Abstract
A toddler with neurofibromatosis type 1 (NF1) was evaluated for tuberculosis (TB) after exposure. Chest X-ray (CXR) revealed a mediastinal mass indicating lymphadenopathy. However, magnetic resonance imaging showed a large plexiform thoracic neurofibroma.
CXR performed for TB screening in NF1 patients cannot clearly differentiate lymphadenopathy from thoracic plexiform neurofibroma. Cross sectional imaging is therefore indicated for classification of mediastinal masses.
Keywords: Neurofibromatosis, Tuberculosis, Mediastinal mass, Children
Case report
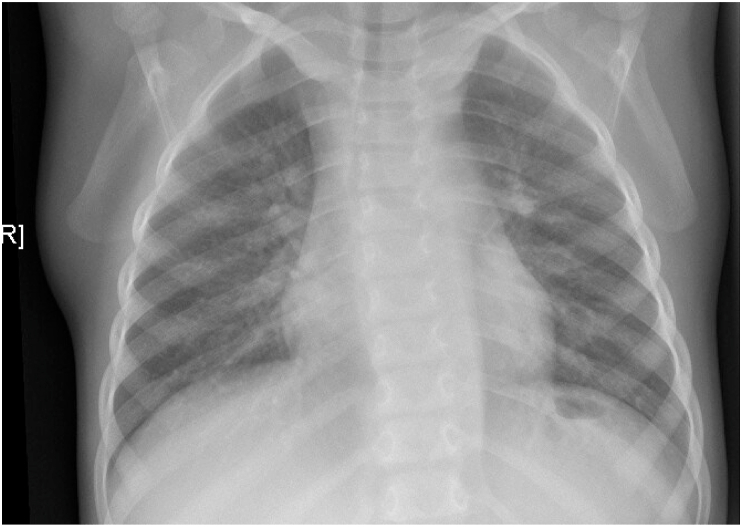
A two-year old girl was presented in our pediatric infectious disease unit for evaluation of tuberculosis (TB) in the context of contact tracing. She was previously diagnosed with neurofibromatosis type 1 (NF1). Chest X-ray (CXR) revealed a mediastinal and hilar mass indicating lymphadenopathy (Fig. 1). However, tuberculin skin test (TST; PPD-RT23; AJ Vaccines A/S, Denmark) and Interferon-Gamma-Release Assay (IGRA; QuantiFERON®-TB Gold; Qiagen, Hilden, Germany) were negative. Furthermore, she had no clinical symptoms of TB. Due to the preexisting disease, magnetic resonance imaging (MRI) was performed, which showed a large, confluent plexiform cervical and thoracic neurofibroma (Fig. 2). Neither enlarged hilar or mediastinal lymph nodes nor other signs of intrathoracic tuberculosis were detectable. The child was examined again eight weeks after the last contact to the TB source case. TST and IGRA remained negative in the asymptomatic child and TB could therefore be virtually excluded.
Fig. 1.
CXR shows an chimney-shaped opacity in the upper mediastinum, the hilus region is rounded. The trachea is shifted to the left side and impressed. The lung parenchyma shows no pathologies. There are no calcifications or apical infiltrates.
Fig. 2.
Magnetic resonance imaging (MRI); HASTE T2 (coronal section) shows a signal intense mass along the sympathic trunk in the upper/lower mediastinum and perihilar that does not resemble lymphatic tissue. There is no pathology in the lung parenchyma.
In young children with tuberculosis, hilar and mediastinal lymphadenopathy are the most frequent findings on CXR [1]. Children may initially be asymptomatic. Moreover, IGRA and TST can be negative in infected children [2]. Therefore, a hilar or mediastinal mass in an TB-exposed young child is highly suspicious for tuberculosis, irrespective of IGRA and TST results or clinical symptom unless a differential diagnosis can clearly be established.
NF1 is an autosomal-dominant inherited disorder characterized by multiple café au lait spots, cutaneous neurofibromas, axillary and inguinal freckling, Lisch nodules, and choroidal freckling. Overall, plexiform neurofibromas (PNF) are diagnosed at varying locations in approximately 50% of NF1 patients [3]. In a large pediatric case series, intrathoracic plexiform neurofibroma have been reported in four out of 260 patients [4].
Early identification of such PNF is critical as symptomatic PNF are associated with increased mortality. Especially thoracic PNF show a more progressive behavior leading to enhanced chances of morbidity [5]. Once a PNF is diagnosed it is mandatory to follow its growth as malignant transformation towards malignant peripheral nerve sheath tumor is possible, which may be proven using glucose-PET [6].
In conclusion, CXR performed for TB screening in NF1 patients cannot clearly differentiate mediastinal or hilar lymphadenopathy from thoracic plexiform neurofibroma. Therefore, cross sectional imaging is indicated in these patients for classification of mediastinal or hilar masses.
Summary and learning points: In TB-exposed children with NF1, cross-sectional imaging is required if a mediastinal or hilar mass is seen on plain CXR to differentiate lymphadenopathy from PNF.
Funding
None.
Declaration of competing interest
I declare, that there is no conflict of interest.
References
- 1.Androunikoou S., Kilborn T. Radiology of childhood tuberculosis. In: Starke J., Donald P., editors. Handbook of Child and Adolescent Ttuberculosis. Oxford university press; New York, USA: 2016. pp. 109–146. [Google Scholar]
- 2.Soler-Garcia A., Gamell A., Santiago B., Monsonis M., Calvo C., Cobo E. Diagnostic accuracy of QuantiFERON-TB Gold plus assays in children and adolescents with tuberculosis disease. J. Pediatr. 2020;223:212–215. doi: 10.1016/j.jpeds.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 3.Gutmann D.H., Ferner R.E., Listernick R.H., Korf B.R., Wolters P.L., Johnson K.J. Neurofibromatosis type 1. Nat Rev Dis Primers. 2017;3:17004. doi: 10.1038/nrdp.2017.4. [DOI] [PubMed] [Google Scholar]
- 4.Schorry E.K., Crawford A.H., Egelhoff J.C., Lovell A.M., Saal H.M. Thoracic tumors in children with neurofibromatosis-1. Am. J. Med. Genet. 1997;74(5):533–537. doi: 10.1002/(sici)1096-8628(19970919)74:5<533::aid-ajmg16>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 5.Prada C.E., Rangwala F.A., Martin L.J., Lovell A.M., Saal H.M., Schorry E.K. Pediatric plexiform neurofibromas: impact on morbidity and mortality in neurofibromatosis type 1. J. Pediatr. 2012;160(3):461–467. doi: 10.1016/j.jpeds.2011.08.051. [DOI] [PubMed] [Google Scholar]
- 6.Tsai L.L., Drubach L., Fahey F., Irons M., Voss S., Ullrich N.J. [18F]-Fluorodeoxyglucose positron emission tomography in children with neurofibromatosis type 1 and plexiform neurofibromas: correlation with malignant transformation. J. Neuro Oncol. 2012;108(3):469–475. doi: 10.1007/s11060-012-0840-5. [DOI] [PubMed] [Google Scholar]