Abstract
Background
The use of regional anesthesia (RA) in pediatric patients remains understudied, although evidence suggests benefits over general anesthesia.
Questions/Purposes
We sought to identify factors associated with RA use in patients under the age of 21 years undergoing ambulatory orthopedic surgery.
Methods
Patients under the age of 21 who underwent anterior cruciate ligament (ACL) repair or reconstruction, knee arthroscopy (KA), or shoulder arthroscopy (SA) were identified from the NY Statewide Planning and Research Cooperative System (SPARCS) database (2005–2015). Frequencies of RA use (defined by femoral nerve block, spinal, epidural, caudal, or brachial plexus anesthesia) were calculated. Multivariable regression analysis identified patient- and healthcare system–related factors associated with the use of RA. Odds ratios (OR) and 95% confidence intervals (CI) were reported.
Results
We identified 87,273 patients who underwent the procedures of interest (ACL n = 28,226; SA n = 18,155; KA n = 40,892). In our primary analysis, 14.4% (n = 1404) had RA as their primary anesthetic; this percentage increased for patients who had ACL or KA. When adjusting for covariates, Hispanic ethnicity (OR 0.78; CI 0.65–0.94) and Medicaid insurance (OR 0.75; CI 0.65–0.87) were associated with decreased odds for the provision of RA. Further, we identified increasing age (OR 1.10; CI 1.08–1.11), ACL versus SA (OR 1.91; CI 1.74–2.10), and sports injuries (OR 1.20; CI 1.10–1.31) as factors associated with increased odds of RA use.
Conclusion
In this analysis, RA was used in a minority of patients under the age of 21 undergoing ambulatory orthopedic surgery. Older age was associated with increased use while Hispanic ethnicity and lower socioeconomic status were associated with lower use.
Electronic supplementary material
The online version of this article (10.1007/s11420-020-09805-0) contains supplementary material, which is available to authorized users.
Keywords: anesthesia, local anesthesia, general anesthesia, pediatrics, arthroscopy
Program Description: This HSS Journal® continuing medical education (CME) activity has been developed by the journal editors. After completing this activity, learners will be able to demonstrate an increase in or affirmation of their knowledge of the relevant topic. They will also be able to evaluate the appropriateness of clinical data and apply it to their practice and the provision of patient care.
Program Format: In each edition, HSS Journal contains one clinically relevant article selected by the editors to be designated for CME credit.
Accreditation: Hospital for Special Surgery (HSS) is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide CME for physicians. HSS designates this journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Disclosure Information: None of the individuals in a position to control the content of this CME activity have any relevant financial relationships to disclose.
Completion Requirement: To complete the activity and earn credit, the participant must read the article, complete an online knowledge assessment with a score of 100%, and complete the evaluation.
To complete the activity and earn CME credit:
Go to http://bit.ly/HSSJournalCME2020 to access the course. Please note that first-time users will need to create a free HSS eAcademy® account to access the course page.
Register for the activity, proceed through the article, and complete the post-course knowledge assessment.
-
Once you have completed the knowledge assessment with a score of 100%, you will be prompted to complete an evaluation and generate your certificate of CME credit.
If you have questions, please email professionaleducation@hss.edu or phone 212–606-1057.
Introduction
A number of studies have suggested that regional anesthesia (RA) may benefit patients undergoing orthopedic surgery [3, 5, 11]. However, data is rare on its use among pediatric and adolescent patients. With sport-related injuries increasing in this patient demographic, an increasing number of patients present for diagnostic and therapeutic surgery [4, 18]. In this population, for example, anterior cruciate ligament (ACL) injury has been shown to be more common than previously thought [4, 14, 18]. ACL injuries account for 6.3% of all sports injuries between the ages of 5 and 12 years and 10.3% between 13 and 17 years [14]. Dodwell et al. estimate that 50 per 100,000 pediatric patients ages 10 to 19 years old undergo ACL reconstruction per year [4]. Similar increases in shoulder procedures have been reported.
It has been suggested that the use of regional techniques, including peripheral nerve blocks, may be associated with more effective pain control and improved early recovery [17]. In pediatric patients undergoing ACL repair, benefits attributed to the use of peripheral nerve blocks include a reduction in opioid consumption, decreased post-operative pain scores, decreased hospital length of stay, and a reduction in post-operative admission rates [9, 13]. Therefore, experts recommend RA techniques to be used as part of a multimodal regimen [17]. With publications by the Pediatric Regional Analgesia Network suggesting that complications are extremely rare, RA techniques should be used routinely in pediatric anesthesia [12, 16].
Despite these suggested benefits, there are few studies exploring the use of RA on a population level. We therefore sought to analyze a state-wide cohort to explore trends and identify factors associated with the use of regional anesthesia in patients below the age of 21 years undergoing ambulatory orthopedic procedures over a 10-year period. We hypothesized that RA use would increase over time and that patient and healthcare system factors associated with its use could be identified.
Methods
Approval for this retrospective study was obtained from the Institutional Review Board, which waived the requirement for informed consent. Data collected for the NY Statewide Planning and Research Cooperative System (SPARCS) database was accessed for the years between 2005 and 2015. We identified patients from the ages of 3 to 21 years who had undergone the following events: shoulder arthroscopy, shoulder fracture, humerus/elbow arthroscopy, humerus/elbow fracture, forearm/wrist arthroscopy, forearm/wrist fracture, hand/fingers fracture, hip arthroscopy, pelvis/hip fracture, knee arthroscopy, anterior cruciate ligament repair, femur/knee fracture, leg/ankle arthroscopy, and leg/ankle fracture. Subsequently, the population of 144,965 procedures was narrowed to patients who had undergone ACL repair, knee arthroscopy (KA), and shoulder arthroscopy (SA) as our main cohort for further analysis (n = 87,273). Those who reported both ACL and KA were categorized as ACL. All were defined by the Current Procedural Terminology (CPT) diagnosis codes (see Appendix I for detailed definitions).
Patient-related variables included age, sex, race (Asian, black, white, other, and unknown), Hispanic ethnicity, NY state residency, type of insurance (Medicaid, private, other, and unknown), and whether the injury was a sports injury. Hospital-related variables included location (urban, rural), procedure type, and year of procedure. Anesthesia type is a SPARCS-defined variable derived from patient anesthesia records. If more than one anesthesia type was administered, primary anesthesia was defined by the database in hierarchical order: general, regional, other, and local. Those without anesthesia information were categorized as “unknown.”
Use of RA was the main outcome of interest. It was defined as including spinal anesthesia, epidural anesthesia, caudal anesthesia, brachial plexus anesthesia (including axillary block, interscalene block, and supraclavicular block), and femoral nerve block.
Statistical Analysis
First, overall trends of major orthopedic ambulatory procedures were assessed over time by the Cochran-Armitage tests. Then, individual trends of ACL, KA, and SA by sports injury and year, as well as anesthesia type by year, were obtained. Use of RA over time was also assessed by the Cochran-Armitage test and explored by patient, hospital, and procedure characteristics. χ-squared tests evaluated group differences. Standardized differences, in addition to p values, were included to further measure relationships due to our large sample size [1, 20]. Multilevel multivariable regression analysis was subsequently performed to identify factors associated with the use of RA, which accounted for the correlation of patients within hospitals.
Due to a large number of individuals with missing anesthesia information, those with “unknown” anesthesia type were excluded from the initial model. To further examine the effect this had on our initial results, two models were run: unknown coded as “RA = no” and unknown coded as “RA = yes.” Subsequently, evaluating hospital-specific percentage of RA use allowed us to identify a potential issue with zero-inflation. Additional sensitivity analysis was then performed where hospitals with 0% RA use were excluded from the model.
All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA), and statistical significance was defined as a 2-sided p value of < 0.05.
Results
A total of 159,629 pediatric patients were identified who underwent ambulatory orthopedic surgeries between 2005 and 2015. Table 1 provides information on surgeries and total sports injuries by year. The incidence of surgeries increased within the decade observed, although the proportion of sports injuries decreased over time.
Table 1.
Pediatric orthopedic ambulatory surgeries identified in SPARCS (2005–2015)
| Procedure | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Shoulder arthroscopy | 1167 | 1433 | 1530 | 1644 | 1768 | 1867 | 1792 | 1840 | 1792 | 1677 | 1685 |
| Shoulder fracture | 52 | 70 | 124 | 133 | 150 | 187 | 232 | 260 | 279 | 287 | 343 |
| Humerus/elbow arthroscopy | 69 | 95 | 85 | 98 | 93 | 100 | 91 | 101 | 106 | 111 | 85 |
| Humerus/elbow fracture | 315 | 396 | 389 | 444 | 445 | 449 | 475 | 604 | 627 | 695 | 737 |
| Forearm/wrist arthroscopy | 123 | 157 | 144 | 200 | 163 | 150 | 121 | 160 | 120 | 125 | 147 |
| Forearm/wrist fracture | 210 | 233 | 543 | 645 | 638 | 727 | 697 | 741 | 733 | 750 | 702 |
| Hand/fingers fracture | 968 | 1067 | 1156 | 1246 | 1297 | 1310 | 1242 | 1317 | 1314 | 1409 | 1397 |
| Pelvis/hip arthroscopy | 63 | 103 | 121 | 164 | 241 | 274 | 342 | 373 | 438 | 485 | 478 |
| Pelvis/hip fracture | 8 | 4 | 5 | 7 | 6 | 8 | 4 | 13 | 8 | 10 | 6 |
| Femur/knee arthroscopy | 4130 | 4691 | 4591 | 4928 | 5046 | 5351 | 5105 | 5323 | 5314 | 5186 | 4910 |
| ACL repair | 1690 | 1996 | 2104 | 2224 | 2569 | 2764 | 2687 | 2941 | 3002 | 3156 | 3119 |
| Femur/knee fracture | 64 | 81 | 75 | 88 | 76 | 114 | 103 | 109 | 125 | 142 | 134 |
| Leg/ankle arthroscopy | 164 | 223 | 244 | 241 | 262 | 293 | 264 | 271 | 313 | 277 | 310 |
| Leg/ankle fracture | 453 | 448 | 486 | 475 | 533 | 554 | 613 | 593 | 641 | 648 | 686 |
| Total | 9476 | 10,997 | 11,597 | 12,537 | 13,287 | 14,148 | 13,768 | 14,646 | 14,812 | 14,958 | 14,739 |
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
| Sports injury | 1496 | 1679 | 1758 | 1841 | 1885 | 2067 | 1917 | 2028 | 2032 | 2053 | 1985 |
| % (accidents of total procedures) | 15.8 | 15.3 | 15.2 | 14.7 | 14.2 | 14.6 | 13.9 | 13.9 | 13.7 | 13.7 | 13.5 |
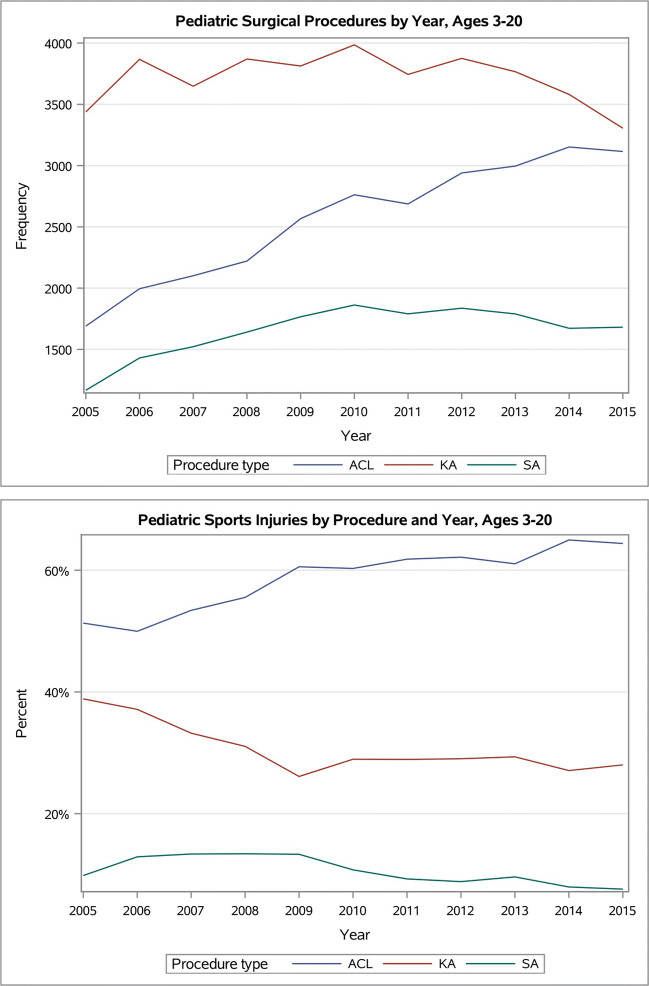
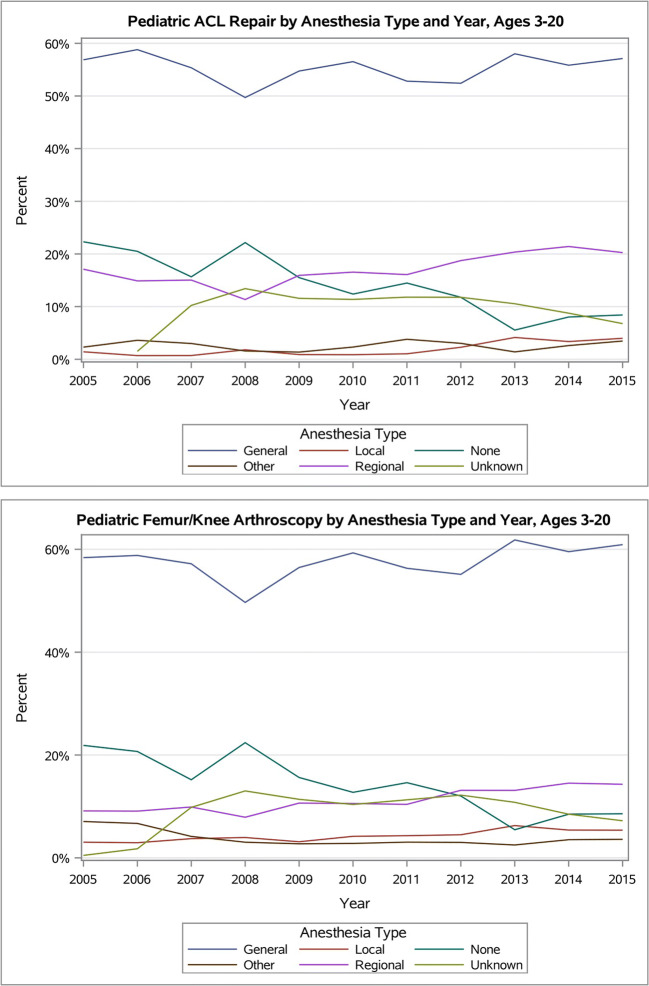
Our primary cohort consisted of 28,226 ACL, 18,155 KA, and 40,892 SA patients. The Cochran-Armitage tests found significant trends within the three procedures over time. When further assessing the trends, ACL frequencies increased the most (Fig. 1a, b), SA increased modestly, and KA did not appear to follow a trend until decreasing after 2013. While the percentage of cases related to sports injuries declined among those undergoing KA and SA, those related to ACL increased over time. Trends of anesthesia type are shown in Fig. 2 a–c. General anesthesia was used most often throughout the years across all three procedures. Patients who underwent KA received local anesthesia more often than patients who had ACL or SA. After conducting a Cochran-Armitage test on RA use, significant trends were identified among ACL and KA cohorts (p values < 0.05).
Fig. 1.
Pediatric surgical procedures identified by year (2005–2015), by a frequency and b percent
Fig. 2.
a, b Trends of primary anesthesia type (2005–2015), by procedure type
Table 2 presents patient-, healthcare-, and procedure-related variables by RA use. Of the 79,190 patients undergoing ACL, KA, and SA surgeries with information on types of anesthesia, 11,404 (14.4%) had RA as the primary anesthetic. Higher frequencies of RA use were observed among those who were non-Hispanic, living in an urban location, and residents of the NY state. Those on Medicaid, having sports injury, or having an ACL received RA more frequently. The incidence of RA use appeared to increase annually, starting at 12.6% in 2005 and reaching 17.0% in 2015.
Table 2.
Regional anesthesia use in pediatric anterior cruciate ligament reconstruction, knee arthroplasty, and shoulder arthroplasty procedures (n = 11,404)
| Characteristics | n | % | p value | Standardized difference |
|---|---|---|---|---|
| Age group | 0.006 | 0.035 | ||
| 3–10 | 101 | 16.7 | ||
| 11–14 | 1376 | 14.7 | ||
| 15–18 | 6821 | 14.1 | ||
| 19–20 | 3106 | 15.0 | ||
| Sex | 0.002 | 0.031 | ||
| Female | 4888 | 14.9 | ||
| Male | 6516 | 14.1 | ||
| Race | < 0.001 | 0.235 | ||
| Asian | 89 | 9.8 | ||
| Black | 575 | 9.7 | ||
| Other | 1289 | 10.8 | ||
| Unknown | 1007 | 23.5 | ||
| White | 8444 | 15.0 | ||
| Hispanic status | < 0.001 | − 0.138 | ||
| No | 11,117 | 14.7 | ||
| Yes | 287 | 7.6 | ||
| Procedure year | < 0.001 | 0.203 | ||
| 2005 | 791 | 12.6 | ||
| 2006 | 801 | 11.2 | ||
| 2007 | 897 | 13.8 | ||
| 2008 | 708 | 10.7 | ||
| 2009 | 944 | 13.1 | ||
| 2010 | 1068 | 13.9 | ||
| 2011 | 927 | 12.8 | ||
| 2012 | 1230 | 16.2 | ||
| 2013 | 1366 | 17.9 | ||
| 2014 | 1389 | 18.1 | ||
| 2015 | 1283 | 17.0 | ||
| Location | < 0.001 | − 0.318 | ||
| Rural | 120 | 2.1 | ||
| Urban | 11,284 | 13.8 | ||
| In-state | < 0.001 | − 0.717 | ||
| No | 3374 | 53.8 | ||
| Yes | 8030 | 11.0 | ||
| Insurance | < 0.001 | 0.391 | ||
| Medicaid | 390 | 5.7 | ||
| Other | 142 | 6.2 | ||
| Private | 6717 | 19.0 | ||
| Unknown | 4155 | 12.0 | ||
| Sports injury | < 0.001 | 0.481 | ||
| No | 7515 | 11.4 | ||
| Yes | 3889 | 28.9 | ||
| Procedure type | < 0.001 | 0.298 | ||
| ACL repair | 4919 | 19.2 | ||
| Knee arthroscopy | 4071 | 10.9 | ||
| Shoulder arthroscopy | 2414 | 15.0 |
*8083 missing anesthesia variable not included
Results of the multivariable regression model are presented in Table 3. When adjusting for covariates, Hispanic ethnicity (OR 0.78; CI 0.65–0.94) and Medicaid insurance status (OR 0.75; CI 0.65–0.87) were associated with decreased odds for the provision of RA. In addition, we identified increasing age (OR 1.10; CI 1.08–1.11), ACL versus shoulder surgery (OR 1.91; CI 1.74–2.10), and surgery for sports injuries (OR 1.20; CI 1.19; 1.31) as factors for increased use of RA. The C-statistic for the model was > 0.9.
Table 3.
Multivariable multilevel regression results for regional anesthesia use
| Characteristics | OR [95% CI] | p value |
|---|---|---|
| Age, continuous | 1.10 [1.08, 1.11] | < 0.001 |
| Sex | ||
| Female | 0.99 [0.92, 1.06] | 0.742 |
| Male | Reference | |
| Race | ||
| Asian | 0.76 [0.54, 1.09] | < 0.001 |
| Black | 0.93 [0.81, 1.07] | |
| Other | 1.11 [0.99, 1.24] | |
| Unknown | 1.39 [1.19, 1.63] | |
| White | Reference | |
| Hispanic status | ||
| Yes | 0.78 [0.65, 0.94] | 0.009 |
| No | Reference | |
| Procedure year | ||
| 2006 | 0.76 [0.65, 0.89] | < 0.001 |
| 2007 | 0.92 [0.78, 1.08] | |
| 2008 | 0.51 [0.43, 0.60] | |
| 2009 | 0.63 [0.54, 0.75] | |
| 2010 | 0.68 [0.53, 0.87] | |
| 2011 | 0.45 [0.34, 0.58] | |
| 2012 | 0.60 [0.46, 0.77] | |
| 2013 | 0.81 [0.63, 1.05] | |
| 2014 | 1.04 [0.80, 1.35] | |
| 2015 | 0.96 [0.74, 1.24] | |
| 2005 | Reference | |
| Provider volume | 1.02 [0.81, 1.30] | 0.854 |
| Location | ||
| Rural | 0.66 [0.25, 1.75] | 0.400 |
| Urban | Reference | |
| In-state | ||
| No | 1.10 [1.00, 1.21] | 0.052 |
| Yes | Reference | |
| Insurance | ||
| Medicaid | 0.75 [0.65, 0.87] | < 0.001 |
| Other | 0.95 [0.75, 1.22] | |
| Unknown | 0.81 [0.66, 0.99] | |
| Private | Reference | |
| Sports injury | ||
| Yes | 1.20 [1.19, 1.31] | < 0.001 |
| No | Reference | |
| Procedure type | ||
| ACL repair | 1.91 [1.74, 2.10] | < 0.001 |
| Knee arthroscopy | 1.19 [1.09, 1.30] | |
| Shoulder arthroscopy | Reference | |
| C-statistic, 0.967 | ||
There were 8083 (10.2%) records removed from the primary analysis because anesthesia technique was listed as “unknown.” Online resource 1 presents the results of including missing data. When unknown anesthesia technique was included as RA = no, in-state status became significant. NY state residents were more likely to have RA administered (OR 1.11; CI 1.00–1.22) than those from other states. While Hispanic status was statistically significant in our original model at a p value of 0.01, including the missing cases as RA = no caused the variable to lose effect, and the p value changed to 0.051. When unknown anesthesia technique was included as RA = yes, sports injury was no longer found to be a significant predictor.
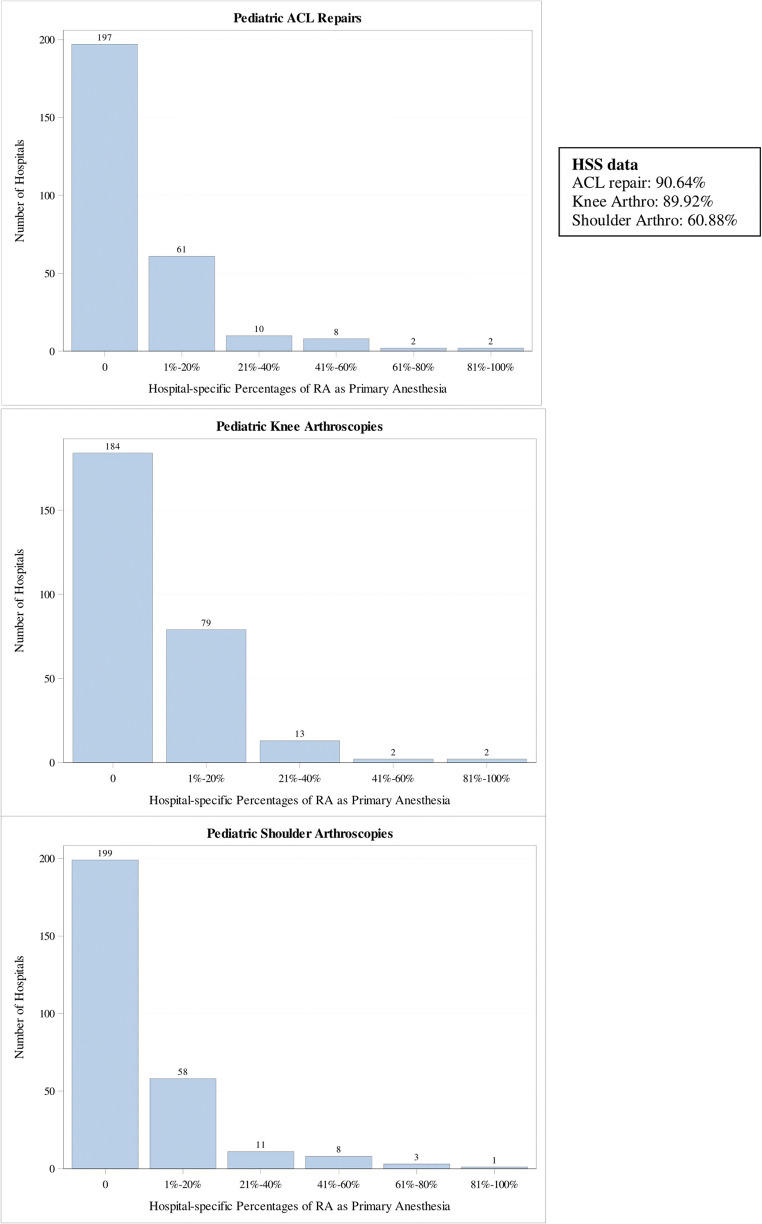
Hospital-level RA use was also explored (Fig. 3), where the number of hospitals were presented by percentage of use (categorized) for ACL, KA, and SA. Across the three procedures, hospitals with 0% RA use were most common (197, 184, and 199, respectively). The percentage of use appeared to decrease exponentially by category. For ACL and KA, two hospitals used RA in the range of 41 to 60%, and two in range of 81 to 100%, respectively. For SA, three hospitals showed 61 to 80% use, and only one had 81 to 100% use, respectively. Results were validated by identifying our own hospital’s percentage of RA use in the database and comparing it with that found in the SPARCS database. Supplementary Table 1 presents the results after excluding procedures done at hospitals with 0% RA use (n = 46,171; 58.3% of original cohort). Here, sex and race lost effect, but in-state status was significant (OR 1.12; CI 1.0–1.23).
Fig. 3.
a–c Hospital-level percentage of regional anesthesia use, by procedure
Discussion
In this study of population-based data collected in the NY state between 2005 and 2015, we found that despite previously reported benefits associated with RA and low related complication rates, these techniques were performed for a minority of patients.
Although, a trend toward increased use of RA was found over time, it remained well below 25%. After adjusting for covariates, Hispanic ethnicity and Medicaid insurance status were associated with decreased odds for the provision of RA, while increasing age, ACL versus SA, and surgery for sports injuries were factors associated with increased use of RA.
Recent literature has suggested an increase in the use of ambulatory pediatric orthopedic surgery in the USA [4, 15]. Using the SPARCS database, we found an increase in frequencies across multiple pediatric orthopedic procedures from 2005 to 2015. The percentage of these procedures that were ACL repairs increased, especially in comparison with KA and SA. We also observed an increase in ACL repairs categorized as sports injury cases, which supports the speculation that increased ACL repairs may be a result of higher sports participation at a younger age and earlier specialization in sports [2, 4, 6]. The rise of this particular procedure within young athletes may also be a result of the changing attitude from non-operative injury management to interventional approaches [7].
Across the three surgeries of interest, we found that general anesthesia was the main technique used. However, an upward trend of RA use in ACL and KA cohorts was observed. A lack of significant use in in shoulder procedures may be related to proximity to sensitive structures in the neck, making precise needle placement necessary. Many practitioners may believe this procedure requires ultrasound guidance, as suggested by Veneziano et al. [19]. However, the lower use of RA might also be explained by the fact that practitioners may not be as familiar with its use.
In our main multivariable model, variables significantly associated with the provision of RA included race, Hispanic status, and insurance type. Race and socioeconomic factors are known to be important components in determining patient outcomes, and previous research indicates that related variables influence peri-operative management of patients. In a prospective study by Ochroch et al., the authors reported that willingness to accept a different analgesic method as part of care for elective surgery was strongly affected by these factors [10]. Patient preferences could be a result of cultural considerations, and access to education on treatment can cause a nonmedical bias with negative perceptions to unfamiliar practices. Language barriers can also affect communication between patient and clinicians, causing difficulties especially when explaining complex treatment options that require patient participation. Finally, unconscious bias introduced by physicians (anesthesiologists and surgeons) may affect the choice of anesthesia, as has been previously suggested in patients undergoing joint arthroplasty [8].
While there are benefits to large-scale observational studies, one of the limitations in using an administrative database includes the lack of clinical details. No causalities can be established and no mechanisms behind trends can be determined. However, observed associations allow for the formation of hypotheses for future research. Variable accuracy and classification may also differ when reported by various centers. Errors in data collection and uncertain compliance are further factors, despite rigorous quality checks put in place to minimize such bias. In addition, because the data was collected in the NY state, our results may not be generalizable to a wider population, including other US states. The results of our study are also limited by missing data.
To address this issue, we performed sensitivity analyses. Interestingly, “unknown” anesthesia type caused effects of a number of study variables to change significance, and thus, related results need to be interpreted with caution. Exploring how demographic variables differ within this subset of patients may be of interest.
In conclusion, our analysis found that RA, despite reported benefits and low complication rates, is used in a minority of pediatric patients undergoing ambulatory orthopedic surgery, although the rate is increasing with time. The factors associated with increased use were older age and type of surgery. Lower rates of use were associated with minority race and lower socioeconomic status. Reasons for the low utilization and for observed disparities require further evaluation and research.
Electronic supplementary material
(DOCX 18 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
Appendix
Appendix I.
Procedure cohort definitions based on Common Procedural Terminology (CPT) codes
| Procedure Cohort | CPT Codes |
|---|---|
| Shoulder Arthroscopy | 29805, 29806, 29807, 29819, 29820, 29821, 29822, 29823, 29824, 29825, 29826, 28927, 29828 |
| Shoulder Fracture | 23515, 23585, 23615, 23616, 23630, 23670, 23680 |
| Humerus/Elbow Arthroscopy | 29830, 29834, 29835, 29836, 29837, 29838 |
| Humerus/Elbow Fracture | 24515, 24516, 24538, 24545, 24546, 24560, 24566, 24575, 24579, 24582, 24586, 24587, 24615, 24635, 24665, 24666, 24685 |
| Forearm/Wrist Arthroscopy | 29840, 29843, 29844, 29845, 29846, 29847, 29900, 29901, 29902 |
| Forearm/Wrist Fracture | 25515, 25525, 25526, 25545, 25574, 25575, 25606, 25607, 25607, 25608, 25609, 25628, 25645, 25651, 25652 |
| Hand/Fingers Fracture | 26608, 26615, 26650, 26665, 26727, 26735, 26746, 26756, 26765 |
| Pelvis/Hip Arthroscopy | 29860, 29861, 29862, 29863, 29914, 29915, 29916 |
| Pelvis/Hip Fracture | 27215, 27216, 27217, 27218, 27220, 27226, 27227,27228, 27235, 27236, 27244, 27245, 27248 |
| Femur/Knee Arthroscopy | 29850, 29851, 29855, 29856, 29870, 29871, 29873, 29874, 29875, 29876, 29877, 29879, 29880, 29881, 29882, 29883, 29884, 29885, 29886, 29887 |
| Anterior Cruciate Ligament Repair | 29888, 29889, 27409, 27427, 27428, 27429 |
| Femur/Knee Fracture | 27506, 27507, 27509, 27511, 27513, 27514, 27519, 27524, 27530, 27535, 27536, 27540, 27556,27557, 27558, 27566 |
| Leg/Ankle Arthroscopy | 29891, 29892, 29894, 29895, 29897, 29898, 29899 |
| Leg/Ankle Fracture | 27756, 27758, 27759, 27766, 27769, 27784, 27792, 27814, 27822, 27823, 27826, 27827, 27828, 27829, 27832, 27846, 27848 |
Funding
This study was funded internally by the Department of Anesthesiology, Critical Care and Pain Management, Hospital for Special Surgery, New York, NY.
Compliance with Ethical Standards
Conflict of Interest
Kathryn DelPizzo MD, Megan Fiasconaro MS, Lauren A. Wilson MPH, Jiabin Liu MD PhD, Jashvant Poeran MD PhD, and Carrie Freeman BS declare that they have no conflicts of interest. Stavros G. Memtsoudis, MD, PhD, MBA, FCCP, is a director on the boards of the American Society of Regional Anesthesia and Pain Medicine (ASRA) and the Society of Anesthesia and Sleep Medicine (SASM); he is a one-time consultant for Sandoz Inc. and Teikoku, is a medical advisory board member for HATH, and has a US patent application pending for a multicatheter infusion system: US-2017-0361063; and he is the owner of SGM Consulting, LLC, and co-owner of FC Monmouth, LLC.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III: Study design?
References
- 1.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck NA, Ganley TJ. Pediatric ACL injuries: Challenges and solutions, from prevention to operative reconstruction. University of Pennsylvania Orthopaedic Journal. 2011;21:50–55. doi: 10.1007/978-3-662-56127-0_17. [DOI] [Google Scholar]
- 3.Chelly JE, Ben-David B, Williams BA, Kentor ML. Anesthesia and post-operative analgesia: Outcomes following orthopedic surgery. Orthopedics. 2003;26:S865–S871. doi: 10.1111/os.12535. [DOI] [PubMed] [Google Scholar]
- 4.Dodwell ER, LaMont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York state. Am J Sports Med. 2014;42:675–680. doi: 10.1177/0363546513518412. [DOI] [PubMed] [Google Scholar]
- 5.Iannotti JP. A delayed physical therapy protocol that limited passive range of motion was similar to a protocol with early passive range of motion after rotator cuff repair. J Bone Joint Surg Am. 2012;94:2094. doi: 10.2106/JBJS.9422.ebo365. [DOI] [PubMed] [Google Scholar]
- 6.Janssen R, Lind M, Engebretsen L, Moksnes H, Seil R, Faunø P, et al. Pediatric ACL injuries: treatment and challenges. In: ESSKA instructional course lecture book. Edited by Kerkhoffs GMMJ, Haddad F, Hirschmann MT, Karlsson J, Seil R: Berlin, Heidelberg, Springer. 2018, pp 241-259. 10.1007/978-3-662-56127-0_17
- 7.Mall NA, Paletta GA. Pediatric ACL injuries: Evaluation and management. Curr Rev Musculoskelet Med. 2013;6(2):132–140. doi: 10.1007/s12178-013-9169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Memtsoudis SG, Poeran J, Zubizarreta N, Rasul R, Opperer M, Mazumdar M. Anesthetic care for orthopedic patients: Is there a potential for differences in care? Anesthesiology. 2016;124:608–623. doi: 10.1097/ALN.0000000000001004. [DOI] [PubMed] [Google Scholar]
- 9.Micalizzi RA, Williams LA, Pignataro S, Sethna NF, Zurakowski D. Review of outcomes in pediatric patients undergoing anterior cruciate ligament repairs with regional nerve blocks. J Pediatr Nurs. 2014;29:670–678. doi: 10.1016/j.pedn.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Ochroch EA, Troxel AB, Frogel JK, Farrar JT. The influence of race and socioeconomic factors on patient acceptance of peri-operative epidural analgesia. Anesth Analg. 2007;105:1787–1792. doi: 10.1213/01.ane.0000290339.76513.e3. [DOI] [PubMed] [Google Scholar]
- 11.Paul JE, Arya A, Hurlburt L, et al. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113:1144–1162. doi: 10.1097/MD.0000000000018056. [DOI] [PubMed] [Google Scholar]
- 12.Polaner DM, Martin LD, Investigators PRAN. Quality assurance and improvement: The pediatric regional anesthesia network. Paediatr Anaesth. 2012;22:115–119. doi: 10.1111/j.1460-9592.2011.03708.x. [DOI] [PubMed] [Google Scholar]
- 13.Schloss B, Bhalla T, Klingele K, Phillips D, Prestwich B, Tobias JD. A retrospective review of femoral nerve block for post-operative analgesia after knee surgery in the pediatric population. J Pediatr Orthop. 2014;34:459–461. doi: 10.1097/BPO.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 14.Stracciolini A, Casciano R, Levey Friedman H, Meehan WP, III, Micheli LJ. Pediatric sports injuries: An age comparison of children versus adolescents. Am J Sports Med. 2013;41:1922–1929. doi: 10.1177/0363546513490644. [DOI] [PubMed] [Google Scholar]
- 15.Tepolt FA, Feldman L, Kocher MS. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop. 2018;38:e49–e494. doi: 10.1097/BPO.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 16.Walker BJ, Long JB, De Oliveria GS, et al. Peripheral nerve catheters in children: An analysis of safety and practice patterns from the pediatric regional anesthesia network (PRAN) Br J Anaesth. 2015;115:457–462. doi: 10.1093/bja/aev220. [DOI] [PubMed] [Google Scholar]
- 17.Wardhan R, Chelly J. Recent advances in acute pain management: Understanding the mechanisms of acute pain, the prescription of opioids, and the role of multimodal pain therapy. F1000Res. 2017;6. 10.12688/f1000research.12286 [DOI] [PMC free article] [PubMed]
- 18.Werner BC, Yang S, Looney AM, Gwathmey FW. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36:447–452. doi: 10.1097/BPO.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 19.Veneziano G, Betran R, Bhalla T, Martin DP, Tobias JD. Peripheral regional anesthesia in infants and children: An update. Anaesth Pain Intensive Care. 2019;18:59–71. doi: 10.1016/j.accpm.2019.02.011. [DOI] [Google Scholar]
- 20.Yang D, Dalton JE. A unified approach to measuring the effect size between two groups using SAS®. SAS Global Forum. 2012;335:1–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 18 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)