Abstract
Background
The optimal method for the determination of ankle stability remains controversial in rotational ankle fractures without medial bony injury.
Questions/Purposes
The purposes of this study were to (1) evaluate whether posterior malleolar (PM) fracture displacement is associated with deltoid ligament injury in supination-external rotation (SER) ankle fractures and (2) compare the diagnostic accuracy of PM displacement and magnetic resonance imaging (MRI) evaluation of the deep deltoid ligament in identifying fractures with deltoid ligament incompetence.
Methods
Patients with rotational bimalleolar injuries containing lateral malleolar and PM fractures without bony medial injury were included. After operative lateral and PM fixation, an external rotation stress test was performed to evaluate deltoid ligament stability. Operative dictations were reviewed to confirm injury pattern, stability on stress test, and visual inspection of the deltoid ligament. Maximum PM displacement was assessed on lateral X-ray. Pre-operative MRI of the ankle was performed following closed reduction and splinting.
Results
The final cohort consisted of 13 trimalleolar equivalent fractures (torn deltoid ligament) and 20 bimalleolar fractures (medial malleolus and deltoid ligament intact). Average PM displacement was significantly higher for SER trimalleolar equivalent patterns when measured on lateral X-ray. The sensitivity of detecting trimalleolar equivalent fracture was higher on all reported X-ray findings than the sensitivity obtained by the reported MRI findings of deltoid ligament injury.
Conclusion
PM displacement on X-ray is a useful adjuvant along with external rotation stress radiography and MRI evaluation of deep deltoid integrity to distinguish between stable and unstable fracture patterns and thus helps facilitate treatment decisions.
Electronic supplementary material
The online version of this article (10.1007/s11420-019-09697-9) contains supplementary material, which is available to authorized users.
Keywords: supination-external rotation, posterior malleolus, deltoid ligament, ankle stability, external rotation stress test, medial clear space
Introduction
Rotational ankle fractures (Orthopaedic Trauma Association [OTA] classification 44) represent the majority of ankle fractures [1]. Acceptable treatment results have been demonstrated with non-operative approaches for stable fractures (isolated lateral malleolar or supination-external rotation [SER] type II); however, unstable fractures (classically bimalleolar or SER type IV fractures) have been shown to benefit significantly from operative treatment [2]. The rates of radiographic post-traumatic arthritis with non-operative fracture care is 3% in stable fractures (18-year follow-up) compared with 66% in unstable patterns (mean, 6.8-year follow-up) [3]. While trimalleolar fractures and fracture dislocations are unequivocally characterized as unstable, the optimal method for the determination of ankle stability remains controversial in trimalleolar equivalent fracture patterns. Furthermore, studies evaluating ankle stability often exclude fractures involving the posterior malleolus. While some view all bimalleolar fractures involving the lateral and posterior malleolus as unstable, another approach is to evaluate both the extent of posterior malleolar displacement and the extent of medial ligamentous injury in these cases to determine operative versus non-operative management.
Anatomical studies have demonstrated the key role of the deep deltoid ligament complex in resisting pathologic lateral translation, external rotation, and valgus of the talus [4, 5]. Specifically, the deep deltoid ligament, which is comprised of anterior and posterior components, is the most important static stabilizer of the medial ankle [6, 7]. Several methods of evaluating the competency of the deltoid ligament in rotational ankle fractures have been studied including clinical signs, stress radiography, and magnetic resonance imaging (MRI). Clinical signs of medial injury such as medial swelling, tenderness, and ecchymosis are widely acknowledged to be unreliable indicators of deltoid ligament injury [8–10]. The most commonly used methods of determining deep deltoid incompetence have been manual external rotation and gravity stress radiographs, using the measurement of the medial clear space to identify lateralization of the talus. However, radiographic threshold criteria for instability have been debated. A recent cadaveric study demonstrated poor accuracy of radiographic medial clear space measurements (MCS) [11], and there is no clear relationship between absolute MCS measurements and MRI findings of complete deep deltoid ligament tears [12]. Furthermore, the available alternative imaging modality of MRI is expensive; some have argued that its utility in routine operative decision-making for rotational ankle fractures is not justified [13].
The majority of studies evaluating the discriminatory ability of radiographic and MRI findings in diagnosing ankle fracture instability have focused on distinguishing between isolated lateral malleolus fractures and bimalleolar equivalent injuries (lateral malleolus fracture with medial ligamentous injury). However, the diagnostic dilemma also applies to the diagnosis of trimalleolar equivalent fracture patterns. In rotational ankle fractures involving both the lateral and posterior malleoli, the inherent pitfalls of measuring medial clear space widening are also present. Alternative criteria to accurately judge fracture stability using currently available imaging modalities would be of value. Using a gold standard of intra-operative ligament assessment, this study evaluates a subgroup of rotational ankle fractures without medial bony injury to determine the utility of posterior malleolar (PM) fracture displacement in identifying fractures with complete deltoid ligament tears. The purpose is twofold: (1) to evaluate whether PM fracture displacement is associated with deltoid ligament injury and (2) to compare the diagnostic accuracy of PM displacement and MRI evaluation of the deep deltoid ligament in identifying trimalleolar equivalent fractures.
Methods
We conducted a retrospective review of patients identified from a single-surgeon database of operatively treated ankle fractures between 2008 and 2016. Patients with external rotation type ankle fractures involving a lateral and posterior malleolar fracture without medial bony injury were eligible for inclusion. Additional inclusion criteria were the availability of presenting radiographs (prior to fracture reduction), pre-operative MRI of the injured ankle, and documented intra-operative assessment of the deltoid ligament. Pre-operative imaging was reviewed to confirm the fracture pattern and associated malleolar injuries. Operative dictations from the attending surgeon were reviewed to document the results of manual stress testing after stabilization of the lateral malleolus, posterior malleolus, and syndesmosis, as well as direct visual assessment of the deltoid ligament in cases with positive stress examinations.
The operative indication for this cohort was the bimalleolar nature of the fracture pattern. The operative strategy was the same for all fractures and included a posterolateral approach to the ankle for the reduction and fixation of both the lateral and posterior malleoli. The reduction and fixation of the lateral malleolus were first achieved using mini fragment plates. The posterior malleolus was visualized through the same posterolateral approach, and reduction of the posterior cortical apex was directly visualized. Fixation of the posterior malleolus was performed with mini fragment buttress plating when fracture pattern allowed or with a single posterior to anterior small fragment screw through a spiked soft tissue washer for smaller fragments. This anatomic-specific approach of posterior malleolus fixation re-tensions the posterior-inferior tibiofibular ligament, providing syndesmotic stabilization [14, 15].
After the lateral and posterior malleolar fixation, fluoroscopic assessment of a manual external rotation stress test was performed. If medial clear space and talar tilt remained unchanged from the non-stress mortise view, the fixation was considered adequate and the deltoid ligament was deemed competent. If the external rotation stress evaluation revealed an increase in medial clear space or evidence of talar tilt, this indicated deltoid ligament insufficiency. Per the surgeon’s treatment algorithm, in the setting of a positive stress examination, the deltoid ligament was approached for visualization and repair. The results of this deltoid ligament inspection as documented in the intra-operative dictation were described as “torn,” “attenuated,” or “partially torn.” This was the gold standard used to determine the final assessment of deltoid ligament competence. Visually torn ligaments were repaired using a 5.0 Mitek suture anchor, as described previously [14]. These cases were deemed trimalleolar equivalent fractures. Attenuated or partially torn ligaments were imbricated using the same suture anchor technique but due to lack of frank tearing were classified as having deltoid competence.
Pre-operative injury radiographs were reviewed quantitatively by two independent observers. Maximum posterior malleolus displacement was assessed on lateral X-ray by judging cortical displacement. All pre-operative MRIs were performed after reduction and splinting of the fracture. A 1.5 Tesla magnet (Signa Horizon LX, General Electric Medical Systems, Milwaukee, WI, USA) was used with an extremity coil, and all MRIs were evaluated by a fellowship-trained musculoskeletal radiologist at the time of imaging acquisition. Reports were reviewed for integrity of the deep deltoid ligament and were categorized as intact, partially torn (low-grade partial tear), or completely torn (high-grade or complete tear) in a manner consistent with prior studies [16].
Differences in patient demographics, fracture characteristics, and PM displacement between the two injury patterns were evaluated using χ2 and nonparametric Wilcoxon rank-sum tests, as appropriate. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for a variety of quantitative X-ray measurement thresholds, as well as MRI deep deltoid findings. Finally, receiver operating characteristic (ROC) curve analysis was performed using the quantitative measurements of PM displacement, and area under the curve (AUC) was calculated to identify whether PM displacement could accurately discriminate between fractures with deltoid competence and deltoid incompetence. An AUC of over 0.80 indicates discriminate ability based on accepted standards [17]. All statistical analyses were performed using SPSS version 22, using two-tailed p values of < 0.05 to indicate statistical significance.
Results
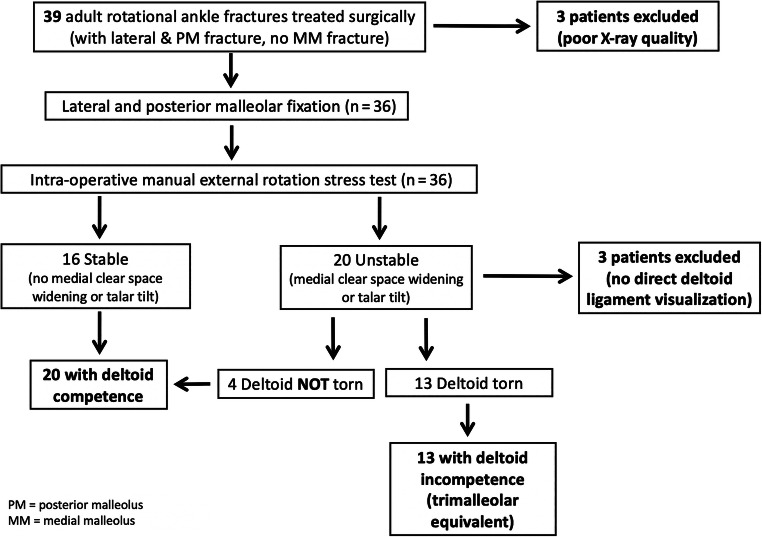
Thirty-nine patients with rotational ankle fractures including lateral malleolus and posterior malleolar fragments without medial bony injury were identified. Three patients were excluded for poor-quality lateral injury radiographs. Three additional patients were excluded due to lack of intra-operative visualization of the deltoid ligament after positive intra-operative stress examination (syndesmotic screw placement instead of deltoid ligament repair). Overall, 39.4% of the final cohort was female (n = 13). The mean age of this cohort was 47.8 ± 14.7 years, and mean body mass index (BMI) was 28.6 ± 6.5. The average percentage of the distal tibial plafond that involved the posterior malleolus fracture was 15.7 ± 4.8%. Posterior malleolar fixation was achieved with buttress plating in 81.8% (n = 27), and posterior to anterior screw fixation in 18.2% (n = 6). There was no difference in rate of open fractures, PM fracture size, or prevalence of posterior buttress plate fixation between injury patterns (Table 1). There was a statistically significant difference in the rate of dislocation on injury films (38.5% of trimalleolar equivalent fractures and 0% of lateral/posterior bimalleolar fractures, p = 0.005).
Table 1.
Demographic and fracture characteristics between injury patterns
| Deltoid competent (bimalleolar), n = 20 | Deltoid incompetent (trimalleolar equivalent), n = 13 | p value | |
|---|---|---|---|
| Age mean (SD) | 47.0 (14.4) | 48.9 (15.6) | 0.842 |
| BMI (kg/m2) mean (SD) | 29.6 (7.3) | 27.2 (5.2) | 0.518 |
| Female n (%) | 8 (40) | 5 (38.5) | 0.930 |
| PM area (% of plafond)a mean (SD) | 16.7 (5.4) | 14.1 (3.5) | 0.052 |
| PM buttress plate n (%) | 16 (80) | 11 (84.5) | 0.715 |
| Dislocated n (%) | 0 (0) | 5 (38.5) | 0.003 |
| Open fracture n (%) | 0 (0) | 1 (7.7) | 0.208 |
The italicized numbers in the p value column indicate statistical significance
aPercent of tibial plafond affected by posterior malleolar fracture
PM posterior malleolus, BMI body mass index
A flow diagram of group allocations is presented in Fig. 1. In the final cohort, after lateral and posterior fixation, the medial clear space and talus appeared unchanged from non-stress mortise X-rays in 16 of 33 (48.5%) patients (competent deltoid group). A positive stress examination warranted surgical approach to the deltoid ligament in the remaining 17 patients. In 13 of these patients (39.4% of the overall cohort, 76.5% of the group undergoing deltoid ligament exploration), the deltoid ligament was visibly torn and was repaired (trimalleolar equivalent group). In four of the cases with positive stress examinations (12.1% of the overall cohort, 23.5% of the cases with positive stress examination), all with mild talar tilt without overt medial clear space widening, direct visualization of the deltoid ligament revealed an attenuated ligament without insertional avulsion or intra-substance tearing. These were included in the group considered to have a competent deltoid ligament.
Fig. 1.
Flow diagram of injury classification and exclusions.
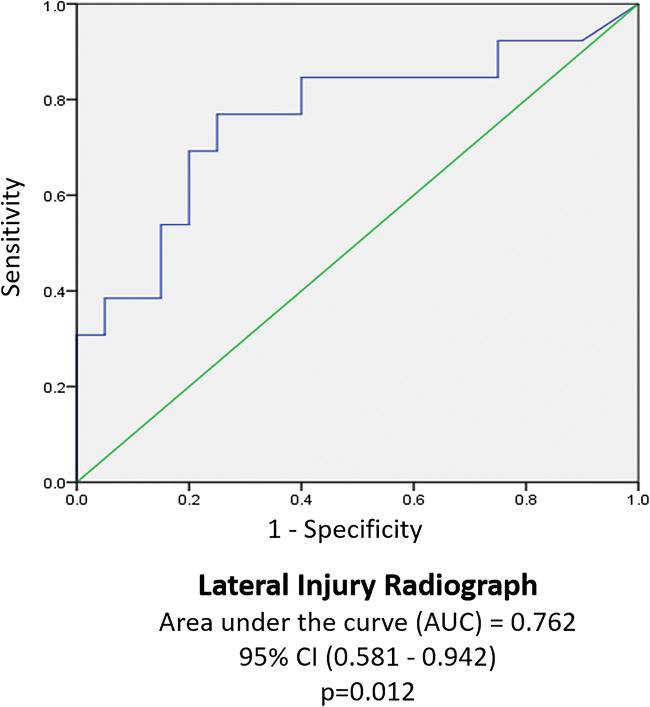
Mean PM displacement was significantly different between fracture patterns on lateral X-ray (Table 2). Injuries ultimately deemed to have a competent deltoid ligament demonstrated on average less than 2 mm of PM displacement, compared to over 2 mm for trimalleolar equivalent patterns. ROC curve analysis using quantitative posterior malleolus displacement on lateral X-ray revealed an area under the curve of 0.762 (Fig. 2).
Table 2.
Posterior malleolar displacement (in mm) by fracture pattern (mean of two observers)
| Deltoid competenta | Deltoid incompetent (trimalleolar equivalent)a | p value | ||
|---|---|---|---|---|
| Lateral x-ray | Mean | 1.53 | 4.85 | 0.012 |
| Median | 1.10 | 3.04 |
The italicized number in the p value column indicates statistical significance
aMeasurements recorded in millimeters (mean of two independent blinded observers)
Fig. 2.
The receiver operating characteristic (ROC) curve analysis of posterior malleolar displacement measurements.
MRI reports falsely indicated complete tearing of the deep deltoid ligament in 10% of fractures that were deemed to have deltoid competence (specificity 90%), and in 6.25% of cases in which the deltoid was not visualized due to a stable intra-operative stress examination. MRI accurately identified complete deltoid ligament tears in only 46.2% of fractures with directly visualized complete deltoid tearing (sensitivity 46%). Sensitivity, specificity, PPV, and NPV for each pre-determined predictor variable are outlined in Table 3. Sensitivity for detecting a trimalleolar equivalent fracture was maximized at 84.6% with a PM displacement of ≥ 1 mm on lateral radiographs. Specificity of PM displacement increased with increasing cutoffs (40% with PM displacement ≥ 1 mm and 70% with PM displacement ≥ 2 mm). Specificity was highest (90%) with MRI findings of a complete deep deltoid tear on MRI. Of note, the sensitivity of detecting a trimalleolar equivalent fracture was higher on all reported X-ray findings (quantitative cutoffs ≥ 1 mm, ≥ 1.5 mm, and ≥ 2 mm) than the sensitivity obtained by the reported MRI findings of deltoid injury (Table 3).
Table 3.
Sensitivity and specificity of posterior malleolus displacement and magnetic resonance imaging (MRI) deep deltoid findings in detecting trimalleolar equivalent injury patterns
| Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) | |
|---|---|---|---|---|
| Displacement on lateral X-ray | ||||
| ≥ 1 mm | 84.6 | 40.0 | 47.8 | 80.0 |
| ≥ 1.5 mm | 76.9 | 65.0 | 58.8 | 81.3 |
| ≥ 2 mm | 76.9 | 70.0 | 62.5 | 82.4 |
| Partial or complete deep deltoid tear on MRI | ||||
| Entire cohort (n = 33) | 69.2 | 70.0 | 60.0 | 77.8 |
| Subgroupa (n = 17) | 69.2 | 25.0 | 75.0 | 20.0 |
| Complete deep deltoid tear on MRI | ||||
| Entire cohort (n = 33) | 46.2 | 90.0 | 75.0 | 72.0 |
| Subgroup† (n = 17) | 46.2 | 75.0 | 85.7 | 30.0 |
aSubgroup of fractures undergoing direct deltoid ligament visualization
Discussion
In this study, rotational ankle fractures with a competent deltoid ligament demonstrated significantly less displacement of the PM fragment, on average, than trimalleolar equivalent fracture patterns (1.5 versus 4.8 mm, respectively). X-ray findings of a displaced posterior malleolus fracture were a more sensitive indicator of deltoid ligament tearing than MRI findings of deep deltoid ligament injury. The ability to accurately distinguish between rotational ankle fracture patterns with and without deltoid ligament competence by using pre-operative imaging has important clinical implications, as many surgeons elect to treat patterns with deltoid ligament competence non-operatively and those with deltoid ligament instability operatively. The treating surgeon for this cohort previously treated all bimalleolar (lateral and posterior) fracture patterns operatively before observing that the deltoid ligament is competent in a subset of cases. The deltoid ligament confers an additional level of stability to the ankle as a medial check-rein. It also provides indirect syndesmotic stability by preventing the talus from levering the fibula out of its anatomic position in the incisura during external rotation. Therefore, in the event of a minimally or non-displaced PM fracture that may ultimately heal and indirectly restore posterior-inferior tibiofibular ligament tension without operative reduction and fixation, the syndesmotic stability conferred by the deltoid ligament may become more clinically important as a mitigating factor.
This study has several limitations including its retrospective nature and small sample size. The variable quality of lateral injury radiographs for the assessment of posterior malleolus displacement decreased the precision of these assessments; however, given that these X-rays were obtained in the process of clinical care, they are typical of those obtained in many clinical settings and therefore speak to the generalizability of these results. The use of manual external rotation stress test intra-operatively to determine which fractures to pursue open deltoid ligament approach and repair is another limitation, with potential for variable force exerted on each examination and inherent inability to quantitatively measure medial clear space on these intra-operative assessments. However, a subgroup analysis of fractures that underwent direct deltoid visualization based on a positive intra-operative external rotation stress test revealed that pre-operative MRI had similar sensitivity and specificity of detecting a trimalleolar injury as compared with the entire cohort (Table 3). This supports the use of intra-operative stress examination as a defining feature in the fracture classification algorithm in this study.
Missed unstable ankle injuries can lead to late instability and post-traumatic arthritis. However, neither stress radiographs nor MRI are perfectly specific in identifying deltoid ligament rupture, and false-positive imaging findings (25% false-positive report of complete deltoid tear on MRI in this sample) may subject patients to potentially unnecessary surgery. As seen in this cohort, even an intra-operative assessment of deltoid ligament stability (after syndesmotic stability has been achieved with PM fixation) is not a perfect measure of identifying deltoid competence, with 20% (4 of 20) fractures with a competent deltoid ligament demonstrating evidence of talar tilt on stress examination. Isolated talar tilt has not been documented as an independent predictor of deltoid instability, as confirmed in this cohort.
The literature regarding the determination of ankle fracture stability contains studies with varying imaging modalities, measurement methodologies, and threshold cutoffs. There is no consensus on the degree of medial clear space widening that warrants surgical fixation, and recent reports have demonstrated that weight-bearing stress radiographs may yield a diagnosis of stability more often than gravity stress radiographs, with those treated non-operatively based on weight-bearing stress test results having good short-term results [18]. Stress radiographs with a threshold of 4 mm have demonstrated 73 to 92% sensitivity and 39 to 46% specificity in discriminating between stable (competent deltoid ligament) and unstable (torn deltoid ligament) injury patterns when MRI is the reference standard [9, 16]. Similarly, when compared with MRI results, an MCS threshold of 5 mm maximizes the combined sensitivity and specificity (66% and 77%, respectively); however, this threshold did not demonstrate discriminatory ability to identify deep deltoid ligament disruption on previous ROC curve analysis [16]. A study by Koval et al. found that only 10% of patients with an MCS of 5 mm or higher had a complete deltoid tear on MRI [12]. Using an operative criteria of complete deep deltoid rupture on MRI in patients with MCS of 5 mm or higher, these authors showed excellent patient-reported outcomes at 1-year follow-up, further calling into question the adequacy of MCS as a decision tool [12]. Furthermore, a study comparing MCS to a gold standard of arthroscopic visualization in rotational ankle fractures found 85.7% sensitivity and a 45% false-positive rate in identifying a complete rupture of the deep deltoid ligament for radiographic MCS widening over 5 mm [19].
While MRI has traditionally been the gold standard for comparison, MRI may not adequately estimate the incidence of complete deltoid tears, and few studies have compared the accuracy of MRI findings with intra-operative direct visual assessment. Crim et al. performed a retrospective analysis comparing MRI and arthroscopic or open surgical findings of the deltoid ligament in 74 ankles with acute and chronic pathologies. MRI detected 26 of 27 deltoid tears (sensitivity, 96.3%), and there was one false-positive MRI, in which the ligament was visualized as normal intra-operatively (specificity, 97.9%). However, Crim et al. included a variety of ankle pathologies, with only two trauma patients in the cohort. The results of the current study revealed a much lower sensitivity of MRI (42.6%) in identifying complete deep deltoid ruptures compared with open intra-operative visualization. The discrepancy may be due to the different patient populations in these two studies and a potential decrease in the ability of MRI to detect complete tearing in the presence of acute ankle trauma.
When compared with prior literature evaluating the sensitivity of MCS widening, X-ray evaluation of posterior malleolus displacement is more sensitive than the accepted cutoff of 5 mm (77 to 85% for PM displacement versus 66% for MCS of 5 mm or more); however, the difference in gold-standard references used in these evaluations leads to an imperfect comparison. Nonetheless, the presence of a significantly displaced PM fragment may indicate instability. Further research is necessary to validate this claim in other cohorts.
Despite its limitations, this study comprises a homogeneous subset of rotational ankle fractures treated with standardized imaging and intra-operative fixation protocols. Furthermore, it is one of the few to evaluate radiographic criteria against a gold standard of intra-operative visualization, and the first to our knowledge to compare MRI findings with intra-operative assessments of the deltoid ligament. In this study, PM displacement was associated with deltoid insufficiency (i.e., trimalleolar equivalent patterns), which can help determine which patients will benefit from surgical fixation. In conclusion, PM displacement on X-ray is a useful adjuvant to conventional methods of external rotation stress radiography and MRI evaluation of deep deltoid integrity to distinguish between stable and unstable rotational ankle fracture patterns and thus helps facilitate treatment decisions.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Funding
This publication was supported by National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (NIH) under award number T32 AR007281.
Compliance with Ethical Standards
Conflict of Interest
Ashley E. Levack, MD, MAS, Elizabeth B. Gausden, MD, MPH, and Aleksey Dvorzhinskiy, MD, declare that they have no conflicts of interest. David S. Wellman, MD, reports personal fees from Synthes, outside the submitted work. Dean G. Lorich, MD, reported personal fees from DePuy Synthes, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Level of Evidence: Level III: Diagnostic Study
Dean G. Lorich died on December 10, 2017.
References
- 1.Bradley AP. The use of the area under the ROC curve in the evaluation of machine learning algorithms. Pattern Recognition. 1997;30:1145–1159. doi: 10.1016/S0031-3203(96)00142-2. [DOI] [Google Scholar]
- 2.DeAngelis NA, Eskander MS, French BG. Does medial tenderness predict deep deltoid ligament incompetence in supination-external rotation type ankle fractures? J Orthop Trauma. 2007;21:244–247. doi: 10.1097/BOT.0b013e3180413835. [DOI] [PubMed] [Google Scholar]
- 3.Egol KA, Amirtharajah M, Tejwani NC, et al. Ankle stress test for predicting the need for surgical fixation of isolated fibular fractures. J Bone Joint Surg Am. 2004;86-A:2393–2398. doi: 10.2106/00004623-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Gougoulias N, Khanna A, Sakellariou A, et al. Supination-external rotation ankle fractures: stability a key issue. Clin Orthop Relat Res. 2010;468:243–251. doi: 10.1007/s11999-009-0988-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gougoulias N, Sakellariou A. When is a simple fracture of the lateral malleolus not so simple? How to assess stability, which ones to fix and the role of the deltoid ligament. Bone Joint J. 2017;99-B:851–855. doi: 10.1302/0301-620X.99B7.BJJ-2016-1087.R1. [DOI] [PubMed] [Google Scholar]
- 6.Koval KJ, Egol KA, Cheung Y, et al. Does a positive ankle stress test indicate the need for operative treatment after lateral malleolus fracture? A preliminary report. J Orthop Trauma. 2007;21:449–455. doi: 10.1097/BOT.0b013e31812eed25. [DOI] [PubMed] [Google Scholar]
- 7.Levack AE, Warner SJ, Gausden EB, et al. Comparing functional outcomes after injury-specific fixation of posterior malleolar fractures and equivalent ligamentous injuries in rotational ankle fractures. J Orthop Trauma. 2018;32:e123–e128. doi: 10.1097/BOT.0000000000001104. [DOI] [PubMed] [Google Scholar]
- 8.Little MM, Berkes MB, Schottel PC, et al. Anatomic fixation of supination external rotation type IV equivalent ankle fractures. J Orthop Trauma. 2015;29:250–255. doi: 10.1097/BOT.0000000000000318. [DOI] [PubMed] [Google Scholar]
- 9.Marsh J, Slongo T, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma. 2007;21:S1–S163. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 10.McConnell T, Creevy W, Tornetta P., 3rd Stress examination of supination external rotation-type fibular fractures. J Bone Joint Surg Am. 2004;86-A:2171–2178. doi: 10.2106/00004623-200410000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Metitiri O, Ghorbanhoseini M, Zurakowski D, et al. Accuracy and measurement error of the medial clear space of the ankle. Foot Ankle Int. 2017;38:443–451. doi: 10.1177/1071100716681140. [DOI] [PubMed] [Google Scholar]
- 12.Michelsen JD, Ahn UM, Helgemo SL. Motion of the ankle in a simulated supination-external rotation fracture model. J Bone Joint Surg Am. 1996;78:1024–1031. doi: 10.2106/00004623-199607000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Nortunen S, Lepojarvi S, Savola O, et al. Stability assessment of the ankle mortise in supination-external rotation-type ankle fractures: lack of additional diagnostic value of MRI. J Bone Joint Surg Am. 2014;96:1855–1862. doi: 10.2106/JBJS.M.01533. [DOI] [PubMed] [Google Scholar]
- 14.Savage-Elliott I, Murawski CD, Smyth NA, et al. The deltoid ligament: an in-depth review of anatomy, function, and treatment strategies. Knee Surg Sports Traumatol Arthrosc. 2013;21:1316–1327. doi: 10.1007/s00167-012-2159-3. [DOI] [PubMed] [Google Scholar]
- 15.Schottel PC, Fabricant PD, Berkes MB, et al. Manual stress ankle radiography has poor ability to predict deep deltoid ligament integrity in a supination external rotation fracture cohort. J Foot Ankle Surg. 2015;54:531–535. doi: 10.1053/j.jfas.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Schuberth JM, Collman DR, Rush SM, et al. Deltoid ligament integrity in lateral malleolar fractures: a comparative analysis of arthroscopic and radiographic assessments. J Foot Ankle Surg. 2004;43:20–29. doi: 10.1053/j.jfas.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Seidel A, Krause F, Weber M. Weightbearing vs gravity stress radiographs for stability evaluation of supination-external rotation fractures of the ankle. Foot Ankle Int. 2017;38:736–744. doi: 10.1177/1071100717702589. [DOI] [PubMed] [Google Scholar]
- 18.van den Bekerom MP, Mutsaerts EL, van Dijk CN. Evaluation of the integrity of the deltoid ligament in supination external rotation ankle fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2009;129:227–235. doi: 10.1007/s00402-008-0768-6. [DOI] [PubMed] [Google Scholar]
- 19.Yde J, Kristensen KD. Ankle fractures: supination-eversion fractures of stage IV. Primary and late results of operative and non-operative treatment. Acta Orthop Scand. 1980;51:981–990. doi: 10.3109/17453678008990904. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)