logic PS knee is much lower than that in a 2010 study of 800 TKAs at 1-year of follow-up (4.6%) [8]. A previous 7-year survivorship study of the Optetrak PS knee found a manipulation rate of 12.3%, which is consistent with another study that found a manipulation rate of 13% with Optetrak PS knees at an average 4-year follow-up [2, 8]. Clearly, the reduction in manipulation rates is multifactorial and can be related to improved pain management over time, as well as implant design improvements.
Our revision rates of 1.15% for the Logic PS and 2.0% in the Optetrak PS are consistent with a 7-year average follow-up that showed a revision rate of 1.8% with the Optetrak PS system [2]. Of note in our current study, the majority of Logic PS revisions were due to aseptic loosening, a rate of only 0.7% (Table 3). The majority of Optetrak PS revisions were due to instability and osteolysis (0.6% each), higher percentages than with the Logic PS (0.2% and 0.07%, respectively). Further studies are needed to examine the relationship between osteolysis and contact stress, although it is reasonable to attribute the reduction in osteolysis to the reduction in contact stress in the Logic PS design.
We report favorable results from the Logic PS system overall. The patients showed good clinical outcomes with improvement in pain and function, primarily a significant reduction in anterior knee pain and reduced manipulation rates. We did find similarity in ROM between the cohorts, which is an interesting finding given the disparity in past studies.
The Kaplan–Meier survivorship curve revealed that the survival rate at the latest follow-up was 92% for Logic PS at 2.6 years and 82% for Optetrak PS at 4.62 years, which were the respective time points of the latest follow-up for our cohorts. Robinson and Ehrhardt et al. showed a survivorship estimate until revision for Optetrak PS of 97% at 7.75 years and 97% at 10 years’ follow-up, respectively [2, 7]. Table 3 still provides support for the longevity of the Logic PS, with a revision rate of only 1.15% in a cohort of 1482.
Although our study is retrospective in nature, our findings demonstrate a reduction in anterior knee pain, overall pain, and incidence of manipulation post-operatively with the newer Logic PS design in a large number of patients. Our findings suggest that the reduction in anterior knee pain may be attributed to the design modifications in the Logic PS compared with the Optetrak PS, particularly the reduction in bone on either side of the trochlear groove and the left and right specific femoral components. In addition, there is evidence to support the improved longevity of the Logic implant from the Kaplan–Meier survivorship curve. Future study should examine the relationship between design modification and revisions performed as a result of osteolysis.
Compliance with Ethical Standards
Conflict of Interest
Jeremy A. Dubin, BA, and Ahava Muskat, BA, declare that they have no conflicts of interest. Geoffrey H. Westrich, MD, reports personal fees from Exactech, during the conduct of this study.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III: Retrospective Cohort Study
References
- 1.Bartel DL, Bicknell VL, Wright TM. The effect of conformity, thickness, and material on stresses in ultra-high molecular weight components for total joint replacement. J Bone Joint Surg Am. 1986;68(7):1041–1051. [PubMed]
- 2.Ehrhardt J, Gadinsky N, Lyman S, Markowicz D, Westrich G. Average 7-year survivorship and clinical results of a newer primary posterior stabilized total knee arthroplasty. HSS Journal. 2011;7(2):120–124. [DOI] [PMC free article] [PubMed]
- 3.Furman BD, Lipman J, Kligman M, Wright TM, Haas SB. Tibial post wear in posterior-stabilized knee replacements is design-dependent. Clin Orthop Relat Res. 2008; 466(11):2650–2655. [DOI] [PMC free article] [PubMed]
- 4.Gilbert SL, Rana AJ, Lipman JD, Wright TM, Westrich GH. Design changes improve contact patterns and articular surface damage in total knee arthroplasty. Knee. 2014;21(6):1129–1134. [DOI] [PubMed]
- 5.Mannion AF, Kämpfen S, Munzinger U, Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther. 2009;11(5):R139. [DOI] [PMC free article] [PubMed]
- 6.Petersen W, Rembitzki IV, Brüggemann GP, et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop. 2014;38(2):319–328. [DOI] [PMC free article] [PubMed]
- 7.Robinson RP. Five-year follow-up of primary Optetrak posterior stabilized total knee arthroplasties in osteoarthritis. J Arthroplasty. 2005;20(7):927–931. [DOI] [PubMed]
- 8.Rubinstein Jr RA, DeHaan A. The incidence and results of manipulation after primary total knee arthroplasty. Knee. 2010;17(1):29–32. [DOI] [PubMed]
- 9.Ruel A, Pui C, Westrich G. Design modifications may improve range of motion following posteriorly stabilized total knee replacement: a matched pair study. HSS J. 2014;10(3):256–259. [DOI] [PMC free article] [PubMed]


