Abstract
Objective
We aimed to explore anxiety status across a broad range of HCWs supporting patients with COVID-19 in different global regions.
Method
This was an international online survey in which participation was on voluntary basis and data were submitted via Google Drive, across a two-week period starting from March 18, 2020. The Beck Anxiety Inventory was used to quantify the level of anxiety.
Results
1416 HCWs (70.8% medical doctors, 26.2% nurses) responded to the survey from 75 countries. The distribution of anxiety levels was: normal/minimal (n = 503, 35.5%), low (n = 390, 27.5%); moderate (n = 287, 20.3%), and severe (n = 236, 16.7%). According to multiple generalized linear model, female gender (p = 0.001), occupation (ie, being a nurse dealing directly with patients with COVID-19 [p = 0.017]), being younger (p = 0.001), reporting inadequate knowledge on COVID-19 (p = 0.005), having insufficient personal protective equipment (p = 0.001) and poor access to hand sanitizers or liquid soaps (p = 0.008), coexisting chronic disorders (p = 0.001) and existing mental health problems (p = 0.001), and higher income of countries where HCWs lived (p = 0.048) were significantly associated with increased anxiety.
Conclusions
Front-line HCWs, regardless of the levels of COVID-19 transmission in their country, are anxious when they do not feel protected. Our findings suggest that anxiety could be mitigated ensuring sufficient levels of protective personal equipment alongside greater education and information.
Keywords: SARS-CoV-2, Coronavirus disease, Protective personal equipment, Workers health, Pandemics
1. Introduction
Thousands of healthcare workers (HCWs) around the world have contributed to the augmented response needed to tackle the coronavirus disease (COVID-19) pandemic. The demand to healthcare systems has increased globally and providing an adequate response has involved HCWs in many cases working long hours under often stressful conditions with limited resources. In addition, front-line HCWs experienced shortage of protective personal equipment (PPE), which could have exposed them to a higher risk of contracting the infection during their working hours even in the most developed countries. COVID-19 contamination was also a concern of potentially transmitting the virus to their families and loved ones [1]. There have been reports of HCWs being quarantined at healthcare facilities unable to return home [2]. Information regarding the transmission, the PPEs required, the treatment algorithms can be confusing, contradicting, and rapidly changing: in one article HCWs reported an even higher level of stress and potentially anxiety in the face of an increasing number of COVID-19 cases and the absence of specific treatment algorithms and without being able to provide the care deemed essential [3]. The leadership has frequently responded late to the needs and challenges of those providing the response at the frontline and thus, the governments have been urged to arrange mental health support for frontline medical staff [4]. These and other factors may have placed physical and psychological stresses on HCWs, but the extent to which HCWs are affected is yet to be fully elucidated.
Previous studies showed severe consequences for the mental health of HCWs responding to outbreaks of infection, these included significant psychological distress both during and after the epidemic [[5], [6], [7]]. It was shown that HCWs were 2 to 3 times more likely to have posttraumatic stress (PTS) symptoms when quarantined, located in high-risk areas such as the severe acute respiratory syndrome (SARS) wards or had friends and relatives that had contacted SARS during the SARS outbreak in China [5]. Currently, data are still limited on the risk factors linked to mental health problems in HCWs working in a pandemic and for the evidence on how best to protect the mental health of HCWs during acute outbreaks [8]. These are crucial because when identified could guide the development of effective preventive and interventional strategies. Hence, the health leaders will identify, which HCWs may be disproportionately affected and require more targeted interventions.
We therefore conducted an international online survey to determine the level of anxiety among HCWs and to investigate its individual and health system-related predictors in different settings and regions. We aimed to rapidly contribute to new evidence in order to best support the mental health of HCWs globally and to draft potential conclusions and guidance for future studies and research and for planning now and in the long-term.
2. Methods
2.1. Ethical consent
Ethical consent was obtained from the ……….University School of Medicine, ……..(2020/0229).
2.2. Development and dissemination of the instrument
We designed an online structured survey (Appendix) with input from the project advisory group. Beck Anxiety Inventory was already available and in use in all three languages in which survey was disseminated. For the rest of the survey, the questions were prepared in English, Italian, and Turkish, and it was tested before being released among the authors for language and content. The translation was done according to standard methods for health-related questionnaires for use in multinational clinical trials which involved forward and back translation [9]. The survey was made of 3 main parts (Supplementary material):
-demographics (age, gender, nationality, etc.)
- Beck Anxiety Inventory which had been validated in various manuscripts and cultures to measure the level of anxiety.
-correlation questions to establish potential causes of the measured level of anxiety.
2.3. Data collection
We implemented a two-week survey conducted through the Infectious Diseases International Research Initiative (ID-IRI) starting from March 18, 2020. ID-IRI is an international platform with 1028 members in e-mail group, 482 in a WhatsApp® list which serves as a network for clinical research on infectious diseases and clinical microbiology (https://infectdisiri.com./). The survey was anonymous and distributed using direct invites to the ID-IRI members and relevant colleagues. In addition, authors of the study used their own social networks and targeted HCWs, particularly nurses and clinicians of any grade and in any setting with the use of a snowballing technique [10,11]. The survey took 10 min to complete online. Participants consented to participating in the research by completing the survey, and an introductory letter highlighted these consenting procedures and plans for the dissemination of results. A follow-up email was sent to non-responders. Participation in the survey was on the voluntary basis and the data were submitted via Google Drive.
2.4. Measurements
The primary outcome of the study was to detect the cardinal parameters leading to anxiety in HCWs serving to COVID-19 patients. The Beck Anxiety Inventory (BAI) [12] was used to quantify the level of anxiety of respondents. This 21-item instrument designed to assess level of anxiety has been shown to be applicable for the general population [[13], [14], [15], [16]]. The questions pertained to physical, emotional and cognitive aspects of anxiety and fear of losing control that the subject had faced the previous week. Each item is rated on a four-point Likert scale ranging from 0 = not at all to 3 = severe. The total score ranged from 0 to 63. Score of 0–7 are categorized as normal/minimal anxiety, 8–15 as mild anxiety, 16–25 as moderate anxiety, and 26–63 as severe anxiety [17].
2.5. Data analysis
Questions pertained to the respondent's region/country of origin, age, gender, the population of the city where the HCWs live, the health-care center where they work (primary, secondary, or referral centers), occupation, specialty, knowledge about COVID-19, the extent to which the respondent felt that they had access to adequate PPE in their workplace, their roles in managing patients, and precautions taken to prevent COVID-19 transmission in the workplace, and their own personal history of chronic illness, drug use, coexisting psychiatric illnesses. In addition, we collated the BAI scores of all responding HCWs.
2.6. Statistical analysis
Descriptive values were computed as median (IQR: Interquartile Range) for continuous variables and frequencies (n, %) for categorical variables. Kolmogorov-Smirnov test was used for normality assumption. Internal consistency between responses to the BAI questions were investigated by using coefficient of Cronbach's alpha. The differences between the categories of the predictor variables with regard to BAI score were compared by using One-Way ANOVA model. In order to find out exactly which categories were different from each other, post hoc Tukey HSD test which will allows us to explore the difference between multiple group means while also controlling for the family-wise error rate was used. Together with the factors that were found to have a statistically significant correlation with BAI on univariate analysis, variables that were clinically important were also included in the generalized linear model. The relation between the BAI score and continuous variables were evaluated by Pearson correlation analysis. Type I error was accepted as 0.05 and all statistical analysis were done in SPSS (version 22).
3. Results
During the study period, 1416 HCWs responded to the survey from 75 countries, with 75.9% living in high-income, 20.6% in upper-middle income, 3.5% in lower-middle income (3.3% in lower-middle income +0.2% in low-income) economies. Out of responders 1101 (77.7%) worked in Europe, 139 (9.8%) in Americas, 120 (8.5%) in Asia, 41(2.9%) in Australia and 15 (1.1%) in Africa (full data reported in supplementary Table). Response rate was 40% to direct ID-IRI email and WhatsApp® list which represented the 40% of the total sample. The remaining was completed using a link to the ID-IRI platform from the social networks of the authors of the study, where the response rate was 80%.
The median age (IQR) of the respondents was 39 years (32–47 years), and 967 (68.3%) were females. Of the 1416 participants, 1002 (70.8%) were medical doctors, 371 (26.2%) were nurses and 43 (3.0%) were other HCWs (ambulance services, nursing assistants, paramedics, pharmacists, midwifes, radiographers, dentists). Descriptive values for BAI scores and other numerical variables are presented in Table 1 . Categorical demographic variables are presented in the Table 2 . The distribution of the respondents professional expertise was as follows: Intensive care (n = 299, 21.1%), infectious diseases (n = 153, 10.8%), general practitioner (n = 114, 8%), surgery (n = 81, 5.7%), internal medicine (n = 77, 5.4%), diagnostics (n = 36, 2.5%), hemato-oncology (n = 30, 2.1%), pediatrics (n = 33, %), emergency medicine (n = 23, 1.6%), pulmonary diseases (n = 10, 0.7%), and others (n = 136, 9.6%). The median period of time the respondent had been working as a HCW was 12 years (7–20 years).
Table 1.
Descriptive values the participants and the countries.
| Your age | What is the number of confirmed COVID-19 cases in your country so far? | What is the current number of cases died of COVID 19 in your country? | How long have you been in medical service? (years) | BAI Score | ||
|---|---|---|---|---|---|---|
| N RESPONDENTS | 1416 | 1416 | 1416 | 1413 | 1416 | |
|
Percentiles |
25th | 32.0 | 1205.0 | 12.0 | 7.0 | 5.0 |
| Median | 39.0 | 1872.0 | 30.0 | 12.0 | 11.0 | |
| 75th | 47.0 | 5683.0 | 280.0 | 20.0 | 21.0 | |
BAI: Beck Anxiety Inventory.
Table 2.
Relationships between categorical demographic variables and Beck Anxiety Inventory.
| Variables | BAI score |
|||||
|---|---|---|---|---|---|---|
| N | Mean | Standard Deviation | Fdf1, df2⁎ | P | ||
| Gender | Male | 449 | 9.64 | 9.25 | 109.71, 1414 | 0.0001 |
| Female | 967 | 16.29 | 11.87 | |||
| The population of the city you live in | <10.000 | 69 | 17.81a | 12.87 | 6.583, 1412 | 0.0001 |
| 10.000–100.000 | 294 | 16.05a | 11.98 | |||
| 100.000–1.000.000 | 494 | 13.63b | 10.46 | |||
| >1.000.000 | 559 | 13.23b | 11.83 | |||
| The health care center where you work in | Primary care | 340 | 17.05a | 12.25 | 14.103, 1412 | 0.0001 |
| Secondary care | 275 | 15.42a | 11.65 | |||
| Tertiary care | 733 | 12.45b | 10.73 | |||
| Other | 68 | 13.49b | 12.28 | |||
| Occupation | Medical Doctor | 1002 | 13.28a | 11.06 | 12.492, 1413 | 0.0001 |
| Nurse | 371 | 15.96b | 12.14 | |||
| Other⁎ | 43 | 19.63c | 13.50 | |||
| Specialty (for medical doctors) | Diagnostics | 36 | 11.11a | 12.37 |
6.1710, 981 |
0.0001 |
| Emergency Medicine | 23 | 13.26a | 10.18 | |||
| General Practitioner | 114 | 18.76b | 11.38 | |||
| Hemato-Oncology | 30 | 16.83ab | 10.58 | |||
| Infectious Diseases | 153 | 10.71a | 10.81 | |||
| Internal medicine | 77 | 15.09ab | 10.54 | |||
| Intensive Care | 299 | 11.21a | 10.46 | |||
| Pediatrics | 33 | 17.33ab | 12.04 | |||
| Pulmonary diseases | 10 | 16.00ab | 12.80 | |||
| Surgery | 81 | 14.10ab | 11.71 | |||
| Other | 136 | 13.28a | 9.79 | |||
a: statistically significant from each other, b: statistically significant from each other, c: statistically significant from each other,
ab: a and b statistically similar, BAI: Beck Anxiety Inventory, Other: Ambulance services, nursing assistant, paramedic, pharmacist, midwife, radiographer, dentist.
: One-Way ANOVA followed by Post-Hoc Tukey HSD test; df1: degrees of freedom for groups, df2: degrees of freedom for error.
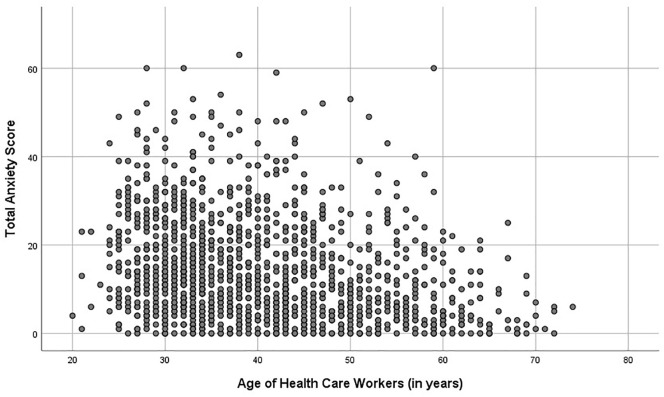
The distribution of anxiety levels in 1416 HCWs were as follows: Normal/minimal (n = 503, 35.5%), low (n = 390, 27.5%); moderate (n = 287, 20.3%), and severe (n = 236, 16.7%). The reliability coefficient (Cronbach's alpha) of the 21-item Anxiety scale was found to be 0·936, highlighting that internal consistency was high. Our data show that BAI scores decreased significantly with older age of the HCW (r = −0.300, p = 0.0001). Before the model-building strategy, a scatter plot was drawn between age and total BAI score. A linear decrease trend was observed in the relationship between age and BAI score (Fig. 1 ). Similarly, those who had been in the medical profession for a greater length of time were reported to experience lower levels of anxiety (r = −0.245, p = 0.0001). No correlation was found between the number of confirmed COVID-19 cases in their country of work and levels of anxiety (r = −0.034, p = 0.202). BAI scores significantly increased with higher income levels of the countries which they live in p < 0.001.
Fig. 1.
The relationship between age and BAI score.
There was no correlation between the number of patients who had died of COVID-19 in the respondents' country at the time of the survey (March 2020) and their BAI scores (r = −0.023, p = 0.381) (Table 1). Data on the respondents history of chronic illness, drug use, coexisting psychiatric illnesses and role in the management of COVID-19 patients and their perceptions on the preventive measures for COVID-19 outbreak and their correlations to BAI scores are presented in Table 3 , and highlight that most of the HCWs 1190 (84%) did not live alone at their homes, 464 (32.7%) were using regular medications, 375 (26.5%) were living with people with chronic diseases, 329 (23.2%) had chronic illnesses, 185 (13.1%) were living with people >60 years of age in their households, 96 (6.7%) had coexisting psychiatric disorders.
Table 3.
Anxiety related to personal issues for the health care workers.
| Variables | BAI Score | |||||
|---|---|---|---|---|---|---|
| Home sharing status/I live with… | N | Mean | SD | Fdf1, df2⁎ | P | |
| None | 1190 | 14.09 | 11.50 | 0.3931, 1414 | 0.531 | |
| Alone | 226 | 14.62 | 11.64 | |||
| None | 1067 | 14.25 | 11.78 | 0.1891, 1414 | 0.663 | |
| My spouse /partner | 349 | 13.95 | 10.71 | |||
| None | 751 | 14.71 | 11.23 | 3.4021, 1414 | 0.065 | |
| My spouse/partner, children | 665 | 13.58 | 11.83 | |||
| None | 1380 | 14.11 | 11.51 | 2.1731, 1414 | 0.141 | |
| My children | 36 | 16.97 | 11.98 | |||
| None | 1378 | 14.21 | 11.59 | 0.3731, 1414 | 0.542 | |
| A flatmate/s | 38 | 13.05 | 8.94 | |||
| None | 1312 | 13.97 | 11.47 | 5.8191, 1414 | 0.016 | |
| My parents | 104 | 16.80 | 11.90 | |||
| A person > 60 years in the household | None | 1231 | 14.07 | 11.20 | 0.7781, 1414 | 0.378 |
| Yes | 185 | 14.88 | 13.49 | |||
| Do you have any chronic illness? | None | 1087 | 13.65 | 11.11 | 9.9281, 1414 | 0.002 |
| Yes | 329 | 15.93 | 12.65 | |||
| Is there a drug that you use regularly? | None | 952 | 13.54 | 11.04 | 8.9471, 1414 | 0.003 |
| Yes | 464 | 15.49 | 12.37 | |||
| Do you have any psychiatric illness? | None | 1320 | 13.57 | 11.05 | 57.241, 1414 | 0.0001 |
| Yes | 96 | 22.60 | 14.32 | |||
| Are there people with chronic diseases in your household? | None | 1041 | 13.75 | 11.07 | 5.3531, 1414 | 0.021 |
| Yes | 375 | 15.36 | 12.64 | |||
|
What is your role in managing patients with COVID-19? |
Indirect role | 662 | 14.95 | 11.81 | 5.6341, 1414 | 0.018 |
| Clinician dealing with patients with COVID-19 | 754 | 13.50 | 11.23 | |||
| None | 1300 | 14.35 | 11.61 | 3.4511, 1414 | 0.063 | |
| Clinician dealing with patients without COVID-19 | 116 | 12.28 | 10.30 | |||
| None | 1131 | 13.52 | 11.17 | 18.591, 1414 | 0.0001 | |
| Nurse dealing with patients with COVID-19 | 285 | 16.79 | 12.51 | |||
| None | 1239 | 14.07 | 11.61 | 0.9041, 1414 | 0.342 | |
| Diagnostic issues | 177 | 14.95 | 10.90 | |||
| None | 1192 | 14.47 | 11.55 | 4.8221, 1414 | 0.028 | |
| Managerial role | 224 | 12.63 | 11.27 | |||
| None | 1315 | 14.27 | 11.53 | 1.0811, 1414 | 0.299 | |
| Public-health management | 101 | 13.03 | 11.48 | |||
| None | 1399 | 14.17 | 11.54 | 0.0751, 1414 | 0.784 | |
| Nurse serving to patients non COVID-19 | 17 | 14.94 | 9.97 | |||
| None | 1332 | 14.08 | 11.44 | 1.7891, 1414 | 0.181 | |
| Other | 84 | 15.81 | 12.77 | |||
| Do you think you have enough knowledge about COVID-19? | No | 387 | 17.44a | 11.50 | 40.572, 1413 | 0.0001 |
| Yes | 692 | 11.49c | 11.06 | |||
| Unsure | 337 | 15.96a | 11.19 | |||
| Sufficient personal protective equipment at your hospital | No | 906 | 15.98 | 11.49 | 64.221, 1414 | 0.0001 |
| Yes | 510 | 10.98 | 10.87 | |||
| Is hand sanitizer or liquid soap available in your hospital? | No | 330 | 17.46 | 12.23 | 35.681, 1414 | 0.0001 |
| Yes | 1086 | 13.18 | 11.12 | |||
| Do you think if you have taken enough precautions to prevent yourself from COVID-19? | No | 223 | 17.86 | 12.21 | 42.712, 1413 | 0.0001 |
BAI: Beck Anxiety Inventory.
: One-Way ANOVA followed by Post-Hoc Tukey HSD test; df1: degrees of freedom for groups, df2: degrees of freedom for error.
The univariate analysis (Table 2, Table 3) showed that anxiety was significantly more common when HCWs faced (p < 0.05 for all): (1) lack of updated information (HCWs felt they had inadequate knowledge on COVID-19) (2) HCWs working in primary or secondary care settings; medical doctors serving as general practitioners compared to specialists; nurses compared to medical doctors; medical staff with less work experience); HCWs dealing directly with severely ill COVID-19 (direct exposure and workload), (3) insufficient medical supplies (PPE, disinfectants, liquid soaps), (4) family concerns (HCWs living with their parents, people with chronic diseases in their households), (5) coexisting medical problems (HCWs with chronic illnesses, psychiatric problems, receiving regular medications), (6) the feeling of absence of the sufficient precautions to prevent themselves, (7) living in relatively small cities, and (8) being a female HCW.
According to multiple generalized linear model (Table 4 ) female gender (p = 0.001), occupations (nurses and support staff) (p = 0.009), being a nurse serving to patients with COVID-19 (p = 0.017), reporting inadequate knowledge on COVID-19 (p = 0.005), having insufficient personal protective equipment (p = 0.001), having insufficient sanitizers or liquid soaps (p = 0.008), and coexisting chronic disorders (p = 0.001) and psychological problems (p = 0.001) were associated with increased anxiety. Moreover, BAI score decreased with increasing age (p = 0.001) and when the age increases by 1 year, the BAI score seemed to decrease by 0.216 point. Older age and greater length of time in the medical profession were not collinear. The correlation between older age and greater length of time in the medical profession was r = 0.882. R-squares did not change when the run time was removed from the model (2nd P column) P values also showed slight changes, i.e. they changed insignificantly. BAI score increased with increasing income levels of countries where they live in (p = 0.048).
Table 4.
Multiple generalized linear model analysis indicating high Beck Anxiety Inventory.
| Risk Factors | Risk category | Reference category | B | Std. Error | 95% Confidence Interval |
P⁎ | P⁎⁎ | |
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Gender | Male | Female | −4.160 | 0.636 | −5.407 | −2.912 | <0.001 | <0.001 |
| The health care center you work in | Primary care | Other | 0.905 | 1.397 | −1.834 | 3.645 | 0.517 | 0.228 |
| Secondary care | 0.419 | 1.422 | −2.371 | 3.208 | 0.768 | |||
| Tertiary care | −0.561 | 1.346 | −3.200 | 2.079 | 0.677 | |||
| Occupation | Medical Doctor | Other | −4.852 | 1.739 | −8.262 | −1.441 | 0.005 | 0.009 |
| Nurse | −5.472 | 1.852 | −9.105 | −1.839 | 0.003 | |||
| Living with the parents | None | My parents | −0.521 | 1.125 | −2.729 | 1.686 | 0.636 | 0.636 |
| Perception to inadequate knowledge about COVID-19 | No | Unsure | 0.870 | 0.780 | −0.661 | 2.401 | 0.265 | 0.005 |
| Yes | −1.414 | 0.717 | −2.817 | −0.010 | 0.049 | |||
| Insufficient personal protective equipment in the hospital | No | Yes | 2.411 | 0.639 | 1.156 | 3.665 | <0.001 | <0.001 |
| Insufficient sanitizers or liquid soaps sufficient in the hospital | No | Yes | 1.841 | 0.696 | 0.476 | 3.206 | 0.008 | 0.008 |
| Being a clinician serving to patients with COVID-19 | No | Yes | −1.279 | 0.778 | −2.806 | 0.247 | 0.096 | 0.096 |
| Being a nurse serving to patients with COVID-19 | No | Yes | −2.949 | 1.233 | −5.368 | −0.530 | 0.017 | 0.017 |
| Having a chronic illness | No | Yes | −3.051 | 0.826 | −4.671 | −1.431 | <0.001 | <0.001 |
| Using medications regularly | No | Yes | 0.503 | 0.771 | −1.009 | 2.015 | 0.514 | 0.514 |
| Having coexistent psychiatric illnesses | No | Yes | −5.817 | 1.162 | −8.097 | −3.537 | <0.001 | <0.001 |
| [Having people with chronic diseases in the household | No | Yes | −0.756 | 0.669 | −2.069 | 0.556 | 0.258 | 0.255 |
| Income levels for country | Lower-Middle + Low | High | −0.818 | 0.746 | −0.818 | 0.746 | 0.273 | 0.048 |
| Upper-Middle | −3.889 | 1.627 | −3.889 | 1.627 | 0.017 | |||
| Age | Continuous variable | −0.206 | 0.059 | −0.322 | −0.091 | <0.001 | <0.001 | |
| The length of working in the medical service (years) | Continuous variable | −0.002 | 0.057 | −0.115 | 0.110 | 0.965 | 0.965 | |
: P-value of t-test for regression coefficient in each category;
: P-value from the General Linear Model (F-test).
4. Discussion
This large international study reports that frontline HCWs were anxious about the pandemic, with severe levels of anxiety in one of six HCWs who responded, regardless of levels of COVID-19 transmission in their countries of origin. The perceptions reflect concerns regarding preparation and resources. Our findings suggest that some individual variables identify subjects at high risk that should target preventive mental health support. Our findings suggest that higher levels of stress are perceived when they do not feel protected. Thus, interventions to improve training and education, and ensure adequate resources such as PPE, could have been better considered.
The survey was able to reach doctors and nurses in the general hospital who were exposed to COVID-19 patients. Furthermore, representation was collected from 75 countries and in several regions of the world not well represented in the current literature. This study highlighted that two-thirds of HCWs reported varying levels of anxiety, but 20% moderate, and 17% showed severe anxiety levels. There was no link between anxiety levels and the number of COVID-19 deaths in country, however HCWs in countries seeing high death rates were likely to report key concerns about their own institutions/health-care settings. Anxiety scores significantly increased with the gender (female staff), younger ages, lack of knowledge on COVID-19, occupation (being a nurse compared to being a medical doctor), insufficient medical supplies (PPE, disinfectants, liquid soaps), the HCWs' own coexisting medical and mental health problems, and living in higher income countries. These data suggest that more could be done to ensure potentially inexperienced younger HCWs and nursing staff are better supported during pandemics, alongside the critical need to give them access to PPE equipment and to ensure that HCWs feel protected. A key focus of healthcare institutions should be to ensure that sufficient education and information is provided and targeted at HCWs, particularly the youngest and most inexperienced. Our findings therefore confer with a recent systematic review, that reported health-care services having positive, safe and supportive learning environments were facilitators of intervention to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic [18].
Anxiety arising from exposure to life-threatening viral infections is a significant challenge to HCWs [19]. During outbreaks, HCWs are forced to cope with high emotional stress due to the risk of exposure, extreme workloads and moral ethical dilemmas. Rapid transmission of the virus and high rates of mortality are likely to have influenced the mental health of HCWs. There have been recent studies carried out to investigate the mental pressure of COVID-19 on HCWs, mainly from China, which report similar concerns raised by HCWs. For example, one cross-sectional study carried out with HCWs in the beginning of the pandemic in China, reported that women, nurses, other front-line workers, and those based in Wuhan were at higher risk of developing mental health symptoms [20]. In another study from the US, authors reported that nurses and advanced practice providers in particular were experiencing COVID-19-related psychological distress, concurring with our findings [21]. In a study, evaluating the psychological impact of the SARS epidemic on hospital employees in China, post-traumatic stress (PTS) symptom levels were associated with age, with younger people (<50 years) more likely to have a high PTS symptom level [5]. In our study, younger HCWs were more commonly anxious. Likewise, those who had a longer duration of experience in the profession had lower anxiety levels. In a recent study from the US, sources of anxiety included: absence of access to PPE, being exposed to COVID-19 at work and risk of infecting family, concerns about family care and responsibilities, and lack of access to up-to-date information and communication [22], which aligns with our findings exploring the views of HCWs globally. In another study done during the SARS Outbreak in Hong Kong, HCWs who were confident about infection control had lower stress levels than healthy control group [23]. In a recent survey performed in the US during COVID-19, ICU clinicians expressed continuing concern about PPE supplies [24], which is reflected in our data.
According to the World Health Organization's (WHO) World Mental Health Survey conducted between 2001 and 2012, generalized anxiety disorder was particularly more common in high-income countries [25]. Accordingly, our results demonstrated a correlation between higher income levels of the countries HCWs live in and anxiety scores. Interestingly, a study among 4875 ICU healthcare workers in the US revealed that they were more concerned about facility preparation than about their salary or personal benefits [26].
In a cross-sectional survey performed between April 30 and May 25, 2020 evaluating the prevalence of burnout syndrome among intensivists facing COVID-19 outbreak, the prevalence of symptoms of anxiety and depression and severe burnout was 46.5%, 30.2%, and 51%, respectively [27]. In the current pandemic, a recent study from China reported that compared with nonmedical health workers, medical HCWs had higher prevalence of insomnia, anxiety, depression, somatization, and obsessive-compulsive symptoms [28]. Although one study reported that stress levels of high-risk HCWs in respiratory medicine did not differ initially during the SARS outbreak in Hong Kong, the high-risk group – compared to HCWs deemed low risk (outside of respiratory medicine) – were associated with higher depression, anxiety, and PTS scores when HCWs were reassessed after the pandemic [29]. Therefore, data are now needed to assess the symptoms of mental health conditions such as post-traumatic stress disorder, depression, insomnia, and obsessive-compulsive disorders in HCWs to ensure we can better explore and assess the long-term impact of the COVID-19 pandemic on HCWs.
This study has several limitations. First, the questionnaires were dispatched non-randomly, so a selective-bias is likely; however, this was the only approach that could be taken given the time and logistical constraints and our aim to get a global set of responses. Although we used an international platform to send out the survey to HCWs all over the world, participation from some countries was limited due to country-specific access restrictions or language barriers. For example, China was not represented, whereas Portugal and the UK was highly represented in terms of numbers of respondents We mitigated against this by translating the survey in English, Italian and Turkish prior to circulation, but it was not possible to cover all languages given the time and resource constraints. Most participants were doctors or nurses and our findings cannot be generalized to other groups of HCWs.
The survey was performed at the beginning of the COVID-19 pandemic in most respondents' countries and next steps would be to explore the impact of the pandemic on HCWs beyond the first peak. Further research should now be done to investigate whether there are national or regional differences in countries hardest hit by the pandemic and the impact that anxiety had on absenteeism, poor performance or insomnia in HCWs.
5. Conclusions
Our study reflects the concerns of an international cohort of HCWs in the early phase of the COVID-19 pandemic and impact on mental health. Several factors were associated with increased anxiety among HCWs during the COVID-19 pandemic and these insights will support responses to future waves of the COVID-19 pandemic and future large-scale outbreaks of infectious diseases. Our data have generated the following policy and planning recommendations: First, health systems should ensure effective and concise training programs targeting HCWs (particularly the least experienced). Second, health systems must ensure rapid and updated communication reaches HCWs. Third, provision of medical supplies including PPE and hand hygiene products should be widely available, and stockpiles will need to be considered for future response.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data sharing
Data will be made available to interested individuals upon formal request made to authors.
Ethical consent
Ethical consent was obtained from Istanbul Medeniyet University School of Medicine (2020/0229).
Declaration of Competing Interest
Dr. Belliato reports personal fees from hamilton medical, bonaduz, Swiss, personal fees from eurosets srl, medolla, Italy, outside the submitted work. The other authors have no other interests to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2020.12.010.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
References
- 1.Jansson M., Liao X., Rello J. Strengthening ICU health security for a coronavirus epidemic. Intensive Crit Care Nurs. 2020;57:102812. doi: 10.1016/j.iccn.2020.102812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rose C., Am I. Part of the cure or Am I part of the disease? Keeping coronavirus out when a doctor comes home. N Engl J Med. 2020 doi: 10.1056/nejmp2004768. [DOI] [PubMed] [Google Scholar]
- 3.Pattison N. End-of-life decisions and care in the midst of a global coronavirus (COVID-19) pandemic. Intensive Crit Care Nurs J. 2020;102862 doi: 10.1016/j.iccn.2020.102862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devlin H. NHS staff need access to mental health services, says Labour. Guardian. 2020 https://www.theguardian.com/society/2020/may/01/nhs-staff-mental-health-services-coronavirus-labour (accessed December 20, 2020) [Google Scholar]
- 5.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ji D., Ji Y.J., Duan X.Z., Li W.G., Sun Z.Q., Song X.A., et al. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014–2015 Ebola outbreak in Sierra Leone: A cross-sectional study. Oncotarget. 2017;8:12784–12791. doi: 10.18632/oncotarget.14498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greenberg N., Wessely S., Wykes T. Potential mental health consequences for workers in the Ebola regions of West Africa - a lesson for all challenging environments. J Ment Health. 2015;24:1–3. doi: 10.3109/09638237.2014.1000676. [DOI] [PubMed] [Google Scholar]
- 8.Ruotsalainen J.H., Verbeek J.H., Mariné A., Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2014;2014 doi: 10.1002/14651858.CD002892.pub4. [DOI] [PubMed] [Google Scholar]
- 9.Acquadro C., Conway K., Hareendran A., Aaronson N. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Heal. 2008;11:509–521. doi: 10.1111/j.1524-4733.2007.00292.x. [DOI] [PubMed] [Google Scholar]
- 10.Baltar F., Brunet I. Social research 2.0: virtual snowball sampling method using Facebook. Internet Res. 2012;22:57–74. doi: 10.1108/10662241211199960. [DOI] [Google Scholar]
- 11.Zdravkovic M., Berger-Estilita J., Sorbello M., Hagberg C.A. An international survey about rapid sequence intubation of 10,003 anaesthetists and 16 airway experts. Anaesthesia. 2020;75:313–322. doi: 10.1111/anae.14867. [DOI] [PubMed] [Google Scholar]
- 12.Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 13.Creamer M., Foran J., Bell R. The Beck anxiety inventory in a non-clinical sample. Behav Res Ther. 1995;33:477–485. doi: 10.1016/0005-7967(94)00082-U. [DOI] [PubMed] [Google Scholar]
- 14.Ulusoy M, Sahin N, psychotherapy HE cognitive, 1998 undefined. Turkish Version of the Beck Anxiety Inventory: Psychometric Properties. n.d.
- 15.The Italian versions of the Beck Anxiety Inventory and the Beck Depression Inventory-II: Psychometric properties and discriminant power. - PsycNET n.d. https://psycnet.apa.org/record/2007-13441-002 (accessed April 15, 2020).
- 16.Magán I., Sanz J., García-Vera M.P. Psychometric properties of a Spanish version of the Beck anxiety inventory (BAI) in general population. Span J Psychol. 2008;11:626–640. doi: 10.1017/s1138741600004637. [DOI] [PubMed] [Google Scholar]
- 17.Beck A.T., Steer R. Psychological Corporation Harcourt Brace & Company; San Antonio, TX: 1993. Beck anxiety inventory manual. [Google Scholar]
- 18.Pollock A., Campbell P., Cheyne J., Cowie J., Davis B., McCallum J., et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. 2020 doi: 10.1002/14651858.CD013779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383:510–512. doi: 10.1056/nejmp2008017. [DOI] [PubMed] [Google Scholar]
- 20.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shechter A., Diaz F., Moise N., Anstey D.E., Ye S., Agarwal S., et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020 doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 23.Chua S.E., Cheung V., Cheung C., McAlonan G.M., Wong J.W.S., Cheung E.P.T., et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49:391–393. doi: 10.1177/070674370404900609. [DOI] [PubMed] [Google Scholar]
- 24.Moghbelli H, Ellithy K, Eslami Z, Vartanian R, Wannous D, El Ghamrawy A, et al. SCCM COVID-19 Rapid-Cycle Survey 2 Report. Crit Care Med n.d.;(In press). doi: 10.1016/j.solener.2019.02.027. [DOI]
- 25.Ruscio A.M., Hallion L.S., Lim C.C.W., Aguilar-Gaxiola S., Al-Hamzawi A., Alonso J., et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiat. 2017;74:465–475. doi: 10.1001/jamapsychiatry.2017.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaplan L.J., Kleinpell R., Maves R.C., Doersam J.K., Raman R., Ferraro D.M. Critical care clinician reports on coronavirus disease 2019. Crit Care Explor. 2020;2 doi: 10.1097/CCE.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Azoulay E., De Waele J., Ferrer R., Staudinger T., Borkowska M., Povoa P., et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020;10 doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang W., Wang K., Yin L., Zhao W., Xue Q., Peng M., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W.T., Sham P.C., et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2