Abstract
Background
Since its release in 2015, the hoverboard has been associated with injuries in children and adolescents. However, its public health implications have yet to be explored in the orthopedic literature across multiple centers.
Purpose/Questions
We sought to assess the nature of orthopedic injuries and the use of clinical resources related to the hoverboard at four high-volume, regional pediatric hospitals.
Methods
Departmental databases of emergency department (ED) consultations and urgent orthopedic clinic (UC) visits were queried for hoverboard injuries. A retrospective medical record review was performed for patients presenting over a 3-month period at four institutions. Data on demographics, injuries, clinical course, and resource use were analyzed. The frequency of hoverboard-related consultations was compared to those for monkey bar–related injuries at the primary study institution.
Results
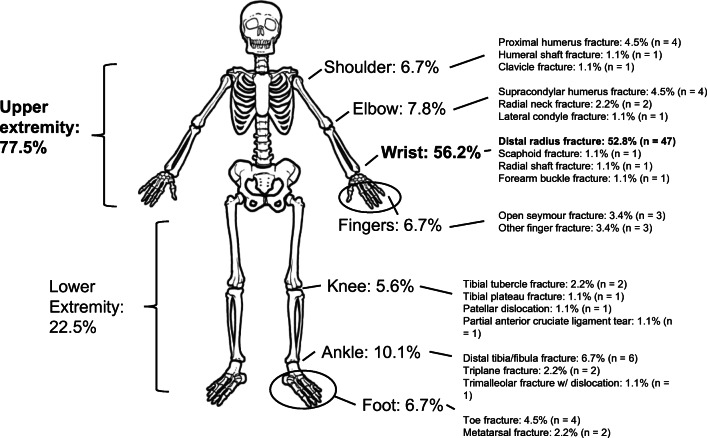
Eighty-nine patients with orthopedic hoverboard injuries presented to the ED and/or UC in the study period. Hoverboard injuries represented 2.2% of orthopedic ED consultations at the primary institution, compared to 1.5% for monkey bar injuries. Sixty-nine out of 89 (77.5%) total injuries involved the upper extremity, including 47 (52.8%) distal radius fractures, the most common hoverboard–related diagnosis. All but one injury (97.8%) underwent radiography, and eight (9%) required surgery. No patients reported wearing protective gear at the time of their injury.
Conclusions
Hoverboards were associated with a variety of pediatric orthopedic injuries and required the use of significant resources in the ED, UC, and operating room. These data may represent a starting point for further prospective multi-center studies and public health efforts toward prevention of hoverboard injuries.
Electronic supplementary material
The online version of this article (10.1007/s11420-019-09682-2) contains supplementary material, which is available to authorized users.
Keywords: hoverboard, pediatrics, distal radius, urgent care
Introduction
The first hoverboard prototype was released in April 2015, and sales surged in the latter half of that year and into the winter holiday season. A hoverboard (or hover board) is a handle-less, motorized, two-wheeled scooter that uses electronics and precision sensors to accelerate in the direction of the user’s transfer of body weight. Its use is associated with sudden accelerations forward or backward, or in rotation, when standing upright. It requires a keen sense of balance and control and poses significant risk of forward, backward, and torsional falls, as well as a risk of fingers and toes catching in the wheels. As a result, the hoverboard has been associated since its release with various orthopedic injuries, particularly in children, including upper-extremity fractures related to falls [2, 6, 9, 12, 13, 17, 18, 20] and non-orthopedic injuries, such as concussions and burns (the devices presented a fire hazard). Around the December 2015 holiday season, many social media and news outlets reported injuries related to hoverboards. Consequently, retailers including Amazon.com imposed a ban on selling many of the products at the time, due to safety concerns, even offering customers refunds in January 2016. Similarly, government safety officials in many countries responded with new legislation and impoundment of the devices, due to their injury risk and explosion history.
As a result, a new burden of injury may have been introduced to the constellation of orthopedic pathology presenting to emergency departments and urgent care clinics. However, this popular toy’s public health implications have yet to be explored in the orthopedic literature in multi-center fashion or across different regions. We therefore sought to assess the nature of orthopedic injuries and clinical resources used that are associated with hoverboard injuries at four high-volume, regional pediatric referral centers in three geographic regions over a discrete 3-month period. Our primary aim was to better understand injury mechanisms, safety concerns and regulations needed, and burden on the health care system and society at large. Our secondary aim was to provide an epidemiologic perspective on hoverboard injuries by comparing the frequency and nature of these injuries to another common cause of pediatric orthopedic injury—monkey bars.
Materials and Methods
A departmental database of emergency department (ED) and urgent orthopedic clinic (UC) visits at a single regional tertiary care pediatric hospital were queried using a word search for “hoverboard” and “hover board” injuries to identify all pediatric and adolescent cases (ages 0 to 19 years) of orthopedic injuries related to hoverboard use between December 25, 2015, and March 25, 2016. An original inter-departmental digital trauma-tracking program designed to monitor all orthopedic consultations was also cross-referenced to optimize the search for orthopedic injuries seen in the ED. Comparable searches were performed at three other hospitals in two additional US regions. All four institutions are American College of Surgeons–verified level-1 trauma centers in urban areas on the East and West Coasts. To provide greater perspective on the resource use associated with hoverboard injuries over time, the entire course of care of patients treated at the primary institution, which included the highest-volume cohort, was analyzed with data obtained from all follow-up visits with orthopedic providers in any orthopedic clinic, including beyond the study period.
A retrospective medical record review was performed to collect various data points, when available, for the resulting study population, including demographic information (date of birth [DOB], age, sex), injury variables (date of injury [DOI], mechanism, diagnosis, location of injury, protective gear worn), clinical course (time missed from school or sports, length of recovery), and hospital resource use (imaging, casting, reduction, surgery, hospital admission). The frequency of hoverboard-related consultations at the primary study institution was compared to that of monkey bar–related injuries at the same institution over the same 3-month period. Statistical analysis consisted of descriptive statistics, means, ranges, and comparisons of injury rates.
Results
Eighty-nine patients with orthopedic hoverboard injuries presented to the ED and/or UC at the four hospitals in the 3-month study period. Of the 89 injuries, 15 (16.8%) occurred on Christmas Day. The study population consisted of 55 males and 34 females, with a mean age of 11.4 years (range, 4 to 18 years), with no difference in mean age detected between the sexes. No patients reported wearing protective gear at the time of their injury.
Thirteen patients presented to the ED at the primary study institution, representing 2.2% of all orthopedic ED consults over the study period, compared to 1.5% for monkey bar injuries. Thirteen additional patients presented to one of the primary institution’s UCs over that same period (three presented to outside EDs before presenting to the UC).
Of the 89 hoverboard–related injuries, 69 (77.5%) involved the upper extremity (Fig. 1); 47 (52.8%) were distal radius fractures, which was the most common hoverboard–related diagnosis. Seven (7.8%) injuries occurred to the elbow, six (6.7%) to the fingers, six (6.7%) to the upper arm or shoulder, and three (3.4%) to the forearm or other wrist bones. These diagnoses included supracondylar humerus fracture (n = 4), lateral condyle fracture (n = 1), radial neck fracture (n = 2), open Seymour fracture (n = 3), forearm buckle fracture (n = 1), scaphoid fracture (n = 1), humeral shaft fracture (n = 1), radial shaft fracture (n = 1), proximal humerus fracture (n = 3), and clavicle fracture (n = 1) (Fig. 1). The ankle was the most common site of lower-extremity injury (n = 9, 10.1%), with injuries including six distal tibia/fibula fractures, two triplane fractures, and a trimalleolar fracture with dislocation. There were five (5.6%) knee injuries, including a patellar dislocation, two tibial tubercle fractures, a partial anterior cruciate ligament tear, and a tibial plateau fracture. There were six fractures to the foot: two (2.2%) metatarsal fractures and four (4.5%) toe fractures.
Fig. 1.
Diagnoses and anatomical sites affected by hoverboard injuries.
At the primary study institution, where 26 patients sought care, the most common specified mechanism of injury was a fall onto outstretched hand (FOOSH), accounting for at least eight (30.8%) of the injuries at this institution. Other common mechanisms of injury included finger entrapment in the wheel (3/26, 11.5%) and falling backward (2/26, 7.7%), although 11/26 (42.3%) had falls with unspecified mechanisms.
Of the 45 patients with diagnostic data provided, all but one (97.8%) required radiographs, and advanced imaging (magnetic resonance imaging or computed tomographic scanning) was used for six (13.3%). Twenty-one patients (80.8%) at the primary institution underwent multiple sets of radiographs, with an average of three sets per patient. Five children (19.2%) underwent five or more sets of X-rays. Of patients from all sites, 31 (34.8%) required anesthesia in the course of care, including 21 (23.6%) reductions of displaced fractures under sedation (four with pinning procedures performed in the ED) and eight (9%) undergoing surgery in the operating room. All three finger fractures at the primary institution were hoverboard wheel injuries requiring surgery, consisting of fracture irrigation and debridement (I&D), nailbed repair, and percutaneous or open fixation. Other surgeries performed across all sites included percutaneous pinning of a lateral condyle fracture, open reduction with internal fixation (ORIF) of a tibial tubercle avulsion fracture, ORIF of a medial malleolus fracture with syndesmosis injury, ORIF of a trimalleolar ankle fracture with dislocation, and I&D with percutaneous fixation of a great toe Seymour fracture. Six patients (13.3%) from three sites were admitted to the hospital. Casting was performed for 35 out of 45 injuries (77.8%) at those same sites, ranging from 2 to 10 weeks of casting duration.
At the primary institution, one child missed 8 weeks of school due to his injury, another attended school in a wheelchair, and at least eight (30.8%) were prescribed an opioid pain medication. All 26 patients at this site were required to discontinue athletic activities for at least 4 weeks and as long as 6 months (mean, 7.4 weeks). After the initial ED or UC visit, patients made an average of 3 (range, 0 to 7) additional visits to the UC for evaluation. The average time at which the orthopedic surgeon discharged from clinic or recommended follow-up on an as-needed basis was 8.1 weeks (range, 4 to 16 weeks), with several patients requiring additional follow-up visits for radiographs to assess for growth disturbance.
Discussion
We found the hoverboard, a popular new recreational device marketed primarily to children, to be associated with a variety of orthopedic injuries. These injuries often required substantial resource use in EDs, UCs, and operating rooms, as well as follow-up care in orthopedic clinics. The hoverboard appears to have been associated with a wide array of injuries to children, considerable time missed from activities, and a new health care burden.
The literature to date is devoid of multi-center or multi-region investigations of pediatric orthopedic hoverboard–related injuries in the USA. This multi-center study substantiates some of the findings and conclusions drawn in previous single-center or single-region studies in children: hoverboards have created a significant burden of injury, particularly upper-extremity fractures from falls [2, 6, 9, 12, 13, 16–18, 20]. All report a significant deficit in the use and regulation of protective gear.
There are limitations to our study. We determined that hoverboard-related injuries accounted for 2.2% of all orthopedic ED consults in a single hospital–based pediatric health care system over a 3-month period. This may be a gross underestimation, for a number of reasons. First, the study took place during winter, with the largest cohort drawn from a northern US region. Therefore, cold and otherwise adverse weather conditions likely deterred many children from using their hoverboards (although cold and wet weather may also increase injury rates in children). In addition, many, if not most, injuries such as abrasions and contusions may not be severe enough for treatment in the ED or UC. Limitations of retrospective methodology pertinent to this study include that some of the medical records may not have included the search terms we used in this study’s methodology. Non-orthopedic injuries such as burns and concussions were also not included, thereby lowering the overall health care burden of hoverboards on the ED and UCs.
Other recreational devices or toys, such as skateboards, in-line roller skates, trampolines, and monkey bars, have been associated with pediatric orthopedic injuries well known to emergency and orthopedic departments. As they became more popular, studies were published in pediatrics, emergency medicine, sports medicine, and orthopedics journals evaluating their use and their associated injury rates. For example, the first known use of the term “monkey bars” was in 1955 [8], and monkey bars have since posed a high falls risk. In the first equipment-specific injury requiring ED evaluation, the American Academy of Pediatrics reported that common injuries include fractures (upper extremity, 90%; supracondylar, 40%) and contusions [19]. In-line roller skates were first patented in 1953, and fractures have been reported to be the most common injury, with two-thirds of the fractures involving the distal forearm [10, 11]. Shortly after the rise of in-line roller skating, the first skateboard was made from roller skates attached to a board. A recent investigation of the epidemiology of skateboarding injuries reported that the most commonly injured body regions were the upper (44.1%) and lower (31.7%) extremities, and fractures and dislocations were the most common diagnoses [7]. Unlike in skateboarding, in which most injuries occur when the board strikes an irregularity in the riding surface, projecting the skateboarder in the direction of travel [4, 8], hoverboards can thrust the rider forward or backward, simply through its inherent function, which relies on electronic accelerometers.
In our study, hoverboard-related injuries represented 2.2% of all orthopedic ED consultations at the primary study institution, compared to 1.5% for monkey bar injuries. When comparing and contrasting rates of injury of upper versus lower extremities across four common or high-risk devices, as described in previous studies (Fig. 2), hoverboards caused more upper-extremity injuries than skateboards and in-line skates but less than monkey bars [7, 15, 19]. As the most common mechanism of injury for these devices is a fall, often onto an outstretched arm, upper-extremity injuries are most prominent. Wrist fractures are the most common diagnosis for these mechanisms, except for monkey bars, which has a higher rate of supracondylar fractures [3, 15, 19].
Fig. 2.
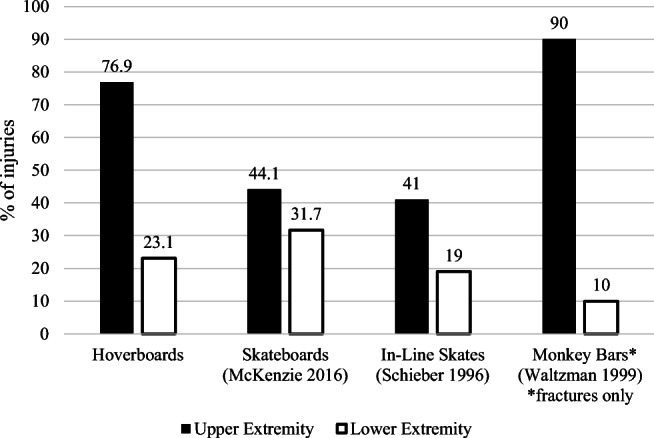
Rates of upper- and lower-extremity injuries related to hoverboards, skateboards, in-line skates, and monkey bars.
In response to the high injury rates from monkey bars, in-line skates, and skateboards, the Centers for Disease Control and Prevention (CDC) [1], the US Consumer Product Safety Commission (CPSC) [5], and the American Academy of Pediatrics [4], among other institutions, have made recommendations on the construction and implementation of these devices. Traffic regulations, safety guidelines, and restrictions based on age and common sense have been implemented at various levels. Although not all have been proven to reduce injury, measures that have been recommended to prevent injuries include wearing personal protective equipment (wrist guards, helmets, knee, and elbow pads), improving environmental conditions, providing lessons for novice users, certifying instructors, encouraging physical preparation and safety education, improving equipment design and standards, and refining government policy and regulation [14]. One study published in the New England Journal of Medicine showed that wrist and elbow guards were effective modes of protection from injury [15].
Considering the high demand for the hoverboard in the year of its introduction, and the resulting high number of unforeseen injuries, we hope that our findings might assist with preparations for the release of other toys and recreational devices. For example, it may be prudent to establish a network for active surveillance of injuries in order to quickly respond with safety recommendations for such situations in the future.
As a result of this investigation, we recommend that more widespread safety regulations be established regarding hoverboards. Several airlines have banned hoverboards on flights to prevent explosion of their lithium batteries, and some regions have regulated where they may be used in public. However, none of the patients in the current study reported wearing safety gear, and the rates of missed school and activities as a result of hoverboard-related injuries were high. Increasing legislation and knowledge of other safety measures similar to those cited above in conjunction with monkey bars, in-line skates, and skateboards would likely aid in preventing the hoverboard-related orthopedic injury burden we found in this study. This is particularly important now, given the recent rise of similar devices. These data may also represent a starting point for further prospective multi-center research and public health efforts toward prevention measures related to hoverboards.
Electronic Supplementary Material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Nicole H. Goldhaber, MA; Amanda N. Goldin, MD; Kristin Livingston, MD; Benjamin J. Shore, MD; Dennis E. Kramer, MD; and Jason E. Jagodzinski, MD, declare that they have no conflicts of interest. Andrew T. Pennock, MD, reports personal fees from Orthopediatrics and stock options from Imagen, outside the submitted work. Donald S. Bae, MD, reports grants from Pediatric Orthopaedic Society of North America and royalties from Lippincott Williams & Wilkins, outside the submitted work. Yi-Meng Yen, MD, PhD, reports personal fees from Smith & Nephew and from Orthopediatrics, outside the submitted work. Benton E. Heyworth, MD, reports stock options from Imagen, royalties from Springer, and grants from Pediatric Orthopaedic Society of North America, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: IV
References
- 1.Centers for Disease Control and Prevention (CDC) Playground-related injuries in preschool-aged children—United States, 1983–1987. MMWR Morb Mortal Wkly Rep. 1988;37:629–632. [PubMed] [Google Scholar]
- 2.Donally CJ, III, Lawrie CM, Rush AJ, III, et al. The season of hoverboards: a case series of fractures. Pediatr Emerg Care. 2017;33(5):325–328. doi: 10.1097/PEC.0000000000001120. [DOI] [PubMed] [Google Scholar]
- 3.Forsman L, Eriksson A. Skateboarding injuries of today. Br J Sports Med. 2001;35(5):325–328. doi: 10.1136/bjsm.35.5.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fountain JL, Meyers MC. Skateboarding injuries. Sports Med. 1996;22(6):360–366. doi: 10.2165/00007256-199622060-00004. [DOI] [PubMed] [Google Scholar]
- 5.Handbook for public playground safety. Washington DC: US Consumer Product Safety Commission; 1991.
- 6.Kattan AE, AlShomer F, Alhujayri AK, et al. A case series of pediatric Seymour fractures related to hoverboards: increasing trend with changing lifestyle. Int J Surg Case Rep. 2017;38:57–60. doi: 10.1016/j.ijscr.2017.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKenzie LB, Fletcher E, Nelson NG, et al. Epidemiology of skateboarding-related injuries sustained by children and adolescents 5-19 years of age and treated in US emergency departments: 1990-2008. Inj Epidemiol. 2016;3(1):10. doi: 10.1186/s40621-016-0075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Merriam-Webster’s Collegiate Dictionary. 11th ed. Merriam-Webster, Inc; 2003.
- 9.Monteilh C, Patel P, Gaffney J. Musculoskeletal injuries associated with hoverboard use in children. Clin Pediatr. 2017;56(10):909–911. doi: 10.1177/0009922817706143. [DOI] [PubMed] [Google Scholar]
- 10.Powell EC, Tanz RR. In-line skate and rollerskate injuries in childhood. Pediatr Emerg Care. 1996;12(4):259–262. doi: 10.1097/00006565-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Powell EC, Tanz RR. Incidence and description of scooter-related injuries among children. Ambul Pediatr. 2004;4(6):495–499. doi: 10.1367/A04-074R1.1. [DOI] [PubMed] [Google Scholar]
- 12.Robinson T, Agarwal M, Chaudhary S, et al. Pediatric hoverboard injuries: a need for enhanced safety measures and public awareness. Clin Pediatr. 2016;55(11):1078–1080. doi: 10.1177/0009922816664066. [DOI] [PubMed] [Google Scholar]
- 13.Schapiro AH, Lall NU, Anton CG, et al. Hoverboards: spectrum of injury and association with an uncommon fracture. Pediatr Radiol. 2017;47:437–441. doi: 10.1007/s00247-016-3766-9. [DOI] [PubMed] [Google Scholar]
- 14.Sherker S, Cassell E. Preventing in-line skating injuries: how effective are the countermeasures? Sports Med. 1999;28(5):325–335. doi: 10.2165/00007256-199928050-00004. [DOI] [PubMed] [Google Scholar]
- 15.Schieber RA, Branche-Dorsey CM, Ryan GW, et al. Risk factors for injuries from in-line skating and the effectiveness of safety gear. N Engl J Med. 1996;335(22):1630–1635. doi: 10.1056/NEJM199611283352202. [DOI] [PubMed] [Google Scholar]
- 16.Siracuse BL, Ippolito JA, Gibson PD, et al. Hoverboards: a new cause of pediatric morbidity. Injury. 2017;48(6):1110–1114. doi: 10.1016/j.injury.2017.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Sobel AD, Reid DB, Blood TD, et al. Pediatric orthopedic hoverboard injuries: a prospectively enrolled cohort. J Pediatr. 2017;190:271–274. doi: 10.1016/j.jpeds.2017.07.041. [DOI] [PubMed] [Google Scholar]
- 18.Valdez AM. Playing it safe: injury prevention for self-balancing motorized-boards. J Emerg Nurs. 2016;42(3):269–271. doi: 10.1016/j.jen.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Waltzman ML, Shannon M, Bowen AP, et al. Monkeybar injuries: complications of play. Pediatrics. 1999;103(5):e58. doi: 10.1542/peds.103.5.e58. [DOI] [PubMed] [Google Scholar]
- 20.Weingart GS, Glueckert L, Cachaper GA, et al. Injuries associated with hoverboard use: a case series of emergency department patients. West J Emerg Med. 2017;18(6):993–999. doi: 10.5811/westjem.2017.6.34264. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)