Abstract
Background
There is increased emphasis on properly allocating healthcare resources to optimize value within orthopedic surgery. Establishing time to maximal medical improvement (MMI) can inform clinical decision-making and practice guidelines.
Purpose
We sought (1) to evaluate the time to MMI as predicted by commonly used patient-reported outcome measures (PROMs) for evaluation of shoulder stabilization and (2) to evaluate typical time to return to sports and employment following surgery.
Methods
A systematic review of the Medline database was conducted to identify outcome studies reporting sequential follow-up at multiple time points, up to a minimum of 2 years after shoulder stabilization surgery. The included studies examined the outcomes of arthroscopic or open surgical techniques on anterior instability. Clinically significant improvements were evaluated utilizing the minimal clinically important difference specific to each PROM. Secondary outcomes included range of motion, return to sport/work, and recurrent instability.
Results
Ten studies comprising 590 surgically managed cases of anterior shoulder instability were included (78% arthroscopic, 22% open). Clinically significant improvements in PROMs were achieved up to 1 year post-operatively for Rowe, Western Ontario Instability Index (WOSI), American Shoulder and Elbow Surgeons (ASES), and Simple Shoulder Test (SST) scores. For the three most utilized tools (Rowe, WOSI, ASES), the majority of improvement occurred in the first 6 post-operative months. Clinically significant improvements in Constant Score and Oxford Shoulder Instability Score (OSIS) were achieved up to 6 months and 2 years after surgery, respectively. No clinically significant improvements were achieved on the Disabilities of the Arm, Shoulder, and Hand (DASH) tool.
Conclusion
Maximal medical improvement as determined by commonly utilized PROMs occurs by 1 year after operative management of anterior shoulder instability. The DASH tool does not appear to demonstrate a reliable time frame for clinically significant outcome improvement.
Electronic supplementary material
The online version of this article (10.1007/s11420-020-09773-5) contains supplementary material, which is available to authorized users.
Keywords: shoulder dislocation, shoulder stabilization, Latarjet, Bankart, maximal medical improvement, minimal clinically important difference, value
Introduction
Healthcare expenditures in the USA are projected to grow at 5.5% per year until 2026, reaching 19.7% of gross domestic product by that time [9]. Sustainable healthcare delivery has therefore become a key issue, with particular focus on maximizing health outcomes achieved per dollar of cost [7, 37]. In the realm of orthopedic sports medicine, these “health outcomes” refer most often to decreased pain, increased function, and improved quality of life, all of which are commonly assessed via patient-reported outcome measures (PROMs) [10, 16, 43, 45]. An important metric in interpreting PROMs is the minimal clinically important difference (MCID). This value quantifies the smallest change in a given score that patients perceive as beneficial, regardless of whether or not that change is statistically significant [21]. The concept of MCID has been used to establish a timeline until post-operative maximal medical improvement (MMI), or the state when improvement has plateaued, following a number of common ambulatory orthopedic procedures [2, 42, 56]. This knowledge assists clinicians in regulating patients’ post-operative expectations, defining an adequate time for follow-up, and reporting outcomes at clinically relevant intervals while avoiding unnecessary visits.
Orthopedic surgery has been documented as a significant contributor to healthcare expenditures [7, 47]. Glenohumeral instability represents one important subset of that burden [54], and stabilization procedures have a high national incidence at approximately seven per 100,000 person-years [15]. The two mainstays of operative treatment for shoulder instability are soft-tissue reconstruction of the capsulolabral complex, known as Bankart repair, and the Latarjet procedure, which involves coracoid bone transfer to augment a deficient glenoid. While both procedures can be effective, depending on the clinical scenario [4, 22, 55], no study to date has investigated maximal medical improvement in these high-volume surgeries.
The primary goal of this study was to evaluate the time to MMI as predicted by commonly used patient-reported outcome measures (PROMs) for evaluation of shoulder stabilization; the secondary goal was to evaluate typical time to return to sports and employment following surgery. We hypothesized that patients would perceive improvements in functional status up to 1 year post-operatively but not beyond.
Materials and Methods
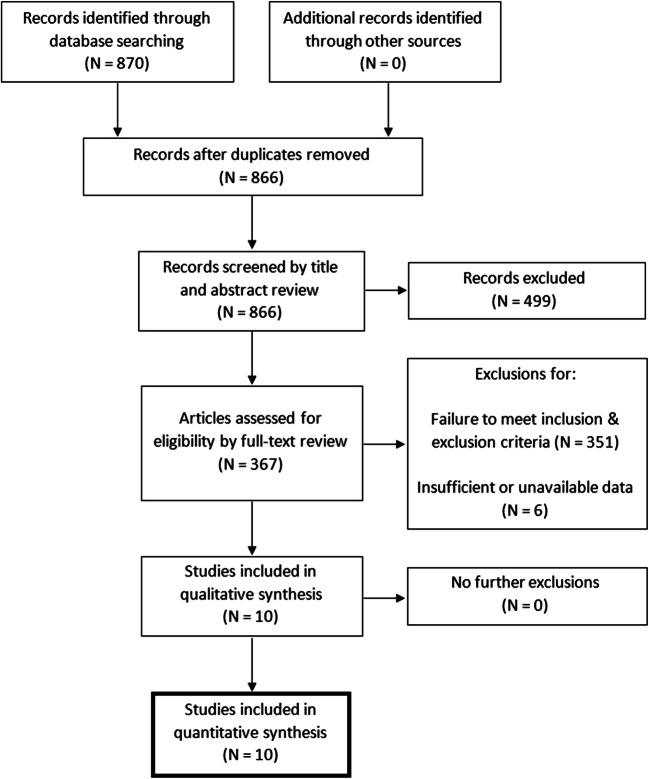
In July 2019, a systematic review of the Medline database was performed using the PubMed interface. The following search terms were used: “((((((WOSI) OR Rowe) OR OSIS) OR Oxford) OR Western Ontario)) AND ((((shoulder stabilization) OR shoulder instability) OR shoulder dislocation) OR shoulder subluxation).” This query returned a total of 870 results. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed, and a PRISMA flow diagram was utilized (Fig. 1). The titles and abstracts of the initially identified articles were screened by two independent reviewers (blinded to reviewers). Full-text review was conducted if (1) the language of publication was English, (2) shoulder stabilization was the primary procedure, (3) the title or abstract mentioned the collection of any clinical outcome at 2-year follow-up or longer, or (4) there was ambiguity regarding outcome reporting. The citations of these articles were also reviewed to identify studies that may not have been captured by the initial search. Upon full-text review, studies were included in this investigation if PROMs were reported at 2 years post-operatively, as well as at least one additional time point prior to 2 years. Articles satisfying this condition and reporting outcome measures at additional time points beyond 2 years were also included. Studies were excluded if they reported on revision shoulder stabilization procedures, reported outcomes at only a single post-operative time point, or did not report outcomes at 2 years post-operatively.
Fig. 1.
PRISMA flow diagram detailing inclusion process for this systematic review.
Data extracted from the selected studies included publication information, details of study design, patient demographics, details of surgical intervention, concomitant injuries, incidence of post-operative complications, and all available patient-reported outcome measures. PROMs that were reported included the following scores: Rowe Score; Western Ontario Shoulder Instability Index (WOSI); Oxford Shoulder Instability Score (OSIS); American Shoulder and Elbow Surgeons Standardized Shoulder Score (ASES); Constant Shoulder Score; Simple Shoulder Test (SST) Score; Disabilities of the Arm, Shoulder, and Hand (DASH) Score and its short form quick-DASH (qDASH) Score; University of California—Los Angeles Shoulder Score (UCLA); Walch–Duplay Score; Single Assessment Numeric Evaluation (SANE); and Short Form Health Survey-12 (SF-12), physical and mental scores. Range of motion (ROM), strength, and return to sport/work (RTS/RTW) data were also extracted when available.
Data Analysis
Data were aggregated and analyzed separately for each measure using techniques previously described to establish time to MMI after rotator cuff repair, anterior cruciate ligament reconstruction, and total shoulder arthroplasty [2, 42, 56]. In brief, reported mean scores were pooled from included studies, and weighted mean and standard deviation were calculated. Clinical outcomes were then compared at the following intervals to quantify the degree of improvement: pre-operative to 6 weeks (or the first time point available in the case of unavailable 6 week data), 6 weeks to 3 months, 6 weeks to 6 months, 3 months to 6 months, 3 months to 1 year, 6 months to 1 year, 6 months to 2 years, and 1 year to 2 years. Additionally, if an included study reported a PROM at only two time points, that metric was not included in data analysis. As noted above, non-consecutive intervals were compared to fully elucidate the time of MMI.
For measures that have established MCID values, a clinically significant improvement was defined as a change in mean outcome score that significantly exceeded the MCID specific to that measure (P < .05). The MCID values utilized in data analysis were as follows: Rowe Score, 9.7 [38]; WOSI, 10.5 [48, 53]; OSIS, 6.0 [51]; ASES, 6.4 [35, 44]; Constant Score, 10.4 [53]; SST, 2.2 [52]; and DASH, 10.2 [44]. Two outcome measures (WOSI and DASH) had multiple reported MCID values in the literature. In the case of WOSI, two authors [48, 53] have reported an MCID of 220/2100 points, or 10.5%, while another investigation [51] has reported an MCID of 14%. For the DASH tool, the MCID has been reported as 10.2, 10.8, and 12.4 by three independent investigations [14, 44, 52]. In these cases, the smallest reported MCID was used for analysis, as this methodology is consistent with the definition of MCID originally described by Jaeschke et al., as “the smallest difference in score […] which patients perceive as beneficial” [21]. Furthermore, as described by Agarwalla et al. and Puzzitiello et al., the use of the smallest available MCID allows for the greatest degree of sensitivity in detecting a significant change in an outcome measure [2, 42].
Clinical significance could not be established for PROMs without previously reported MCIDs for shoulder pathology (UCLA, Walch–Duplay, SANE, and SF-12 scores). For these measures, data was pooled by the same methods as for the other PROMs. However, differences in mean outcome scores were evaluated at the aforementioned intervals without any consideration of MCID. While shoulder-specific MCIDs have been published for the quick-DASH tool [14, 52], this measure was reported by only a single study, at only two time points. Therefore, qDASH was not considered for data analysis.
Statistical Analysis
All statistical analysis was performed utilizing Excel 365 (Microsoft, Seattle, WA, USA). Student’s t tests were used to determine levels of significance for comparisons of PROMs between time points for all analyzed scores (P < .05). The point of MMI was determined by identifying the latest time point at which such a clinically significant improvement occurred and after which further clinically significant improvement was not detected. For objective clinical outcomes including range of motion, strength, RTS/RTW, and post-operative complications, inconsistent techniques for measurement and reporting precluded pooled statistical analysis. Therefore, these results are presented descriptively.
Results
Ten unique studies satisfied inclusion criteria for this review (Table 1). All studies were on anterior shoulder instability. Seven of these (70%) excluded patients with concomitant rotator cuff tears, and the remaining three studies (30%) made no mention of rotator cuff pathology. All studies were prospective in nature. The average time of final follow-up was 2.3 ± 0.6 years, and outcomes were reported at an average of 4.5 ± 1.1 distinct follow-up time points per study. The mean number of distinct PROMs reported per study was 2.8 ± 1.8. Overall, the included studies comprised 616 patients who underwent shoulder stabilization surgery, two of whom had bilateral procedures. Of these 618 surgical shoulders, 590 were included in data reporting by the individual investigations (Table 2).
Table 1.
Characteristics of included studies
| Author | Year | Study designa | LOEb |
|---|---|---|---|
| Edouard [12] | 2010 | Case series | IV |
| Fakih [13] | 2016 | Cohort study | II |
| Gigis [18] | 2014 | Cohort study | II |
| Kemp [25] | 2012 | Case series | IV |
| Koyonos [28] | 2016 | Cohort study | II |
| McRae [34] | 2016 | RCT | II |
| Mohtadi [36] | 2014 | RCT | I |
| Potzl [41] | 2003 | Case series | IV |
| Saier [46] | 2017 | Case series | III |
| Vadala [50] | 2017 | Case series | IV |
LOE level of evidence, RCT randomized controlled trial
aAll studies were designed as prospective investigations
bLOE is presented as reported by the study, or if not reported, as determined by the guidelines of the Oxford Centre for Evidence-Based Medicine
Table 2.
Study characteristics and patient demographics
| Level of evidence (n = 10 studies) | |
| I | 1 (10%) |
| II | 4 (40%) |
| III | 1 (10%) |
| IV | 4 (40%) |
| Mean age (years) | 26.27 ± 3.17 |
| Males | 458 (78%)a |
| Females | 130 (22%)a |
| Mean follow-up (years) | 2.3 ± 0.6 |
| Arthroscopic surgery | 461 (78%) |
| Open surgery | 129 (22%) |
| Bankart repair (n = 546, 92.5%) | |
| Isolated | 438 (80%) |
| + Capsulorrhaphy | 44 (8%) |
| + Capsular plication | 32 (6%) |
| + Remplissage | 32 (6%) |
| Latarjet procedure (n = 44, 7.5%) | |
| Isolated | 44 (100%) |
| Concomitant SLAP lesion (n = 250) | 59 (24%) |
aTwo patients of unspecified gender had bilateral procedures; total n = 590
The Rowe and WOSI scores were reported by five and six studies, respectively, while other measures were available from three or fewer studies each. The greatest number of patients was evaluated by use of WOSI (n = 385), ASES (n = 327), and Rowe (n = 201) scores. Results of interval PROM changes for all measures with reported MCIDs are displayed in Table 3. The latest time point of significant clinical improvement was at 1 year post-operatively for the majority of measures, including Rowe, WOSI, ASES, and SST scores. The majority of improvement in Rowe, WOSI, and ASES appears to occur in the first 6 post-operative months; the 3-month-to-1-year interval was clinically significant while the 6-month-to-1-year interval was not. OSIS demonstrated a clinically significant increase as late as 2 years post-operatively; however, the increase from 1 to 2 years was not significant. The Constant Score significantly improved from pre-operative to 6 months, but not beyond this point. The DASH tool, reported by only a single study, did not demonstrate clinically significant improvements at either of the two intervals available for evaluation. On the basis of these cumulative findings, MMI following shoulder stabilization surgery was determined to occur at 1 year post-operatively.
Table 3.
Interval subjective outcome changes for measures with established MCID values
| Pre-op to 6 weeks | 6 weeks to 3 months | 6 weeks to 6 months | 3 months to 6 months | 3 months to 1 year | 6 months to 1 year | 6 months to 2 years | 1 year to 2 years | |
|---|---|---|---|---|---|---|---|---|
| Rowe (MCID 9.7; n = 201) | ||||||||
| Significant clinical improvement?a | Yes | No | Yes | No | Yes | No | No | No |
| ΔMean | 20.60 | 10.48 | 20.69 | 10.21 | 10.78 | 0.56 | 2.40 | 1.83 |
| P value | < .001 | 0.10 | < .001 | .14 | .001 | > .999 | > .999 | > .999 |
| WOSI (MCID 10.5; n = 385) | ||||||||
| Significant clinical improvement?a | No | Yes | Yes | Yes | Yes | No | No | No |
| ΔMean | 7.48 | 14.51 | 27.02 | 12.51 | 15.95 | 3.43 | 5.61 | 2.18 |
| P value | > .999 | < .001 | < .001 | < .001 | < .001 | > .999 | > .999 | > .999 |
| OSIS (MCID 6.0; n = 77) | ||||||||
| Significant clinical improvement?a | No | No | Yes | Yes | Yes | No | Yes | No |
| ΔMean | − 8.54 | 7.20 | 19.31 | 12.11 | 17.00 | 4.89 | 6.38 | 1.49 |
| P value | > .999 | 0.20 | < .001 | < .001 | < .001 | .86 | < .001 | > .999 |
| ASES (MCID 6.4; n = 327) | ||||||||
| Significant clinical improvement?a | No | – | – | Yes | Yes | No | No | No |
| ΔMean | 5.70b | – | – | 11.05 | 15.37 | 4.32 | 2.83 | − 1.49 |
| P value | .97 | – | – | < .001 | < .001 | > .999 | > .999 | > .999 |
| Constant (MCID 10; n = 155) | ||||||||
| Significant clinical improvement?a | Yes | – | – | – | – | No | No | No |
| ΔMean | 13.02c | – | – | – | – | 6.60 | 6.90 | 0.30 |
| P value | < .001 | – | – | – | – | > .999 | > .999 | > .999 |
| SST (MCID 2.2, n = 34) | ||||||||
| Significant clinical improvement?a | No | – | Yes | – | – | Yes | No | No |
| ΔMean | − 0.81 | – | 4.05 | – | – | 0.28 | − 0.32 | − 0.60 |
| P value | > .999 | – | < .001 | – | – | < .001 | > .999 | > .999 |
| DASH (MCID 10.2, n = 24) | ||||||||
| Significant clinical improvement?a | No | – | – | – | – | – | No | – |
| ΔMean | − 14.00d | – | – | – | – | – | − 11.00 | – |
| P value | > .999 | – | – | – | – | – | > .999 | – |
Dashes indicate intervals for which ΔMean could not be calculated due to unavailability of data at either time point. Italicized text indicates that the later bound of this time interval is the time of maximal medical improvement (MMI)
WOSI Western Ontario Shoulder Instability Index, OSIS Oxford Shoulder Instability Score, ASES American Shoulder and Elbow Surgeon Score, SST Simple Shoulder Test, DASH Disabilities of the Arm, Shoulder, and Hand, MCID minimal clinically important difference, n summed pre-operative enrollment for all studies reporting respective measure
aP < .05 utilized for all statistical comparisons
bThree-month data utilized in place of 6-week data. (Three-month data was the earliest available for ASES.)
cSix-month data utilized in place of 6-week data. (Six-month data was the earliest available for Constant or DASH.)
Measures without established MCID values were used in fewer than 60 patients each. Interval improvements in these PROMs are displayed in Table 4. The UCLA Score demonstrated statistically significant improvements at all analyzed intervals up to 2 years post-operatively. The latest time point for statistically significant improvement for the Walch–Duplay, SANE, SF-12 physical, and SF-12 mental scores was 6 months, 2 years, 1 year, and 3 months, respectively.
Table 4.
Interval subjective outcome changes for measures without established MCID values
| Pre-op to 6 weeks | 6 weeks to 3 months | 6 weeks to 6 months | 3 months to 6 months | 3 months to 1 year | 6 months to 1 year | 6 months to 2 years | 1 year to 2 years | |
|---|---|---|---|---|---|---|---|---|
| UCLA (n = 58) | ||||||||
| Statistically significant improvement?a | Yes | – | Yes | – | – | Yes | Yes | Yes |
| ΔMean | 2.75 | – | 6.43 | – | – | 2.73 | 3.04 | 0.31 |
| P value | < .001 | – | < .001 | – | – | < .001 | < .001 | .01 |
| Walch–Duplay (n = 20) | ||||||||
| Statistically significant improvement?a | Yes | – | – | Yes | – | – | No | – |
| ΔMean | 7.70b | – | – | 23.00 | – | – | 4.80 | – |
| P value | .04 | – | – | < .001 | – | – | .07 | – |
| SANE (n = 34) | ||||||||
| Statistically significant improvement?a | Yes | – | Yes | – | – | No | No | Yes |
| ΔMean | 2.18 | – | 27.82 | – | – | − 1.82 | − 0.53 | 1.29 |
| P value | .004 | – | < .001 | – | – | > .999 | > .999 | < .001 |
| SF-12, physical (n = 53) | ||||||||
| Statistically significant improvement?a | No | Yes | Yes | Yes | Yes | Yes | No | No |
| ΔMean | − 8.27 | 5.62 | 14.58 | 8.96 | 11.38 | 2.42 | − 0.05 | − 2.47 |
| P value | > .999 | < .001 | < .001 | < .001 | < .001 | .03 | .52 | .97 |
| SF-12, mental (n = 53) | ||||||||
| Statistically significant improvement?a | No | Yes | No | No | No | No | No | No |
| ΔMean | − 0.32 | 1.81 | 2.08 | 0.27 | − 1.76 | − 2.03 | − 0.42 | 1.61 |
| P value | .58 | .05 | .06 | .42 | .85 | .88 | .64 | .08 |
Dashes indicate intervals for which ΔMean could not be calculated due to unavailability of data at either time point
UCLA University of California—Los Angeles Shoulder Score, SANE Single Assessment Numeric Evaluation, SF-12 Short Form Health Survey-12, MCID minimal clinically important difference, n summed pre-operative enrollment for all studies reporting respective measure
aP < .05 utilized for all statistical comparisons
bThree-month data utilized in place of 6-week data. (Three-month data was the earliest available for Walch–Duplay.)
Trends in all PROMs over time are displayed in Fig. 2 as a percentage of the maximum possible score. Other than the Short Form tools, all scores demonstrate a decrease in the rate of improvement after the 6-month time point. However, the Short Form surveys are designed such that linear transformation of scores results in a mean of 50 ± 10 based on national population data [49], which is consistent with the results of the present investigation. Only two studies reported any PROM after 2 years post-operatively. Gigis et al. and Potzl et al. both reported the Rowe Score at 3 years, as 87 and 92, respectively. When this 3-year data was pooled and the 2-year to 3-year interval was analyzed by the previously described methods, the difference in mean score was not clinically significant (ΔMean = − 0.03, P > .999).
Fig. 2.
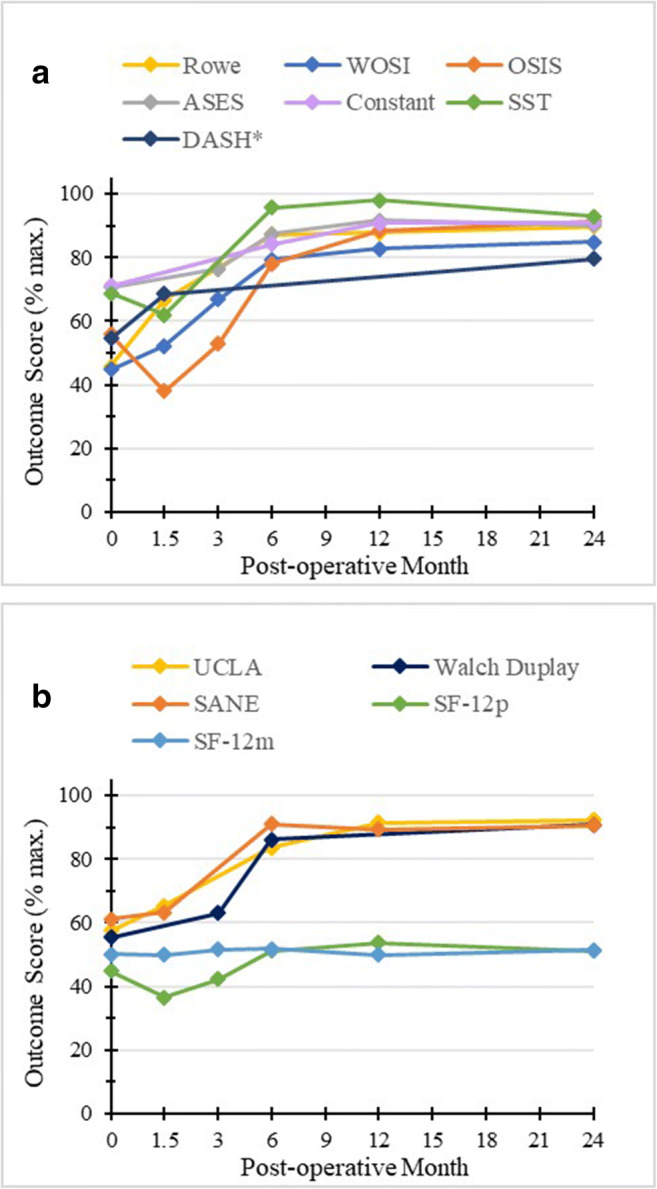
Trends in clinical outcome scores (a) with and (b) without established MCIDs. WOSI Western Ontario Shoulder Instability Index, OSIS Oxford Shoulder Instability Score, ASES American Shoulder and Elbow Surgeon Score, SST Simple Shoulder Test, DASH Disabilities of the Arm, Shoulder, and Hand, UCLA University of California—Los Angeles Shoulder Score, SANE Single Assessment Numeric Evaluation, SF-12 Short Form Health Survey-12. *Lower score on DASH indicates better patient status. This scale was reversed, to display post-operative improvement.
Edouard et al. [12] was the only author to report detailed strength data. In their cohort of 20 Latarjet patients, they found a significant decrease in strength of internal and external rotation (ER) at 3 months post-operatively, when compared to pre-operative scores, as well as 6 and 21 months post-operatively (all P < .05).
Range of motion (ROM) before and after surgery was reported by four included investigations. Fakih et al. [13] reported a mean ER deficit of 9 to 10° vs. the contralateral shoulder (P < .0001) 2 years following Bankart repair with remplissage. In a study on 85 open Bankart repairs, Potzl et al. [41] reported nine instances of deficit in ER 3 years post-operatively (10.6%), seven of which were 10° or greater. Vadala et al. [50] found that all 24 of their Latarjet patients experienced full post-operative recovery of ROM in abduction, flexion, and internal rotation. However, there was a mean deficit of 7° in ER, which the authors postulated was due to the intra-operative vertical tenotomy of the subscapularis. Finally, in a randomized trial comparing open vs. arthroscopic Bankart repair, Mohtadi et al. [36] found that ROM was equivalent in the two groups at 2 years post-operatively.
Data on return to sport/work (RTS/RTW) was available from six studies in total. Four of these [13, 18, 41, 50] reported RTS at the pre-operative level, which occurred in 68 of 90 patients (75.6%). Rate of RTS in the individual studies ranged from 66.7 to 92.6%. A few included investigations provided additional detail regarding the intensity of these sports. Fakih et al. [13] reported RTS in 15 of their 22 patients at the pre-operative level, but that only two of these patients returned to contact sports. Gigis et al. [18] reported RTS in 25 of 27 patients at the pre-operative level, nine to contact sports. Potzl et al. [41] did not report on contact vs. non-contact sports but did state that of 17 high-level overhead athletes, 12 continued at the same or higher level. Additionally, Saier et al. [46] reported that mean time to RTW was 2.0 ± 1.9 months in their analysis of 44 arthroscopic Bankart repairs. The authors stratified this result by level of physicality of occupation and found that RTW occurred at 3.1 ± 2.4 and 1.3 ± 0.9 months in cases of heavy and light physical workload, respectively (P = .002). Lastly, Edouard et al. [12] analyzed the RTS item of the Walch–Duplay Score independently of other measures and found a significant increase in score from 3 to 6 months post-operatively (P < .05) but not at other follow-up intervals.
All ten included studies reported on rates of post-operative instability. In total, data was available for 558 patients, 77 of whom experienced at least one re-dislocation or multiple re-subluxations (13.8%). The rate of recurrent instability ranged from 0% in a 24-patient Latarjet cohort [50] to 23% in an 87-patient cohort of arthroscopic Bankart repairs [36]. Due to heterogeneity in reporting, it was not possible to calculate the mean latency to post-operative instability events. However, five studies explicitly commented on this parameter (Table 5).
Table 5.
Timing of post-operative instability events
| Author | Recurrent instability, n (%) | Timing of events |
|---|---|---|
| Fakih[13] | 2/32 (6.3) | Mean: 17 ± 1.4 months |
| Gigis[18] | 5/38 (13.2) |
Post-op year 1: 0 (0%) Post-op year 2: 2 (40%) Post-op year 3: 3 (60%) |
| Koyonos[28] | 6/28 (21.4) |
Post-op year 1: 3 (50%) Post-op year 2: 3 (50%) |
| Potzl[41]a | 9/85 (10.6) |
Post-op year 1: 3 (33%) Post-op year 2: 3 (33%) Post-op year 7: 1 (11%) |
| Saier[46] | 2/50 (4.0) | > 6 months post-op: 2 (100%) |
aPotzl et al. did not report timing for 2 patients experiencing re-subluxations
Discussion
This review established that patients achieve MMI by 1 year following operative management of anterior shoulder instability, confirming our hypothesis. Interval analysis revealed that the majority of this improvement occurs within the first 6 post-operative months. Additionally, for the vast majority of analyzed PROMs, rate of absolute improvement decreases after this time point. Secondary outcome analysis demonstrated that there may be a post-operative deficit in external rotation of 7 to 11° and that RTS and recurrent instability occurred in 75% and 14% of cases, respectively.
This study is not without limitations. The included articles were heterogeneous in their consideration of concomitant injuries and procedural technique. However, accompanying injuries are common in cases of instability [3, 8] and this breadth may ultimately increase the generalizability of our findings. We included both arthroscopic and open procedures and both Bankart and Latarjet techniques, which provided a broad overview of treatments for shoulder instability, but the time to MMI may be different among these options. Additionally, this review included only two randomized controlled trials, although all studies were designed as prospective investigations, and all analyzed data was collected prospectively, tempering this potential weakness and lending validity to the primary conclusions. Furthermore, data on subjective outcome measures was not available in any study at the 9-month time point. Given the analysis above, this interval is relevant in the recovery of operatively managed instability patients. Consideration of 9-month data could further inform the most efficacious timeline for follow-up and maximal medical improvement. Lastly, analysis of secondary outcomes including range of motion, return to sport/work, and recurrent instability was relatively limited by sparse data and various reporting methodologies. This includes a lack of detailed reporting on complication rates other than post-operative instability, which may be different among the various included procedural techniques (open vs. arthroscopic, Bankart vs. Latarjet).
Our determination of MMI at 1 year post-operatively was largely based on data from the WOSI, Rowe, and ASES measures, which all demonstrated clinical improvement up to, but not beyond, 1 year post-operatively. These measures were the most utilized of all available PROMs in terms of number of patients evaluated, indicating maximal power from the available data. Furthermore, the credibility of these tools has been thoroughly investigated in the shoulder surgery literature. Multiple authors have noted that WOSI was developed specifically to assess shoulder stability, and as such demonstrates the strongest psychometric properties (intra-class correlation coefficient (ICC) 0.87–0.98; effect size 1.67) and has been subject to the most rigorous validation testing [26, 53]. Therefore, it is regarded as the gold standard of instability evaluation [6, 51, 53] and is the PROM most suited for determination of MMI in this circumstance. Though ASES is not specific for instability, it has been validated for this application. Kocher et al. report acceptable test–retest reliability (ICC 0.94), internal consistency (Cronbach’s α 0.61), floor/ceiling effects (0 and 1.3%, respectively), and responsiveness to change (standardized response mean 0.93) [27]. The Rowe Score was developed with older methodology than other PROMs, but it remains the most commonly utilized shoulder score for instability and demonstrates fair reliability (ICC 0.7) and very good responsiveness (effect size 1.2) [53]. Taken together, this information instills a high degree of confidence in the conclusions of the present investigation.
Of note, our analysis also showed that SST demonstrated clinically significant improvements up to 1 year post-operatively, but this result has limited value given SST’s well-documented shortcomings in instability evaluation [6, 19, 53]. Similarly, the Constant Score, which demonstrated clinically significant improvements up to six months post-operatively, is known to provide a poor assessment of stability [11, 26, 53]. Regarding the remaining PROMs with established MCID values, significant improvements in OSIS occurred up to 2 years post-operatively. However, the increase from 1 to 2 years was not significant, and it appears that the majority of improvement occurs prior to 1 year post-operatively. Moreover, this measure was available from only 77 patients across two studies, limiting the reliability of this analysis to some degree. Lastly, we were unable to determine MMI based on the DASH tool, as no clinically significant improvements were achieved. This may be a result of sparse data, as DASH data was available for only 24 patients from a single study. All PROMs without established MCIDs were utilized in fewer than 60 patients, and interpretation of these results is similarly limited. In addition, statistically significant changes in outcome scores may or may not be clinically meaningful [23]. Future research on these outcome measures, including establishment of MCID values, is needed to provide clinicians context for interpretation of post-operative results.
In 2010, Porter et al. criticized the current framework for evaluating value across all healthcare fields. They contended that the most impactful method for appraising efficiency involves measuring cost throughout the relevant care cycle and weighing this burden against appreciable outcomes [40]. Other authors also contend that accurate, valid reporting of outcomes is central to ensuring quality and value in orthopedic care [33]. To that end, our systematic review provides a meaningful time frame for providers and stakeholders to optimize value following operative anterior shoulder stabilization. Follow-up after the time of MMI at 1 year post-operatively may be on the wrong end of this cost–benefit analysis. As the majority of improvement appears to occur within the first 6 post-operative months, this may be the time frame best suited for concentrating strained healthcare resources in the majority of cases.
However, continued follow-up may be warranted in patients at high risk of post-operative recurrence. Several studies included in this review (Table 5) as well as other investigations [5, 24] have reported that recurrent instability may occur at greater than 1 year post-operatively. The Instability Severity Index Score (ISIS) is one tool that can be utilized pre-operatively to identify high-risk patients. Loppini et al. recently found that patients with pre-operative ISIS of 4 to 6 points were at double the risk of recurrence patients with ISIS 3 points or lower (hazard ratio [HR] = 2.43, 95% CI 1.38–4.28, P = .002), and patients with ISIS of more than 6 points were at nine times greater risk of recurrence (HR = 9.42, 95% CI 5.20–17.7, P < .001) [31]. Other risk factors for post-operative failure include more than one pre-operative dislocation event [17], off-track Hill–Sachs lesions [30], and more than 6-month latency between original dislocation and surgery [30]. Moreover, it may be particularly prudent of orthopedic providers to concentrate post-operative resources on these patients; Makhni et al. found that early surgical intervention with arthroscopic revision (incremental cost-effectiveness ratio [ICEFR] = 3082) or Latarjet procedure (ICEFR = 1141) is cost-effective versus prolonged conservative management [32]. Therefore, pre-operative identification of high-risk patients, in conjunction with the MMI timeline established by this review, can aid providers in setting appropriate follow-up schedules that optimize value. Future high LOE investigations on the timing of post-operative recurrent instability would further inform clinical decision-making.
With regard to RTS following shoulder stabilization surgery, timing varies by operative technique. Recent reviews and meta-analyses have found that RTS time ranges from approximately 5 months following Latarjet to 8 months following open Bankart repair. Moreover, these investigations concluded that 65 to 97.5% of operatively managed instability patients return to sports at the pre-injury level [1, 20]. While RTW has not been as thoroughly investigated, existing literature clearly indicates that RTW occurs prior to RTS [4, 29], which is consistent with our findings. Therefore, based on the 1-year point of MMI, it is probable that the majority of patients will continue to experience subjective clinical improvements even after RTS or RTW. In this way, providers can utilize the time frame of MMI to set appropriate post-operative expectations to patients. Ensuring physician–patient congruence with accurate and informed counseling is of particular importance in cases of operative shoulder stabilization, as patients have particularly high pre-operative expectations [39].
In conclusion, on the basis of reliable PROMs, this review establishes that maximal medical improvement occurs at 1 year following operative management of anterior shoulder instability. This provides a concrete and substantial frame of reference for providers and stakeholders to establish appropriate patient expectations and maximize value in post-operative follow-up.
Electronic supplementary material
(PDF 2.17 mb)
Compliance with Ethical Standards
Conflict of Interest
Bhavik H. Patel, BS, Yining Lu, BA, Avinesh Agarwalla, MD, Richard N. Puzzitiello, MD, Benedict U. Nwachukwu, MD, MBA, Gregory L. Cvetanovich, MD, declare that they have no conflicts of interest. Jorge Chahla, MD, PhD, reports being an unpaid consultant to Arthrex, Conmed Linvatec, and Smith & Nephew, outside the submitted work. Brian Forsythe, MD, reports receiving royalties from Elsevier, research support from Arthrex, stock or stock options from Jace Medical, personal fees and research support from Stryker, and fellowship support from Smith & Nephew and Ossur, outside the submitted work.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level IV, systematic review of level I–IV studies
References
- 1.Abdul-Rassoul H, Galvin JW, Curry EJ, Simon J, Li X. Return to sport after surgical treatment for anterior shoulder instability: a systematic review. Am J Sports Med. 2019;47(6):1507–1515. 10.1177/0363546518780934 [DOI] [PubMed]
- 2.Agarwalla A, Puzzitiello RN, Liu JN, et al. Timeline for maximal subjective outcome improvement after anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(10):2501–2509. [DOI] [PubMed]
- 3.Atef A, El-Tantawy A, Gad H, Hefeda M. Prevalence of associated injuries after anterior shoulder dislocation: a prospective study. Int Orthop. 2016;40(3):519–524. doi: 10.1007/s00264-015-2862-z. [DOI] [PubMed] [Google Scholar]
- 4.Bliven KCH, Parr GP. Outcomes of the Latarjet Procedure compared with bankart repair for recurrent traumatic anterior shoulder instability. J Athl Train. 2018;53(2):181–183. doi: 10.4085/1062-6050-232-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boileau P, Villalba M, Hery J, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 6.Booker S, Alfahad N, Scott M, Gooding B, Wallace WA. Use of scoring systems for assessing and reporting the outcome results from shoulder surgery and arthroplasty. World J Orthop. 2015;6(2):244–251. doi: 10.5312/wjo.v6.i2.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Callahan CD, Adair D, Bozic KJ, Manning BT, Saleh JK, Saleh KJ. Orthopaedic surgery under national health reform: an analysis of power, process, adaptation, and leadership: AOA Critical Issues. J Bone Joint Surg Am. 2014;96(13):e111. doi: 10.2106/JBJS.M.01067. [DOI] [PubMed] [Google Scholar]
- 8.Carrazzone OL, Tamaoki MJS, Ambra LFM, Neto NA, Matsumoto MH, Belloti JC. Prevalence of lesions associated with traumatic recurrent shoulder dislocation. Rev Bras Ortop. 2015;46(3):281–287. doi: 10.1016/S2255-4971(15)30196-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services. National Healthcare expenditure projections 2017-2026––forecast summary. 2018. Available from https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/ForecastSummary.pdf. Accessed Nov 1, 2018.
- 10.Chad Mather RC, Bozic KJ. Value-based care. J Shoulder Elbow Surg. 2013;22(12):1599–1600. doi: 10.1016/j.jse.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Am. 1999;81(3):420–426. doi: 10.1302/0301-620x.81b3.9044. [DOI] [PubMed] [Google Scholar]
- 12.Edouard P, Beguin L, Fayolle-Minon I, Degache F, Farizon F, Calmels P. Relationship between strength and functional indexes (Rowe and Walch-Duplay scores) after shoulder surgical stabilization by the Latarjet technique. Ann Phys Rehabil Med. 2010;53(8):499–510. doi: 10.1016/j.rehab.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 13.Fakih R, Hamie M, Yassine M. Comparative study on the management of glenohumeral joint dislocation. Closed reduction vs. arthroscopic remplissage with Bankart lesion repair. J Med Liban. 2016;64(3):175–180. doi: 10.12816/0031528. [DOI] [PubMed] [Google Scholar]
- 14.Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH) J Orthop Sports Phys Ther. 2013;44(1):30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 15.Frank RM, Chalmers PN, Moric M, Leroux T, Provencher MT, Romeo AA. Incidence and changing trends of shoulder stabilization in the United States. Arthroscopy. 2018;34(3):784–792. doi: 10.1016/j.arthro.2017.08.289. [DOI] [PubMed] [Google Scholar]
- 16.Gagnier JJ. Patient reported outcomes in orthopaedics. J Orthop Res. 2017;35(10):2098–2108. doi: 10.1002/jor.23604. [DOI] [PubMed] [Google Scholar]
- 17.Gasparini G, De Benedetto M, Cundari A, et al. Predictors of functional outcomes and recurrent shoulder instability after arthroscopic anterior stabilization. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):406–413. doi: 10.1007/s00167-015-3785-3. [DOI] [PubMed] [Google Scholar]
- 18.Gigis I, Heikenfeld R, Kapinas A, Listringhaus R, Godolias G. Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J Ped Orthop. 2014;34(4):421–425. doi: 10.1097/BPO.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 19.Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: Psychometric properties by age and injury type. J Shoulder Elbow Surg. 2007;16(3):260–267. doi: 10.1016/j.jse.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Ialenti MN, Mulvihill JD, Feinstein M, Zhang AL, Feeley BT. Return to play following shoulder stabilization: a systematic review and meta-analysis. Orthop J Sports Med. 2017;5(9):2325967117726055. doi: 10.1177/2325967117726055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–415. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 22.Jeon YS, Jeong HY, Lee DK, Rhee YG. Borderline glenoid bone defect in anterior shoulder instability: Latarjet procedure versus Bankart repair. Am J Sports Med. 2018;46(9):2170–2176. doi: 10.1177/0363546518776978. [DOI] [PubMed] [Google Scholar]
- 23.Jevsevar DS, Sanders J, Bozic K, Brown GA. An introduction to clinical significance in orthopaedic outcomes research. J Bone Joint Surg Rev. 2015;3(5). [DOI] [PubMed]
- 24.Kavaja L, Lähdeoja T, Malmivaara A, Paavola M. Treatment after traumatic shoulder dislocation: a systematic review with a network meta-analysis. Brit J Sports Med. 2018;52(23):1498–1506. doi: 10.1136/bjsports-2017-098539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kemp KA, Sheps DM, Beaupre LA, Styles-Tripp F, Luciak-Corea C, Balyk R. An evaluation of the responsiveness and discriminant validity of shoulder questionnaires among patients receiving surgical correction of shoulder instability. ScientificWorldJournal. 2012;2012:410125. 10.1100/2012/410125 [DOI] [PMC free article] [PubMed]
- 26.Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI) Am J Sports Med. 1998;26(6):764–772. doi: 10.1177/03635465980260060501. [DOI] [PubMed] [Google Scholar]
- 27.Kocher MS, Horan M, Briggs K, Richardson T, O’Holleran J, Hawkins RJ. Reliability, validity, and responsiveness of the American Shoulder and Elbow Surgeons subjective shoulder scale in patients with shoulder instability, rotator cuff disease, and glenohumeral arthritis. J Bone Joint Surg Am. 2005;87(9):2006–2011. doi: 10.2106/JBJS.C.01624. [DOI] [PubMed] [Google Scholar]
- 28.Koyonos L, Kraeutler MJ, O'Brien DF, Ciccotti MG, Dodson CC. A prospective cohort study investigating the effect of generalized joint hypermobility on outcomes after arthroscopic anterior shoulder stabilization. Phys Sportsmed. 2016;44(4):380–384. 10.1080/00913847.2016.1248225 [DOI] [PubMed]
- 29.Kraus TM, Freude T, Fiedler S, Schroter S, Stockle U, Ateschrang A. Incapacity of work after arthroscopic Bankart repair. Arch Orthop Trauma Surg. 2015;135(10):1429–1436. doi: 10.1007/s00402-015-2288-5. [DOI] [PubMed] [Google Scholar]
- 30.Lee SH, Lim KH, Kim JW. Risk factors for recurrence of anterior-inferior instability of the shoulder after arthroscopic Bankart repair in patients younger than 30 years. Arthroscopy. 2018;34(9):2530–2536. doi: 10.1016/j.arthro.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 31.Loppini M, Delle Rose G, Borroni M, et al. Is the instability severity index score a valid tool for predicting failure after primary arthroscopic stabilization for anterior glenohumeral instability? Arthroscopy. 2019;35(2):361–366. doi: 10.1016/j.arthro.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 32.Makhni EC, Lamba N, Swart E, et al. Revision arthroscopic repair versus latarjet procedure in patients with recurrent instability after initial repair attempt: a cost-effectiveness model. Arthroscopy. 2016;32(9):1764–1770. doi: 10.1016/j.arthro.2016.01.062. [DOI] [PubMed] [Google Scholar]
- 33.Marjoua Y, Butler CA, Bozic KJ. Public reporting of cost and quality information in orthopaedics. Clin Orthop Relat Res. 2011;470(4):1017–1026. doi: 10.1007/s11999-011-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McRae S, Leiter J, Subramanian K, Litchfield R, MacDonald P. Randomized controlled trial of arthroscopic electrothermal capsulorrhaphy with Bankart repair and isolated arthroscopic Bankart repair. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):414–421. 10.1007/s00167-015-3543-6 [DOI] [PubMed]
- 35.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–594. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 36.Mohtadi NGH, Chan DS, Hollinshead RM, et al. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. J Bone Joint Surg Am. 2014;96(5):353–360. doi: 10.2106/JBJS.L.01656. [DOI] [PubMed] [Google Scholar]
- 37.Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316(5):525–532. doi: 10.1001/jama.2016.9797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park I, Lee JH, Hyun HS, Lee TK, Shin SJ. Minimal clinically important differences in Rowe and Western Ontario Shoulder Instability Index scores after arthroscopic repair of anterior shoulder instability. J Shoulder Elbow Surg. 2018;27(4):579–584. doi: 10.1016/j.jse.2017.10.032. [DOI] [PubMed] [Google Scholar]
- 39.Plath JE, Saier T, Feucht MJ, et al. Patients’ expectations of shoulder instability repair. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):15–23. doi: 10.1007/s00167-017-4489-7. [DOI] [PubMed] [Google Scholar]
- 40.Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 41.Pötzl W, Witt KA, Hackenberg L, Marquardt B, Steinbeck J. Results of suture anchor repair of anteroinferior shoulder instability: a prospective clinical study of 85 shoulders. J Shoulder Elbow Surg. 2003;12(4):322–326. doi: 10.1016/s1058-2746(03)00032-6. [DOI] [PubMed] [Google Scholar]
- 42.Puzzitiello RN, Agarwalla A, Liu JN, et al. Establishing maximal medical improvement after anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 27(9):1711–1720. [DOI] [PubMed]
- 43.Ring D, Bozic KJ. Value-based healthcare: the value of considering patient preferences and circumstances in orthopaedic surgery. Clin Orthop Relat Res. 2016;474(3):633–635. doi: 10.1007/s11999-015-4648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roy J-S, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Care & Research. 2009;61(5):623–632. doi: 10.1002/art.24396. [DOI] [PubMed] [Google Scholar]
- 45.Ruzbarsky JJ, Marom N, Marx RG. Measuring quality and outcomes in sports medicine. Clin Sports Med. 2018;37(3):463–482. doi: 10.1016/j.csm.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Saier T, Plath JE, Waibel S, et al. How Satisfied are patients with arthroscopic Bankart repair? A 2-year follow-up on quality-of-life outcome. Arthroscopy. 2017;33(10):1777–1785. [DOI] [PubMed]
- 47.Sathiyakumar V, Jahangir A, Mir H, et al. Patterns of costs and spending among orthopedic surgeons across the United States: a national survey. Am J Orthop (Belle Mead NJ). 2014;43(1):E7–E13. [PubMed] [Google Scholar]
- 48.Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(3):277–285. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Turner-Bowker D, Hogue SJ. Short Form 12 Health Survey (SF-12) In: Michalos AC, editor. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer Netherlands; 2014. pp. 5954–5957. [Google Scholar]
- 50.Vadalà A, Lanzetti RM, De Carli A, et al. Latarjet procedure: evolution of the bone block and correspondent clinical relevance—a clinical and radiological study. Musculoskelet Surg. 2017;101(Suppl 2):113–120. doi: 10.1007/s12306-017-0482-z. [DOI] [PubMed] [Google Scholar]
- 51.van der Linde JA, van Kampen DA, van Beers LWAH, van Deurzen DFP, Saris DBF, Terwee CB. The responsiveness and minimal important change of the Western Ontario Shoulder Instability Index and Oxford Shoulder Instability Score. J Orthop Sports Phys Ther. 2017;47(6):402–410. doi: 10.2519/jospt.2017.6548. [DOI] [PubMed] [Google Scholar]
- 52.van Kampen DA, Willems WJ, van Beers LWAH, Castelein RM, Scholtes VAB, Terwee CB. Determination and comparison of the smallest detectable change (SDC) and the minimal important change (MIC) of four-shoulder patient-reported outcome measures (PROMs) J Orthop Surg Res. 2013;8(1):40. doi: 10.1186/1749-799X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wylie JD, Beckmann JT, Granger E, Tashjian RZ. Functional outcomes assessment in shoulder surgery. World J Orthop. 2014;5(5):623–633. doi: 10.5312/wjo.v5.i5.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92(3):542–549. doi: 10.2106/JBJS.I.00450. [DOI] [PubMed] [Google Scholar]
- 55.Zhu Y, Jiang C, Song G. Arthroscopic versus open latarjet in the treatment of recurrent anterior shoulder dislocation with marked glenoid bone loss: a prospective comparative study. Am J Sports Med. 2017;45(7):1645–1653. doi: 10.1177/0363546517693845. [DOI] [PubMed] [Google Scholar]
- 56.Zuke WA, Leroux TS, Gregory BP, et al. Establishing maximal medical improvement after arthroscopic rotator cuff repair. Am J Sports Med. 2018;46(4):1000–1007. doi: 10.1177/0363546517707963. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 2.17 mb)