Abstract
Management of severe coronavirus disease 2019 requires advanced respiratory support modalities including invasive mechanical ventilation (IMV), continuous positive airway pressure (C-PAP), and non-invasive ventilation ((NIV). IMV leads to either subtle forms of lung injury (pulmonary edema, lung cysts) or more severe form of lung injury manifested as subcutaneous emphysema, pneumomediastinum, and pneumothorax (herein collectively termed barotrauma). We have described two cases showing the two end of spectrum of ventilator associated lung injury (VALI).
Abbreviations: ARDS, Acute Respiratory Distress Syndrome; VALI, Ventilator Associated Lung Injury; IMV, Invasive Mechanical Ventilation; COVID-19, Coronavirus Disease 19; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
1. Introduction
Acute respiratory distress syndrome (ARDS) and hypoxemic respiratory failure are the most feared complication of severe COVID-19 disease.
Positive pressure ventilation (PPV) is non-physiological and invasive intervention that can be lifesaving in these patients. PPV, like any other intervention, carries its own risk and complication as it can lead to ventilator-associated lung injury, which may be associated with multisystem organ failure in these patients with increased mortality and duration of hospital stay [1].
Different guidelines, including the last surviving sepsis campaign guidelines for COVID-19 patients recommends using low Vt (4−8 ml/kg) as it is believed to decrease VALI in a lung suffering from ARDS [2]. Other lung-protective strategies include targeting plateau pressures (Pplat) of <30 cm H2O to limit lung injury as Pplat > 32 were associated with higher short-term mortality and driving pressure (Pplat minus positive end expiratory pressure) below 13−15 cm H2O.
Because VALI may not be readily defined nor detected, our ability to determine its independent risk factors, incidence, and effects on outcome is inherently hampered. Barotrauma, which is more evident clinically and radiologically, is therefore used as a surrogate measure of VALI. The reported incidence rate of barotrauma is 4.8–11% in ARDS patients receiving IMV (3). However, the reported incidence of barotrauma is 15 % in severe COVID-19 patients requiring IMV and is more likely to occur in younger patients [3].
2. Case number 1
A 37 year old male patient was admitted in our hospital; complaining of cough, shortness of breath and fever with RT-PCR (Reverse Transcriptase- Polymerase Chain Reaction) confirmed COVID-19 disease. He was a smoker with undiagnosed prediabetes and no known preexisting lung disease. The CXR taken at the time of admission revealed no significant abnormality (Fig. 1). The patient condition significantly deteriorated clinically in the first week of his admission in medical ward and he had to be shifted to ICU requiring IMV, due to severe hypoxemia (PaO2 69 % on high flow oxygen). As the patient hypoxemia worsened further, in an effort to maintain lung protective IMV strategy (Pplat of <30 cm H2O and driving pressure below 15 cm H2O), veno-venous extracorporeal membranous oxygenation (ECMO) was employed 7 days after patient’s admission in ICU.
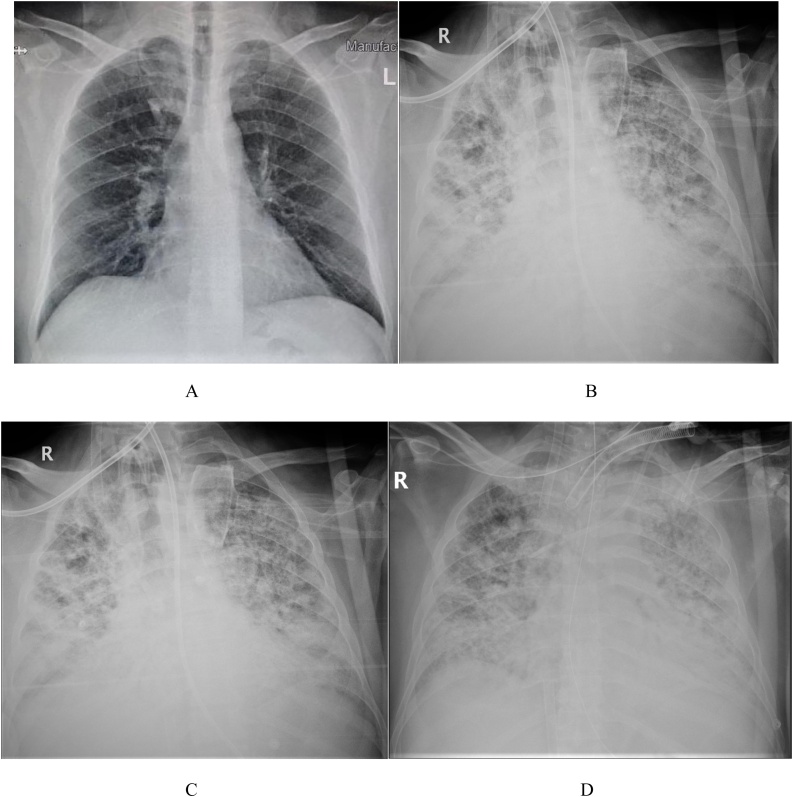
Fig. 1.
(A to D). (A) CXR on admission showing no significant abnormality (B) CXR one day prior to HRCT chest with patient on veno-venous ECMO and invasive mechanical ventilation, showing extensive areas of consolidations in both lungs with greater affection of both mid and lower zones (C) CXR one week after HRCT and (D) CXR one day prior to patient’s death showing no Radiological improvement with further worsening of both lung involvement.
The patient’s condition, however didn’t improve and after 4 weeks on IMV and ECMO, the treating physician noticed abnormal breathing pattern & gasping whenever he tried to reduce patient’s sedation. Serial CXRs were taken during this time and the findings correlated with worsening clinical condition of the patient and ARDS. The CXR taken a day before HRCT Chest was requested showed extensive areas of consolidations in both lungs with greater affection of right lung and both lungs mid and lower zones, along with suspicion of cystic air filled spaces in right lung upper zone paratracheal region (Fig. 1).
High resolution CT chest was requested after 6 weeks of his admission in ICU. HRCT chest was done on as per routine protocol on a MDCT scanner with 64 multidetector rows (Siemens Somatom Definition Edge). Volumetric spiral HRCT Chest with 1 mm slice thickness and 3 mm gap was done with reconstruction at 1 mm increment and dedicated ultra-sharp hard B157 kernel. The images were sent to PACS (Picture Archiving and Communications System) for interpretation.
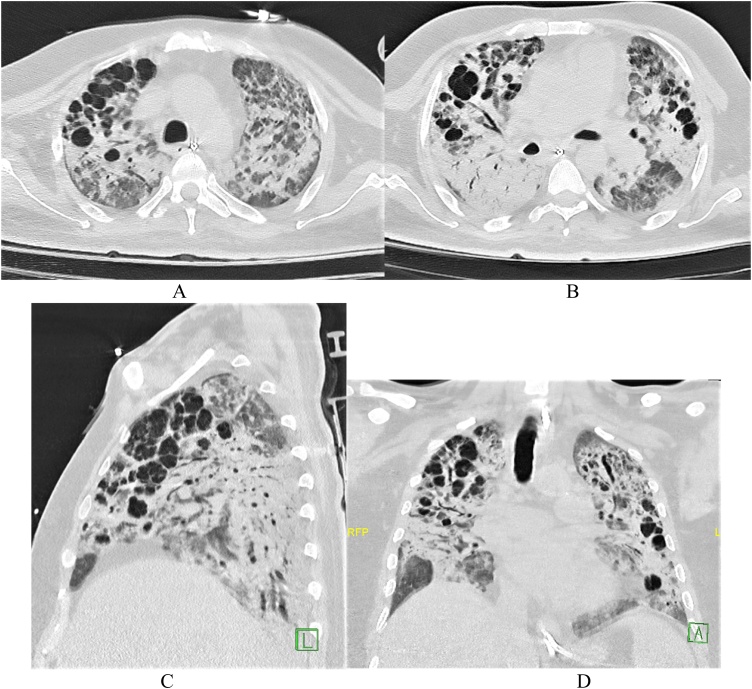
HRCT chest revealed extensive areas of ground glass opacities mixed with large areas of consolidation with air bronchogram showing antero-posterior gradient in both lungs, the typical imaging findings of ARDS. Discrete bizarre shaped scattered air filled variable size cystic lesions were seen in both lungs upper lobes more anteriorly & in right lung middle lobe with few internal septations within (Fig. 2). One of the differential diagnosis for the lung cysts seen is Langerhans Cell Histiocytosis (LCH) with patient’s history of smoking, however the lung cysts described with LCH are generally smaller and clustered with upper and mid lobe distribution and associated with scattered centrilobular nodules in both lungs with sparing of cardio phrenic and costophrenic regions.
Fig. 2.
(A to D). HRCT Chest (A) & (B) Axial images at the level of aortic arch and carina, showing bizarre shaped multiple air filled cysts in anterior more aerated parts of both lungs with protective effective of consolidations in posterior dependent region of both lungs (C) Sagittal reformatted image showing multiple air filled cysts within anterior part of right lung upper and middle lobes with protective effect of consolidations in right lower lobe (D) Coronal reformatted image showing multiple bizarre air filled cysts in more aerated parts of both lungs with few small subpleural cysts and mild bronchiectatic changes in left lung upper lobe.
Consolidations have a protective effect on the lung parenchyma under positive end expiratory pressure (PEEP) used in conjunction with IMV. The ventrally located areas of more aerated lung are more prone to the effects of VALI.
The patient’s condition didn’t improve clinically and radiologically (on serial CXRs) and he could not be weaned from IMV and ECMO. CXR taken one week after the CT scan didn’t show any improvement with diffuse areas of consolidations in both lungs and serial CXRs thereafter showed greater involvement of both lungs with denser areas of consolidations (Fig. 1). The patient succumbed to death 16 days after CT scan and 57 days after he was put on invasive mechanical ventilation secondary to respiratory and multiorgan failure.
Learning Points
-
•
VALI in the form of air filled cysts is predominantly seen in anterior more normal lungs (better ventilated areas) because of the protective mechanism of consolidation in posterior dependent regions of lungs in patients with ARDS.
3. Case number 2
A 70 year old male patient was admitted to our hospital complaining of cough and shortness of breath with RT-PCR confirmed COVID-19 disease. He was known hypertensive and diabetic with no history of preexisting lung disease. At the time of admission, his CXR revealed left lung mid and lower zone haziness with mild density peripheral air space opacities (Fig. 3). Patient initial oxygen saturation was 96 % on 5 L oxygen mask. After 5 days of admission in medical ward, the patient’s condition started deteriorating with increased oxygen demand reaching up to 15 L oxygen on oxygen mask to maintain 94 % PaO2.
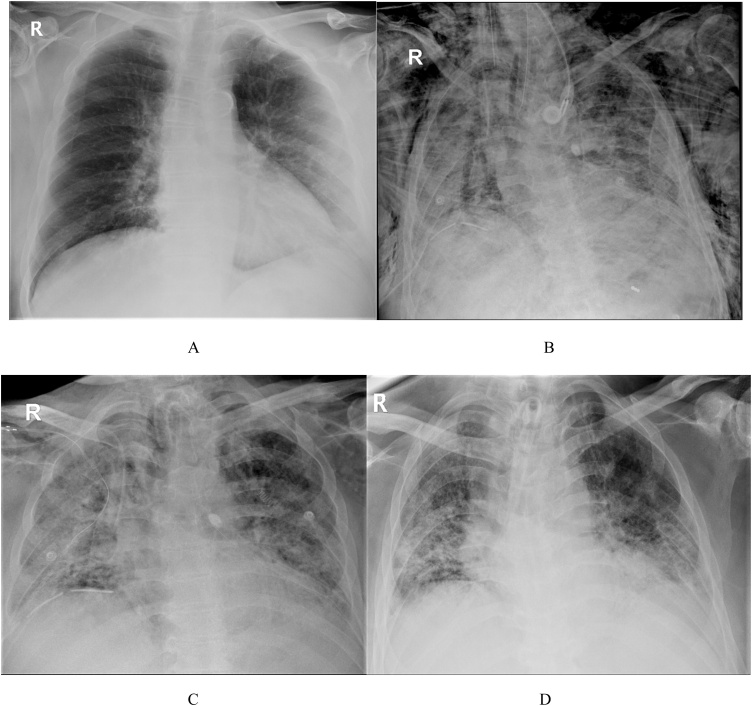
Fig. 3.
(A to D). (A) CXR on admission showing haziness in left lung mid and lower zones with peripheral air space opacities (B) CXR 12 days prior to HRCT chest with patient on invasive mechanical ventilation, showing patchy areas of consolidations in both lungs with bilateral chest wall and lower neck emphysema and pneumomediastinum with minimal right pneumothorax. Intercostal drainage tube is seen along right lateral chest wall in situ (C) CXR 8 days after HRCT showing almost complete resolution of VALI with persistent both lungs areas of consolidation (D) CXR 4 weeks after CT, showing significant interval Radiological improvement with reduced both lungs areas of consolidation and complete resolution of VALI.
The patient had to be shifted to ICU with increased oxygen demand and worsening hypoxemia. He had to be intubated and put on IMV. Serial CXRs were taken to monitor the severity of COVID-19 pneumonia and lung injury.
After 5 days on mechanical ventilation, patient’s CXR revealed minimal right pneumothorax, pneumomediastinum and mild chest wall and neck emphysema which got worsened on serial CXRs (Fig. 3). Intercostal drainage tubes were placed along both lateral chest wall to relieve pneumothorax. However, pneumomediastinum and chest wall emphysema continue to worsen on serial CXRs. After 12 days of worsening pneumomediastinum and chest wall emphysema, HRCT chest was done to determine the extent of barotrauma related complications.
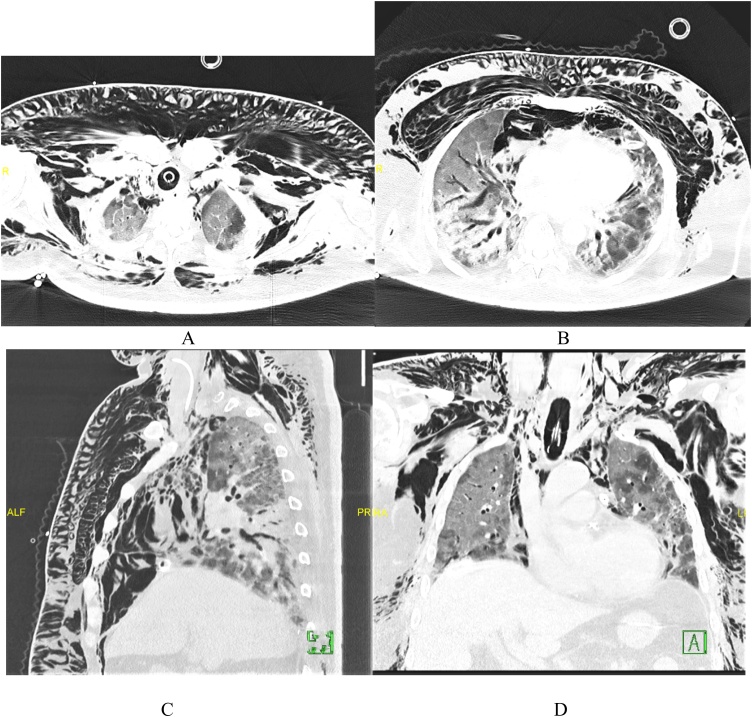
HRCT Chest revealed extensive neck, chest and upper abdominal wall emphysema with significant pneumomediastinum. Within the lungs, extensive areas of ground glass opacity mixed with consolidation showing antero-posterior gradient was seen in both lungs with right lung being more affected. Few small ∼3−5 mm subpleural cystic lesions were seen in both lungs. Inter and intralobular septal thickening was seen within the areas of ground-glass opacification with subpleural lines, as described in COVID-19 pneumonia common imaging findings. Mild cylindrical bronchiectatic changes more common in both lower lobes, affecting central bronchi predominantly, was seen (Fig. 4).
Fig. 4.
(A to D). HRCT Chest (A) & (B) Axial images at the level of proximal trachea and heart, showing extensive bilateral chest wall and neck emphysema, with pneumomediastinum and typical findings of COVID-19 pneumonia with ARDS (C) Sagittal reformatted image of right hemithorax showing barotrauma with lung findings of ground glass opacity mixed with consolidations showing anteroposterior gradient with bronchiectatic changes (D) Coronal reformatted image showing barotrauma, with few scattered small subpleural cysts in left lung.
Post CT scan patient was taken off from IMV and put on C-PAP as patient clinical condition and blood oxygenation level improved. Patient pneumomediastinum and chest wall emphysema gradually resolved and serial CXRs suggested almost complete resolution of barotrauma related complications 8 days after CT scan, and 23 days after the first sign of barotrauma on CXR (Fig. 3).
Learning points:
-Changing ventilator settings or shifting patient from IMV to C-PAP or NIMV if possible (depending upon patient blood oxygenation and clinical condition) remains the mainstay of treatment of barotrauma [2].
4. Discussion
The incidence of barotrauma (surrogate measure of VALI) varies according to the indication for mechanical ventilation, and patients with underlying lung disease (pneumonia, chronic interstitial lung disease) are more prone to barotrauma compared to patients who are intubated for septic shock or develop ARDS for a non-pulmonary insult.
With over 37.5 million confirmed cases of COVID-19 worldwide as of October 12, 2020, the lack of consensus in patient management recommendations makes supportive care as still the mainstay of management of severe COVID-19 disease. Respiratory failure in patients with COVID-19 infection was initially thought to be due to viral pneumonitis progressing to ARDS; thus, many patients with severe COVID-19 disease were put on IMV with high positive end-expiratory pressure (PEEP). Increased incidence of barotrauma has been reported in patients with severe COVID-19 disease and is seen more in younger patients [3].
Several mechanisms may explain increase incidence of barotrauma in COVID-19. Pathologic processes such as interstitial pneumonia, consolidation, and in-situ thrombosis, all seen in COVID-19 pneumonia, increases the friability of lung parenchyma and pleura, thus increasing the risk of fistulation between the distal airways and pleural space or hilum [3].The peripheral predominance of COVID-19 pneumonia and its propensity to cause cystic change, may further explain increase risk in these patients [4].
In ARDS, edema and atelectasis leads to reduced aerated lung volume in both lungs, predominantly in posterior dependent regions. This can result in damage from regional over distension in recruited lung (volutrauma), increased shear strain in ventilated alveolar tissue (atelectrauma), high transpulmonary pressures (barotrauma), and surfactant dysfunction and inflammation (biotrauma), different forms of VALI. The process of subpleural air cyst formation associated with VALI in patients with ARDS begins with rupture of weaker alveoli along the margins of interlobular septa and vascular structures. Air then dissects along the interlobular septa and vascular structures, producing interstitial emphysema. The interstitial air may rupture into pleural space (pneumothorax) or into the mediastinum (pneumomediastinum). Air may collect in extra alveolar spaces forming lung cysts [4,5].
In our first patient detailed above, bizarre multiple air filled cystic lesions were seen on HRCT scan in the anterior more normal lungs with rest of both lungs showing imaging’s findings of ARDS. Consolidation in posterior dependent areas of both lungs seen in ARDS have a protective effect on the lung parenchyma under PEEP ventilation, while the ventrally located areas of more aerated lung are more prone to the effects of VALI in the form of air cysts and bronchiectatic changes [6]. In addition to IMV, the patient was also on ECMO because of refractory hypoxemia. Unusually high incidence of pulmonary thromboembolism is seen in COVID-19 patients on ECMO that can affect the lungs besides other vascular complications associated with it (likely due to increased incidence of widespread thrombosis with microangiopathy and alveolar capillary microthrombi in patients with COVID-19) [7].
In our second case, HRCT chest revealed more common and severe detectable form of VALI that is barotrauma with evidence of extra-alveolar air.
5. Conclusion
VALI is a common subtle complication in severe COVID-19 pneumonia patients on IMV and may reflect a worse prognosis. Our case reports, showed two completely different end of spectrum of VALI associated with the management of severe COVID-19 pneumonia. Both the Radiologists and the treating physician should be aware of increased incidence of VALI and its possible manifestations in COVID 19 pneumonia with its unique ventilator management challenges.
Compliance with ethical standards
This retrospective study involving human participants was in accordance with the ethical standards of Ministry of Health, Kuwait and prior approval has been taken from MOH, Kuwait research ethics committee.
Informed consent was waived off, as ours is a retrospective study and patient identifying details are not revealed in entire manuscript.
We give the rights to the corresponding author to make necessary changes as per the request of the journal, do the rest of the correspondence on our behalf and he/she will act as the guarantor for the manuscript on our behalf.
Funding statement
We certify that there was no source of funding for any of the author involved in preparation of this manuscript.
Declaration of Competing Interest
We certify that we do not have conflict of interest.
This retrospective study involving human participants was in accordance with the ethical standards of Ministry of Health, Kuwait and prior approval has been taken from MOH, Kuwait research ethics committee.
Informed consent was waived off, as ours is a retrospective study and patient identifying details are not revealed in entire manuscript.
We give the rights to the corresponding author to make necessary changes as per the request of the journal, do the rest of the correspondence on our behalf and he/she will act as the guarantor for the manuscript on our behalf.
References
- 1.Abdallat M., Khalil M., Al-Awwa G., Kothuru R., Punzina C. Barotrauma in COVID-19 patients. J. Lung Health Dis. 2020;4:8–12. [Google Scholar]
- 2.Alhazzani W., Møller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intensive Care Med. 2020;46(5):854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGuinness G., Zhan C., Rosenberg N., Azour L., Wickstrom M., Mason D.M. High incidence of Barotrauma in patients with COVID-19 infection on invasive mechanical ventilation. Radiology. 2020 doi: 10.1148/radiol.2020202352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones E., Gould A., Pillay T.D., Khorasanee R., Sykes R., Bazo-Alvarez J.C. Subcutaneous emphysema, pneumomediastinum, and pneumothorax in critically ill patients with coronavirus disease 2019: a retrospective cohort study. Crit. Care Expl. 2020;2(9):e0210. doi: 10.1097/CCE.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International consensus conferences in intensive care medicine: ventilator-associated Lung Injury in ARDS. This official conference report was cosponsored by the American Thoracic Society, the European Society of Intensive Care Medicine, and the Societé de Réanimation de Langue Française, and was approved by the ATS Board of Directors, July 1999. Am. J. Respir. Crit. Care Med. 1999;160(6):2118–2124. doi: 10.1164/ajrccm.160.6.ats16060. [DOI] [PubMed] [Google Scholar]
- 6.Treggiari M.M., Romand J.A., Martin J.B., Suter P.M. Air cysts and bronchiectasis prevail in nondependent areas in severe acute respiratory distress syndrome: a computed tomographic study of ventilator-associated changes. Crit. Care Med. 2002;30(8):1747–1752. doi: 10.1097/00003246-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt M., Hajage D., Lebreton G., Monsel A., Voiriot G., Levy D. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30328-3. Published August 13. [DOI] [PMC free article] [PubMed] [Google Scholar]