Abstract
Objectives:
To explore strategies to improve type 2 diabetes mellitus (T2DM) self-management among low-income and minority groups.
Methods:
Focus groups centered on T2DM self-care behaviors were conducted using convenient sample of patients with T2DM (N = 17), caregivers (N = 5) and healthcare providers (N = 15).
Results:
Patients and caregivers perceived strategies included improving patient-provider communication, providers’ accessibility and compassion, and flexible clinic hours. Strategies identified by providers were realistic patient’s expectations, family support, and community resources.
Conclusions:
To our knowledge, this study is the first to elicit strategies to improve T2DM self-management through a joint meeting of patients, caregivers, and healthcare providers. Study findings could help inform future efforts to assist patients better manage their T2DM.
Keywords: diabetes management, health behavior, health disparities
Diabetes self-management often remains suboptimal for many patients, and this has been especially evident in under-resourced communities and minority populations.1 Examination of a national sample of patients with diabetes found that non-Hispanic Blacks (17.6%) and Hispanics (16.2%) had a higher prevalence of poor glycemic control compared to non-Hispanic Whites with diabetes (9.7%).2 It is also well documented that minority groups are at higher risk for diabetes-related deaths than the majority of the population3 and that both education and income are important contributing factors.4 In Tennessee, the annual average number of deaths from diabetes-related causes was 2.5 higher for black women (68.8 per 100,000 population) than for white women (27.0 per 100,000 population) from 2006 to 2011.5
The American Association of Diabetes Educators (AADE) identified 7 key self-care behaviors critical for optimal blood glucose control and to reduce the risk of diabetes complications.6 State-based diabetes management programs including, diabetes education programs have been developed to assist those with diabetes better manage their disease.7 Other programs such as the Diabetes Recognition Program (DRP) are also available to encourage providers to use evidence-based measures and provide excellent care for their patients.8 Despite existing programs, scientific innovations and the development of improved medication delivery systems, diabetes self-management continues to be a challenge for many patients, particularly those in low-income, largely minority communities.9–12
The day-to-day implementation of diabetes self-care requires patients’ personal commitment and knowledge in multiple domains.13 Cultural influences as well as socioeconomic and psychosocial factors can contribute to poor diabetes outcomes.10,11,14,15 Although studies that are aimed at individual goal-setting principles and tailored to incorporate behavioral changes have helped patients better manage their diabetes, the resultant self-care improvements have been short term.16,17 Given the health outcomes associated with poor diabetes management, effective strategies that can help patients with diabetes, particularly at-risk populations, adopt and sustain recommended self-care behaviors are urgently needed. Thus, using an exploratory qualitative approach, we sought to gain insight into strategies that would help facilitate the adoption of better self-care practices for those with type 2 diabetes mellitus (T2DM) from the perspectives of patients with diabetes, caregivers and healthcare providers.
METHODS
Study Design and Participants
The study was conducted using a mixed methods design to assess potential solutions to perceived barriers to T2DM self-care. Data were collected using focus groups and written questionnaires. Participants were recruited from the Family Medicine Clinic (FMC) at Meharry Medical College, a private, historically black institution in Nashville, Tennessee (USA). The FMC draws heavily on patients from the local area which has one of the highest prevalence rates of diabetes in metropolitan Nashville/Davidson County.
Participants included 17 adult patients with T2DM, 5 caregivers of patients with T2DM, and 15 healthcare providers (14 physicians and 1 nurse practitioner, who was also a registered dietician). Patients had to be ≥ 21 years of age, diagnosed with T2DM for at least one year, residents of Nashville/Davidson County, and able to communicate in English. Patients were identified from the Meharry FMC patient database; their charts were reviewed to determine eligibility. Eligible patients were contacted by phone and invited to participate in the study. Caregivers were family members who cared for persons with T2DM by assisting with administration of medications, transportation to clinic appointments, filling prescriptions, and meal preparations as well as providing emotional and physical support. Caregivers were recruited using flyers posted in the waiting area in the Meharry FMC. Healthcare providers were those who provided care to patients with T2DM at the Meharry FMC. Providers were recruited by personal invitation announced during weekly medical grand rounds in Meharry’s Department of Family Medicine.
Measures and Instruments
All participants completed a written questionnaire: demographic characteristics of patients with T2DM (ie, age, sex, race/ethnicity, household income, education, duration of diabetes, and current diabetes therapy), caregivers (age, sex, race/ethnicity, and relationship with diabetes patient), and providers (age, sex, race/ethnicity, specialty, and years of clinical experience). Enrolled patients with T2DM also completed 3 diabetes-related instruments. Basic knowledge about T2DM was assessed in focus group patients using the SKILLD (The Spoken Knowledge in Low Literacy Patients with Diabetes).18 It is a 10-item questionnaire which measures knowledge and core concepts in diabetes that are required for practical, daily self-care. Health literacy was assessed using the Short Form Test of Functional Health Literacy in Adults (s-TOFHLA),19 a 7-minute timed instrument with 36 items. Diabetes self-care behaviors were measured using the Summary of Diabetes Self-Care Activities (SDSCA).20 Patients were asked how often (number of days) during the last 7 days they performed recommended diabetes self-care activities. Patients’ responses to the SKILLD, s-TOFHLA and SDSCA measures were scored according to authors’ instructions. In addition, patients’ recent (≤ 6 months) clinical information including, body mass index (BMI), blood pressure, and laboratory values for lipids and HbA1c were obtained from medical records.
Study Procedures
Seven focus group discussions were conducted: 6 barrier-centered and one strategy-centered. The barrier-centered focus groups were designed to assess barriers to T2DM self-management as perceived by patients with T2DM, caregivers and providers. After the barrier-centered focus groups were completed, the same participants were invited to take part in a strategy-centered focus group session to discuss possible solutions to previously identified barriers. Of the 6 barrier-centered focus groups, 5 were conducted with 22 participants, a mix of 17 patients with T2DM and 5 caregivers. Size of focus groups for the patients and caregivers ranged between 4 and 5 per group, and each focus group lasted approximately 1 hour. The 6th barrier-centered focus group was conducted with 15 healthcare providers. The strategy-centered focus group (N = 15) was a joint discussion that included 8 T2DM patients, one caregiver, and 6 providers. Due to the size of the healthcare providers’ focus group (N = 15) and the strategy-centered focus group (N = 15), each focus group lasted between 1-½ to 2 hours to provide equal participation of all participants in the discussion. Members of the research team developed 2 focus group guides. The guides consisted of a moderator’s guide for focus group design, questions, and probes for the focus group discussions, and an implementation guide for assessing and cataloging focus group findings.21,22 During the focus group discussions, participants were asked to identify factors they perceived to hinder T2DM self-management and strategies they believed can help address them. Questions centered on healthy eating, staying active, medication compliance, monitoring of blood glucose, regular check-ups, and stress management. Each focus group was videotaped and audiotaped. A member of the research team was trained as a moderator and facilitated each focus group discussion. Two other research team members were also present at each focus group as an observer and note-taker and to help with the focus group logistics. A third year medical student also assisted with the note-taking. All participants were compensated with a $20 gift card for their participation at the end of each focus group discussion.
Data Analysis
Demographic characteristics were expressed as the median and interquartile range (IQR) or percentages and were generated using the Stata Statistical Software (Version 11.2, StataCorp. 2011, College Station, TX). Diabetes knowledge (SKILLD) performance for individual items was computed and patients’ overall scores (total range, 0%-100%) were calculated. A total score of <50% was categorized as having “low diabetes knowledge” and a score of ≥ 50% was categorized as having “high diabetes knowledge.” Individual S-TOFHLA overall scores were calculated with potential scores ranging from 0 to 36. The scores were categorized into: inadequate (0 to 16), marginal (17 to 22), or adequate (23 to 36). The SDSCA scores were calculated for each domain creating 5 subscales: general diet, specific diet, exercise, self-monitoring of blood glucose (SMBG), and foot care. Scores were computed using the mean number of days for items in individual domains. Scores for each domain were grouped into: ≤ 3 days and > 3 days (diet); < 3 days and ≥3 days (exercise); and less than daily and daily (SMBG and foot care).
Focus group discussions were transcribed verbatim by an experienced and qualified transcriptionist. For the qualitative data, the implementation guide was used to guide the analysis of focus group transcripts.21,22 First, a 5-column table was created on a Microsoft Excel spreadsheet for the barrier-centered and strategy-centered focus groups and labeled respondent, question number, response, theme, and category. All participants’ responses were entered into the Excel spreadsheets and grouped by question. Second, after reading the organized transcripts, research team members independently identified emerging barriers- and strategies-related themes across the entries for each question, and organized them into categories. Themes were content areas (for example, words, phrases or sentences) that reflected barriers or solutions that participants expressed during the focus groups. Where applicable, categories were broken into subcategories to allow better distinction and differentiation. Next, all members met to review and discuss their independent analyses. During these meetings, conflicting themes were explored, and if a theme did not belong to a submitted category, a new category was generated. How subcategories were related to each other within a category and to participants’ responses also was discussed. Discussions continued until saturation was reached, and all discrepancies were reconciled through group consensus.
RESULTS
Approximately 100 patients with T2DM were contacted, 50 patients expressed interest, and of the 50, 17 patients attended the focus groups. Among those who could not attend, some expressed concerns about scheduling conflicts (N = 12) or lack of transportation (N = 8); others could not be reached after the initial contact. Demographic characteristics of focus group participants are summarized in Table 1. All patients with T2DM had received care at the FMC for at least one year. Approximately 65% of the patients had never attended a diabetes class led by a diabetes educator; 53% had not seen an optometrist or ophthalmologist, and 76% had not had their teeth examined or cleaned by a dentist within the past 12 months. Most patients did not adhere to recommended diabetes self-care activities (SDSCA scores); 65% followed a healthful eating plan less than 3 days/week; 71% ate fruits and vegetables less than 3 days/week and high fat foods more than 3 days/week; 94% exercised less than 3 days/week. SMBG (82%) and foot care (100%) activities were performed by patients less than daily. The overall median score for patients’ diabetes knowledge (SKILLD test) was 30 (IQR: 10 – 50), with only 6 % and 12% of patients reported knowing normal HbA1c and complications of uncontrolled diabetes, respectively. Caregivers included 3 adult women and 2 adult men, with ages ranging from 28 to 54 years (Table 1). Providers (9 adult women and 6 adult men, age 29-54 years) included 14 physicians (Table 1) with 10 board certified physicians and 4 physicians in their 3rd year family medicine residency training program.
Table 1.
Characteristics of Focus Group Participants
| Patients (N = 17)a | |
| Age, median (IQR), years | 53.2 (49.9 – 55.7) |
| Race, % (N) | |
| Black | 82 (14) |
| White | 12 (2) |
| Education level, % (N) | |
| Less than high school | 47 (8) |
| High school graduate/GED | 24 (4) |
| Some college or technical school | 29 (5) |
| Household annual income, % (N) | |
| < $15,000 | 53 (9) |
| $15,000 - $24,999 | 35 (6) |
| $25,000 - $29,999 | 12 (2) |
| Smoking status, % (N) | |
| Current smoker, % | 35 (6) |
| Health insurance, % (N) | |
| Employer group plan | 24 (4) |
| Medicare/Medicaid | 42 (7) |
| No insurance | 34 (6) |
| Health literacy (s-STOFHLA), % (N) | |
| Inadequate (score 0-16) | 53 (9) |
| Marginal (score 17-22) | 6 (1) |
| Adequate (score 23-36) | 41 (7) |
| Diabetes duration, median (IQR), years, | 8.0 (5.0 – 8.0) |
| Medical comorbidity, % (N) | |
| Hypertension | 71 (12) |
| Hyperlipidemia | 47 (8) |
| Family history of diabetes (1st immediate relative), % (N) | 65 (11) |
| Diabetes therapy, % | |
| Oral hypoglycemic agent only | 53 (9) |
| Insulin + Oral hypoglycemic agent | 41 (7) |
| HbA1c,b median (IQR), % | 7.4 (7.1 – 9.6) |
| Blood pressure,b median (IQR), mm Hg | |
| Systolic | 141.5 (121.0 – 151.0) |
| Diastolic | 79.5 (71.0 – 91.0) |
| LDL-cholesterol,b median (IQR), mg/dl | 98.0 (78.0 – 113.0) |
| Body mass index,b median (IQR), kg/m2 | 37.9 (28.7 – 39.1) |
| Caregivers (N = 5) | |
| Race, % (N) | |
| Black | 100 (5) |
| Relationship with diabetes patient, N | |
| Daughter | 1 |
| Spouse | 4 |
| Providers (N = 15)c | |
| Race, % (N) | |
| White | 93 (14) |
| Black | 7 (1) |
| Specialties, % (N) | |
| Family Medicine | 100 (15) |
| Family Medicine/Obstetrics/Gynecology | 7 (1) |
| Clinical experience, median (IQR), years | 4.0 (3.0 – 4.0) |
Notes.
N = 15 for HbA1c, blood pressure, LDL-cholesterol, and body mass index.
Values were obtained from medical chart review, all other data obtained at same visit as focus group discussion.
Race/ethnicity was not reported for 1 patient. Abbreviations: IQR, interquartile range; HbA1c, glycosylated hemoglobin; LDL, Low-density lipoprotein.
Providers included 10 board certified physicians, 4 physicians in their 3rd year family medicine residency training program, and 1 nurse practitioner/registered dietician.
Participants’ Perceived Barriers to T2DM Management
Several themes emerged from the barriers-centered focus groups (Table 2). T2DM patients voiced being often overwhelmed by what was asked of them. When asked about how they perceived the seriousness and long-term complications of uncontrolled T2DM, most patients believed that the disease was inevitable, because as some stated, “It runs in my family.”
Table 2.
Perceived Barriers to Type 2 Diabetes Self-management among Focus Group Participants with Representative Quotes
| Patients and Caregivers (N = 22) | Providers (N = 15) a | |
|---|---|---|
| Patient-related Barriers | ||
| Patient motivation | ||
| Medication side effects | Not understanding health benefits | |
| Finger pain/Soreness | ||
| Preference of physicians over residents | ||
| Knowledge deficit | ||
| Healthy food choices | Diabetes complications | |
| Portion control | Health Literacy and numeracy | |
| Complex insulin therapy/sliding scale | ||
| Understanding doctor’s instructions | ||
| ”….if they take insulin and they are on a sliding scale, they cannot do it effectively….and they don’t want to drop too low.” (Provider) | ||
| “I would like to say …sometimes they [patients] don’t come back because the instructions are not clear…We need to reach out and consider the patient’s needs….” (Provider) | ||
| Resources | ||
| Transportation cost with multiple trips to clinic/pharmacy | Means of transportation | |
| Work schedule | ||
| “I have too many visits scheduled close to each other. I am tired and frustrated going to the doctor every week”. (Patient) | ||
| Beliefs/Attitudes/Expectations | ||
| Fear of hypo and hyperglycemia | Unrealistic weight management goals | |
| Rigid diet schedule | ||
| Poor self-control-craving | ||
| Difficulty breaking family habits | ||
| ” I have patients who said”: “I have tried this. I have tried that for a couple weeks and I am the same size. ” (Provider) | ||
| Structure-related Barriers | ||
| Clinic | ||
| Taking time off work-loss of income | Requesting follow up visits for refills | |
| Long waiting time at the clinic | Number of visits allowed | |
| Not seeing same provider at each visit | ||
| “I see different doctors each time and each time I am told something different and they give me something different and I am tired of that”. (Patient) | ||
| “The number of visits. Sometimes it’s an issue, especially with the older folks. They are only allowed so many doctors’ visits. So if they are seeing other specialists, they run out of the number of doctor’s visits, so they won’t want to come… …So frequent doctors’visits can detour them from coming back.” (Provider) | ||
| Provider | ||
| Provider insensitivity | Patient Lack of trust | |
| Limited access to provider | ||
| Poor provider-pharmacist coordination | ||
| “Sometimes I want to speak to the doctor about my medicine. When I called the doctor, he is not there. Sometimes they asked me to make an appointment to see the doctor. I don’t need that for a simple question ” (Patient) | ||
| “You go to get your prescription and the pharmacist tells you that you can’t have it. The prescription can’t be refilled. They try to call your doctor and the doctor doesn’t call right back. So you have to go without it and running back and forth to the pharmacy.” (Caregiver) | ||
| Community | ||
| Easy access to fast foods | ||
| Poor access to grocery stores | ||
| Neighborhood safety | ||
Note.
Providers included 10 board certified physicians, 4 physicians in their 3rd year family medicine residency training program and 1 nurse practitioner/registered dietician.
Participants’ Strategies to T2DM Management
Patients and caregivers expressed interest in diabetes education classes at the clinic to help patients have a better understanding of their diabetes and how to prevent complications. One patient stated: “Why is my sugar still high after I take my medicines? I don’t think the medicines are working.” Another patient noted: “My mom and dad are gone. They died from the same disease I have. I want to live to see my daughter get married.” Providers also recognized the need for diabetes education classes and suggested that having a diabetes support group could allow patients to share successes, which in turn could motivate other patients to care for their diabetes better. Participants’ strategies to address identified barriers to T2DM self-behaviors are presented in Table 3.
Table 3.
Participants’ Suggested Self-care Behavior Strategies
| Patients and Caregivers (N = 22) | Self-care behaviors | Providers (N = 15) |
|---|---|---|
| Improving nutrition literacy | Healthy eating | Patient Education |
| Knowledge of food guides | Exploring seasonal foods | |
| Understanding/use of food labels | Local farmer markets | |
| Adequate meal planning | Involving family members | |
| Provider compassion | Staying active | Help patients manage expectations |
| Setting realistic goals | ||
| Choosing sustainable exercise plans | ||
| Provider-pharmacist coordination | Medication compliance | Provide medication consultation |
| Support outside the clinic | Encourage patient to be proactive | |
| Use courtesy refills registry | ||
| Reasonable testing frequency | Blood glucose monitoring | Develop patient support groups |
| Patient motivation and commitment | ||
| Flexible hours | Doctor visits | Outreach from providers |
| Later/weekend clinic hours | Reminder and follow-up calls | |
| Shorter clinic waiting time | Explaining purpose of visits | |
| Family support | Stress management | Patient education on copying skills |
DISCUSSION
Poor management of T2DM is associated with devastating health outcomes leading to premature deaths. Yet, many patients continue to struggle with the day-to-day implementation of T2DM self-management activities.13 The purpose of this study was to elicit what patients with T2DM, caregivers, and healthcare providers perceived to be solutions to barriers to T2DM self-care.
The need for diabetes education at the clinic was the most common agreed upon strategy among patients/caregivers and providers. Studies indicated that the challenges to achieving optimal self-care are even greater in ethnic and racial minority populations including, those with low socioeconomic status,23 and that patients with inadequate health literacy and low diabetes knowledge have worse diabetes outcomes.24 The association between health literacy and knowledge of self-care behaviors and glycemic control also has been documented,24,25 and studies indicate that diabetes education improves diabetes self-management, diabetes knowledge and glycemic control in low literacy patients.26 In this study, most patients had low health literacy and less than optimal self-care behaviors. In addition, the average patient’s score on the SKILLD test was low (30%) with large deficits in patient responses to knowledge of individual items. Many patients at risk for poor diabetes control are not capable of accessing diabetes education services.27 In our patient sample the majority had never had a formal diabetes education class, which could explain the low diabetes knowledge performance score.
Improving patient-provider communication (patients/caregivers) and improving the patient’s proactivity (providers) were viewed as important strategies to help patients understand and follow their treatment regimen. Studies indicate that patients and providers understand diabetes and perceive diabetes treatment goals differently,28,29 and this may be due to a lack of patient-provider collaboration in discussing treatment goals and strategies. Another contributing factor to this gap is providers not seeking to reach out to patients.30
Patients’ motivation for self-care is as critical as their knowledge because over time, the commitments needed to achieve optimal diabetes self-care become difficult to maintain as the motivation diminishes. Flexible clinic hours, shorter clinic waiting times, a reasonable number of daily/weekly episodes of self-monitoring of blood glucose, better coordination of medication refills, as well as improving patients’ perception of provider sensitivity and trust could directly and indirectly influence patients’ motivation, and thus, help change their behaviors (beliefs and attitudes) to adhere to recommended diabetes self-care activities.
Limitations
There are several limitations associated with this study. Participants recruited for this study consisted of patients and providers who were seen or provided care at Meharry’s FMC and who spoke English, thereby limiting the generalizability of our findings to a larger minority population. In addition, the size of patients’ and caregivers’ barrier-centered focus groups was small and may not have been representative of all patients at risk of diabetes complications. However, our findings are consistent with previous studies investigating barriers to diabetes care when surveying large cohort of patients with diabetes, including low-income minorities.11,14,26,31,32 Although a range of 6 to 10 participants per focus group has been suggested,33 focus group size in several studies has ranged from 3 to 16.34–36 In this study, poor patient attendance was due to schedule conflict and lack of transportation.
To our knowledge, this study is the first to elicit strategies to improve diabetes self-management through a joint meeting of patients, caregivers, and healthcare providers. Our findings can inform future diabetes self-management interventions for under-resourced communities that need to focus on the impact of the strategies identified in this study on patient self-care knowledge, motivation, self-efficacy, and health outcomes (Figure 1). Furthermore, addressing structure-related barriers including, patient access to services such diabetes education, could provide an excellent outreach strategy and a step toward ensuring optimal diabetes self-care for the more disadvantaged patients.
Figure 1.
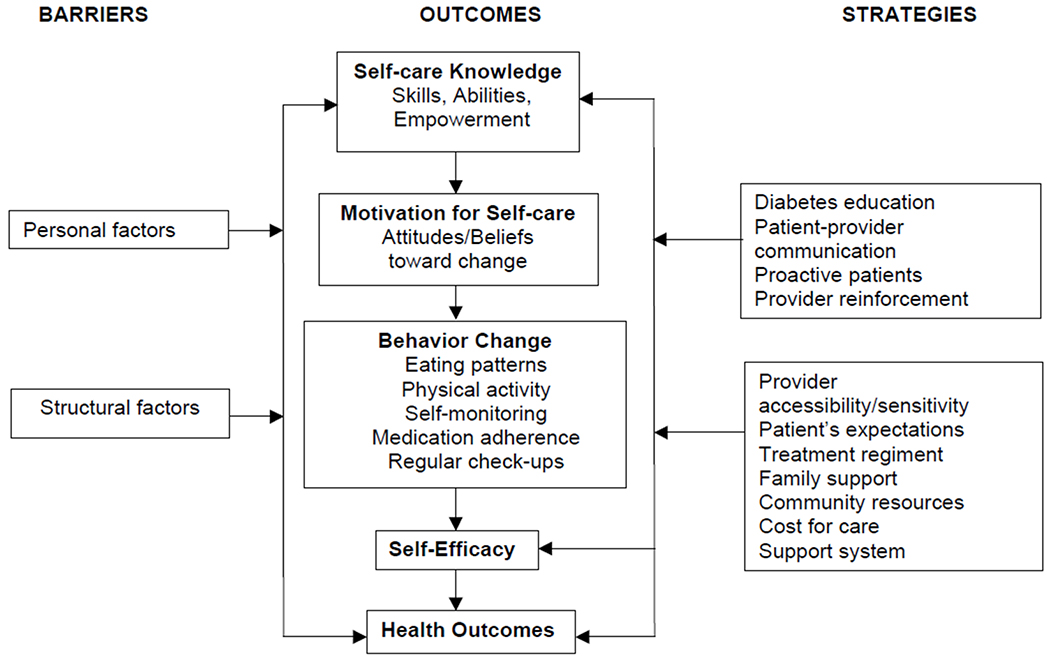
Model Illustrating Potential Strategies to Address Barriers to Type 2 Diabetes Self-Management
Acknowledgments
The project was supported by TCDPHI-GR082257300 from The State of Tennessee, Center for Diabetes Prevention and Health Improvement, UL1 TR000445 from NCATS/NIH, and Center for Diabetes Translational Research (Community Outreach and Health Disparity Core). Part of this study was presented at the 44th Society of Teachers of Family Medicine (STFM) Annual Spring Conference. New Orleans, LA, April 27-May 1, 2011.
The authors thank all the participants for their enthusiasm and commitment to this study. They also thank Mrs. Turner for helping with patient recruitment and assisting with note taking during the focus group discussions and Dr Marver for her critical review of the manuscript. Finally, they acknowledge Drs Sidani and Zoorob for their support during this project.
Footnotes
Human Subjects Statement
The Meharry Medical College Institutional Review Board approved the study and all procedures. Written informed consent was obtained from participants prior to data collection.
Conflict of Interest Statement
The authors have no competing interests with respect to this research.
Contributor Information
Sylvie A. Akohoue, Department of Family and Community Medicine, Meharry Medical College, Nashville, TN.
Kushal Patel, Department of Public Health, Health Administration and Health Sciences, Tennessee State University, Nashville, TN.
LeMonica L. Adkerson, Department of Family and Community Medicine, Meharry Medical College, Nashville, TN.
Russell L. Rothman, Vanderbilt University School of Medicine, Vanderbilt Center for Health Services Research, Nashville, TN.
References
- 1.Harris MI, Eastman RC, Cowie CC, et al. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22:403–408. [DOI] [PubMed] [Google Scholar]
- 2.Ali MK, McKeever BK, Imperatore G, et al. Characteristics associated with poor glycemic control among adults with self-reported diagnosed diabetes—National Health and Nutrition Examination Survey, United States, 2007-2010. MMWR Morb Mortal Wkly Rep. 2012;61(2):32–37. [PubMed] [Google Scholar]
- 3.Department of Health and Human Services, Office of Minority Health. Diabetes and African Americans (on-line). Available at: http://minorityhealth.hhs.gov/templates/content.aspx?ID=3017 Accessed December 12, 2013.
- 4.Saydah S, Lochner K. Socioeconomic status and risk of diabetes-related mortality in the U.S. Public Health Rep. 2010;125(3):377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tennessee Women’s Health Report Card 2013. (on-line). Available at: https://medicineandpublichealth.vanderbilt.edu/twhrc/2013whrc.pdf Accessed May 10, 2013.
- 6.AADE7 Self-Care Behaviors. Diabetes Educ. 2008;34:445–459. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. National diabetes prevention programs (on-line). Available at: http://www.cdc.gov/diabetes/states/ Accessed December 10, 2012.
- 8.National Committee for Quality Assurance. Diabetes Recognition Program (on-line). Available at: http://www.ncqa.org/tabid/139/Default.aspx Accessed December 10, 2012.
- 9.Tennessee Department of Health, Office of Policy Planning and Assessment. Tennessee Behavioral Risk Factor Surveillance System (on-line). Available at: http://apps.nccd.cdc.gov/BRFSS/ Accessed December 10, 2012.
- 10.Shenolikar RA, Balkrishnan R, Camacho FT, et al. Race and medication adherence in Medicaid enrollees with type-2 diabetes. J Natl Med Assoc. 2006;98:1071–1077. [PMC free article] [PubMed] [Google Scholar]
- 11.Trinacty CM, Adams AS, Soumerai SB, et al. Racial differences in long-term self-monitoring practice among newly drug-treated diabetes patients in an HMO. J Gen Intern Med. 2007;22:1506–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Funnell MM. The diabetes attitudes, wishes, and needs (DAWN) study. Clinical Diabetes. 2006;24:154–155. [Google Scholar]
- 13.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;24:454–459. [DOI] [PubMed] [Google Scholar]
- 14.Bell RA, Summerson JH, Konen JC. Racial differences in psychosocial variables among adults with non-insulin-dependent diabetes mellitus. Behav Med. 1995;21:69–73. [DOI] [PubMed] [Google Scholar]
- 15.Glasgow RE, Hampson SE, Strycker LA, Ruggiero L. Personal-model beliefs and social-environmental barriers related to diabetes self-management. Diabetes Care. 1997;20:556–561. [DOI] [PubMed] [Google Scholar]
- 16.Sperl-Hillen J, Beaton S, Fernandes O, et al. Comparative effectiveness of patient education methods for type 2 diabetes: a randomized controlled trial. Arch Intern Med. 2011;171:2001–2010. [DOI] [PubMed] [Google Scholar]
- 17.Weinger K, Beverly EA, Lee Y, et al. The effect of a structured behavioral intervention on poorly controlled diabetes: a randomized controlled trial. Arch Intern Med. 2011;171:1990–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothman RL, Malone R, Bryant B, et al. The Spoken Knowledge in Low Literacy in Diabetes Scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ. 2005;31:215–224. [DOI] [PubMed] [Google Scholar]
- 19.Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 20.Toobert D, Glasgow R. Assessing diabetes self-management: the Summary of Diabetes Self-care Activities Questionnaires In Bradley C. Handbook of Psychology and Diabetes. New York, NY: Psychology Press; 1994:351–375. [Google Scholar]
- 21.Rabiee F Focus-group interview and data analysis. Proc Nutr Soc. 2004;63:655–660. [DOI] [PubMed] [Google Scholar]
- 22.Krueger RA. Analyzing focus group interviews. J Wound Ostomy Continence Nurs. 2006;33:478–81. [DOI] [PubMed] [Google Scholar]
- 23.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. [DOI] [PubMed] [Google Scholar]
- 24.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998; 158:166–172. [DOI] [PubMed] [Google Scholar]
- 25.Schillinger D, Barton LR, Karter AJ, et al. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaw K, Killeen M, Sullivan E, Bowman P. Disparities in diabetes self-management education for uninsured or underinsured adults. Diabetes Educ. 2011;37:813–819. [DOI] [PubMed] [Google Scholar]
- 27.Saberi S, Heisler M. Speaking the same language? Contrasting provider and patient definitions of good diabetes control. Primary Care Diabetes. 2008;10:270–280. [Google Scholar]
- 28.Loewe R, Freeman J. Interpreting diabetes mellitus: differences between patient and provider models of disease and their implications for clinical practice. Cult Med Psychiatry. 2000;24:379–401. [DOI] [PubMed] [Google Scholar]
- 29.Glasgow RE, Boles SM, Calder D, et al. Diabetes care practices in primary care: results from 2 samples and 3 measurement sets. Diabetes Educ. 1999;25:755–763. [DOI] [PubMed] [Google Scholar]
- 30.Glasgow RE, Strycker LA. Preventive care practices for diabetes management in 2 primary care samples. Am J Prev Med. 2000;19:9–14. [DOI] [PubMed] [Google Scholar]
- 31.Cox RH, Carpenter JP, Bruce FA, et al. Characteristics of low-income African-American and Caucasian adults that are important in self-management of type 2 diabetes. J Community Health. 2004;29:155–170. [DOI] [PubMed] [Google Scholar]
- 32.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31:391–398. [DOI] [PubMed] [Google Scholar]
- 33.Morgan DL. Focus groups as qualitative research: planning and research design for focus groups (on-line). Available at: http://www.uk.sagepub.com/gray3e/study/chapterl8/Book%20chapters/Planning_and_designing_focus_groups.pdf Accessed December 08, 2014.
- 34.Shangase P, Egbe CO. Barriers to accessing HIV services for black African communities in Cambridgeshire, the United Kingdom. J Community Health. 2015;40(1):20–26. [DOI] [PubMed] [Google Scholar]
- 35.Zeldenryk L, Gray M, Gordon S, et al. The use of focus groups to develop a culturally relevant quality of life tool for lymphatic filariasis in Bangladesh. Qual Life Res. 2014;23:299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hu J, Amirehsani K, Wallace DC, Letvak S. Perceptions of barriers in managing diabetes: perspectives of Hispanic immigrant patients and family members. Diabetes Educ. 2013;39:494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]


