Abstract
Background
As more adults undergo surgical fixation of clavicle fractures with improved outcomes, interest is renewed in managing clavicle fractures in adolescents. The medial clavicular physis does not fuse until 23 to 25 years of age, but studies report minimal clavicular growth during adolescence—studies that employed cross-sectional methodologies, which cannot not capture growth in patients over time. The assumption that clavicle length at each stage is uniform, as is the final overall length, may not be accurate if the age groups studied comprise various ethnicities, socioeconomic status, or height.
Questions/Purposes
We sought to quantify longitudinal clavicular growth on serial radiographs in adolescents and young adults. Our hypothesis was that substantial clavicular growth would be seen beyond the age of 12 years.
Methods
We conducted a longitudinal case series of non-syndromic patients in a single orthopedic clinic and analyzed serial radiographic images of the clavicles. For ethical reasons, only patients with non-neuromuscular scoliosis and kyphosis (in whom the existing standard of care includes serial thoracic radiographs) were considered for inclusion. Patients ages 10 to 25 years old were included in the study if three or more serial thoracic radiographs over a minimum 5 years were available that captured the entire length of at least one non-rotated clavicle. Three types of radiographs were included for analysis: digital low-dose-radiation stereoradiographic (EOS Imaging, Paris, France), non-EOS digital, and non-EOS printed. The overall longitudinal growth, yearly growth, and the yearly growth percentage were calculated for each clavicle.
Results
Fifty-seven patients (22 male and 35 female) met the inclusion criteria. In male patients, at ages 12 to 15 years, the clavicular growth was 4.9 mm/year, or 4%/year; at ages 16 to 19 years, growth was 3.2 mm/year, or 2.4%/year; and at ages 20 to 25 years, growth was 1.7 mm/year, or 1.1%/year. In female patients, at ages 12 to 15 years, growth was 4.7 mm/year, or 4%/year; at 16 to 19 years, growth was 2.2 mm/year, or 1.7%/year; and at ages 20 to 25 years, growth was 0.2 mm/year or 0.1%/year. We could not detect the age of terminal growth in either sex because growth was ongoing in most patients in the oldest group.
Conclusion
We found substantial clavicular growth potential after age 18 years, when growth is thought to be nearly finished, as well as remodeling potential even up to age 25 years. Further research is needed, but our findings suggest that strategies for managing clavicle fracture in adults may not be applied universally to adolescents and young adults.
Electronic supplementary material
The online version of this article (10.1007/s11420-020-09754-8) contains supplementary material, which is available to authorized users.
Keywords: clavicle, adolescents, fracture, trauma, remodeling
Introduction
Amid renewed interest in the management of displaced clavicle fractures [8, 19, 20, 23], there has been a remarkable increase in the rate of operative fixation of adolescent clavicle fractures, a logical follow-up to improvements in operative outcomes in adults [4]. This interest is also due in part to cadaveric studies suggesting abnormal biomechanical stress across the shoulder girdle secondary to clavicular deformity [11], as well as reports of high rates of patient satisfaction and functional outcomes after operative fixation that have appeared in the adult and adolescent literature [13, 14, 20]. These findings are further supported by a 2009 study by McGraw et al. suggesting limited clavicular growth and remodeling potential in male patients over the age of 12 years and in female patients over the age of 9 years [12].
McGraw et al. provide the most comprehensive study to date on clavicular growth [12], although several surgeon–investigators have observed significant fracture remodeling even in older adolescents, perhaps a result of greater clavicular growth in such patients than had previously been reported [17]. Furthermore, it is estimated that 80% of the longitudinal growth of the clavicle occurs from the medial physis [16, 24] and that the medial epiphysis does not complete ossification until about 20 years of age and does not fully fuse until 23 to 25 years of age [9, 16, 18]. Given that the upper age limit in the analysis by McGraw et al. was 18 years, it is possible that the full remodeling potential of the clavicle has not yet been appreciated. Another limitation of existing literature results is that clavicular growth has been assessed using cross-sectional methodology [3, 12]. Conclusions from these studies are based on the mean clavicle length in each age group separately and not over time, which has led to an assumption that the clavicle length at each stage is uniform, as is the final, overall length. Such assumptions may not be accurate if the age groups comprise patients of different ethnicities, socioeconomic status, or height.
In light of the limitations of cross-sectional analysis, the use of imaging—specifically, serial radiography—to follow an individual from adolescence until physeal closure is likely a more accurate means of measuring clavicular growth.
The purpose of this study was to fill in this gap in the literature in an ethically sound manner. A study of patients in whom serial radiation exposure is not clinically indicated would be difficult to justify. To that end, we performed longitudinal evaluation of clavicular growth in patients with non-neuromuscular scoliosis and kyphosis—patients, in other words, in whom the existing standard of care includes serial thoracic radiographs. We hypothesized that substantial clavicular growth would be observed beyond the age of 12 years.
Methods
After we obtained institutional review board approval, we performed a retrospective review of data collected from an adolescent idiopathic scoliosis (AIS) registry and all male patients who had undergone surgical correction for Scheuermann’s kyphosis at a single institution from the ages of 10 to 25 years. For patients to be included, serial thoracic spinal radiographs covering an interval of at least 5 years had to be available. Demographic and clinical data were extracted from the database, including sex, date of birth, height, and underlying diagnosis. We collected additional information from the radiographs, including the date of radiograph, the Risser stage, and whether the triradiate cartilage was open or closed.
Patients with underlying neuromuscular syndromes or a prior clavicle fracture were excluded. Patients were also excluded if there were not at least three radiographs available that captured the entire length of at least one clavicle over a minimum 5 years. Patients with spinal instrumentation obscuring the medial end of the clavicle were also excluded; consistently, such cases involved posterior spinal fusions with instrumentation above the T5 level because the implants often obscured the sternoclavicular joint, making accurate and reproducible radiographic measurements of length a challenge. Patients were also excluded if their radiographs showed malrotation or a change in rotation if the ratio of the distance (in millimeters) from the right T4 pedicle to the tip of the T4 spinous process to the distance from the left T4 pedicle to the tip of the T4 spinous process was not consistent throughout all radiographs (Fig. 1).
Fig. 1.
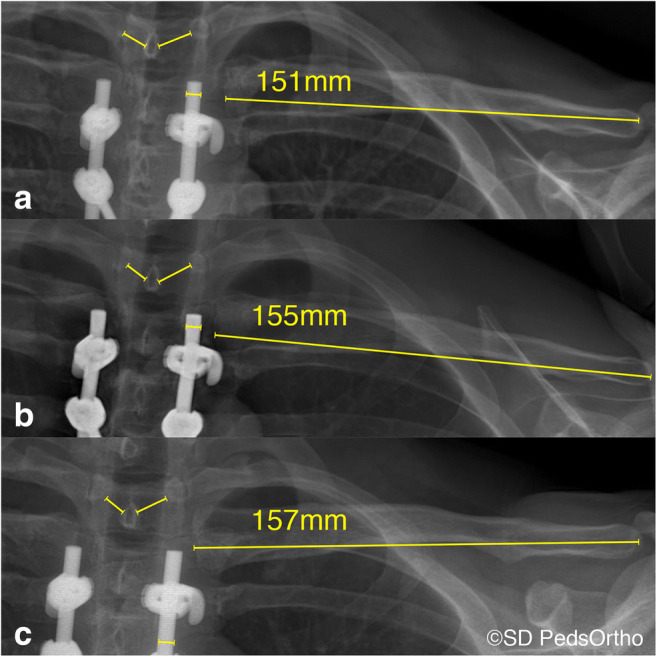
X-ray measurement technique. a Twenty-one-year-old male patient with a normalized clavicle length of 151 mm. b The same male patient at 24 years of age with a normalized length of 155 mm. c The same male patient at age 25 with a normalized length of 157 mm. To ensure consistent rotation, the distance between the right pedicle to the tip of the spinous process was compared to the distance of the left pedicle to the tip of the spinous process in each radiograph. In addition, all clavicle measurements were normalized for potential magnification using the rod diameter.
Radiographs were performed using upright biplanar slot scanning technology, which calibrates automatically and is not subject to magnification error [15]. Radiographic measurements were performed on all available scoliosis films in the patient’s chart. Images were measured in random order, and the researcher recording measurements was blinded to the patients’ height and Risser and triradiate cartilage status (open versus closed) in order to minimize measurement bias. Clavicle length measurements were performed by one author (J.L.H.) on two different occasions, as well as by another author (A.T.P.). The intra-class correlation coefficient was used to assess both inter- and intra-observer reliability [5]. Clavicular length was measured using the digital caliper tool on the Amicas picture archiving and communication system (PACS) (Chicago, IL, USA) to the nearest tenth of a millimeter. When patients had images from both clavicles available, the clavicle with the greatest number of serial measurements was used for analysis. The laterality of the clavicle was kept consistent; in other words, the same clavicle was used for all measurements (for example, the right clavicle at age 12 years was compared to the right clavicle at age 14 years, not left clavicle at age 14 years).
During the study period, the majority of the scoliosis films were obtained with a digital low-dose-radiation stereoradiography system (EOS Imaging, Paris, France). The EOS technology generates true-to-size images—direct measurements, in other words—unlike conventional radiography, which requires a specified distance from the X-ray beam to minimize magnification of the image [6, 15]. A minority of scoliosis films were obtained using conventional radiography. To normalize the magnification in those cases, the rod diameter, which was documented in the operative report, was used to calibrate the measurement of the clavicle length.
In situations in which no instrumentation was present, one of two calculated magnification factors was used. For digitally produced radiographs, 20 non-EOS digital radiographs with hardware were randomly selected. The rod in each film was measured, and the average of those measurements was used to designate the magnification factor. For conventional, film-based radiographs that had been scanned into the PACS, 20 clavicle films with hardware and one uploaded printed radiograph that had the hardware were randomly selected. Again, the 20 rod measurements were then averaged to designate a magnification factor.
After normalization of all clavicle measurements, the measurements were organized into three groups according to age at the time of image acquisition: group 1, 12 to 15 years; group 2, 16 to 19 years; and group 3, 20 to 25 years. To calculate the clavicular growth difference within each group, the difference between the “oldest” (latest) clavicular measurement and the “youngest” (earliest) clavicular measurement within the designated age group was calculated for each patient. To determine the rate of growth per year in the respective groups, the calculated growth was divided by the number of years between the ages of the two measurements. For example, if the age 12 clavicle measured 120 mm and the age 15 clavicle measured 150 mm, the calculation would be (150–120) / 3 or 10 mm/year. Thus, predicted length at age 14 years = 120 + 10 + 10 = 140 mm. The percentage of clavicular growth was relative to the youngest measurement used in the age group. For example, 10 mm/year growth difference from clavicle that measured 120 mm at age 12 would be calculated as (10 / 120) × 100 = 8.33%/year. Because these calculations were made for individual patients, the mean plus or minus the standard deviation for each age and age group was then generated for male and female subjects separately.
Results
Fifty-seven patients (22 male, 35 female) met the inclusion criteria. Nineteen female patients and four male patients had bilateral clavicles available. After applying the random string generated to determine which clavicle was to be included, the distribution of right and left clavicles was 19 and 16 for female patients, respectively, and 20 and 2 for male patients, respectively. The earliest data points captured in both male and female patients were from patients 11 years old and the latest data points were captured from both male and female patients 25 years old (Table 1).
Table 1.
Longitudinal adolescent clavicular growth
| 12–15 years Female | 12–15 years Male | 16–19 years Female | 16–19 years Male | ≥ 20 years Female | ≥ 20 years Male | |
|---|---|---|---|---|---|---|
| No. of clavicles (R + L) | 16 | 11 | 25 | 11 | 6 | 5 |
| Mean growth (mm/year)a | 4.7 ± 1.9 | 4.9 ± 2.1 | 2.2 ± 1.8 | 3.2 ± 0.9 | 0.2 ± 1.0 | 1.7 ± 1.0 |
| Mean growth (%/year)b | 4.0 ± 1.7% | 4.0 ± 1.7% | 1.7 ± 1.4% | 2.4 ± 0.7% | 0.1 ± 0.4% | 1.1 ± 0.7% |
aGrowth per year measured as the difference between the oldest clavicular measurement and the youngest clavicular measurement within the designated age groups divided by the number of years between the two ages of the measurement. (Example: age 12 clavicle measured 120 mm and age 15 measured 150 mm: (150–120) / 3 = 10 mm/year)
bPercentage of growth per year of the clavicle relative to the youngest measurement used in the age group. (Example: 10 mm/year growth difference from clavicle 12 year that measured 120: (10/120) × 100 = 8.3%/year) All measurements were normalized based on radiograph type.
Inter-observer reliability for the randomly selected 20 clavicles was 0.99 for the right clavicle and 1.0 for the left clavicle. The intra-observer reliability was 0.98 for the right clavicle and 0.99 for the left clavicle, denoting nearly perfect inter- and intra-observer reliability. The magnification factor for non-EOS digital radiographs was calculated to be 1.07 and for non-EOS-printed radiographs was 1.16. A total of 324 clavicle measurements were made, of which 252 (78%) were made directly from the EOS images, 54 (17%) were made using the known implant sizes as a measurement aid, and 18 (5%) were made using the magnification-correction factor.
Male Patients
In male patients, from ages 12 through 15 years, the mean growth was 4.9 ± 2.1 mm/year. The average percentage growth in the 12- to 15-year age group was 4.0 ± 1.7%/year. From the ages of 16 through 19 years, clavicle grown in male patients was 3.2 ± 0.9 mm/year, with a percentage growth per of 2.4 ± 0.7%/year. Finally, male patients ages 20 to 25 years had clavicular growth of 1.7 ± 1 mm/year and a percentage growth of 1.1 ± 0.7%/year (Table 1; Figs. 2, 3, and 4) Interestingly, in the available clavicles in the 20- to 25-year age group, there was still some measurable growth even at 25 years of age (Fig. 2). In male subjects, the average clavicle length at age 12 was 129 mm; at age 16 years, it was 136 mm; and at age 20 years, it was 144 mm.
Fig. 2.
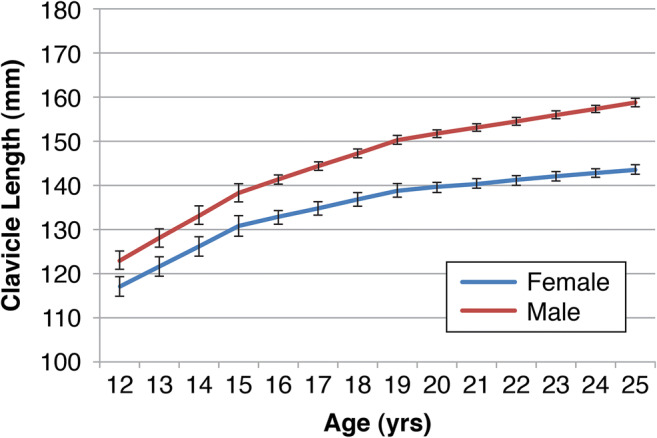
Estimated clavicular growth after age 12. All measurements were normalized as necessary according to radiograph type (digital low-dose-radiation stereoradiographic [EOS], non-EOS digital, or non-EOS printed).
Fig. 3.
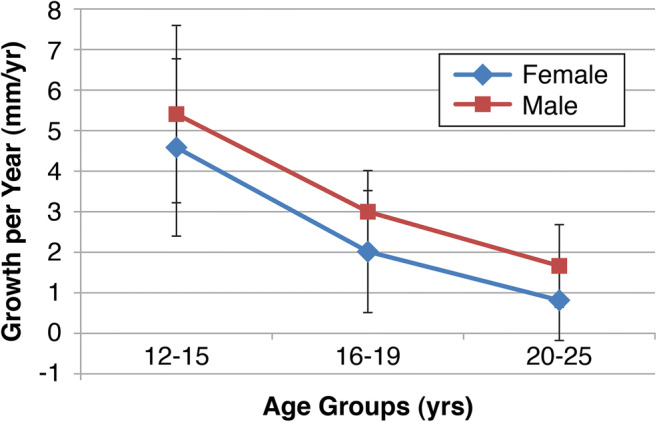
Calculated clavicular annular growth rate. Values are reported in millimeters per year.
Fig. 4.
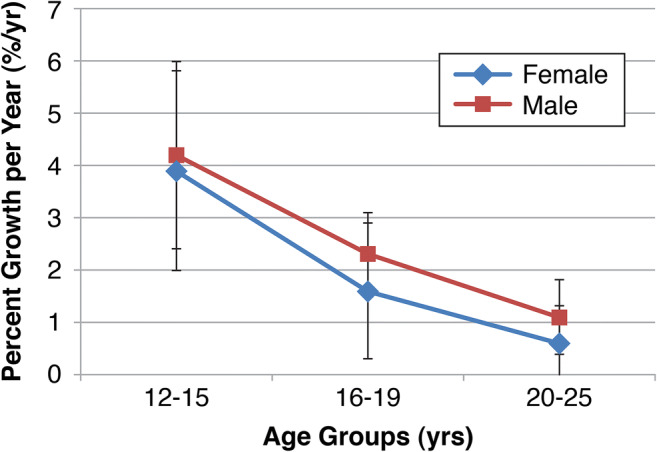
Percentage growth per year, as measured relative to the youngest measurement taken in each age group. Values are reported as a percentage of clavicular length change per year. All measurements were normalized according to radiograph type (digital low-dose-radiation stereoradiographic [EOS], non-EOS digital, or non-EOS printed).
Female Patients
In female patients, from ages 12 through 15 years, the mean clavicular growth was 4.7 ± 1.9 mm/year, with a percentage growth of 4 ± 1.7%/year. From the ages of 16 through 19 years, female subjects’ clavicles grew 2.2 ± 1.8 mm/year, with a percentage growth per of 1.7 ± 1.4%/year. Finally, female patients ages 20 to 25 years old had a clavicular growth of 0.2 ± 0.5 mm/year, or a percentage growth of 0.1 ± 0.4%/year (Table 1; Figs. 2, 3, and 4). In female patients, the average clavicle length at age 12 was 117 mm; at age 16 years, it was 129 mm; and at age 20 years, it was 135 mm.
Discussion
This study demonstrates that the clavicle grows considerably after the age of 12 years in both sexes. In male subjects, the mean growth from age 12 to age 25 years was as much as 34%, accounting for roughly 45 mm of longitudinal growth. In female subjects, from ages 12 to 25 years, there was roughly 33 mm of longitudinal growth and as much as 26% growth. These findings suggest that the open medial clavicular physis allows for substantial longitudinal growth late into adolescence and early adulthood, particularly in male patients.
Our study has limitations. One is that we were unable to have sequential radiographs of the patients at every age. This was a retrospective review of a scoliosis database (the AIS), and the number and timing of the radiographs was based on the institution’s standard post-operative protocol after scoliosis surgery. Second, it is unclear whether the clavicular growth seen in scoliosis patients can be generalized to the greater adolescent population. There was a limited number of male patients within the AIS and kyphosis databases, which has the potential to limit generalizability. Regarding the imaging modalities, we used multiple methods, including EOS, digital radiographs, and film radiographs. Although we normalized for magnification, there is variability in the imaging format. Another limitation is that the clavicle is a three-dimensional S-shaped bone and the current study measured only the medial-to-lateral length of clavicle. Therefore, any growth that occurred in the other dimensions during development was not accounted for. However, the measurement we used remains clinically relevant because shortening between the sternoclavicular and acromioclavicular joints in the frontal plane has been shown to predict functional outcomes after both operative and non-operative treatment. Finally, because of the limited number of subjects, we used 4-year age-group intervals, making it difficult to pinpoint the timing of growth spurts or declines. We acknowledge that there would be some measurement error, particularly in the older female patients with less than a millimeter of average growth per year. As our scoliosis database grows, re-evaluation using larger sample sizes will further elucidate clavicular growth patterns.
Our data suggest there is more growth potential during adolescence than reported by McGraw et al., whose data suggested only 20% of total clavicular growth remaining between the ages of 9 and 18 years in female patients and 12 and 18 years in male patients [12]. In addition, of the 961 radiographs measured by McGraw et al., only 94 were measured twice, only 12 were measured three times, three were measured four times, and two were measured five times [12]. We found that, from ages 12 through 18 years, there was an estimated 24% clavicular growth in male subjects and 20% clavicular growth in female subjects, in contrast to the 20% after age 9 found by McGraw et al. It should be noted that our study had shorter mean clavicular lengths in both male and female subjects, which could have contributed to the discrepancy in the growth percentages. However, McGraw et al. used standard anteroposterior chest radiographs that have inherent magnification. The current study normalized for magnification using EOS images and known implant dimensions. Our methodology is a more accurate predictor of adolescent growth potential because measurements were normalized for radiographic magnification error and were made using sequential measurements of each clavicle.
Our study is unique in that it demonstrates continued longitudinal clavicular growth beyond 18 years of age in both sexes. There was as much as 10% more growth after the age of 18 years in male subjects and as much as 6% in female subjects. Previous literature has reported that in a normal clavicle, 80% of longitudinal growth occurs from the medial physis [16, 24] and that the medial physis does not fuse until 23 to 25 years of age [9, 16, 18]. An open physis and the fact that the physis contributes substantially to fracture remodeling in other long bones suggest that even after 18 years of age, there is still remodeling potential for clavicle fractures [1, 21, 22]. Remodeling of a healed fracture depends on the child’s growth potential at the time of the fracture, the periosteum, and the location of the fracture relative to the open physis, as well as whether the fracture is in the plane of the physis. The remodeling potential required to minimize symptomatic malunion after clavicle fracture is unknown and will need to be studied further. From our original patient pool, we identified a patient who had experienced a clavicle fracture at the age of 17 (Fig. 5). He was, therefore, not included in our final study population, but as the figure illustrates, he had remarkable remodeling of his fracture into young adulthood.
Fig. 5.
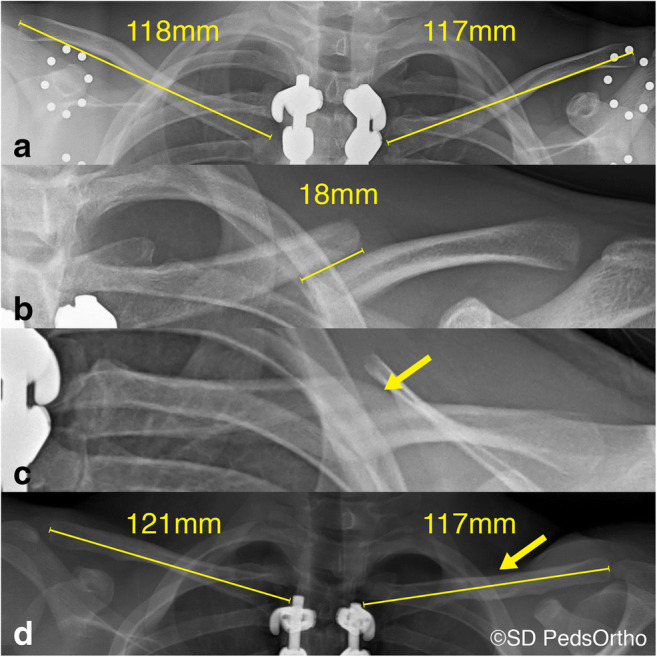
X-ray images illustrating remodeling potential in an older adolescent. The patient was 17 years old and male and had undergone fusion and instrumentation for adolescent idiopathic scoliosis (because of which he was excluded from the study pool). a At age 17, before his clavicle fracture, his right clavicle had a normalized length of 118 mm and his left clavicle had a normalized length of 117 mm. Five months later, he sustained a midshaft right clavicle fracture (b) that was treated non-operatively (c). Images c, d demonstrate the remodeling of the fracture at 6 months and 1 year after treatment. At age 18.5 years, the patient’s left clavicle had a normalized length of 117 mm and his right clavicle had a normalized length of 121 mm.
Clinically, non-operatively treated displaced midshaft clavicle fractures in adolescents are associated with fewer functional deficits than those in adults [2, 7, 10, 17]. The continuing growth and remodeling potential may help explain some of these discrepancies [4, 17]. Also, given the further growth seen in this study, different surgical criteria likely need to be applied to this younger patient population. Future studies will, it is hoped, clarify these surgical indications.
In conclusion, our findings suggest that there is continued longitudinal growth of the clavicle during adolescence and even as late as age 25. Although it is unclear how this should affect surgical decision making, more research is required to determine the clavicular physeal contribution to fracture remodeling, particularly in regard to fracture location (midshaft versus proximal or distal) and shortening. Our study suggests that current clavicle fracture management strategies for adults cannot be applied universally to adolescents and young adults.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1225 kb)
(PDF 1225 kb)
(PDF 1225 kb)
Funding Information
This study was supported by Rady Children’s Hospital, San Diego, Division of Orthopedics.
Compliance with Ethical Standards
Conflict of Interest
Tracey Bastrom, MS, declares no conflicts of interest. Jessica L. Hughes, MD, reports personal fees or other material support from Depuy Synthes, Medical Device Business Services, Axogen, Stryker, Globus Medical, and Sanofi-Aventis, outside the submitted work. Peter O. Newton, MD, reports personal fees or other material support from Nuvasive, Zimmer Biomet, K2M, Medtronic USA, Merck Sharp & Dohme Corp., Globus Medical, Ethicon, and Depuy Synthes, outside the submitted work. Peter D. Fabricant, MD, MPH, reports personal fees or other material or nonfinancial support from Smith & Nephew, Medical Device Business Services, and Arthrex, and personal fees and board membership from Clinical Orthopedics and Related Research, Pediatric Orthopedic Society of North America, Pediatric Research in Sports Medicine Society, and Research in OsteoChondritis of the Knee (ROCK), outside the submitted work. Andrew T. Pennock, MD, reports personal fees or other material support from Stryker, Sportstek Medical, Orthopediatrics, Smith & Nephew; personal fees and board membership from American Orthopedic Society for Sports Medicine and Pediatric Orthopedic Society of North America; and stock or stock options from Imagen, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was obtained from all patients for being included in this study.
Required Author Forms:
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV: Retrospective case series
References
- 1.Abraham E. Remodeling potential of long bones following angular osteotomies. J Pediatr Orthop. 1989;9(1):37–43. [DOI] [PubMed]
- 2.Bae DS, Shah AS, Kalish LA, Kwon JY, Waters PM. Shoulder motion, strength, and functional outcomes in children with established malunion of the clavicle. J Pediatr Orthop. 2013;33(5):544–550. [DOI] [PubMed]
- 3.Black S, Scheuer L. Age changes in the clavicle: from the early neonatal period to skeletal maturity. Int J Osteoarchaeol. 1996;6(5):425–434.
- 4.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89(1):1–10. [DOI] [PubMed]
- 5.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284.
- 6.Glaser DA, Doan J, Newton PO. Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine (Phila Pa 1976). 2012;37(16):1391–1397. [DOI] [PubMed]
- 7.Heyworth BE, Kocher MS. Shoulder instability in the young athlete. Instr Course Lect. 2013;62:435–444. [PubMed]
- 8.Heyworth B, Suppan C, Kocher M. Change in the volume of operative treatment of clavicle fractures in children and adolescents: national trends and practice patterns. American Orthopaedic Society for Sports Medicine; 2014.
- 9.Jit I, Kulkarni M. Times of appearance and fusion of epiphysis at the medial end of the clavicle. Indian J Med Res. 1976;64(5):773–782. [PubMed]
- 10.Li Y, Donohue KS, Robbins CB, et al. Reliability of radiographic assessments of adolescent midshaft clavicle fractures by the FACTS Multicenter Study Group. J Orthop Trauma. 2017;31(9):479–484. [DOI] [PubMed]
- 11.Matsumura N, Ikegami H, Nakamichi N, et al. Effect of shortening deformity of the clavicle on scapular kinematics: a cadaveric study. Am J Sports Med. 2010;38(5):1000–1006. [DOI] [PubMed]
- 12.McGraw MA, Mehlman CT, Lindsell CJ, Kirby CL. Postnatal growth of the clavicle: birth to 18 years of age. J Pediatr Orthop. 2009;29(8):937–943. [DOI] [PMC free article] [PubMed]
- 13.McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94(8):675–684. [DOI] [PubMed]
- 14.Mehlman CT, Yihua G, Bochang C, Zhigang W. Operative treatment of completely displaced clavicle shaft fractures in children. J Pediatr Orthop. 2009;29(8):851–855. [DOI] [PubMed]
- 15.Melhem E, Assi A, El Rachkidi R, Ghanem I. EOS® biplanar X-ray imaging: concept, developments, benefits, and limitations. J Child Orthop. 2016;10(1):1–14. [DOI] [PMC free article] [PubMed]
- 16.Pandya NK, Namdari S, Hosalkar HS. Displaced clavicle fractures in adolescents: facts, controversies, and current trends. J Am Acad Orthop Surg. 2012;20(8):498–505. [DOI] [PubMed]
- 17.Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg. Am. 2013;95(13):1159–1165. [DOI] [PubMed]
- 18.Shah RR, Kinder J, Peelman J, Moen TC, Sarwark J. Pediatric clavicle and acromioclavicular injuries. J Pediatr Orthop. 2010;30:S69–S72.
- 19.Suppan CA, Bae DS, Donohue KS, Miller PE, Kocher MS, Heyworth BE. Trends in the volume of operative treatment of midshaft clavicle fractures in children and adolescents: a retrospective, 12-year, single-institution analysis. J Pediatr Orthop. B. 2016;25(4):305–309. [DOI] [PubMed]
- 20.Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30(4):307–312. [DOI] [PubMed]
- 21.Wallace ME, Hoffman EB. Remodelling of angular deformity after femoral shaft fractures in children. J. Bone Joint Surg. Br. 1992;74(5):765–769. [DOI] [PubMed]
- 22.Wilkins KE. Principles of fracture remodeling in children. Injury. 2005;36(Suppl 1):A3–A11. doi: 10.1016/j.injury.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Yang S, Werner BC, Gwathmey FW Jr. Treatment trends in adolescent clavicle fractures. J Pediatr Orthop. 2015;35(3):229–233. [DOI] [PubMed]
- 24.Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD, Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19(7):504–507. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1225 kb)
(PDF 1225 kb)
(PDF 1225 kb)


