Abstract
Immigration detention centers are densely populated facilities in which restrictive conditions limit detainees’ abilities to engage in social distancing or hygiene practices designed to prevent the spread of COVID-19. With tens of thousands of adults and children in more than 200 immigration detention centers across the United States, immigration detention centers are likely to experience COVID-19 outbreaks and add substantially to the population of those infected.
Despite compelling evidence indicating a heightened risk of infection among detainees, state and federal governments have done little to protect the health of detained im-migrants. An evidence-based public health framework must guide the COVID-19 response in immigration detention centers.
We draw on the hierarchy of controls framework to demonstrate how immigration detention centers are failing to implement even the least effective control strategies. Drawing on this framework and recent legal and medical advocacy efforts, we argue that safely releasing detainees from immigration detention centers into their communities is the most effective way to prevent COVID-19 outbreaks in immigration detention settings. Failure to do so will result in infection and death among those detained and deepen existing health and social inequities.
As of September 3, 2020, the Centers for Disease Control and Prevention (CDC) has reported 185 092 deaths and over six million infections in the United States due to the novel coronavirus, SARS-CoV-2.1 Both the CDC and the World Health Organization declared COVID-19, the disease caused by SARS-CoV-2, a pandemic.2 The patchwork of US national, state, and local responses to the pandemic has left vulnerable populations unprotected and highly susceptible to the virus and to developing COVID-19. Not surprisingly, COVID-19 cases and deaths are concentrated in low-income communities of color,3 reflecting the powerful influences of the social determinants of health and the enduring structural inequities that are exacerbated by the pandemic. There are several types of settings—including prisons, meatpacking plants, and nursing homes—in which population density and unsanitary conditions have led to large, concentrated outbreaks of infection.4
In the United States, tens of thousands of adults and children held in over 200 immigration detention centers are uniquely vulnerable to coronavirus outbreaks. The most recent data from Immigration and Customs Enforcement (ICE) show that in 2019, the average length of stay in ICE detention centers was 46 days.5 Most people in immigration detention centers are held in facilities operated by private companies, often in decommissioned jails or prisons.6 Conditions in many detention centers have historically been found to be quite poor—with overcrowding, subpar medical care, and the presence of environmental hazards—according to investigations by the media, watchdog organizations, and the Department of Homeland Security (DHS) Office of Inspector General.7 In addition, infectious disease outbreaks in these facilities are common.8 The prevalent conditions of overcrowding and medical neglect are directly relevant to attempts to control outbreaks of COVID-19. An evidence-based public health framework must guide the COVID-19 response in immigration detention centers.
In this commentary, we draw on the hierarchy of controls framework to argue that safely releasing detainees from immigration detention centers into their communities is the most effective way to prevent the spread of COVID-19 in these settings. Failure to do so will result in infection and death from a novel communicable disease and deepen inequities for a population group that already experiences many structural and systemic threats to health and well-being.9
EVIDENCE-BASED FRAMEWORK TO CONTROL COVID-19
The hierarchy of controls framework,10 often used in occupational safety, is a useful framework for classifying different approaches to controlling hazard exposures, including infectious pathogens. The framework has previously been used to discuss infection control for staff and inmates in carceral settings.11 The framework guides attention and focus for mitigating risk when unrelated individuals are sharing spaces and engaging in group activities by identifying multiple levels of strategies for controlling hazards. These strategies include the use of personal protective equipment (PPE), administrative controls that change the day-to-day workflow of the environment, engineering controls that isolate people from the hazard, and elimination or removal of the hazard from the physical environment (Figure 1). The controls on the bottom of the pyramid, such as the use of PPE, are least effective, whereas the controls at the top of the pyramid are most effective.
FIGURE 1—
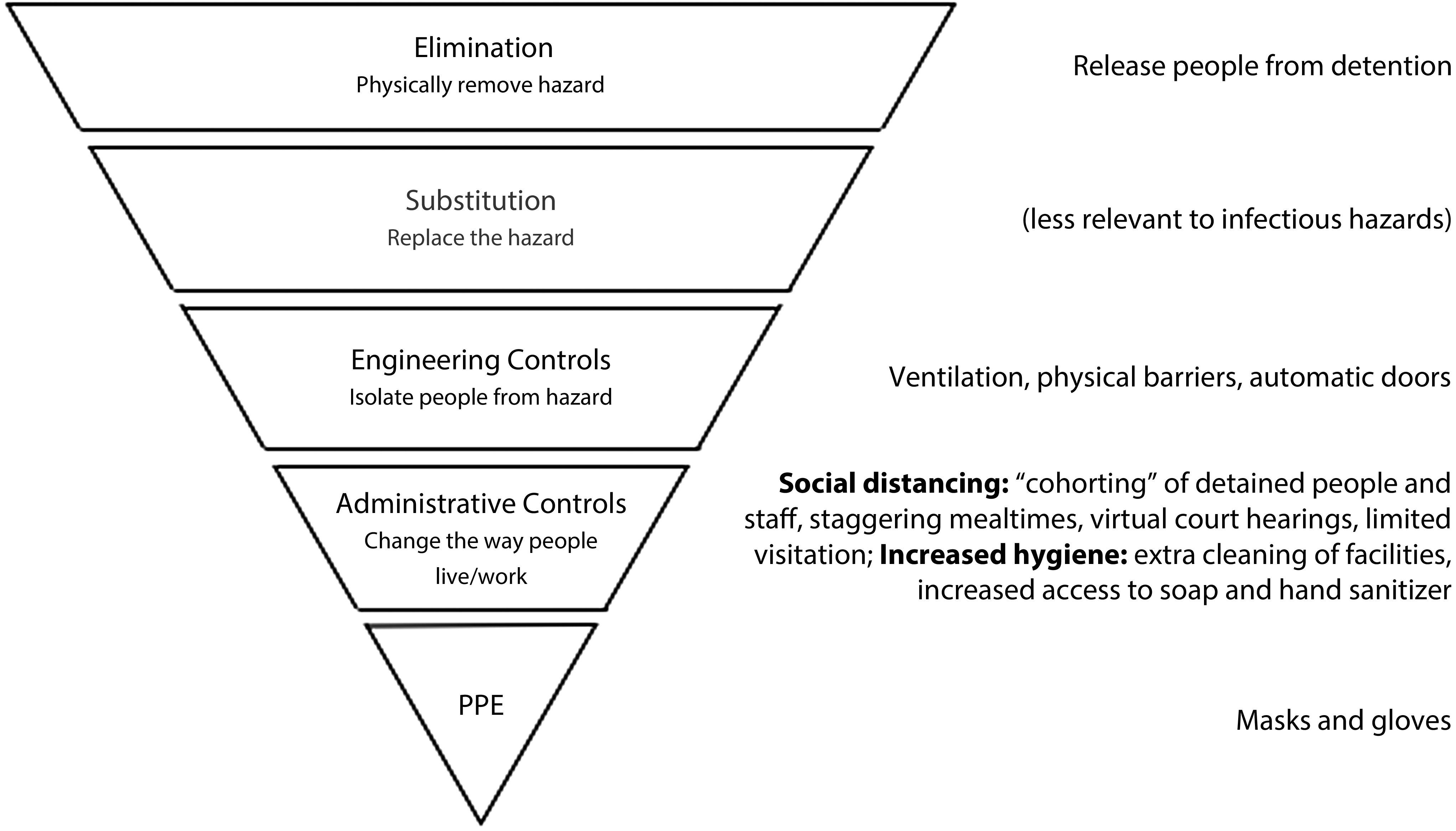
Effectiveness of COVID-19 Controls in Immigration Detention Settings
Note. PPE = personal protective equipment. Figure presents a hierarchy of controls as applied to COVID-19 control in immigration detention. The width of the pyramid corresponds to the effectiveness of the control strategy.
Source. Adapted from the National Institute of Occupational Safety and Health (https://www.cdc.gov/niosh/topics/hierarchy/default.html).
COVID-19 as a Hazard in Detention Centers
The virus that causes COVID-19 is highly contagious. A recent meta-analysis found an R0 (the basic reproduction number of a virus) of 2.79 for novel coronavirus, meaning that one infected person—in a completely susceptible population in a community setting—would infect nearly three people.12 A separate study estimated a median R0 of 5.7.13 Seasonal influenza, by contrast, has an average R0 of 1.3,14 suggesting that SARS-CoV-2 is multiple times more contagious than seasonal influenza. The context in which the transmission occurs affects the basic reproduction number, leading to more secondary infections in densely populated settings. One study that modeled R0 after the outbreak on the Diamond Princess, a densely populated cruise ship, estimated R0 to be an astonishingly high 14.8.15
Immigration detention centers—the largest of which are repurposed jails or prisons now run by private contractors6—have space and population densities similar to those of cruise ships, but have poor conditions of confinement alongside frequently documented detainee neglect.6,7 Often overcrowded, generally with shared communal living, eating, and lavatory spaces, little capacity for hygienic practices, and frequent interaction between guards, staff, and detainees, detention center conditions aggravate the risk of SARS-CoV-2 infection. One study16 modeled the growth of SARS-CoV-2 cases in immigration detention centers, finding that optimistically assuming an R0 of 2.5, between 72% and 80% of detainees could become infected within 90 days. As of September 2,, 2020 at 2:15 pm, ICE reported that 5416 individuals currently or formerly in ICE custody and 45 ICE employees working in immigration detention centers had tested positive for COVID-19 (employee infection rate updated as of June 18, 2020). Six detainees have died after testing positive for SAR-CoV-2.17
Stopping the Spread of COVID-19
Viewed through the hierarchy of controls framework, COVID-19 control measures thus far applied—such as separating groups of detainees, limiting visitors, providing PPEs, and changing cleaning practices—have focused on administrative controls, which are located at the lower, less effective end of the control pyramid.10 These measures have been central to the broader public health approach to containing the spread of SARS-CoV-2; when properly implemented in other settings, they have significantly reduced the risk of virus spread from both symptomatic and asymptomatic carriers. However, they are extremely challenging to implement in the densely populated infrastructure of immigration detention centers specifically designed to decrease distance between detainees to facilitate surveillance. Further, even if these measures were feasible, ICE’s previous track record of failing to implement hygiene practices casts doubt on its ability to effectively implement even the most basic PPE and administrative controls. Prior to the COVID-19 pandemic, the DHS Office of Inspector General reported numerous health standards violations in ICE detention centers, including spoiled food, inadequate medical facilities, dilapidated bathrooms, and lack of clothing and hygiene items.7 If this is any indication of ICE’s ability to effectively implement the most basic controls—already the least effective methods of infection control—infection rates in immigration detention centers are likely to increase rapidly among the detained population.
Finally, in places with vulnerable populations under space constraints, such as immigration detention centers, regular, frequent testing for SARS-CoV-2 can provide early warning of an outbreak and is a crucial part of disease control.18 This is particularly important because a spike in coronavirus infections among detainees would likely overwhelm immigration detention centers’ medical facilities, which lack the capacity and necessary supplies to handle such outbreaks. Immigration detention centers would thus be forced to rely on community hospitals and health care facilities, contributing to the mounting stress on nearby medical institutions. This could be especially catastrophic in rural and remote areas, where many immigration detention centers are located. One study found that outbreaks in only 7% of ICE facilities would overwhelm intensive care unit beds within a 50-mile radius of those facilities over a 90-day period.16
Release Detainees Into Safe Environments
Given the barriers to effective implementation of PPE and administrative controls to prevent the spread of SARS-CoV-2 in immigration detention centers, an evidence-based public health approach suggests moving up the hierarchy of controls to more effective measures. Engineering controls, such as added ventilation, negative pressure rooms, building additional cells that house only one person, or the use of alternative spaces such as trailers and automatic doors, are expensive, difficult to implement quickly, and highly unlikely because of the profit-maximization missions of the corporations that operate many immigration detention centers. Thus, the public health response to the pandemic must include COVID-19 controls in the “elimination” level of the hierarchy of controls. Specifically, we advocate for the release of detainees from immigration detention centers, as this strategy will reduce the likelihood of person-to-person infection and enhance the possibility of engaging in meaningful social distancing and hygienic practices as directed by the CDC. In other similar settings, such as prisons and jails, corrections officials have suggested the release of incarcerated individuals as a critical step in preventing the spread of SARS-CoV-2, and several states have released thousands of prisoners over the past few months.19 Immigration detention centers should follow suit to prevent and reduce the scale of outbreaks of COVID-19.
We do not advocate for selective release or mass deportation of detainees as infection control measures. Selective release can be inconsistent, arbitrary, and discriminatory. Additionally, selective release would be insufficient to prevent outbreaks, as detention centers are specifically designed to cluster populations in spaces that allow for efficient surveillance and control. Similarly, mass deportation to prevent outbreaks of COVID-19 is not only inhumane, potentially accelerating the spread of SAR-CoV-2 to vulnerable communities abroad, but is also not permissible under the legal protections afforded to immigrants in deportation proceedings: deportation is generally the result of an administrative determination regarding a detainee’s status in the United States, and immigration enforcement officials cannot simply subvert this process. Accordingly, our recommendation for the release of detainees not only comports with established, evidence-based public health practice but is also consistent with current law.
There are concerns that the conditions into which detainees would be released would not eliminate the risk of SARS-CoV-2 exposure in their communities. Although it is true that moving from detention to a community setting would not eliminate risk of infection entirely, individuals can more safely isolate and engage in social distancing and hygiene practices in community settings, and could seek diagnostic testing or––should they become infected––health care from nonprofit organizations, charitable clinics, or community health centers that are better resourced than immigration detention centers.
Others have warned about “spillover” infections from immigration detention centers to receiving communities.20 But this spillover risk is already occurring: first, as guards and staff commute from immigration detention centers to home communities, and secondly, during transfers of detainees from one detention center to another. ICE has reported21 that they do not test detainees prior to transfer unless detainees present symptoms of SARS-CoV-2 infection (although, reportedly, the symptom screening practiced by ICE is not comprehensive and may miss individuals presenting with less common coronavirus symptoms). This has resulted in the transfer of asymptomatic individuals to other facilities, or of those with less common symptoms, resulting in more outbreaks. In Broward County, Florida, for example, of 33 detainees recently transferred from detention in Miami–Dade County, 16 later tested positive.21 In one recent study,20 researchers highlighted the benefits of prison release for low-risk offenders, and further considered the relationship between “jail cycling”—or arrest and subsequent cycling in and then out of jails while awaiting hearings and trial—and community infection rates of SARS-CoV-2 at the zip code level in Chicago. The authors found that this jail cycling is associated with nearly 16% of all documented COVID-19 cases in Illinois. These findings are relevant to the current commentary for two reasons. First, the authors do not interpret these data as illustrative of the risks posed by the release of those incarcerated, but rather of the community risk created by the incarceration system: “[A]s arrested individuals are exposed to high-risk spaces for infection in jails and then later released to their communities, the criminal justice system is turning them into potential disease vectors for their families, neighbors, and, ultimately, the general public.”20(p1417) In the current case, immigration detention is not only creating “potential disease vectors” for communities in the United States, but also transporting these infections abroad by continuing to deport immigrants without protective measures in place.22 Secondly, DHS has discretion to release many immigration detainees while the administrative proceedings regarding their civil immigration status are pending; immigration proceedings are not a direct analog to criminal proceedings and operate independently of any state or federal criminal proceedings.
Yet it is certainly possible for infections to move from immigration detention centers to communities upon release. Thus, releasing detainees must be done safely and with appropriate public health guidelines in place. Although a full description of efforts to increase the safety of detainee release is beyond the scope of this commentary, guidelines from the Women’s Refugee Commission, in collaboration with Physicians for Human Rights and Freedom for Immigrants, has been publicly available.23 The guidelines—written for both ICE and receiving communities—consider preparation of medical documentation, health and treatment summaries, communication with lawyers and sponsors about symptoms, suggestions for appropriate preventive measures prior to release, safe transportation from detention to community settings, and risk mitigation strategies at the final destination. Notably, the recommendations argue that “Release should not be halted if the individual is showing symptoms, because release will facilitate isolation and prevent further spread within the detention center and the community.”23
Release Detainees for Public Health
Detainees and their advocates have taken social and legal action to promote release from detention centers; yet although apprehensions and detention numbers have declined, relatively few immigrants have been released as a result of these efforts. These efforts have included encouraging congressional committees with jurisdiction over the DHS to engage in oversight that protects detainees, as well as filing complaints with the DHS Office for Civil Rights and Civil Liberties and the DHS Office of Inspector General. Advocates and detainees have also made requests for bond redetermination or parole in the cases of those who might be eligible for discretionary release. In federal courts, litigation efforts range from individual petitions challenging the legality of continued detention in light of the COVID-19 pandemic to complex class action cases seeking broader release or reform. At the state and local level, advocacy efforts have also included pressure on state policymakers and local law enforcement to stop all transfers to ICE during the pandemic. Further, there are readily available evidence-based alternatives to detention through which community-based organizations provide support and guidance to immigrants as they navigate court appointments and other aspects of their immigration case while living in their communities. Regardless of such programs, data show high rates of hearing attendance generally; a recent review of immigration court data from 2008 to 2018 found that 83% of immigrants who were not detained attended all their hearings.24
In the current political climate, the COVID-19 pandemic has exacerbated immigrant communities’ existing vulnerabilities. The federal government has leveraged the pandemic to enforce increasingly restrictive immigration policies, including the deportation of migrant children, effectively closing the US land borders, suspending visa processing, and attempting to bar international students from using student visas if their course instruction moved online. These efforts subordinate public health–focused interventions to address the pandemic. Accordingly, reducing the detained population is not only a logical, public health–oriented, and humane next step necessary to save lives,25 but it also combats political efforts to use the pandemic as a mechanism for expanding aggressive immigration enforcement efforts. Releasing detainees is a public health imperative.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Centers for Disease Control and Prevention. Cases in the US. September 3, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed September 4, 2020.
- 2.World Health Organization. Preparedness, prevention and control of COVID-19 in prisons and other places of detention. March 15, 2020. Available at: http://www.euro.who.int/__data/assets/pdf_file/0019/434026/Preparedness-prevention-and-control-of-COVID-19-in-prisons.pdf?ua=1. Accessed July 10, 2020.
- 3.Garg S, Kim L, Whitaker M et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frieden TR, Lee CT. Identifying and interrupting superspreading events—implications for control of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(6):1059–1066. doi: 10.3201/eid2606.200495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dias I. ICE is detaining more people than ever—and for longer. Pacific Standard. August 1, 2019. Available at: https://psmag.com/news/ice-is-detaining-more-people-than-ever-and-for-longer. Accessed July 10, 2020.
- 6.Cho EH, Tidwell Cullen T, Long C. Justice-free zones: US immigration detention under Trump. ACLU Research Report. 2020. Available at: https://www.hrw.org/sites/default/files/supporting_resources/justice_free_zones_immigrant_detention.pdf. Accessed September 4, 2020.
- 7.Office of the Inspector General. Concerns about ICE detainee treatment and care at four detention facilities. June 3, 2019. Available at: https://www.oig.dhs.gov/sites/default/files/assets/2019-06/OIG-19-47-Jun19.pdf. Accessed September 4, 2020.
- 8.Leung J, Elson D, Cloud B et al. Mumps in detention facilities that house detained migrants—United States, September 2018–April 2019. Open Forum Infect Dis. 2019;6(suppl 2):S589–S590. doi: 10.1093/ofid/ofz360.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ornelas IJ, Yamanis TJ, Ruiz RA. The health of undocumented Latinx immigrants: what we know and future directions. Annu Rev Public Health. 2020;41(1):289–308. doi: 10.1146/annurev-publhealth-040119-094211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The National Institute for Occupational Safety and Health. Hierarchy of controls: overview. January 13. 2015. Available at: https://www.cdc.gov/niosh/topics/hierarchy/default.html. Accessed July 10, 2020.
- 11.Francis J. Curry National Tuberculosis Center and California Dept of Health Services. Tuberculosis infection control plan template for jails. 2002. Available at: http://www.tb-ipcp.co.za/downloads/training/files/buildingDesign_2012/References/FJCurry_2002_TBICPlanTemplateforJails.pdf. Accessed September 4, 2020.
- 12.Liu Y, Gayle AA, Wilder-Smith A, Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa021. ):taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biggerstaff M, Cauchemez S, Reed C, Gambhir M, Finelli L. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature. BMC Infect Dis. 2014;14:480. doi: 10.1186/1471-2334-14-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocklöv J, Sjödin H, Wilder-Smith A. COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. J Travel Med. 2020;27(3) doi: 10.1093/jtm/taaa030. :taaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Irvine M, Coombs D, Skarha J et al. Modeling COVID-19 and impacts on US Immigration and Enforcement (ICE) detention facilities, 2020. J Urban Health. 2020;97(4):439–447. doi: 10.1007/s11524-020-00441-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.US Immigration and Customs Enforcement. ICE guidance on COVID-19. September 2, 2020. Available at: https://www.ice.gov/coronavirus. Accessed September 4, 2020.
- 18.Malloy GSP, Puglisi L, Brandeau ML, Harvey TD, Wang EA. The effectiveness of interventions to reduce COVID-19 transmission in a large urban jail. medRxiv. doi: 10.1101/2020.06.16.20133280. June 18, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prison Policy Initiative. Responses to the COVID-19 pandemic. May 12, 2020. Available at: https://www.prisonpolicy.org/virus/virusresponse.html. Accessed May 12, 2020.
- 20.Reinhard E, Chen D. Incarceration and its disseminations: COVID-19 pandemic lessons from Chicago’s Cook County Jail. Health Aff. 2020. Epub ahead of print June 4, 2020. [DOI] [PubMed]
- 21.Madan MO. ICE admits to transferring detainees with COVID-19, says it can’t test everybody. Miami Herald. May 27, 2020. Available at: https://www.miamiherald.com/news/local/immigration/article243031176.html. Accessed July 20, 2020.
- 22.Blitzer J. The Trump administration’s deportation policy is spreading the coronavirus. The New Yorker. May 13, 2020. Available at: https://www.newyorker.com/news/daily-comment/the-trump-administrations-deportation-policy-is-spreading-the-coronavirus. Accessed July 20, 2020.
- 23.Women’s Refugee Commission. Recommendations for safe release procedures from immigration detention during the COVID-19 pandemic. May 28, 2020. Available at: https://www.womensrefugeecommission.org/research-resources/recommendations-safe-release-procedures-immigration-detention-covid-19. Accessed July 20, 2020.
- 24.Eagly I, Shafer S. Measuring in absentia removal in immigration court. U Penn Law Rev. 2020;168(4):817–876. Available at: https://www.pennlawreview.com/wp-content/uploads/2020/06/Eagly-Shafer_Final.pdf. Accessed November 4, 2020. [Google Scholar]
- 25.Ferrer B. Immigrant health: anchoring public health practice in a justice framework. Am J Public Health. 2019;109(9):1156–1157. doi: 10.2105/AJPH.2019.305235. [DOI] [PMC free article] [PubMed] [Google Scholar]


