Highlights
-
•
Little is known about barriers to PrEP prescribing in safety-net settings.
-
•
We identified low provider knowledge of PrEP as a barrier to PrEP prescribing.
-
•
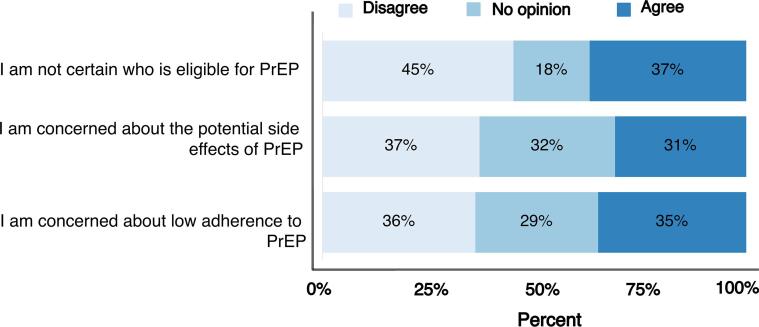
PrEP eligibility, side effects and adherence concerns were key unmet knowledge needs.
Keywords: HIV, Prevention, Pre-exposure prophylaxis, Implementation, Primary Care, Safety-net
Abstract
Safety-net health systems are a primary source of care for socioeconomically disadvantaged individuals who may be eligible for HIV pre-exposure prophylaxis (PrEP) and are priority groups under the Ending the HIV Epidemic (EHE) initiative. Nevertheless, little evidence is available about barriers to PrEP implementation in safety-net settings. We aimed to assess the association between PrEP knowledge and prescribing practices, and to ascertain unmet knowledge needs to implement PrEP. In 2019, we surveyed primary care providers (PCPs) in a safety-net health system that serves an EHE priority jurisdiction located in North Texas. Our questionnaire ascertained self-reported prescribing practices, knowledge, and training needs related to PrEP. We used penalized logistic regression to estimate odds ratio (OR) and 95% posterior limits (PL) for the association between provider self-rated knowledge of PrEP and PrEP prescribing. Our study population comprised 62 primary care providers, of whom 61% were female, 60% were non-Hispanic White, 76% were physicians (76%), 57% had ≥ 10 years of practice experience, 45% reported low self-rated PrEP knowledge, and 35% prescribed PrEP in the past year. Providers with low PrEP knowledge had 69% lower odds of prescribing PrEP within the past year (OR = 0.31, 95% PL: 0.12, 0.82). Eligibility for PrEP, side effects and adherence concerns were key unmet knowledge needs. Our findings suggest that low provider PrEP knowledge may be a barrier to PrEP prescribing among safety-net PCPs. Our results provide insight about specific educational needs of PCPs in a safety-net health system, which are amenable to educational intervention.
1. Background
The United States (US) government recently launched a new federal initiative, Ending the HIV Epidemic (EHE), to reduce the number of incident HIV infections in the US by 90% within the next decade (Fauci et al., 2019). This initiative prioritizes geographic regions such as the southern US because over half of new HIV cases in 2018 were diagnosed in this region and predominantly among racial/ethnic and sexual minorities (CDC, 2019a, CDC, 2019b). HIV pre-exposure prophylaxis (PrEP) is a critical component of this initiative (Giroir, 2020). PrEP using tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) or tenofovir alafenamide/emtricitabine (TAF/FTC) reduces HIV transmission when taken as prescribed (Baeten et al., 2012, Grant et al., 2010, McCormack et al., 2016). PrEP is currently recommended for susceptible at-risk individuals, which includes people who are injection drug users (IDU), have a recent bacterial sexually transmitted infection (STI), are engaged in commercial sex work, or have a high number of sex partners (Smith et al., 2018a, Smith et al., 2018b). A key challenge for the EHE initiative is implementation of PrEP by primary care providers (PCPs) in healthcare systems.
Prior studies have reported low PrEP use across the country (Huang et al., 2018, Mayer et al., 2018, Sullivan et al., 2018). For example, in an analysis of 2017 prescription data, the lowest PrEP-to-need ratio was seen in US South residents, and less than 10% of the estimated 1.2 million eligible individuals received PrEP (Siegler et al., 2018). Several barriers to PrEP implementation have been identified among PCPs including stigma, lack of knowledge, and inadequate skills to prescribe PrEP (Mayer et al., 2020, Pleuhs et al., 2020). Nevertheless, limited evidence is available about potential barriers to PrEP implementation among PCPs in safety-net health systems, which may be particularly important in geographic regions where HIV incidence has increased (CDC, 2019c, Singh et al., 2018). Safety-net health systems are a primary source of care for socioeconomically disadvantaged populations that have a high risk of HIV acquisition (IOM, 2000). Safety-net health systems also serve more ethnically and racially diverse communities, which are priority groups for PrEP implementation under the EHE initiative. Knowledge of barriers to PrEP implementation in this setting could inform interventions to increase PrEP adoption and facilitate access for individuals who would not otherwise have access to PrEP. Therefore, we aimed to assess the association between knowledge of PrEP and prescribing practices among PCPs in a safety-net health system that serves a county designated as an EHE priority area. In addition, we aimed to ascertain specific unmet knowledge needs to implement PrEP (Fig. 1).
Fig. 1.
Unmet needs for knowledge training among safety-net primary care providers.
2. Methods
2.1. Study setting
JPS Health Network (JPS) is the only safety-net health system in Tarrant County, Texas. The network includes a 578-bed academic teaching hospital and over 40 satellite clinics and accredited Primary Care Medical Homes (PCMHs) distributed across the county. Tarrant County is a national HIV hotspot with a prevalence of 281 per 100,000 population and increasing HIV incidence (Texas Department of State Health Services, 2019). In 2019, Tarrant County was identified as a priority area by the EHE initiative for targeted implementation efforts (Fauci et al., 2019). This study was approved by the North Texas Institutional Review Board (IRB #2019-073).
2.2. Study population
We surveyed in-network clinicians (physicians, excluding medical residents, nurse practitioners, clinical pharmacists, and physicians assistants) who provided outpatient primary care services at any JPS facility. Eligible providers were identified from an email list of primary care providers compiled by JPS Medical Staff Office and invited for the survey by direct email. The survey was conducted over a 30-day period from October 2nd to October 31st, 2019. All eligible providers received a total of six emails during the survey window: one email sent a week before survey, an introductory email invitation containing a consent statement and a URL link to the web based survey located on the JPS intranet, three reminder emails (days 14, 21, and 28 of the survey window), and one closing email sent on last day of the survey. Survey responses were kept anonymous and participants were discouraged from forwarding survey emails to their peers to reduce the potential for selective participation.
2.3. Variables
We used an 18-item survey instrument (Supplementary Materials) that included questions about providers’ knowledge and attitudes about PrEP, practices of PrEP, training needs, and demographics. Survey questions were adapted from validated surveys used in previous studies on PrEP (Blumenthal et al., 2015, Puro et al., 2013, Sharma et al., 2014, Wood et al., 2018). Demographic questions on the survey included gender identity, age, race/ethnicity, practice specialty, and years since completing residency or training. Provider knowledge and comfort with prescribing PrEP was assessed using three questions that asked participants to rate their knowledge of PrEP and if they knew enough about PrEP to have an informed discussion with their patients. A third question provided a multiple choice question on a scenario where PrEP was indicated. We assessed providers’ attitudes towards PrEP by asking participants to rank a list of statements about prescribing PrEP that endorsed their perspective. Response options used a five-point Likert scale that ranged from “strongly agree” to “strongly disagree”. We asked providers who had experience with PrEP to indicate which category of patients asked about PrEP, if the discussion was initiated by the provider, and if there was a risk assessment tool available at their practice to help screen and identify patients who may benefit from PrEP. Lastly, providers reported if they were interested in PrEP education, their training needs, and their preferred model of PrEP implementation in their practice.
2.4. Data analysis
We used logistic regression to estimate the odds ratio (OR) and 95% confidence limits (CL) for the association between self-rated low knowledge of PrEP and PrEP prescribing within the past year. Low PrEP knowledge was defined as self-reported low or no knowledge of PrEP. We adjusted for covariates assumed to be common causes of both low knowledge and PrEP prescribing based on subject-matter knowledge (Hernan et al., 2002, Robins, 2001). Specifically, our estimate was adjusted for provider age, gender, race/ethnicity, and years of clinical practice. To reduce sparse categories for analysis, we collapsed categories for some variables. Age was categorized as ≤40 years, 41–50 years, and >50 years. Gender was dichotomized as male or female. Race/ethnicity was dichotomized as non-Hispanic White and racial/ethnic minorities (i.e. non-Hispanic Black, Hispanic, and Asian). Years of clinical practice was dichotomized as <10 years and ≥10 years. Despite this initial reduction of sparse categories, we recognized the potential for sparse-data bias (Greenland et al., 2016, Greenland et al., 2000) because of few observations in certain strata of covariates. Consequently, we used penalized logistic regression to reduce the magnitude of sparse-data bias (Discacciati et al., 2015, Greenland, 2006, Greenland and Mansournia, 2015). This semi-Bayesian approach involved combining the observed OR with a null-centered prior (i.e. ORprior = 1.0) and variance of 0.5 for ln(ORprior), which corresponded to a 95% CL between 0.25 and 4.0 for ORprior. These prior limits were liberal considering an upper limit of 4.0 implied an improbable 4 times higher odds of prescribing PrEP for providers who self-reported low knowledge. Nevertheless, smaller variance would have over-weighted the prior assumptions relative to the observed data. Lastly, we estimated the frequency of knowledge needs and individual components of self-reported knowledge, where 5-point Likert responses were collapsed to three-category responses to reduce potential sparse categories. Respondents who answered “strongly agree” or “agree” were considered as endorsing agreement, responses of uncertain or no opinion were considered uncertain, and responses of “strongly disagree” or “disagree” were considered as endorsing disagreement.
3. Results
Our eligible population included 283 providers, of whom 62 (22%) responded with sufficient data for this analysis. Table 1 summarizes demographic characteristics of the study population. The majority of respondents were female (61%), non-Hispanic White (60%), and primary care/internal medicine physicians (76%). In addition, 57% of respondents had been practicing medicine for ≥10 years.
Table 1.
Demographic characteristics of primary care provider respondents at an urban safety-net health system.
| Characteristics | n (%) |
|---|---|
| Number of survey respondents | 62 |
| Gender | |
| Male | 21 (34) |
| Female | 38 (61) |
| Age, years | |
| <30 | 1 (2) |
| 31–40 | 20 (32) |
| 41–50 | 19 (31) |
| 51–60 | 15 (24) |
| >60 | 5 (8) |
| Race/ethnicity | |
| Non-Hispanic White | 37 (60) |
| Non-Hispanic Black | 7 (11) |
| Asian | 12 (19) |
| Hispanic | 5 (8) |
| Provider type or specialty | |
| Primary care physician | 29 (47) |
| Internal medicine | 17 (27) |
| Nurse practitioner | 7 (11) |
| Infectious disease | 3 (5) |
| Othera | 5 (9) |
| Years in clinical practice | |
| <5 | 15 (24) |
| 5–9 | 11 (18) |
| 10–14 | 10 (16) |
| 15–19 | 8 (13) |
| ≥20 | 17 (27) |
Abbreviations: PrEP = Pre-exposure prophylaxis for HIV; PCP = Primary care provider.
Other: Physician Assistant = 1; Obstetrician/Gynecologist = 1; Clinical Pharmacists = 1; Dentist = 2.
3.1. Provider knowledge and PrEP prescription
Overall, 45% of participants self-reported low knowledge of PrEP and 35% prescribed PrEP in the past year. Table 2 summarizes estimates for the association between self-rated low knowledge of PrEP and PrEP prescribing within the past year. PCPs who self-reported low knowledge of PrEP had 91% lower odds of prescribing PrEP (OR = 0.09, CL: 0.02, 0.45). Nevertheless, using methods to address sparse-data bias, PCPs who self-reported low knowledge of PrEP had 69% lower odds of prescribing PrEP within the past year (OR = 0.31, 95% PL: 0.12, 0.82).
Table 2.
Self-rated low knowledge of HIV pre-exposure prophylaxis (PrEP) and PrEP prescribing among primary care providers in an urban safety-net health system.
| Adjusted probability of prescribing PrEP within the past yeara | Odds ratioa (95% CLb) | Penalized odds ratioa (95% PLc) | |
|---|---|---|---|
| Low knowledge | 15% | 0.09 (0.02, 0.45) | 0.31 (0.12, 0.82) |
| Medium or high knowledge | 59% | 1.0 (reference) | 1.0 (reference) |
Adjusted for age, gender, race/ethnicity, and years of clinical practice.
CL: confidence limits.
PL: posterior limits.
3.2. Status of PrEP knowledge among safety-net PCPs
PrEP awareness among providers was high (98%), but more than half (55%) endorsed insufficient knowledge about PrEP to have an informed discussion with their patients. In addition, 55% did not initiate a discussion about PrEP as a prevention option with their patients in the past year. Among providers who endorsed sufficient knowledge about PrEP, 23% had been asked by patients about PrEP in the past year (predominantly MSM [31%] or individuals in a serodiscordant relationship [11%]). The majority of participants (71%) reported that the lack of an available screening tool in their practice was a barrier to identify high risk patients.
4. Discussion
Our results suggest that low self-reported knowledge of PrEP has a strong inverse association with PrEP prescribing within the past year among PCPs in a safety-net health system. Nevertheless, providers had a high awareness of PrEP and were willing to prescribe PrEP if given additional information. Specific knowledge barriers included uncertainty about who was eligible for PrEP, and concerns about adherence and side effects.
Our findings should be considered in the context of certain limitations. The response proportion for our survey was comparable with other PrEP surveys among physicians, (Silverman et al., 2018) but selection bias is a consideration for explaining findings in our study and prior studies. We were unable to obtain detailed demographic data for the 283 PCPs eligible for our survey, but we explored gender distributions as a crude indicator of selective participation. For example, 35% of physicians who participated in our survey were male, whereas 67% of family medicine physicians in JPS Health Network are male. If a high proportion of male non-participants had low self-reported knowledge of PrEP, then we may be underestimating the prevalence of low self-reported knowledge or other knowledge needs. Nevertheless, underestimated prevalence of low self-reported knowledge is unlikely to explain the inverse association with PrEP prescribing within the past year. Consider that the prevalence of PrEP prescribing within the past year would also have to be high among non-participating PCPs with low self-reported knowledge, which seems behaviorally counterintuitive and implausible because of universally low PrEP uptake.
Several studies have described provider lack of knowledge or low knowledge as a putative implementation barrier to PrEP prescription (Bacon et al., 2017, Blackstock et al., 2017, Blumenthal et al., 2015, Clement et al., 2018, Hakre et al., 2016, Mimiaga et al., 2014, Ojile et al., 2017, Petroll et al., 2017, Seidman and Weber, 2016, Tripathi et al., 2012, Walsh and Petroll, 2017, Wood et al., 2018). Nevertheless, few studies aimed to estimate the magnitude of association between low knowledge and PrEP prescription, which could provide insight about whether low knowledge would be an impactful target for intervention. Blumenthal et al. (2015) reported that providers with a high PrEP knowledge score had higher odds of prescribing PrEP (OR = 1.6, 95% CL: 1.1, 2.3) (Blumenthal et al., 2015). Wilson et al. (2020) also reported that providers with high self-reported knowledge had higher odds of PrEP prescribing but with less precision than Blumenthal et al. (2015) (OR = 2.2, 95% CL: 0.95, 4.9). The collective evidence (including our study) about the association between knowledge and PrEP prescribing seems consistent with expectations, but the magnitude of association is difficult to interpret because of imprecise estimates and variation across studies. For example, the characteristics of providers and settings, measurement of PrEP knowledge, and covariates selected for adjustment to reduce confounding bias varied across studies. Nevertheless, evidence from intervention studies supports the idea that improving PrEP knowledge can increase PrEP adoption and prescribing among PCPs (Bunting et al., 2020, Clement et al., 2018, Sales et al., 2019).
PrEP knowledge encompasses diverse concepts such as PrEP awareness. Prior studies reported PrEP awareness between 61% and 93% among providers (Blumenthal et al., 2015, Krakower et al., 2015, Petroll et al., 2017, Smith et al., 2016, Wood et al., 2018). The proportion of providers who reported PrEP awareness in our study was high (98%), but providers in our study had longer exposure to PrEP than providers in prior studies (e.g. through increased media attention). Furthermore, as reported in other studies (Wilson et al., 2020), participants who responded to the survey were more interested in PrEP. Nevertheless, awareness does not necessarily translate to prescribing. Similar to our findings, Blackstock et al. (2017) surveyed academic general internists in primary care, of whom 93% were aware of PrEP but only one-third had ever prescribed or referred a patient for PrEP.
We also elicited PCPs attitudes about PrEP to ascertain potential targets for an educational intervention. Providers in our survey endorsed interest in receiving educational trainings on PrEP and integrating PrEP services into primary care. This finding is encouraging because PCPs and HIV specialists often disagree about whom should be responsible for prescribing PrEP. This “Purview Paradox” is frequently cited as a significant barrier to PrEP adoption in primary care settings (Krakower et al., 2014, Lee and Petersen, 2018, Pinto et al., 2018, Pleuhs et al., 2020). Notably, in a recent study, the majority of surveyed PCPs preferred a PrEP implementation model in which patients received PrEP care within their clinical practice rather than be referred elsewhere, but these findings may not be generalizable to physicians in non-academic settings (Edelman et al., 2020). Additional research is needed to determine which implementation models can facilitate optimal PrEP adoption within primary care settings and areas where uptake is low.
In summary, assuming no major biases, our findings suggest that low provider knowledge may be a barrier to PrEP prescribing among safety net PCPs, which emphasizes the need for educational interventions to increase PrEP prescribing. Our results also provide insight about specific educational needs of PCPs in a safety-net health system, which can be used to design an intervention. Given that our setting is generally representative of safety-net health systems (Clark et al., 2020), our findings may also be relevant to other safety-net settings and EHE priority jurisdictions where focused PrEP implementation efforts are needed.
5. Financial disclosure
There are no financial disclosures to report by any authors of this paper.
6. Availability of data and materials
The data that support the findings of this study are available from the authors upon reasonable request and within the limits of IRB rules.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101266.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Bacon O., Gonzalez R., Andrew E., Potter M.B., Iniguez J.R., Cohen S.E., Liu A.Y., Fuchs J.D. Brief report: informing strategies to build PrEP capacity among San Francisco bay area clinicians. J. Acquir. Immune Defic. Syndr. 2017;74:175–179. doi: 10.1097/QAI.0000000000001182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeten J.M., Donnell D., Ndase P., Mugo N.R., Campbell J.D., Wangisi J., Tappero J.W., Bukusi E.A., Cohen C.R. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 2012;367:399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackstock O.J., Moore B.A., Berkenblit G.V., Calabrese S.K., Cunningham C.O., Fiellin D.A., Patel V.V., Phillips K.A., Tetrault J.M. A cross-sectional online survey of HIV pre-exposure prophylaxis adoption among primary care physicians. J. Gen. Intern. Med. 2017;32:62–70. doi: 10.1007/s11606-016-3903-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal J., Jain S., Krakower D., Sun X., Young J., Mayer K., Haubrich R., Team C.C.T.G. Knowledge is power! increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19:802–810. doi: 10.1007/s10461-015-0996-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunting S.R., Saqueton R., Batteson T.J. Using a student-led, community-specific training module to increase PrEP uptake amongst at-risk populations: results from an exploratory pilot implementation. AIDS Care. 2020;32:546–550. doi: 10.1080/09540121.2019.1659916. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2019a. HIV Surveillance Data Tables (early release): Core indicators for monitoring the Ending the HIV Epidemic initiative, data reported through December 2020. HIV Surveillance Data Tables http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
- Centers for Disease Control and Prevention, 2019b. HIV Surveillance Report, 2018 (Preliminary). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
- Centers for Disease Control and Prevention, CDC data confirm: Progress in HIV prevention has stalled, 2019c, https://www.cdc.gov/media/releases/2019/0227-hiv-prevention-stalled.html, March 20th 2020.
- Clark D., Roberson B., Ramiah K. Essential Hospitals Institute; 2020. Essential Data: Our Hospitals, our Patients. [Google Scholar]
- Clement M.E., Seidelman J., Wu J., Alexis K., McGee K., Okeke N.L., Samsa G., McKellar M. An educational initiative in response to identified PrEP prescribing needs among PCPs in the Southern U.S. AIDS Care. 2018;30:650–655. doi: 10.1080/09540121.2017.1384534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Discacciati A., Orsini N., Greenland S. Approximate Bayesian logistic regression via penalized likelihood by data augmentation. Stata J. 2015;15:712–736. [Google Scholar]
- Edelman E.J., Moore B.A., Calabrese S.K., Berkenblit G., Cunningham C.O., Ogbuagu O., Patel V.V., Phillips K.A., Tetrault J.M. Preferences for implementation of HIV pre-exposure prophylaxis (PrEP): results from a survey of primary care providers. Prev. Med. Rep. 2020;17 doi: 10.1016/j.pmedr.2019.101012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauci A.S., Redfield R.R., Sigounas G., Weahkee M.D., Giroir B.P. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321:844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- Giroir B.P. The time is now to end the HIV epidemic. Am. J. Public Health. 2020;110:22–24. doi: 10.2105/AJPH.2019.305380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant R.M., Lama J.R., Anderson P.L., McMahan V., Liu A.Y., Vargas L., Goicochea P., Casapia M., Guanira-Carranza J.V. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 2010;363:2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Bayesian perspectives for epidemiological research: I. Foundations and basic methods. Int. J. Epidemiol. 2006;35:765–775. doi: 10.1093/ije/dyi312. [DOI] [PubMed] [Google Scholar]
- Greenland S., Mansournia M.A. Penalization, bias reduction, and default priors in logistic and related categorical and survival regressions. Stat. Med. 2015;34:3133–3143. doi: 10.1002/sim.6537. [DOI] [PubMed] [Google Scholar]
- Greenland S., Mansournia M.A., Altman D.G. Sparse data bias: a problem hiding in plain sight. BMJ. 2016;352 doi: 10.1136/bmj.i1981. [DOI] [PubMed] [Google Scholar]
- Greenland S., Schwartzbaum J.A., Finkle W.D. Problems due to small samples and sparse data in conditional logistic regression analysis. Am. J. Epidemiol. 2000;151:531–539. doi: 10.1093/oxfordjournals.aje.a010240. [DOI] [PubMed] [Google Scholar]
- Hakre S., Blaylock J.M., Dawson P., Beckett C., Garges E.C., Michael N.L., Danaher P.J., Scott P.T., Okulicz J.F. Knowledge, attitudes, and beliefs about HIV pre-exposure prophylaxis among US Air Force Health Care Providers. Medicine (Baltimore) 2016;95 doi: 10.1097/MD.0000000000004511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernan M.A., Hernandez-Diaz S., Werler M.M., Mitchell A.A. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am. J. Epidemiol. 2002;155:176–184. doi: 10.1093/aje/155.2.176. [DOI] [PubMed] [Google Scholar]
- Huang Y.A., Zhu W., Smith D.K., Harris N., Hoover K.W. HIV Preexposure Prophylaxis, by Race and Ethnicity – United States, 2014–2016. MMWR Morb. Mortal. Wkly Rep. 2018 doi: 10.15585/mmwr.mm6741a3. 67:1147–5010.15585/mmwr.mm6741a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on the Changing Market, Managed Care, and the Future Viability of Safety Net Providers, 2000. The Core Safety Net and the Safety Net System, in: Ein Lewin, M., Altman, S. (Eds.), Americas's Health Care Safety Net: Intact but Endangered, Washington (DC). [PubMed]
- Krakower D.S., Oldenburg C.E., Mitty J.A., Wilson I.B., Kurth A.E., Maloney K.M., Gallagher D., Mayer K.H. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: results from a survey of healthcare providers in New England. PLoS ONE. 2015;10 doi: 10.1371/journal.pone.0132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakower D., Ware N., Mitty J.A., Maloney K., Mayer K.H. HIV providers' perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18:1712–1721. doi: 10.1007/s10461-014-0839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.S., Petersen E. Overcoming 'purview paradox' to make way for the effective implementation of PrEP in preventing HIV transmission. Int. J. Infect. Dis. 2018;77:105–106. doi: 10.1016/j.ijid.2018.10.018. [DOI] [PubMed] [Google Scholar]
- Mayer K.H., Agwu A., Malebranche D. Barriers to the wider use of pre-exposure prophylaxis in the united states: a narrative review. Adv. Ther. 2020;37:1778–1811. doi: 10.1007/s12325-020-01295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer, K. H.; Grasso C.; Levine, K.; Krakower, D.; Powell, V.; Boswell, S.L.; Marcus, J.L., 2018. Increasing PrEP Uptake, Persistent Disparities in At-Risk Patients in a Boston Center, Conference on Retroviruses and Opportunistic Infections, Seattle, WA.
- McCormack S., Dunn D.T., Desai M., Dolling D.I., Gafos M., Gilson R., Sullivan A.K., Clarke A., Reeves I. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387:53–60. doi: 10.1016/S0140-6736(15)00056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga M.J., White J.M., Krakower D.S., Biello K.B., Mayer K.H. Suboptimal awareness and comprehension of published preexposure prophylaxis efficacy results among physicians in Massachusetts. AIDS Care. 2014;26:684–693. doi: 10.1080/09540121.2013.845289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojile N., Sweet D., Kallail K.J. A preliminary study of the attitudes and barriers of family physicians to prescribing HIV preexposure prophylaxis. Kans. J. Med. 2017;10:40–42. [PMC free article] [PubMed] [Google Scholar]
- Petroll A.E., Walsh J.L., Owczarzak J.L., McAuliffe T.L., Bogart L.M., Kelly J.A. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21:1256–1267. doi: 10.1007/s10461-016-1625-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto R.M., Berringer K.R., Melendez R., Mmeje O. Improving PrEP implementation through multilevel interventions: a synthesis of the literature. AIDS Behav. 2018;22:3681–3691. doi: 10.1007/s10461-018-2184-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pleuhs B., Quinn K.G., Walsh J.L., Petroll A.E., John S.A. Health care provider barriers to HIV pre-exposure prophylaxis in the United States: a systematic review. AIDS Patient Care STDS. 2020;34:111–123. doi: 10.1089/apc.2019.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puro V., Palummieri A., De Carli G., Piselli P., Ippolito G. Attitude towards antiretroviral Pre-Exposure Prophylaxis (PrEP) prescription among HIV specialists. BMC Infect. Dis. 2013;13:217. doi: 10.1186/1471-2334-13-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins J.M. Data, design, and background knowledge in etiologic inference. Epidemiology. 2001;12:313–320. doi: 10.1097/00001648-200105000-00011. [DOI] [PubMed] [Google Scholar]
- Sales J.M., Cwiak C., Haddad L.B., Phillips A., Powell L., Tamler I., Sheth A.N. Brief report: impact of PrEP training for family planning providers on HIV prevention counseling and patient interest in PrEP in Atlanta, Georgia. J. Acquir. Immune Defic. Syndr. 2019;81:414–418. doi: 10.1097/QAI.0000000000002057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidman D., Weber S. Integrating preexposure prophylaxis for human immunodeficiency virus prevention into Women's Health Care in the United States. Obstet. Gynecol. 2016;128:37–43. doi: 10.1097/AOG.0000000000001455. [DOI] [PubMed] [Google Scholar]
- Texas Department of State Health Services, Texas HIV Surveillance Report, 2018 Annual Report, 2019, https://www.dshs.texas.gov/hivstd/reports/.
- Sharma M., Wilton J., Senn H., Fowler S., Tan D.H. Preparing for PrEP: perceptions and readiness of canadian physicians for the implementation of HIV pre-exposure prophylaxis. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0105283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler A.J., Mouhanna F., Giler R.M., Weiss K., Pembleton E., Guest J., Jones J., Castel A., Yeung H. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann. Epidemiol. 2018;28:841–849. doi: 10.1016/j.annepidem.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman, T.B., Schrimshaw, E.W., Franks, J., Hirsch-Moverman, Y., Ortega, H., El-Sadr, W.M., Colson, P.W., 2018. Response rates of medical providers to internet surveys regarding their adoption of preexposure prophylaxis for HIV: methodological implications. J. Int. Assoc. Provid. AIDS Care 17:232595821879837310.1177/2325958218798373. [DOI] [PMC free article] [PubMed]
- Singh S., Song R., Johnson A.S., McCray E., Hall H.I. HIV incidence, prevalence, and undiagnosed infections in U.S. Men who have sex with men. Ann. Intern. Med. 2018;168:685–694. doi: 10.7326/M17-2082. [DOI] [PubMed] [Google Scholar]
- Smith, D. K., Koenig, L. J., Martin, M. , Mansergh, G. , Heneine, W. , Ethridge, S. , Morgan, M., Mermin, J., Fenton, K., Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: A Clinical Practice Guide. US Public Health Service, Centers for Disease Control and Prevention, 2018a, https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf, December 8th 2018.
- Smith, D.K., Koenig, L.J., Martin, M., Mansergh, G., Heneine, W., Ethridge, S., Morgan, M., Mermin, J, Fenton, K, Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: Clinical Providers Supplement. US Public Health Service, Centers for Disease Control and Prevention, 2018b, https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-provider-supplement-2017.pdf, December 8th 2018.
- Smith D.K., Mendoza M.C., Stryker J.E., Rose C.E. PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009–2015. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan P.S., Giler R.M., Mouhanna F., Pembleton E.S., Guest J.L., Jones J., Castel A.D., Yeung H., Kramer M. Trends in the use of oral emtricitabine/tenofovir disoproxil fumarate for pre-exposure prophylaxis against HIV infection, United States, 2012–2017. Ann. Epidemiol. 2018;28:833–840. doi: 10.1016/j.annepidem.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathi A., Ogbuanu C., Monger M., Gibson J.J., Duffus W.A. Preexposure prophylaxis for HIV infection: healthcare providers’ knowledge, perception, and willingness to adopt future implementation in the southern US. South. Med. J. 2012;105:199–206. doi: 10.1097/SMJ.0b013e31824f1a1b. [DOI] [PubMed] [Google Scholar]
- Walsh J.L., Petroll A.E. Factors related to pre-exposure prophylaxis prescription by U.S. Primary Care Physicians. Am. J. Prev. Med. 2017;52:e165–e172. doi: 10.1016/j.amepre.2017.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson K., Beckett C.G., Blaylock J.M., Okulicz J.F., Scott P.T., Hakre S. Provider knowledge gaps in HIV PrEP affect practice patterns in the US Navy. Mil. Med. 2020;185:e117–e124. doi: 10.1093/milmed/usz131. [DOI] [PubMed] [Google Scholar]
- Wood B.R., McMahan V.M., Naismith K., Stockton J.B., Delaney L.A., Stekler J.D. Knowledge, practices, and barriers to HIV preexposure prophylaxis prescribing among Washington State medical providers. Sex. Transm. Dis. 2018;45:452–458. doi: 10.1097/OLQ.0000000000000781. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the authors upon reasonable request and within the limits of IRB rules.