Abstract
This paper describes a case of papulonecrotic tuberculid after Bacille Calmette-Guerin (BCG) vaccination. A 6-month-old boy was seen in our emergency room with a fever and erythematous papular. He received BCG vaccination at the age of 5 months and there were no systemic problems after the vaccination. There were no abnormal physical findings except for skin lesions and fever. Histopathologically, the lesion was associated with pyogenic granulomatous inflammation and fibrosis, with multiple instances of vascularization and infiltration of various inflammatory cells. Acid-fast stain, culture,and polymerase chain reaction for tuberculous bacillus DNA of the papulonecrotic skin lesions were negative. He was diagnosed papulonecrotic tuberculid caused by BCG vaccination. The fever lasted 10 days, and all lesions healed spontaneously in 2 months. Papulonecrotic tuberculid is a vasculitis caused by an allergic reaction to an internal focus of Mycobacterium tuberculosis or its metabolites. The appearance of an unexplained skin rash may cause parental anxiety, nevertheless the disease may require no treatment unless the patient is immunocompromised. It is necessary to improve awareness regarding the disease as a side effect of BCG vaccination.
Keywords: BCG vaccination, Papulonecrotic tuberculid, Erythematous papular lesions, Papulonecrotic skin lesions, Tokyo-172 BCG vaccination complications
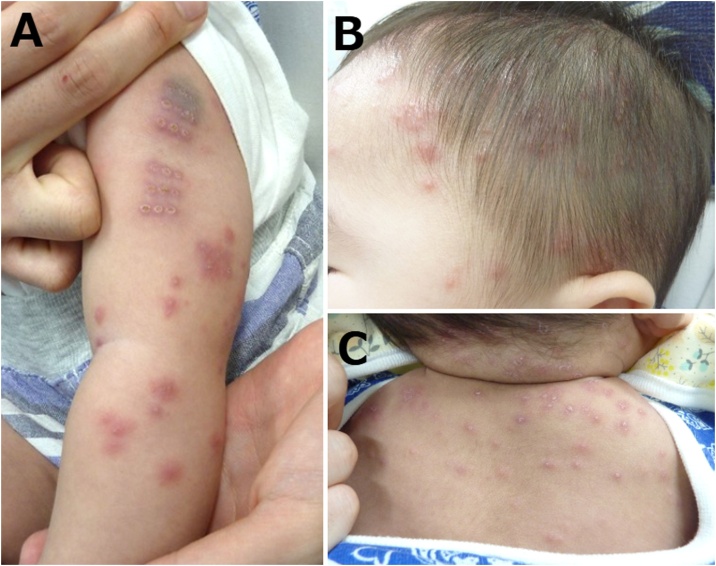
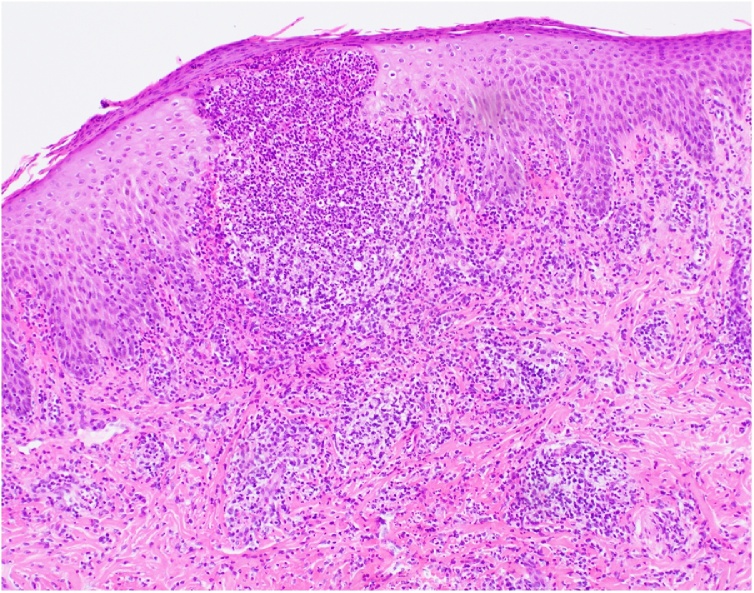
This report describes a case of papulonecrotic tuberculid after Bacille Calmette-Guerin (BCG) Tokyo-172 vaccination. The patient was a 6-month-old boy seen in our emergency room for a complaint of fever and generalized erythematous papular lesions 1 month after BCG vaccination. The boy was born at 40 weeks’ gestation with a body weight of 3148 g. His growth and development corresponded to his age. He received BCG vaccination on the left arm at the age of 5 months, and there were no systemic problems after the vaccination. In the emergency room, there were no abnormal physical findings except for skin lesions and fever. The patient had developed several small papulonecrotic lesions on the right upper limb, which had spread to the entire trunk as well as the face, head, and limbs at 35 days post-vaccination (Fig. 1). There was no superficial lymph node swelling. Histopathologically, the lesion was associated with pyogenic granulomatous inflammation and fibrosis with vasculitis, without acantholysis of the epidermal layer of the skin. There was a nodular lesion in the dermis and subcutaneous adipose tissue surrounding the hair follicle, with multiple instances of vascularization and infiltration of various inflammatory cells (Fig. 2). There was no family history of pulmonary tuberculosis, and a chest radiograph was normal. Acid-fast stain and culture of the papulonecrotic skin lesions were negative. Polymerase chain reaction for tuberculous bacillus DNA was negative. We diagnosed the patient as having papulonecrotic tuberculid caused by BCG vaccination. We considered varicella as the differential diagnosis in this case. However, the lesion was not associated with bullae, and there was no elevated varicella IgM, which ruled out varicella. The fever lasted 10 days, and all lesions healed spontaneously in 2 months.
Fig. 1.
Disseminated erythematous papules. A. Site of vaccination on the left limb; B. Head and Face; C. Neck and Back.
Fig. 2.
Pyogenic granulomatous inflammation and fibrosis.
Cutaneous lesions are the most frequent complications of BCG vaccination [1,2]. Papulonecrotic tuberculid is a vasculitis caused by an allergic reaction to an internal focus of Mycobacterium tuberculosis or its metabolites [[3], [4], [5]]. However, the pathogenesis of papulonecrotic tuberculid after BCG vaccination is still poorly understood. The appearance of an unexplained skin rash may cause parental anxiety; however, the disease may require no treatment unless the patient is immunocompromised, and this case required no treatment at all. There have been few reports of papulonecrotic tuberculid caused by BCG vaccination; it is, therefore, necessary to improve awareness regarding the disease as a side effect of BCG vaccination.
Contributions
KA, II, and TA managed the patient. KA and MM wrote and edited the manuscript. All authors have read and approved the final manuscript.
Consent for publication
Written informed consent was obtained from the parents of the patient for the publication of this report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Kotaro Araki: Project administration, Supervision, Writing - review & editing. Itsuki Inamine: Project administration, Supervision, Writing - review & editing. Takeo Aoki: . Miyuki Magota: Writing - original draft, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
We are grateful to Ikemoto for managing the patient.
Contributor Information
Kotaro Araki, Email: kotaro002@gmail.com.
Itsuki Inamine, Email: itkinm29@gmail.com.
Takeo Aoki, Email: aoki.takeo@taupe.plala.or.jp.
Miyuki Magota, Email: miyumagomago@gmail.com.
References
- 1.Bellet J.S., Prose N.S. Skin complications of Bacillus calmette-Guerin immunization. Curr Opin Infect Dis. 2005;18:97–100. doi: 10.1097/01.qco.0000160895.97362.4f. [DOI] [PubMed] [Google Scholar]
- 2.Figueiredo A., Poiares-Baptista A., Branco M., da Mota H.C. Papular tuberculids post-BCG vaccination. Int J Dermatol. 1987;26:291–294. doi: 10.1111/j.1365-4362.1987.tb00191.x. [DOI] [PubMed] [Google Scholar]
- 3.Morrison J.G., Fourie E.D. The papulonecrotic tuberculide. From Arthus reaction to lupus vulgaris. Br J Dermatol. 1974;91:263–270. doi: 10.1111/j.1365-2133.1974.tb12894.x. [DOI] [PubMed] [Google Scholar]
- 4.Brinca A., Andrade P., Vieira R., Figueiredo A. Papulonecrotic tuberculid: report of a clinical case. Dermatol Reports. 2011;3:e29. doi: 10.4081/dr.2011.e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tirumalae R., Yeliur I.K., Antony M., George G., Kenneth J. Papulonecrotic tuberculid-clinicopathologic and molecular features of 12 Indian patients. Dermatol Pract Concept. 2014;4:17–22. doi: 10.5826/dpc.0402a03. [DOI] [PMC free article] [PubMed] [Google Scholar]