Abstract
Background:
Double epidural hematomas (EDHs) have a higher mortality rate compared to single EDHs and same Glasgow Coma Scale (GCS), although double EDHs incidence is less common.
Case Description:
We present the case of a 34-year-old female who underwent single skin incision and frontotemporal and suboccipital craniotomies for fatal traumatic double acute EDHs, then, a literature review was performed.
Conclusion:
Double EDHs in association with low GCS at presentation and traumatic diastasis of cranial sutures or other maxillofacial injuries are associated to an unfavorable outcome.
Keywords: Epidural hematoma, Neurotrauma, Traumatic brain injury

Double epidural hematomas (EDHs) have an overall incidence of 2–9% of all EDHs.[2] EDHs are often the result of a traumatic brain injury (TBI) and have a mortality rate of more than 30%.[8] In patients with double EDHs and Glasgow Coma Scale (GCS) score between 3 and 8, the mortality rate is 47.6% compared to 25% in patients with single EDHs and same GCS.[8] The ipsilateral occurrence of more than 1 EDH is uncommon.
We present the case of a 34-year-old female who underwent single skin incision and frontotemporal and suboccipital craniotomies for fatal traumatic double acute EDHs. Her neurological examination on admission was poor (GCS 7). Computed tomography (CT) scans [Figure 1] revealed two different EDHs, the first one located in the right temporal region and the second one in the right posterior cranial fossa, and a diastasis of the lambdoid suture, suggestive of high-speed impact trauma. The patient underwent surgery in three-quarters prone position. A single C-shaped skin incision starting anteriorly from the right frontal region and ending posteriorly on the middle line until C1 level, passing from the inion, was performed. Then, two different craniotomies, right frontotemporal and right suboccipital, were performed [Figure 2]. The only bleeding vessel found was the dural parietal branch of the posterior division of the middle meningeal artery (MMA). In posterior cranial fossa, we did not find any bleeding vessel. As the posterior meningeal artery was not affected by bone fracture and the transverse sinus was intact, we thought that this posterior fossa EDH arose from occipital diploic veins. The postoperative CT scan showed complete removal of both hematomas [Figure 1], but unfortunately, the patient died 2 days later due to diffuse axonal injury (DAI). When possible, a single skin incision, which allows doing more than 1 craniotomy, can make surgical evacuation faster and safer.
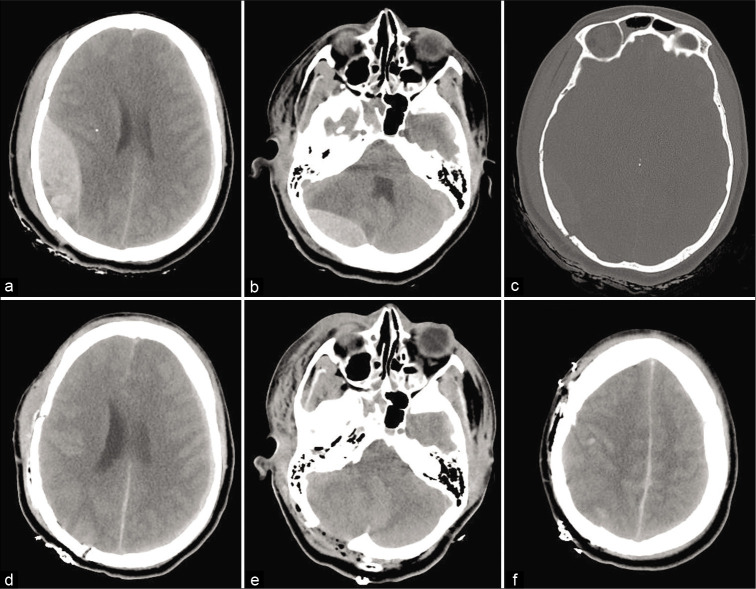
Figure 1:
Preoperative noncontrast CT head scans show a right temporal epidural hematomas (EDHs) (a), a right posterior cranial fossa EDH (b), and a temporal bone fracture with diastasis of the lambdoid suture (c). Postoperative CT head scans (d-f) show evacuation of EDHs and resolution of the downward herniation.
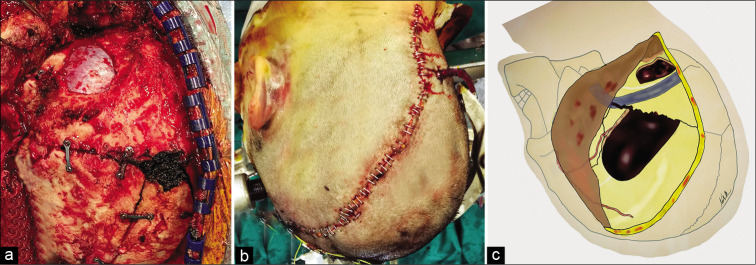
Figure 2:
Intraoperative (a) and postoperative (b) pictures show two different craniotomies and a single C-shaped skin incision starting from the right frontal region and ending to C1 level. Illustration depicting (c) shows the middle meningeal artery, transverse and sigmoid sinuses, and the craniotomies performed during surgery.
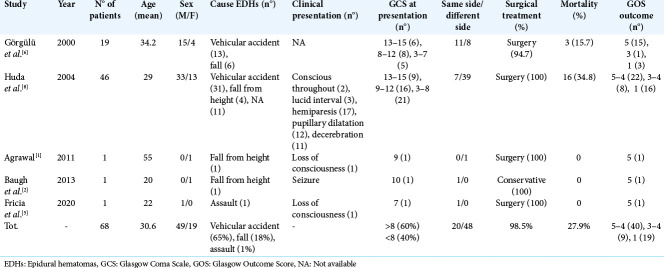
From a literature review, 68 cases were found with double EDHs.[1,2,5,6,8] Median age was 30.6 years with a higher incidence in men (72%). Vehicular accidents represent the most common cause (65%) of double EDHs, whose GCS at presentation is less than 8 in 40% of cases. Just one patient was treated conservatively. Overall mortality was 27.9%. [Table 1] shows all details.
Table 1:
Review of acute traumatic double epidural hematomas.
EDHs arise from injury to the MMA or from its terminal arterial branches in about 55% of the patients, from the middle meningeal vein in 30% of cases and from diploic veins or a torn dural venous sinus in the remaining 15% of cases.[8] Posterior fossa EDHs are rare in association with other EDHs and represent about the 4–7% of the cases of all EDHs. This rare condition is rapidly fatal, because of limited space in posterior cranial fossa.[3] Unlike supratentorial EDHs, where the source of bleeding is usually the MMA, posterior cranial fossa EDHs have a venous origin in 85% of the cases and usually develop as a result of injury to the transverse or sigmoid sinuses secondary to a linear occipital bone fracture or a diastatic lambdoid fracture.[7] In particular, when a diastasis of the lambdoid suture is present, EDHs are typically associated with complicated venous sinus injuries and uncontrollable bleeding.[7] However, in our case, no injury of the sigmoid sinus nor transverse sinus was found and the bleeding was easily controlled with hemostatic agents.[9] However, a diastatic fracture of the lambdoid suture potentially represents itself a cause of instant death and it is associated to an unfavorable outcome.[7] Huda et al.[8] reported a mortality rate 4 times higher in patients with double EDHs compared to patient with single EDHs. Double EDHs can be the result of a coup injury occurring under the site of impact in addition to a contrecoup injury occurring on the posterior fossa, whereas DAI, due to rapid acceleration-deceleration of the head, causes both stretching and compression of the brain tissue, resulting in a poor clinical outcome despite early surgical evacuation of double EDHs.[10]
The authors hope this case report and literature review could increase the awareness of the fatal consequences of double EDH associated with diastasis of the lambdoid suture. Double EDHs in association with low GCS at presentation and traumatic diastasis of cranial sutures or other maxillofacial injuries lead to a poor prognosis. This paper confirms what it is strongly recommended, that is, surgical evacuation as soon as possible in patients with acute single or double EDHs with a GCS score <9.[4] Double EDHs are the result of a severe TBI with distinct presentation and high morbidity and mortality.
Footnotes
How to cite this article: Montemurro N, Santoro G, Marani W, Petrella G. Posttraumatic synchronous double acute epidural hematomas: Two craniotomies, single skin incision. Surg Neurol Int 2020;11:435.
Contributor Information
Nicola Montemurro, Email: nicola.montemurro@unipi.it.
Giorgio Santoro, Email: giorgio8480@gmail.com.
Walter Marani, Email: wmarani10@gmail.com.
Giandomenico Petrella, Email: gdpetrella@gmail.com.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Agrawal A. Bilateral symmetrical parietal extradural hematoma. J Surg Tech Case Rep. 2011;3:34–6. doi: 10.4103/2006-8808.78469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baugh AD, Baugh RF, Atallah JN, Gaudin D, Williams M. Craniofacial trauma and double epidural hematomas from horse training. Int J Surg Case Rep. 2013;4:1149–52. doi: 10.1016/j.ijscr.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benedetto N, Gambacciani C, Montemurro N, Morganti R, Perrini P. Surgical management of acute subdural haematomas in elderly: Report of a single center experience. Br J Neurosurg. 2017;31:244–8. doi: 10.1080/02688697.2016.1244249. [DOI] [PubMed] [Google Scholar]
- 4.Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al. Surgical management of acute epidural hematomas. Neurosurgery. 2006;58(Suppl 3):S7–15. [PubMed] [Google Scholar]
- 5.Fricia M, Umana GE, Scalia G, Raudino G, Passanisi M, Spitaleri A, et al. Posttraumatic triple acute epidural hematomas: First report of bilateral synchronous epidural hematoma and a third delayed. World Neurosurg. 2020;133:212–5. doi: 10.1016/j.wneu.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Görgülü A, Cobanoglu S, Armagan S, Karabagli H, Tevrüz M. Bilateral epidural hematoma. Neurosurg Rev. 2000;23:30–3. doi: 10.1007/s101430050028. [DOI] [PubMed] [Google Scholar]
- 7.Holzschuh M, Schuknecht B. Traumatic epidural haematomas of the posterior fossa: 20 new cases and a review of the literature since 1961. Br J Neurosurg. 1989;3:171–80. doi: 10.3109/02688698909002792. [DOI] [PubMed] [Google Scholar]
- 8.Huda MF, Mohanty S, Sharma V, Tiwari Y, Choudhary A, Singh VP. Double extradural hematoma: An analysis of 46 cases. Neurol India. 2004;52:450–2. [PubMed] [Google Scholar]
- 9.Montemurro N, Murrone D, Romanelli B, Ierardi A. Postoperative textiloma mimicking intracranial rebleeding in a patient with spontaneous hemorrhage: Case report and review of the literature. Case Rep Neurol. 2020;12:7–12. doi: 10.1159/000505233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ng SY, Lee AY. Traumatic brain injuries: Pathophysiology and potential therapeutic targets. Front Cell Neurosci. 2019;13:528. doi: 10.3389/fncel.2019.00528. [DOI] [PMC free article] [PubMed] [Google Scholar]