Abstract
Background
The introduction of new devices for total hip arthroplasty (THA) offers surgeons the ability to address deficits in the portfolio. However, once introduced, data regarding the performance of devices is not publicly available until their use is widespread.
Purpose/Questions
The objective of this study was to compare the clinical and radiographic performance, including patient reported outcomes and radiographic evidence of osseointegration, subsidence, and stress shielding, of the newer Actis femoral component to the Corail stem (DePuy Synthes, Warsaw, IN, USA), which has an extensive clinical history.
Methods
This short-term, retrospective cohort study was a single surgeon series of 330 anterior approach THAs, consisting of 165 cases using the Actis stem and 165 cases using the Corail stem. Both devices were cementless, titanium, tapered, hydroxyapatite–coated stems. They differed in geometry, neck choices, broach philosophy, and collar availability. Data was obtained for 1 year following THA. Functional outcomes were measured with the Hip Dysfunction and Osteoarthritis Outcome Score for Joint Replacement (HOOS, JR.) survey. Complications were recorded from patient charts, and radiographic analysis was performed for signs of osseointegration, subsidence, and stress shielding.
Results
The groups shared similar demographic characteristics except the Actis population was younger with fewer women. The complication rate did not significantly vary, and no patient required revision within the first year. Radiographically, one patient in each group demonstrated subsidence. No cases exhibited radiolucent lines, and the prevalence of stress shielding at 1 year was comparable. HOOS, JR. scores did not significantly vary at 8 weeks or 1 year.
Conclusion
The Actis stem does not carry an increased risk of device-related complications compared with the Corail implant. Although aspects of bone remodeling differed between groups, Actis achieved radiographic signs of bone ingrowth at the 1-year mark and performed well clinically, with equivalent patient reported outcome scores to the Corail stem.
Electronic supplementary material
The online version of this article (10.1007/s11420-020-09792-2) contains supplementary material, which is available to authorized users.
Keywords: total hip arthroplasty, Actis, Corail, complications, outcomes
Introduction
Total hip arthroplasty (THA) implant technology continues to evolve. Femoral stem designs have progressed, with aims to decrease blood loss, minimize pain, prevent fracture, limit loosening, permit activity, and increase implant survivorship [16]. The frequently utilized Corail femoral stem (DePuy Synthes, Warsaw, IN, USA) has demonstrated 96.3% survival at 23 years [1]. Since its release in 1986, the Corail stem has encountered a few issues. Use of the Corail stem was associated with an increased risk of adverse reaction to metal debris in metal-on-metal bearings [21]. Batches of the second generation Corail stem, which contained a laser-etching on the stem’s neck, were recalled after reports of increased fracture rates [19]. More recently, a Canadian study inspected the treatment for intracapsular displaced hip fractures within a group of hospitals and reported a higher incidence of intraoperative periprosthetic fractures in patients who received a cemented Corail in comparison with a cemented OmniFit EON (Stryker, Kalamazoo, MI, USA) stem [17]. Nevertheless, the Corail stem has generally exhibited positive outcomes with some of the highest gains in life after total hip arthroplasty in comparison with other femoral stems [20]. Now on its 3rd generation model, the Corail stem comes in sizes ranging from 95 to 170 mm and features a stepped geometry, which is meant to improve compression loading, decrease shear forces, and increase range of motion. It is available as a standard collarless or collared stem, a high offset collarless stem, and a coxa vara collared alternative. The collared options were designed with the goal of limiting subsidence and providing rotational stability [7]. In addition, it is entirely coated with hydroxyapatite to block the release of metal ions and promote osseointegration with the endosteal surface [24].
In 2016, DePuy Synthes began evaluating its new Actis® Total Hip System, which was designed to aid surgeons in tissue-sparing approaches. The “fit and fill” titanium stem features a medial collar and triple taper geometry designed to resist early subsidence, permit early weight bearing, and improve stem stability [6, 8]. Actis offers a shorter range of stem lengths than the Corail, with sizes varying from 95 to 170 mm. In addition, the stem is inserted with a hybrid broach, which combines extraction and compaction broaching technology to allow for an adequate fit while preserving patient anatomy [5, 6]. Like Corail, Actis is coated in hydroxyapatite; however, the proximal portion of the Actis stem contains Duofix® (DePuy Synthes, Warsaw, IN, USA), which consists of a coating composed of titanium sintered beads with the addition of a hydroxyapatite layer to promote fixation [5]. The company’s early evaluation of the Actis system in 1183 patients indicated positive short-term outcomes, with only five adverse events reported (0.42%), including two intraoperative calcar fractures, one periprosthetic fracture that occurred 2.5 weeks post-operatively, one femoral perforation that occurred due to misdirected broaching, and one case of cellulitis 20 days post-operatively. The company reviewed radiographs from 325 patients and reported that no signs of loosening, radiolucent lines, or dislocation were observed [8].These findings were not compared with other stems.
Data regarding the results of new THA devices frequently lag years behind the introduction of the technology, with industry sponsored studies often being the only source of early data. When a new femoral component, such as the Actis stem, is used in its early phases, the surgeon does not have information on what is “normal” or expected clinically and radiographically, which presents difficulties in interpreting patient complaints in the first year after arthroplasty. Surgeons who are familiar with the Corail and perform anterior approach hip arthroplasty may be eager to transition to the Actis due to its perceived advantages of implantation through this approach. Presently, there is no peer-reviewed literature pertaining to Actis, and to the authors’ knowledge, this is the first investigation of the new stem without industry involvement or conflicts of interest.
The purpose of this study was to evaluate the Actis femoral stem and compare it to the well-established Corail stem. In particular, we aimed to answer the following questions: (1) Does the Actis stem vary in complication and reoperation rates within the first year following THA? (2) Do THA patients who receive an Actis stem report similar post-operative functional outcomes compared to those with a Corail stem? (3) How does the radiographic behavior, including pre-operative templating size, evidence of osseointegration, rate of subsidence, and rate of stress shielding, of the Actis stem compare with that of the Corail stem?
Methods
In this short-term, retrospective cohort study, we reviewed the charts and radiographs of 330 patients who underwent THA and who met inclusion criteria (out of 361 cases examined for potential eligibility). Cases were included in the study if the patient was at least 18 years old, received a primary THA performed by one orthopedic surgeon, had surgery between November 2016 and July 2018, and received either an Actis or Corail stem. Charts with missing 2-week post-operative radiographs were excluded, as the radiograph was a necessary baseline that 8-week and 1-year imaging would later be compared to. The cohort was subdivided based on whether an Actis or Corail femoral stem was implanted, with 165 cases in each group. The choice on whether to use an Actis or Corail was based on surgeon judgment. Each case underwent digital templating prior to surgery using commercially available software (OrthoView, Plymouth, MI, USA). At that time, variables such as patient age and gender, femoral morphology, and a subjective assessment of bone density were performed with the templating to select the ideal femoral stem. A collar was utilized in all cases when available, which included all Actis, as well as standard and varus offset Corail cases. High offset Corail was not available with a collar during the study period and this group was implanted without a collar. In addition, each case was performed via an anterior approach with an orthopedic table and utilized the Pinnacle acetabular cup (DePuy Synthes, Warsaw, IN) with a polyethylene liner.
Data was collected for 1 year following each patient’s procedure. Standard patient follow-up appointments were at 2 weeks, 8 weeks, and 1 year after surgery. Information obtained from electronic health records consisted of patient demographics, surgical data, implant choice, template stem size, actual stem size utilized, intra- and post-operative complications, American Society of Anesthesiologists (ASA) physical classification, and post-operative radiographs. Complications were defined as dislocation, intraoperative calcar fracture, post-operative periprosthetic fracture, infection with return to the operating room for wound irrigation and debridement, a rectus muscle tear diagnosed by ultrasound, and arthroplasty revision. Outcomes were measured via 8-week and 1-year Hip Dysfunction and Osteoarthritis Outcome Score for Joint Replacement (HOOS, JR.) surveys. The HOOS, JR. survey contains 6 questions assessing hip pain and daily function [18]. An interval score of 0 signifies complete hip disability, whereas 100 indicates ideal hip health.
Radiographic analysis was performed by two trained evaluators (SVK and ACG) for 2-week, 8-week, and 1-year scans. Subsidence was amongst the primary radiographic outcomes assessed and defined as an increase in prosthesis-greater trochanter distance of ≥ 2 mm [10]. Femoral component zones, as described by Gruen et al. [13, 15], were further examined for signs of radiolucency and bony changes, including the formation of pedestals, spot welds, cortical hypertrophy, calcar rounding, calcar atrophy, and stress shielding [2]. A pedestal is defined as sclerosis at the distal tip of the femoral stem, which bridges the medullary canal. Similarly, a spot weld is an area of new endosteal bone, which contacts the prosthesis [25]. Cortical hypertrophy refers to the increase in the cortical thickness along the femoral diaphysis medially and/or laterally. Calcar rounding was defined as smoothing of the proximal medial corner of the femoral neck osteotomy [9, 23].We distinguished calcar rounding from calcar atrophy, with the latter defined as resorption of calcar bone extending distally from the proximal edge of the femoral neck osteotomy adjacent to the implant [3]. Lastly, stress shielding is the redistribution of a load (i.e., stress on the bone) from the femoral and intertrochanteric region to the femoral diaphysis, resulting in bone resorption at the proximal-lateral aspect of the femur and hypertrophy on the medial side of the femur [25]. Sample size was calculated based on previously published studies [1, 9, 11, 26] from which the investigators anticipated an expected proportion (P), ≤ 0.10 ± 0.05 (width = 0.10) with a 90% confidence level of radiographic evidence of subsidence, bone ingrowth, and bone remodeling in both stems; which called for a minimum of 100 charts per group for a total of at least 200 charts. Statistical analysis was conducted utilizing a t test for continuous (mean ± standard deviation), normally distributed data and a χ-square test for categorical (percent) data. A two-tailed p value of ≤ 0.05 was deemed statistically significant. Analyses were computed using SPSS for Windows, version 22.0 (IBM Corp., Armonk, NY, USA).
Results
Out of the 330 THA cases reviewed in this series, 290 (144 Actis and 146 Corail) followed-up on time and had available progress notes and radiographs through 1 year in the electronic medical record. Patients who received an Actis stem were younger (62.66 vs. 69.79 years, p < 0.001) with fewer women (43% vs. 73.3%, p < 0.001) than in the Corail group. While the majority of procedures were performed within a hospital for both groups, the Actis cohort had a higher percentage of surgeries done at an ambulatory surgical center (13.9% vs. 4.2%, p = 0.002). There were 2 intraoperative calcar fractures (1.4%), 2 rectus muscle tears (1.4%), and 1 dislocation (0.7%) in the Corail group, with no Actis cases experiencing these complications. Neither group sustained a periprosthetic fracture, and no patients required stem revision within the first year following THA. In addition, 3 Actis and 3 Corail patients returned to the operating room for irrigation and debridement. In the Corail group, the indications for return to the operating room were two cases of superficial wound breakdown requiring debridement and closure with the use of oral antibiotics and one deep infection that underwent debridement and polyethylene liner/femoral head exchange in addition to a 6-week course of intravenous antibiotics followed by oral suppression. There has been no recurrence of infection in these cases at the time of last follow-up. There were no deep infections in the Actis group, with two of the debridements done for wound breakdown and the other performed for an evacuation of a noninfected seroma. Each of these patients recovered uneventfully. Further demographic data and list of complications are presented in Table 1.
Table 1.
Subject demographics (N = 330)
| Characteristic | Actis (n = 165) | Corail (n = 165) | P value |
|---|---|---|---|
| Age at surgery, in years | 62.66 ± 9.2a | 69.79 ± 7.3 | < 0.001 |
| Gender | < 0.001 | ||
| Male | 94 (57)b | 44 (26.7) | |
| Female | 71 (43) | 121 (73.3) | |
| Body mass index (Kg/m2) | 29.13 ± 4.9 | 28.20 ± 5.7 | 0.117 |
| ASA class | 2.09 ± 0.51 | 2.15 ± 0.42 | 0.230 |
| Side | 0.911 | ||
| Right | 96 (58.2) | 97 (58.8) | |
| Left | 69 (41.8) | 68 (41.2) | |
| Operation time (min) c | 78.65 ± 11.1 | 82.31 ± 15.6 | 0.016 |
| Length of hospital stay (days) | 1.54 ± 1.1 | 2.09 ± 1.1 | < 0.001 |
| Discharge disposition | |||
| Home (vs. SNF)d | 136 (82.9) | 118 (72.4) | 0.022 |
| Length of follow-up (days) | 433.7 ± 119.7 | 444.6 ± 150.7 | 0.496 |
| Difference between template and actual stem size | 0.92 ± 0.92 | 0.92 ± 0.77 | 0.983 |
| Complications | |||
|
Intraoperative calcar fracture Periprosthetic fracture Dislocation Infection Revision Rectus muscle tear |
0 0 0 3 0 0 |
2 0 1 3 0 2 |
0.156 ----- 0.317 1.000 ----- 0.156 |
| HOOS, JR. score | |||
|
8-week 1-year |
83.26 ± 13.0 91.77 ± 12.8 |
83.86 ± 13.4 91.30 ± 11.4 |
0.783 0.768 |
aData are expressed as mean ± standard deviation
bData are expressed as number (percent)
cFirst cut to close
dSkilled nursing facility
HOOS, JR. outcome scores were comparable at 8 weeks (83.26 in Actis and 83.86 in Corail, p = 0.783) and 1 year (91.77 in Actis and 90.30 in Corail, p = 0.768). We further separated the number of cases that fell into excellent, satisfactory, and poor HOOS, JR. score categories (Table 3). There was no significant difference between the percentage of Actis and Corail patients that scored ≥ 80, 60–79, or ≤ 59 points at 8 weeks or 1 year following arthroplasty.
Table 3.
Breakdown of HOOS, JR. outcomes
| Score Range | ≥ 80 | 60–79 | ≤ 59 | P value |
|---|---|---|---|---|
| 8-week | 0.902 | |||
|
Actis Corail |
45 (60) 47 (62.7) |
26 (34.7) 25 (33.3) |
4 (5.3) 3 (4.0) |
|
| 1-year | 0.085 | |||
|
Actis Corail |
90 (79.6) 107 (87.7) |
21 (18.6) 11 (9.0) |
2 (1.8) 4 (3.3) |
|
aData are expressed as number (percent)
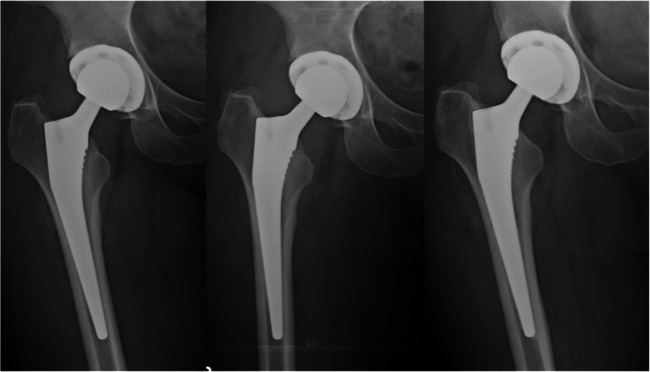
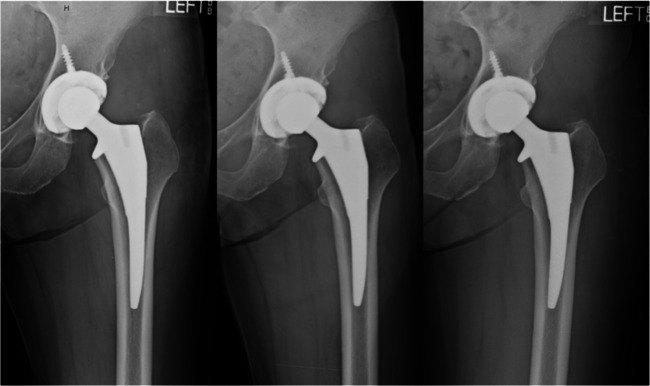
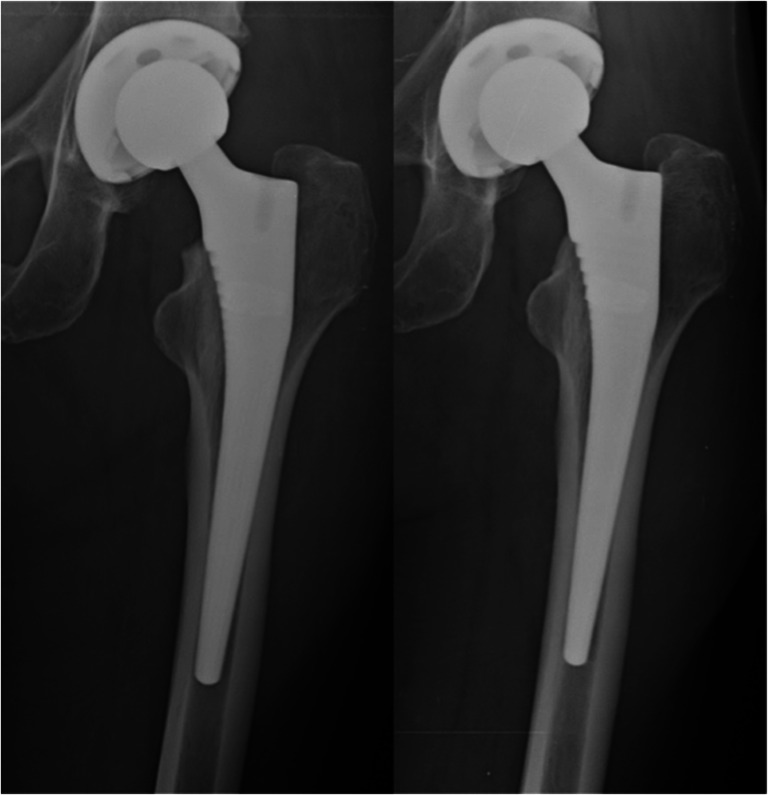
Imaging was reviewed for all patients in the study, with 290 patients having a complete set of radiographs through the first post-operative year and included in radiographic analysis. Radiographic evaluation revealed one case in each group that exhibited subsidence greater than 2 mm. Overall, the average change in greater trochanter-to-stem shoulder distance between 2 weeks and 1 year was 0.535 mm for Actis and 0.512 mm for Corail (p = 0.660) (Fig. 1). No cases demonstrated radiolucency 2 mm or greater around the implant at any time. Pedestal formation occurred in 6 Actis and 9 Corail cases, all of which were seen on the 1-year radiographs (p = 0.442) (Figs. 2 and 3). Fewer Actis patients displayed spot-welding at 8 weeks (38.2% vs. 63.0%, p < 0.001) and 1 year (90.3% vs. 97.3%, p = 0.014). Cortical hypertrophy was unusual at 8 weeks but was found in 14.6% and 6.2% (p = 0.019) of Actis and Corail cases on 1-year radiographs, respectively (Figs. 2 and 3). A greater number of Actis patients demonstrated calcar atrophy at 8 weeks (8.3% vs. 2.1%, p = 0.016) and 1 year (9.0% vs. 0.7%, p = 0.001). The only radiographic difference between the Corail subsets was that collarless stems experienced a higher rate of calcar rounding than their collared counterparts at 1 year (61.9% vs. 13.2%, p < 0.001). However, calcar rounding had a similar prevalence in both groups as a whole, with 46.5% of Actis and 47.3% of Corail patients exhibiting calcar round-off at 1 year (p = 0.901) (Fig. 4). Finally, stress-shielding was rarely seen on 8-week radiographs but was noted in 7.6% of Actis (Figs. 2 and 5) and 13.7% of Corail 1-year radiographs (p = 0.095) (Table 2).
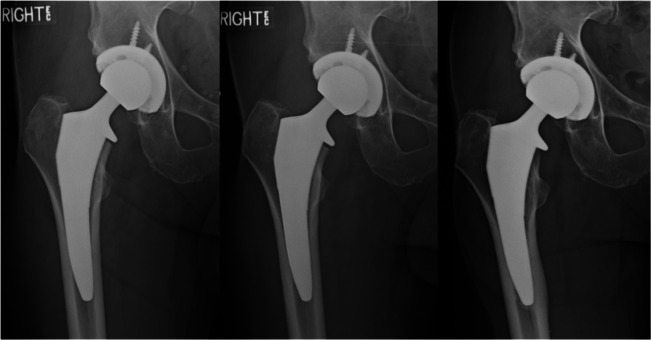
Fig. 1.

Radiograph of a right-sided Actis implant at 8-week postarthroplasty. The perpendicular distance from the tip of the greater trochanter to the shoulder of the stem was measured for 2-week, 8-week, and 1-year radiographs. Subsidence was calculated by taking the difference in these measurements between each interval. A difference of ≥ 2 mm was considered significant.
Fig. 2.
Two-week (left), 8-week (middle), and 1-year (right) radiographs of a patient with an Actis stem. Cortical hypertrophy, pedestal formation, calcar rounding, and stress shielding are evident at 1-year.
Fig. 3.
Two-week (left), 8-week (middle), and 1-year (right) radiographs of a patient with a collarless Corail stem. Cortical hypertrophy, pedestal formation, and spot-welding are visible at 1-year.
Fig. 4.
Development of calcar rounding in a patient with a Corail stem between 2-week (left) and 1-year (right) follow-up appointments.
Fig. 5.
Patient with a left Actis femoral component exhibiting radiographic stability between 2-week (left), 8-week (middle), and 1-year (right) follow-up appointments.
Table 2.
Radiographic findings (N = 290)
| Radiographic characteristic | Actis (n = 144) | Corail (n = 146) | P value |
|---|---|---|---|
| Subsidence ≥ 2 mm | 1 | 1 | – |
| Radiolucent lines ≥ 2 mm | 0 | 0 | – |
| Pedestal formation (1-year) | 6 (4.2)a | 9 (6.1) | 0.442 |
| Spot weld formation | |||
|
8-week 1-year |
55 (38.2) 130 (90.3) |
92 (63.0) 142 (97.3) |
< 0.001 0.014 |
| Cortical hypertrophy | |||
|
8-week 1-year |
4 (2.8) 21 (14.6) |
4 (2.7) 9 (6.2) |
0.984 0.019 |
| Calcar rounding | |||
|
8-week 1-year |
9 (6.3) 67 (46.5) |
6 (4.1) 69 (47.3) |
0.411 0.901 |
| Calcar atrophy | |||
|
8-week 1-year |
12 (8.3) 13 (9.0) |
3 (2.1) 1 (0.7) |
0.016 0.001 |
| Stress shielding | |||
|
8-week 1-year |
2 (1.4) 11 (7.6) |
5 (3.4) 20 (13.7) |
0.259 0.095 |
aData are expressed as number (percent)
Analysis was further performed by comparing these data points for a subgroup consisting of women ages 70 and older. There were 14 Actis and 59 Corail cases that fit into this category. Actis female 70+ cases had shorter operation times (73.14 vs. 83.36 min; p = 0.048), consistent with the overall shorter operation duration for the Actis cohort. Likewise, fewer Actis 70+ women exhibited spot-welding at 8 weeks (7.1% vs. 62.7%; p < 0.001) and 1 year (84.6% vs. 100%; p = 0.006). However, Actis 70+ women exhibited a smaller difference between the templated and actual stem size utilized (0.38 vs. 0.92; p = 0.021). In addition, a greater percentage of this Actis subgroup received a high offset stem (28.6% vs. 1.7%, p < 0.001). Each group had one 70+-year-old female who experienced a complication, both of which were infections requiring irrigation and debridement. There were no other significant differences between the two subgroups, and the data was consistent with the overall results for Actis and Corail cases.
Discussion
The main purpose of this study was to assess the clinical and radiographic behavior of the Actis stem in comparison with the well-studied Corail. The results of our short-term study indicate the Actis stem offers similar clinical and radiographic results to the Corail, without an increased rate of mechanical complications. Specifically, the Actis stem did not have an increased incidence of intraoperative calcar fracture, subsidence, periprosthetic fracture, or aseptic loosening compared with the Corail. Additionally, the 8-week and 1-year HOOS, JR. scores also did not differ between groups. However, the Actis and Corail did demonstrate significant differences in some radiographic signs of bone ingrowth. Radiographs of cases with the Actis stem had a lower incidence of spot welds (38.2% vs. 63%), but a higher incidence of calcar atrophy (8.3% vs 2.1%) at 8 weeks compared with the Corail. At 1 year, Actis cases were more likely to demonstrate cortical hypertrophy (14.6% vs. 6.2%) and calcar atrophy (9% vs. 0.7%) compared with the Corail. Overall, more than 90% of cases in this series demonstrated radiographic spot welding 1-year post-operatively.
This study has several limitations including its retrospective nature, lack of randomization, single surgeon results, absence of an interobserver reliability test, and short-term follow-up. Ideally, a study comparing two femoral components would be performed in a prospective, randomized fashion. As this was not the case in the current work, bias may be introduced. The most obvious bias is that patients were not randomized to either group; they were assigned to a group based on surgeon judgment. This resulted in demographic variation within the Actis and Corail groups, with Actis patients being significantly younger and having a higher proportion male. This difference certainly limits the generalizability of our data to the larger population. Age and gender have been shown to influence femoral component survivorship [4, 12, 14]. In an effort to minimize complications with a new device until it was proven to be safe and effective, the senior author was more likely to assign lower risk patients to the Actis stem. We did study a subset of cases, women over 70 years, in an effort to mitigate this limitation. Although only 14 Actis cases were women over 70, their results and complication rates were similar to Corail and to the study population as a whole. The single surgeon nature also limits the generalizability of the results but does provide a consistent technique between the groups in this study. There was no formal interobserver reliability test between the radiograph evaluators; however, both evaluators reviewed each radiograph in the study and were in agreement regarding measurements and radiographic findings. Finally, while the short term follow-up does not provide information on the long-term durability of these devices, it did help us answer the question of whether the new device carried a higher immediate risk of femoral complications.
Despite these limitations, we feel that our research was able to answer the study questions posed. As new devices are introduced, they are often adopted quickly with little supporting data. Additionally, much of the early data comes from sources with ties to the device manufacturer, which may bias the results. The primary study question we set out to answer was if the Actis stem had a higher risk of femoral complications compared to the Corail. The Corail stem has low reported rates of fracture and loosening [22, 26], but this data currently does not exist for the Actis. Our study demonstrates a very low complication rate for the Actis stem, with no cases of loosening or periprosthetic fracture in the first year after surgery in our study cohort.
Currently, there is no peer reviewed information on how patients report their outcomes with the Actis stem. Patient complaints about pain or dysfunction in the first year after THA are difficult to interpret for a new femoral stem, when its clinical course is unknown. Along these lines, another question we sought to answer was whether the Actis and Corail had similar short-term patient reported outcomes (PRO). We used HOOS, JR. scores as the PRO because of its simplicity, availability, and our practice’s concomitant use of it for quality reporting. Our results indicate similar improvement in HOOS, JR. scores at 8 weeks and 1 year for both the Actis and Corail groups. We also wanted to compare how many patients in each group had poor early outcomes, and how these patients ultimately progressed. Poor HOOS, JR. scores were rare and similar between groups at 8 weeks and 1 year post-operatively. This can be interpreted that patients with an Actis stem do not typically have more pain or dysfunction than Corail patients at 8 weeks or 1 year. Thus, if an Actis patient experiences unexpected symptoms, the surgeon should follow similar work up as he or she would for a patient with a Corail stem.
The third aim of this study was to investigate the radiographic behavior of the Actis stem. This information is critical for surgeons as it is a main factor in interpreting whether a patient complaint is related to a mechanical complication. When using templating software, intraoperative questions arise when the implanted and planned sizes differ. This can be a result of calibration error or user error. With regard to the pre-operative planning of Actis, our data indicates that experienced surgeons who use this templating software should expect similar results of final implant size compared with templated size as with the Corail. The Actis stem achieved radiographic evidence of bone ingrowth at 1 year, with over 90% of cases exhibiting spot welding, although less than the 97% of Corail cases that demonstrated this finding. Similar to the Corail, the Actis stem had a quiet radiographic appearance with no cases demonstrating radiolucent lines > 2 mm in any Gruen zone. The Actis also had low rates of stress shielding (7.6%), cortical hypertrophy (14.6%), and calcar atrophy (9%), which suggest that the proximal geometry and collared design are working as intended to transfer load physiologically to the proximal femur. For the surgeon interpreting radiographs at 8 weeks, it should be stated that signs of bone ingrowth (spot welding, calcar rounding) were subtle and not present in over half the cases and should not be considered pathological.
In conclusion, development of new total hip arthroplasty devices increases a surgeon’s options when selecting the most appropriate femoral component for a given patient. Decisions regarding the quality of a new device are more informed once the device has been in use, and patient outcomes have been reported. Although patient demographics and bony changes varied, this study revealed that the new Actis stem has similar patient outcomes to the better studied Corail stem. Longer-term studies to evaluate the proximal femoral bone behavior as well as more diversified patient groups are needed. Overall, Actis effectively achieves signs of bone ingrowth and does not carry an increased risk of complications within 1 year of surgery in our study group, making this device a viable option in total hip arthroplasty.
Electronic supplementary material
(PDF 753 kb)
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III: Therapeutic Study
References
- 1.Al-Najjim M, Khattak U, Sim J, Chambers I. Differences in subsidence rate between alternative designs of a commonly used uncemented femoral stem. J Orthop. 2016;13(4):322–326. doi: 10.1016/j.jor.2016.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakkai A, Ryan P, Goga I. Tapered uncemented HA-coated femoral stems: a radiological study. SA Orthop J. 2017;16(3):27–30. doi: 10.17159/2309-8309/2017/v16n3a2. [DOI] [Google Scholar]
- 3.Bodén HS, Sköldenberg OG, Salemyr MO, Lundber HJ, Adophson PY. Continuous bone loss around a tapered uncemented femoral stem: a long-term evaluation with DEXA. Acta Orthop. 2006;77(6):877–885. doi: 10.1080/17453670610013169. [DOI] [PubMed] [Google Scholar]
- 4.DePuy Synthes. Actis™ Total Hip System Surgical Technique. Johnson & Johnson. 2017. http://synthes.vo.llnwd.net/o16/LLNWMB8/US%20Mobile/Synthes%20North%20America/Product%20Support%20Materials/Technique%20Guides/Actis%20Surgical%20Technique%20March%202018.pdf.2007. [accessed 8 December 2019].
- 5.DePuy Synthes. Actis® Total Hip System Design Rationale. Johnson & Johnson. 2016 http://synthes.vo.llnwd.net/o16/LLNWMB8/US%20Mobile/Synthes%20North%20America/Product%20Support%20Materials/Technique%20Guides/Actis%20Design%20Rationale.pdf. [accessed 8 December 2019].
- 6.DePuy Synthes. Corail® Hip System: Product Rationale and Surgical Technique. Johnson & Johnson. 2019. http://www.corailpinnacle.net/sites/default/files/DSEMJRC061606652%20CORAIL%20Platform%20Brochure.pdf. [accessed 31 March 2020].
- 7.de Thomasson E, Caux I, Guingand O, Terracher R, Mazel C. Total hip arthroplasty for osteoarthritis in patients aged 80 years or older: influence of co-morbidities on final outcome. Orthop Traumatol Surg Res. 2009;95(4):249–53. doi: 10.1016/j.otsr.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Diaz R, Mantel J, Lee K. Actis™ Total Hip System: Early Clinical Results. Johnson & Johnson. 2016. https://jnjinstitute.com/sites/default/files/2019-06/DSUSJRC07172231-ACTIS-Early-Performance-Data-Collection.pdf. [accessed 8 December 2019].
- 9.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69(1):45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 10.Engh CA, Hooten JP, Jr., Zettl-Schaffer KF, et al. Porous-coated total hip replacement. Clin Orthop Relat Res. 1994:(298):89–96. [PubMed]
- 11.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;(257):107–28. [PubMed]
- 12.Fang M, Noiseux N, Linson E, Cram P. The Effect of Advancing Age on Total Joint Replacement Outcomes. Geriatr Orthop Surg Rehabil. 2015;6(3):173–9. doi: 10.1177/2151458515583515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 14.Inacio MC, Ake CF, Paxton EW, Khatod M, Wang C, Gross TP, Kaczmarek RG, Marinac-Dabic D, Sedrakyan A. Sex and risk of hip implant failure: assessing total hip arthroplasty outcomes in the United States. JAMA Intern Med. 2013;173(6):435–41. doi: 10.1001/jamainternmed.2013.3271. [DOI] [PubMed] [Google Scholar]
- 15.Johnston RC, Fitzgerald RH, Jr, Harris WH, Poss R, Muller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Joint Surg Am. 1990;72(2):161–8. doi: 10.2106/00004623-199072020-00002. [DOI] [PubMed] [Google Scholar]
- 16.Kim JT, Yoo JJ. Implant Design in Cementless Hip Arthroplasty. Hip Pelvis. 2016;28(2):65–75. doi: 10.5371/hp.2016.28.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Laflamme M, Angers M, Vachon J, Pomerleau V, Arteau A. High Incidence of Intraoperative Fractures With a Specific Cemented Stem Following Intracapsular Displaced Hip Fracture. J Arthroplasty, 2019. 10.1016/j.arth.2019.09.017 [DOI] [PubMed]
- 18.Lyman S. HOOS, JR. and KOOS, JR. Outcome Surveys. Hospital of Special Surgery. https://www.hss.edu/hoos-jr-koos-jr-outcomes-surveys.asp. 2017 [accessed 3 July 2019].
- 19.Merini A, Viste A, Desmarchelier R, Fessy MH. Cementless Corail femoral stems with laser neck etching: Long-term survival, rupture rate and risk factors in 295 stems. Orthop Traumatol Surg Res. 2016;102(1):71–6. doi: 10.1016/j.otsr.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Pennington MW, Grieve R, van der Meulen JH. Lifetime cost effectiveness of different brands of prosthesis used for total hip arthroplasty: a study using the NJR dataset. Bone Joint J. 2015;97-B(6):762–70. doi: 10.1302/0301-620X.97B6.34806. [DOI] [PubMed] [Google Scholar]
- 21.Reito A, Puolakka T, Elo P, Pajamaki J, Eskelinen A. High prevalence of adverse reactions to metal debris in small-headed ASR hips. Clin Orthop Relat Res. 2013;471(9):2954–61. doi: 10.1007/s11999-013-3023-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rivière C, Grappiolo G, Engh CA, Jr, et al. Long-term bone remodelling around ‘legendary’ cementless femoral stems. EFORT Open Rev. 2018;3(2):45–47. doi: 10.1302/2058-5241.3.170024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Santori FS, Santori N. Mid-term results of a custom-made proximal loading femoral component. J Bone Joint Surg Br. 2010;92(9):1231–7. doi: 10.1302/0301-620X.92B9.24605. [DOI] [PubMed] [Google Scholar]
- 24.Selvaratnam V, Shetty V, Sahni V. Subsidence in Collarless Corail Hip Replacement. Open Orthop J. 2015;9:194–7. doi: 10.2174/1874325001509010194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vanrusselt J, Vansevenant M, Vanderschueren G, Vanhoenacker F. Post-operative radiograph of the hip arthroplasty: what the radiologist should know. Insights Imaging. 2015;6(6):591–600. doi: 10.1007/s13244-015-0438-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vidalain JP. Twenty-year results of the cementless Corail stem. Int Orthop. 2011;35(2):189–94. doi: 10.1007/s00264-010-1117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 753 kb)