Abstract
Hospital admissions for trampoline-related injuries are a metric of injury severity. The literature shows hospital admissions are more likely to occur from trampoline park injuries rather than home trampoline injuries. The purpose of this study was to investigate the demographics, injury characteristics, patient experiences, and economic impact of home versus trampoline park injuries requiring admission to hospital before and after two indoor trampoline parks opened in the catchment area of a Level II trauma centre. A case series research design was used. All patients who were admitted to hospital following a trampoline injury were contacted. For those who consented, clinical data was recorded from patients' charts and electronic health records. A subset of participants consented to a telephone interview wherein patient narratives were collected on the mechanism of injury, recovery process, and impact of the injury. During the study period, 15 patients required 17 hospital admissions. Twelve consented to participate in the study. Nine of the 12 required an operative intervention. Eight of the 12 were trampoline park injuries. Anatomical location of the injuries, injury type and severity scores, hospital stay, and median age were similar. The economic impact of home trampoline and trampoline park injuries varied. Overall, there were more hospital admissions and more operative interventions for trampoline park injuries during the four-year study period. Seven participants who consented to be interviewed provided additional insights into the injury experience and long-term outcomes. This study contributes to the literature on trampoline-related injuries, focusing on hospital admissions, economic impact, and adds the important perspective of patients in evaluating the effect of these injuries.
Keywords: Trampoline park injuries, Home trampoline injuries, Hospital admissions, Patient experience
Trampoline-related injuries range from minor to devastating and are well documented in the literature [[1], [2], [3]]. Trampolining has increased in popularity as evidenced by the exponential growth of indoor commercial trampoline parks, from three in 2009 to over 1000 worldwide by 2017 [4]. Media reports have raised concerns about the serious injuries and deaths that occur at indoor trampoline parks [5,6]. Hospital admissions, an indication of injury severity, are more likely to occur with trampoline park injuries (TPIs) than home trampoline injuries (HTIs) [7]. Moreover, lower extremity injuries, greater severity of injury, older age, and longer hospital stays are associated with TPIs compared with HTIs [8]. The economic burden of these injuries is also a factor. Research on trampoline-related fractures in the US over a 10-year period, found 35,773 fracture cases (9.9%) were admitted to hospital for a total cost of $257.6 million dollars [9]. A recent study of 71 TPIs that occurred over a span of 17 months in the United Kingdom reported a hospital admission rate of 25% with a total estimated cost of £20,506 for the 18 admitted cases [10].
Despite evidence of the inherent risk of trampoline use whether at home or at indoor trampoline parks, there is limited information on the costs to hospitals and the impact of these injuries on patients. The present study investigates the demographic features, injury characteristics, economic impact, and patient narratives of trampoline injuries requiring hospital admission during a four-year period in which two indoor trampoline parks opened within one month of one another in the catchment area of a 381-bed Level II trauma centre servicing approximately 232,000 people.
Methods
Research ethics board approval was granted with the inclusion criteria of any trampoline injury hospital admission between October 2014 and October 2018. This time frame was determined by the demarcation point of late October/early November 2016, the opening of two indoor trampoline parks. Exclusions were controlled settings such as school or gymnastic clubs. Study introduction letters were mailed to potential participants and consent was obtained by telephone. Interest in participating in an interview to collect narratives about the injury and the recovery was noted and separate consent was obtained. Patient demographics, injury type, body part injured, and treatment were recorded from the patients or parent/guardian and from the health record. Interviews captured the mechanism of injury and any other pertinent information related to the cause or other mitigating factors affecting to the injury and recovery. Estimated costs for medical treatment and follow-up care were calculated from resource intensity weights and physician billing codes.
Results
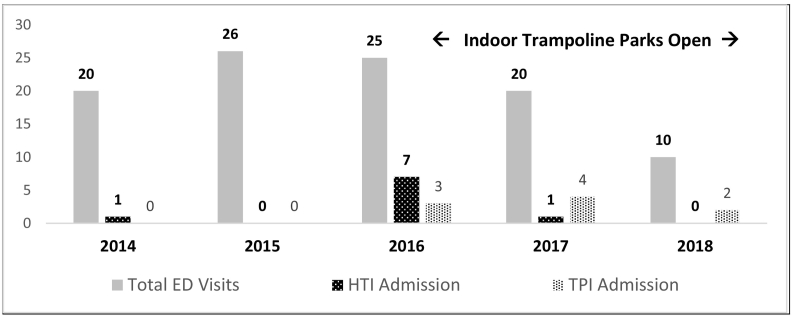
There were 82 emergency department (ED) visits by 80 patients for trampoline-related injuries from 2014 to 2018. As the location where the injury occurred is not always captured during ED admission at our institution, the exact number of trampoline injuries presenting to the ED cannot be verified and thus may be under reported. The hospital discharge abstract database does identify trampoline injuries and during the study period, 15 patients required 17 hospital admissions (two patients were admitted twice, one for two separate trampoline injuries, the other for the same injury). Fig. 1 shows trampoline injury ED visits per year from 2014 to 2018 and trampoline injury hospital admissions by injury location.
Fig. 1.
ED visits and hospital admissions for trampoline injuries by year and location; HTI = home trampoline injury; TPI = trampoline park injury.
Twelve patients and/or parents/guardians consented to participate in the study, of those seven agreed to be interviewed. Case summaries and costs are shown in Table 1 and details of the operative interventions for the nine patients requiring surgery is in Table 2.
Table 1.
Summary of trampoline injury admission cases.
| Case | Age | Gender | Body part injured | CTAS triage | Diagnosis | Mechanism of injury | ISS | OR | LoS | Cost (CAN$) |
|---|---|---|---|---|---|---|---|---|---|---|
| Home trampoline injuries | ||||||||||
| 001 | 3 | F | Tibia | 3 | Fracture | Collision | 4 | N | 2 | 4005 |
| 003 | 12 | F | Head | 2 | Concussion | Fall | 9 | N | 1 | 1873 |
| 005 | 13 | F | Tibia | 5 | Fracture | S Impact | 4 | Y | 2 | 7791 |
| 017 | 38 | M | Knee, bilateral | 2 | Rupture | S Impact | 9 | Y | 14 | 17,068 |
| Trampoline park injuries | ||||||||||
| 007 | 41 | M | Knee | 2 | Dislocation | S Impact | 16 | Y | 26 | 51,878 |
| 009 | 25 | M | Trunk | 2 | Pneumothorax | S Impact | 9 | N | 2 | 3332 |
| 010 | 19 | F | Ankle | NA | Dislocation | P impact | 9 | Y | 3 | 5920 |
| 011 | 17 | M | Knee | 2 | Fracture | S Impact | 4 | Y | 4 | 6470 |
| 013 | 13 | F | Ankle | 3 | Fracture | Fall | 4 | Y | 1 | 2502 |
| 014 | 16 | F | Ankle | 5 | Fracture | S Impact | 4 | Y | 1 | 2849 |
| 015 | 15 | F | Ankle | NA | Fracture | NA | 4 | Y | 1 | 4230 |
| 016 | 14 | M | Ankle | 5 | Fracture | NA | 4 | Y | 1 | 5411 |
Note. Age = years. CTAS = Canadian Triage and Acuity Scale: Level 1 = resuscitation; Level 2 = emergent; Level 3 = urgent; Level 4 = less urgent; Level 5 = non-urgent. ISS = injury severity score. OR = OR intervention required. LoS = length of stay in hospital, days. Cost ($C) = total cost of injury in Canadian dollars. F = female. M = male. Collision = collision with other jumper. S Impact = impact with trampoline surface. P Impact = impact with padding around trampoline bed. N = no. Y = yes. NA = not available from chart/patient.
Table 2.
Trampoline injury OR cases.
| Case | Injury location | Detailed diagnosis | Description of OR intervention | OR time (h, m) |
|---|---|---|---|---|
| 005 | Home | Tillaux fracture, right distal tibia | ORIF of the distal tibia with cannulated screw. | 0 h, 59 m |
| 007 | Park | Right knee dislocation; popliteal dissection; reperfusion syndrome | Closed reduction right knee and revascularization; revision of prosthetic graft with reversed cephalic vein from left arm; closure of lower extremity fasciotomy wounds. | 5 h, 22 m; 2 h, 41 m |
| 010 | Park | Gustilo grade II dislocation left ankle; fibula buttonholed through lateral tissues | Debridement, open left ankle dislocation; operative repair open dislocation left ankle with ligamentous suturing, capsule repair and repair of tendon sheath; injection left ankle. | 1 h, 3 m |
| 011 | Park | Right lateral true knee dislocation | Multiple ligament repair and repair of lateral meniscus including ACL, PCL, and MCL. | 1 h, 25 m |
| 013 | Park | Left bimalleolar fracture | ORIF of the left ankle with plate and screw and cannulated system. | 0 h, 45 m |
| 014 | Park | Left bimalleolar fracture with displaced lateral malleolus and non-displaced medial malleolar fractures | Operative repair left ankle fracture with compression screws. Injection of left ankle. | 1 h, 5 m |
| 015 | Park | Left ankle sprain with evulsion of the anterior tibia-fibular and calcaneal fibula ligaments and osteochondral fracture | Left ankle open repair of osteochondral defect of talus. Multiple ligament repair. Injection of left ankle. | 0 h, 58 m |
| 016 | Park | Salter-Harris ankle fracture; left distal tibia and fibula fractures | ORIF of distal tibial fracture. | 0 h, 27 m |
| 017 | Home | Bilateral patella tendon rupture | Bilateral patellar tendon repair. Repair of multiple ligaments superficial and deep medial collateral ligaments bilaterally. | 3 h, 13 m |
Note. ORIF = open reduction internal fixation. Home = home trampoline, Park = trampoline park.
Patient interviews
Case 001 (HTI, 2016) is a three-year old female with a closed tibia fracture treated non-operatively with a cast. The patient's mother was interviewed and stated she was not present when the injury occurred. She was told a group of approximately five children (ages 3–12 years) had been on a neighbour's trampoline and an older child collided with the patient, landing on her leg. The two-day hospital stay was described as uneventful. Three years later the patient is healthy and active with no long-term issues related to the injury. The mother states trampoline use is allowed as long as rules are followed, specifically one jumper at a time.
Case 005 (HTI, 2016) is a 13-year old female with a closed tibia fracture treated operatively. The patient's mother was interviewed, she recalls being at work at the time of the injury. Her daughter described jumping with two friends on their home trampoline, attempting a flip and landing awkwardly. She said her daughter's most vivid memory is the sound of the injury. After two days in hospital, the leg was serial casted for nine weeks. The mother recalled the patient's frustration with mobility limitations due to the wheelchair and being unable to see friends. Now age 16, the patient experiences pain when running or standing for long periods of time and uses an ankle brace for instability. The trampoline was removed from the backyard and the daughter is not allowed to go to trampoline parks.
Case 007 (TPI, 2017) is an anterior dislocation of the right knee with popliteal artery transection resulting from an impact with the surface of a trampoline bed. The male patient age 41 with a history of uncontrolled hypertension and GERD was taken by ambulance to the ED. The injury resulted in a hospital stay of 26 days. In the interview the patient stated the impact of the injury was life changing, as he can no longer run. His most vivid memory was the sound of the injury. He said his knee will never be 100% and he will live with this for the rest of his life. He stated he cannot be there for his family the way he could before the injury. He has vowed never to jump on a trampoline again.
Case 009 (TPI, 2017) is a spontaneous pneumothorax sustained by a 25-year old, male who reported landing on his back on the trampoline surface. The patient was otherwise healthy, with no prior pneumothorax. A chest tube was inserted in the ED and the patient was transferred to the surgical unit where he remained for two days. The patient's interview reveals an uneventful hospital stay and recovery period. One adverse issue was opioid-induced constipation, which required a visit to his local ED. The patient states no long-term injury effects and has returned to pre-injury sport and recreational activities.
Case 010 (TPI, 2017) is 19-year old female, described as healthy with no previous ankle injury. She sustained a Gustilo grade II dislocation of the left ankle after landing on the padding around the trampoline bed while playing dodgeball. She recalls the sound of the injury as a loud pop. She was three days in hospital and non-weight bearing for eight weeks. Her interview highlights the social toll of the injury as the patient had little contact with friends and limited outings as mobilizing was challenging. She returned to work three weeks after her injury with accommodations made for her non weight bearing status. Two-years post-injury, she describes fatigue after long shifts and experiences residual pain if she stands too long or rolls her ankle. She continues to jump on trampolines.
Case 014 (TPI, 2018) is a 16-year old female who lost her balance when another jumper rebounded as she was exiting the trampoline pad. She recalled hearing the crack of her ankle. She underwent surgery as was casted for five weeks. She was home schooled for one month because of mobility issues. Despite visits from friends and extended family, she says the recovery time felt extremely long. She states no lasting effect from the injury and can walk and run long distances. She cautions trampoline users to be careful and be alert.
Case 017 (HTI, 2018) is a healthy 38-year old male who sustained bilateral patella tendon ruptures having had no previous knee symptoms or pain. The patient described jumping over his young daughter and hearing a loud “crack” and feeling “everything pop” upon landing. Unable to weight bear or straight leg raise, he taken by ambulance and later underwent surgery. He describes the recovery period as long and difficult, 14 days in hospital, a wheelchair for four months, and leg braces for three months. He states the injury had a lasting impact on his family, work, and sports. One year later, he describes some activities of daily living as challenging. He states while his overall health his good, his knees are only 70%. He recommends being very careful on trampolines, especially for those who are older.
Discussion
During the study time frame, there were eight home trampoline injury (HTI) and nine indoor trampoline park injury (TPI) hospital admissions. There were more operative interventions for TPIs versus HTIs. Although the median age of those admitted was slightly older for TPIs (16.5 years versus 12.5 years), the anatomical location of the injuries, injury type and severity scores, and length of stay were similar. Comparisons of overall health system costs of HTIs versus TPIs are difficult because we lack information on the four HTIs and one TPI that did not participate in the study. The total cost per case for HTIs ranged from $1873 to $17,068 and $2502 to $51,878 for TPIs. Comparing the lowest case costs, the TPI was 29% higher, for mid-range case costs, the HTI was 18% higher, and for the highest case costs, the TPI was 101% higher. There is a paucity in the literature investigating the impact of trampoline injuries on patients, the interviews included here address this issue and contribute additional insights. Many patients vividly described the sound of their injuries. Four of the seven patients interviewed continue to have ongoing issues with pain and mobility. Limitations of the study include an incomplete narrative of the patients' experience of trampoline injuries as only seven of the 12 agreed to be interviewed and incomplete date as only 12 of the 17 consented for the study. However, the information collected does show the risks and the potential lasting effects of these injuries from both home trampolines or trampoline parks. It is noteworthy that both indoor trampoline parks are now closed, one prior to the COVID-19 pandemic and the other likely as a result of the pandemic. This study, focusing specifically on hospital admissions, adds to the literature on trampoline injuries by outlining the economic impact on the hospital system, and the important, yet often under-reported perspective of patients who experience and live with the long term effects of these injuries.
Acknowledgements
Shelly Wilbur and Dr. Bryn Robinson of Horizon Health Network for injury cost data.
Research grants were received from the Atlantic Provinces Orthopaedic Society and the New Brunswick Trauma Program. There was no involvement by these funders in the study design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
References
- 1.Canadian Paediatric Society, Canadian Academy of Sports . vol. 12. 2007. Position Statement: Trampoline Use in Homes and Playgrounds. [Google Scholar]
- 2.Kasmire K.E., Rogers S.C., Sturm J.J. Trampoline park and home trampoline injuries. Pediatrics. 2016;138(3):e20161236. doi: 10.1542/peds.2016-1236. [DOI] [PubMed] [Google Scholar]
- 3.Rao D.P., McFaull S.R., Cheesman J., Do M.T., Purcell L.K., Thompson W. The ups and downs of trampolines: Injuries associated with backyard trampolines and trampoline parks. Paediatr. Child Health. 2018:1–7. doi: 10.1093/pch/pxy066. (May) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.International Association of Trampoline Parks International Association of Trampoline Parks (IATP) Statement in Response to Incident at Extreme Air Park. 2018. http://c.ymcdn.com/sites/www.indoortrampolineparks.org/resource/resmgr/docs/IATP_Statement_in_response_t.pdf
- 5.Proctor J. “They are very dangerous”: Trampoline Park Death Highlights Calls for Regulation. CBC News British Columbia. January 25, 2018. http://www.cbc.ca/news/canada/british-columbia/trampoline-injuries-death-regulation-1.4504378
- 6.Ross A. “He's determined to walk out of here”: Teen Breaks Neck at Trampoline Park. CBC News Edmonton. January 11, 2017. http://www.cbc.ca/news/canada/edmonton/he-s-determined-to-walk-out-of-here-teen-breaks-neck-at-trampoline-park-1.3929347
- 7.Mulligan C.S., Adams S., Brown J. Paediatric injury from indoor trampoline centres. Inj. Prev. 2016:352–354. doi: 10.1136/injuryprev-2016-042071. [DOI] [PubMed] [Google Scholar]
- 8.Roffe L., Pearson S., Sharr J., Ardagh M. The effect of trampoline parks on presentations to the Christchurch Emergency. New Zeal Med. Assoc. J. 2018;131(1468):43–53. [PubMed] [Google Scholar]
- 9.Loder R.T., Schultz W., Sabatino M. Fractures from trampolines: results from a national database, 2002 to 2011. J. Pediatr. Orthop. 2014;34(7):683–690. doi: 10.1097/BPO.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 10.Jordan S.J., To C.J., Shafafy R., Davidson A.E., Gill K., Solan M.C. Trampoline park injuries and their burden on local orthopaedic and emergency services. Bull. Emerg. Trauma. 2019;7(2):162–168. doi: 10.29252/beat-070212. [DOI] [PMC free article] [PubMed] [Google Scholar]