The important and timely article “Optimal Allocation of Societal HIV-Prevention Resources to Reduce HIV Incidence in the United States” by Sansom et al. (p. 150) models different federal and private HIV-prevention resource allocation strategies to prioritize HIV funding through 2027. Modeling exercises are useful starting points for decision making yet may not fully incorporate real-world complexities because of model assumptions and limited quantifiable inputs. Models provided exclude multilevel interventions, policy and structural-level initiatives, and within-group cost differentiation, all key considerations for affecting communities at highest risk for HIV infection.
Sansom et al. punctuate the misalignment between epidemic burden and resource allocation. Current allocations for HIV screening among low-risk heterosexuals constitute 25.3% of the total prevention budget and are 22 times greater than funds earmarked for high-risk men who have sex with men (MSM). MSM accounted for 69% of incident HIV diagnoses in 2018, more than seven times the number of new HIV diagnoses of heterosexual sex.1 Within MSM, Black or Latinx MSM account for 67% and MSM younger than 35 years account for 65% of new diagnoses. New infections are concentrated in the South. The Ending the HIV Epidemic strategy is an important step forward in directing HIV-prevention resources to jurisdictions experiencing the highest HIV burdens.2 Although the most likely (limited reach) scenario modeled by Sansom et al. begins this process of resource realignment, we advocate more intentional rectification of these misalignments by redistributing HIV-prevention resources so they reach the populations most at risk: young Black and Latinx MSM and transgender women (transwomen).
The Pareto principle applies to the current HIV epidemic in the United States: a small proportion of people—Black and Latinx MSM and transwomen younger than 35 years, accounting for less than 1% of the US population—experience a large proportion (> 30%) of new cases.1 Populations with the highest HIV burden in the United States face intersecting social–structural stigma (intersectional stigma), including racism and homo-, bi-, and transphobia, creating a cycle in which stigma increases risk and disease burden exacerbates stigma. Structural inequities, including poverty, health insurance deficits, homelessness, unemployment, discrimination, and incarceration are implicated in worse HIV-prevention and care outcomes. Social stigma inhibits provision and uptake of HIV prevention and care; experiences and anticipation of stigma in health care settings are associated with lower rates of HIV testing, preexposure prophylaxis uptake, retention in care, and antiretroviral therapy adherence. Thus, relying solely on biomedical HIV prevention for young Black and Latinx gay and bisexual men and transwomen will not constitute a sufficient response to their needs.
Historically, allocative misalignments result in underservice on the ground. For example, a statewide review of Pennsylvania HIV-prevention monitoring data from 2007 through 2010 uncovered a critical gap in service: young Black MSM and transwomen received 0.8% of state-funded HIV-prevention interventions while accounting for more than 20% of total cases during that period. In response, local researchers collaborated with local sexual and gender minority youths of color to develop, implement, and evaluate a multilevel HIV-prevention and care intervention.3
The Pennsylvania Department of Health and the state’s HIV Planning Group, whose composition has robustly included most-at-risk populations empowered to identify priority populations and recommend resource allocations, supported and promoted the project for statewide scale-up. However, historical underservice created implementation capacity deficiencies that persisted even when allocations were realigned to reflect underserved communities’ epidemic burden. Citing their lack of capacity to engage with “hard-to-reach” populations, few organizations applied for pilot funding to diffuse this model. One health services organization director wrote:
There are several core components of the intervention that we do not meet, particularly related to asset-based youth development, agency buy-in and support, and competency in programming designed specifically for Black and Latino populations. (personal e-mail communication, June 14, 2016)
A Ryan White Coalition director wrote, “I have not been able to identify a provider who wants to consider this” (personal e-mail communication, June 17, 2016). Populations are only hard to reach if no one tries to reach them.
Coordinated, combination interventions that include biomedical components and address multiple social ecological levels continue to be essential: preexposure prophylaxis is not housing, antiretroviral therapy is not a job, and linkage to care interventions do not supplant the need for sustained social capital. Emerging research incorporating wraparound clinical harm reduction4 and intersectional stigma reduction5 into biomedical HIV prevention shows promise. Because of their complexity, such interventions are difficult to operationalize, field, and consolidate into cost-per-person metrics; for these reasons, multilevel, social determinants-based interventions are excluded from allocation models provided. Models disregarding larger social and structural determinants, such as economic inequality, retain biomedical concision at the cost of epidemiological myopia.
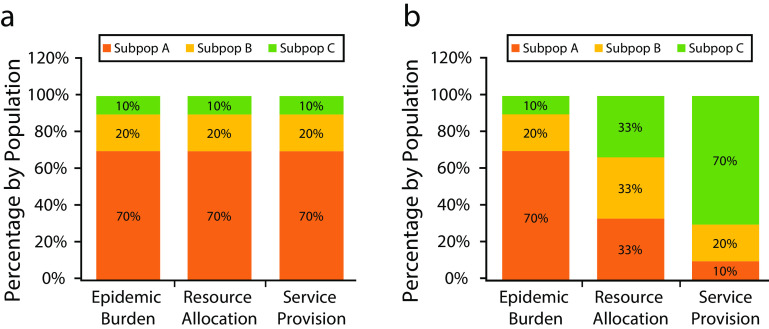
We advocate the development, refinement, and adoption of a new framework for combating infectious diseases: an Equity in Epidemic Allocations (EqEA) prototype. The EqEA prototype framework acknowledges that infectious disease epidemics (1) become rapidly concentrated in the most oppressed places and populations; (2) require allocations from private and public sources to places and populations proportional to their epidemic burden; (3) necessitate additional infrastructural development and capacity building so that service provision is aligned with both epidemic burden and allocations; and (4) compel continuous surveillance along epidemiological, allocation, service provision, and cost domains.
EqEA (Figure 1) is an allocations-level corollary to Meaningful Involvement of People Living With HIV/AIDS principles. EqEA acknowledges that infectious disease prevention must happen first, continually, and sustainably among populations experiencing the highest disease burden, especially when such populations are historically oppressed and underserved. Manifesting an EqEA response impels such supportive actions as recognizing, using, and respecting existing community-based wisdom by ensuring that indigenous experts are meaningfully included in allocation-prioritization bodies and epidemic-response planning and staffing; investing in the infrastructure of organizations with established ties to most-at-risk populations but potentially lacking fiscal stability and scientific expertise because of structural inequality; and designing larger structural innovations built to remediate underlying causes of disproportionate disease burden.
FIGURE 1—
Percentage of Hypothetical Subpopulations by (a) The Equity in Epidemic Allocations (EqEA) Framework and (b) an Example of Allocative Misalignment
Note. The figure shows proportions of hypothetical subpopulations A, B, and C across infectious disease epidemic burden, resource allocation, and service provision domains.
Relying solely on cost-effectiveness metrics in allocation modeling leads to overreliance on interventions that are the most efficiently deployed, thereby ignoring underserved populations who may require greater cost-per-person investments; in such cases, researchers have argued for a balance between efficiency and equity.6 Although Sansom et al. are unable to differentiate within-group cost-per-person metrics, it is likely that effectively reaching racial/ethnic minorities requires higher upfront costs. We communicate four suggestions for inclusion into the optimal allocations models promoted: (1) nesting analyses so that race/ethnicity, age, gender, and region are used to make allocation decisions; (2) analyzing risk group intersections (e.g., bisexually behaving men, MSM who inject drugs); (3) accounting for the effects of injectable preexposure prophylaxis on HIV-prevention success; and (4) design, refinement, and adoption of an EqEA framework.
The field of HIV prevention and care has never been more advanced or poised for success, yet we cannot succeed if we are myopic to viable, multilevel solutions. Resource allocation models must account for the historic, intersectional mechanisms that maintain HIV inequities among racial/ethnic and sexual and gender minorities. The proposed EqEA framework may help achieve Ending the HIV Epidemic endpoints and offers insights for other infectious diseases, such as directing COVID-19 prevention resources to minority communities wherein SARS-CoV-2 is exacting a disproportionately lethal toll and federal aid formulas for hospitals have large-scale racial biases.7 Adopting equitable allocation strategies will ensure that resources do not remain woefully misaligned and our systems do not exacerbate the well-defined shortcomings of decades of efforts.
ACKNOWLEDGMENTS
C. J. Chandler was supported by the National Institutes of Health (grant NIH 5T32MH094174).
We acknowledge Anthony J. Silvestre, PhD, for his support, guidance, and groundbreaking work in pursuing health equity over his distinguished career. We are thankful to the Pennsylvania HIV Planning Group and the Pennsylvania Department of Health, Division of HIV Disease for their structural commitment to parity, inclusion, representation, and health equity in HIV prevention and care.
CONFLICT OF INTERESTS
The authors have no potential conflicts of interest to disclose.
Footnotes
See also Sansom et al., p. 150.
REFERENCES
- 1.Centers for Disease Control and Prevention. HIV surveillance report. 2018;Vol. 31:2020. Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed October 31, 2020. [Google Scholar]
- 2.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 3.Adams B, Krier S, Netto J, Feliz N, Friedman MR. “All we had were the streets”: lessons learned from a recreation-based community health space for young Black MSM and trans women across the HIV prevention and care continuum. AIDS Educ Prev. 2018;30(4):309–321. doi: 10.1521/aeap.2018.30.4.309. [DOI] [PubMed] [Google Scholar]
- 4.Hawk M, Coulter RWS, Egan JE et al. Harm reduction principles for healthcare settings. Harm Reduct J. 2017;14(1):70. doi: 10.1186/s12954-017-0196-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauermeister JA, Muessig KE, LeGrand S et al. HIV and sexuality stigma reduction through engagement in online forums: results from the HealthMPowerment intervention. AIDS Behav. 2019;23(3):742–752. doi: 10.1007/s10461-018-2256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaplan EH, Merson MH. Allocating HIV-prevention resources: balancing efficiency and equity. Am J Public Health. 2002;92(12):1905–1907. doi: 10.2105/AJPH.92.12.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kakani P, Chandra A, Mullainathan S, Obermeyer Z. Allocation of COVID-19 relief funding to disproportionately Black counties. JAMA. 2020;324(10):1000–1003. doi: 10.1001/jama.2020.14978. [DOI] [PMC free article] [PubMed] [Google Scholar]