Abstract
The anonymized data of an epidemiology study on incidence of toluene diisocyanate (TDI)-related occupational asthma in three US-based TDI production facilities have been reanalyzed to identify where to best focus exposure reduction efforts in industrial practice to reduce the risk of sensitization to TDI. Since the induction of sensitization has sometimes been attributed to cumulative exposure, this relationship was examined first. Gross cumulative exposure values (i.e. not taking into account whether respiratory protection was used or not) and net cumulative exposure values (i.e. accounting for the use of respiratory protection) per participant were calculated based on the duration of their study participation and the average time-weighted average value of the exposure group to which they belonged. These two sets of cumulative exposure data were compared with asthma incidence using logistic regression. Incidence was zero among workers who rarely come into contact with open plant systems (e.g. during maintenance or spills). Notwithstanding, no statistically significant relationship between asthma incidence and either gross or net cumulative exposure could be determined. This is shown to be consistent with the results of several other epidemiology studies on TDI-related occupational asthma. In conclusion, cumulative exposure values are not a good indicator of the risk of developing TDI-related occupational asthma.
Keywords: Toluene diisocyanate (TDI), occupational asthma, cumulative exposure, risk indicator, respiratory protection
Introduction
Toluene diisocyanate (TDI) is an important industrial commodity chemical used to make polyurethane products such as foams, coatings, and adhesives. It is typically produced as an 80:20 mixture of the 2,4- and 2,6-isomers. Studies have been conducted to evaluate respiratory health effects of TDI exposure in the workplace: early studies reported irritation in the eyes and throat (Fuchs and Valade, 1951), accelerated lung function decline (Adams, 1975; Peters et al., 1968; Wegman et al., 1974), and TDI induced asthma (Bruckner et al., 1968; Franzinelli et al., 1978). In the meantime, significant improvements have been implemented in ventilation, use of respiratory protective equipment, medical surveillance and worker training.
Several further epidemiology studies have been conducted since (Supplemental Information-1), with those of Bodner et al. (2001), Bugler et al. (1991), Clark et al. (1998), Collins et al. (2017), Diem et al. (1982), Jones et al. (1992), Ott et al. (2000), and Weill et al. (1981) being the most relevant ones to the topic at hand. Yet, it is difficult to derive from these studies targeted exposure reduction measures aimed at minimizing the risk of acquiring occupational asthma. The joint study investigating health effects of exposure to TDI in three US-based TDI production facilities conducted between 2007 and 2012 by the American Chemistry Council (ACC) and the US National Institute for Occupational Safety and Health (NIOSH) offers an opportunity to investigate this in more detail. The study followed 197 workers over a 5-year period. The results were published in a series of four articles. Medical surveillance (Cassidy et al., 2017) was based on self-reported symptoms from questionnaires and interviews, as well as longitudinal spirometry (Wang et al., 2017). Seven cases “consistent with TDI-induced asthma” were identified by a pulmonologist reviewing the exposure and medical information of 31 participants that met certain criteria. Middendorf et al. (2017) characterized workplace exposure by full-shift time-weighted average (TWA) personal samples and calculated cumulative exposures. They concluded that sufficient samples were available to adequately characterize TWA values, but high-potential-exposure task-related measurements were judged to be too “limited and sporadic” to be included in their analysis. As a unique feature, exposure data included information about the use of respiratory protection during sampling, but this was not fully explored by Middendorf et al. (2017). The results of Middendorf et al. (2017) served as input for Collins et al. (2017) who examined asthma risk and incidence in the cohort of TDI production plant workers and derived an average incidence of asthma of 0.9 per hundred person-years. Logistic regression models suggested that both peak and cumulative exposure were associated with TDI-induced asthma.
The potential role of cumulative exposure in the development of TDI-induced asthma was an unexpected finding with little supporting evidence from other published worker epidemiology evaluations on TDI, as is illustrated by the overview of relevant literature in Table 1.
Table 1.
Overview of relevant studies and observed trends of incidence as a function of cumulative exposure.a
|
Diem et al.
(1982) Weill et al. (1981) Study information 1 US TDI production N = 277 Avg. TDI 3.5 ppb Incidence 1.0 |
Range of cumulative exposures
Cumulative exposure was used as a dichotomous parameter, “low” and “high” groups were split at 68.2 ppb-months (5.7 ppb-years). Range of cumulative exposure was not reported by the authors but can be estimated based on the reported maximum exposure (4.5 ppb for the high exposure group) and study duration (5 years) as 0–22 ppb-years. Relationship between incidence and cumulative exposure Diem et al. (1982) only investigated decline in FEV1 as a surrogate indicator for asthma and found that the decline was correlated with cumulative exposure. Weill et al. (1981: table 25, page 125) reported 12 cases of asthma. All cases that were observed within the first 68.2 (ppb-months)/4.5 (max. exposure) = 15 months of study participation belong with certainty to the “low” exposure group. At least nine of the cases fall into that category (from less than 1 week to 7 months of exposure). Yearly incidence was higher in the low exposure group: 9 cases for 149 participants (=1.2), compared to 3 cases for 74 participants (=0.8) in the high exposure group. Trend Incidence slightly decreasing with increasing cumulative exposure. |
|
Ott et al.
(2000) Study information 1 US TDI production N = 297 Avg. TDI 4.2 ppb Incidence 1.1 |
Range of cumulative exposures
Reported by the authors: average 234 ppb-months (19.5 ppb-years), range 0–983 ppb-months (0–82 ppb-years). Relationship between incidence and cumulative exposure No link with cumulative exposure reported. Risk of developing asthma was reported to be increased by prior incident exposure to TDI or phosgene, and to be reduced by increasing duration of exposure. Trend Tendentially incidence slightly decreasing with increasing cumulative exposure. |
|
Bodner et al.
(2001) Study information 1 US TDI production N = 305 Avg. TDI 2.3 ppb Incidence 0.5 |
Range of cumulative exposures
Reported by the authors: average 96.9 ppb-months (8 ppb-years), range 0–639 ppb-months (0–53 ppb-years); quartiles 0–2.5–6–11 ppb-years. Relationship between incidence and cumulative exposure No difference observed in incidence of asthma symptoms between the exposure quartiles. Trend “Flat line,” that is, no trend observed as a function of increasing cumulative exposure. |
|
Bugler et al.
(1991) Clark et al. (1998) Study information 12 UK TDI foaming N = 1462 Avg. TDI 2.1 ppb Incidence 0.8 |
Range of cumulative exposure
Three exposure groups were defined: “low,” “handling,” and “exposed”. Range of cumulative exposure was not reported by the authors but can be estimated based on reported daily cumulative exposure and the study duration (5 years): “exposed” 0–80 ppb-hours/day or 0–50 ppb-years, “handling” 0–20 ppb-years, and “low” less than 6 ppb-years. Relationship between incidence and cumulative exposure A statistically significant difference was observed in development of asthma symptoms between the “handling” and “exposed” groups and the “low” exposure group. Development of symptoms was however “not greatly different” between the “handling” and “exposed” groups. Trend “Stepwise response”, that is, symptoms seem to be related to there being exposure but show little evolution with increasing cumulative exposure. |
|
Collins et
al. (2017) Middendorf et al. (2017) Study information 3 US TDI production N = 197 Avg. TDI 0.7 ppb Incidence 0.9 |
Range of cumulative exposure
Reported by Middendorf et al. (2017): 0–22 ppb-years. Relationship between incidence and cumulative exposure Slope parameter in a logistic model expressing odds of developing asthma as a function of the natural logarithm of cumulative exposure was reported to be 0.73. Since probability is low, this means that probability of developing asthma can be approximated by a power function of cumulative exposure with an exponent of approximately 0.7. This is confirmed by the risks for TDI-induced asthma reported by Collins et al. (2017: table 3): 5.3% at 5 ppb-years, 8.5% at 10 ppb-years, 11.1% at 15 ppb-years, and 13.4% at 20 ppb-years. Regression by a power curve shows an exponent of 0.67. Trend Incidence strongly increasing with increasing cumulative exposure. |
|
Jones et al.
(1992) Study information 2 US TDI foaming N = 386 Avg. TDI 2.0 ppb Incidence 0.7 |
Relationship between incidence and cumulative
exposure
Could not be investigated by the authors because of lack of sufficient follow-up data. |
FEV1: forced expiratory volume in one second; TDI: toluene diisocyanate.
a Incidence per hundred person-years.
In order to best focus practical industrial hygiene and product stewardship measures aimed at reducing the incidence of TDI-related occupational asthma, it is necessary to understand what aspects of exposure are most important. The reexamination of the data from the ACC-NIOSH study reported in the current work was initiated with the dual purpose of investigating why conclusions linking cumulative exposure with asthma incidence as reported by Collins et al. (2017) differ from results of other published epidemiology studies on the same subject of TDI-induced asthma (this paper—Part I), and whether the data permit establishing a link between asthma incidence and indicators of peak exposure (accompanying paper—Part II). Specifically, in Part II (Plehiers et al., 2020), it was investigated whether 8-h TWA values could serve as an alternative way of characterizing peak exposure.
Access to the anonymized study records was granted by the ACC, one of the data owners. A data use agreement with ACC is in effect. The protocol for and the report of the current study were reviewed and approved by the Human Studies Review Board of The Dow Chemical Company (Ref. 2019-HSRB-207).
The reader of this article is referred to Middendorf et al. (2017) and Collins et al. (2017) for a thorough description of the data grouping used in those papers and in this reanalysis. The Similar Exposure Groups based upon plant and job function (Plant/SEGs) as defined by Middendorf et al. (2017) were used unaltered in the present work. For quick reference, a concise summary of essential information about the ACC-NIOSH study is given in Supplemental Information-2.
Methods
The overall approach was to first verify that the information and the exposure measurements in the anonymized study data set were consistent with the published information, then to recalculate cumulative exposures and to put these into relation with asthma incidence. Details on data verification methods can be found in Supplemental Information-3.
TWA and TWA-8 values
In this work, TWA values were calculated from the raw workplace analysis data as the sum of 2,4- and 2,6-TDI, as documented, that is, not converted to an 8-h value. To maintain comparability with Middendorf et al. (2017), only samples marked as “Routine” were considered, regardless of the use of respiratory protection, and half the detection limit was used for “non-detects” in calculating cumulative exposure values.
TWA-8 (8-h adjusted) values were calculated by adjusting for shift duration in accordance with equation (1):
| 1 |
For this reevaluation, TWA-8 values take into account all samples. This includes samples taken under non-routine conditions (“Start-up”, “Upset”, and “Turnaround”), since these are the circumstances that would typically contribute to peak or unexpected exposures. The adjustment to TWA-8 values provides a better basis for comparison of exposure per workday across Plant/SEGs (8 to 12 h work regimens).
Calculation of gross cumulative exposure
Gross cumulative exposure (meaning cumulative exposure without taking into account whether respiratory protection was used or not) was calculated for each participant as described below:
The exposure period for gross cumulative exposure and asthma incidence calculations was considered to start with either the beginning date of the study or the hiring date of the participant, whichever was later.
The exposure period was the lesser of the duration of the study (5 years) or of individual participation in the study.
The average TWA value, μ A, of the Plant/SEG to which the employee belonged was used for the calculation. It was not adjusted for shift duration: the same yearly number of hours worked was assumed for all participants.
This method to calculate gross cumulative exposure deviates from the one used by Middendorf et al. (2017) and incorporated in Collins et al. (2017) in two aspects. First, pre-study exposure, which could be estimated for part of the study population only, is not included in this method. Second, the average (μ A—column (6) in Table S3-1—Supplemental Information-3) of the untransformed TWA values was used in lieu of the geometric mean (GM—column (1) in Table S3-1). For the given distributions of TWA values, the latter is a poor representation of cumulative exposure, since it tends to overrepresent the many “non-detects” (see Figure S3-1).
Calculation of net cumulative exposure
Net cumulative exposure (meaning cumulative exposure taking into account the reduction in exposure afforded by using respiratory protection) was calculated in a similar fashion based on the average TWA values of the Plant/SEG the individual employee belonged to, taking into account only those samples during which no respiratory protection was documented (samples marked as “None” or “Blank”). Since self-contained breathing apparatus was the type of respiratory protection used in all cases, the error induced by assuming full protection was estimated to be less than 0.01 ppb-years (max. 20 ppb-years/2000 (assigned protection factor used by Middendorf et al., 2017)).
Data processing
In general, calculations and data analysis were conducted using Excel (Microsoft Corp., Redmond, WA, USA). The regressions and parameter evaluations reported in Supplemental Information-4 and Supplemental Information-6 were performed using Maple (R.2019; MapleSoft Inc., Waterloo, ON, Canada). The t-test within Maple was used to check whether the determined regression parameters were significantly different from zero at the 95% confidence level.
The hypothesis that TDI-induced asthma is related to cumulative exposure was tested against the individual exposure data points and their respective binary “asthma outcome” by means of logistic regression. The JMP statistics software package (v13.2.1; SAS Institute Inc., Cary, NC, USA) was used to perform the logistic regression and sensitivity analyses reported in the main text and in Supplemental Information-5.
The resulting prediction models were evaluated based on the standard criteria included in the JMP output:
A Wald-χ 2-test is used to evaluate whether either intercept or slope parameters were zero (null hypotheses). A model was determined to be significant only if the probability values associated with both intercept and slope parameters were below 5% (p < 0.05).
The whole model evaluation is based on a χ 2-test for the difference of the full (including both intercept and slope parameters) and reduced (excluding the slope parameter) models. A model was concluded to provide a significant prediction of the outcome variable only if the probability of achieving a higher χ 2-value with the reduced model compared to the full model was less than 5% (p < 0.05).
Results
Data verification
Consistency of the exposure data with those in the original publications was confirmed (Supplemental Information-3). Relevant other findings are summarized hereunder.
Participants and potential data limitations
Collins et al. (2017) reported that 197 employees participated through the entire study. The anonymized study records allowed to assign only 178 entries with certainty to a Plant/SEG (Similar Exposure Group as defined by Middendorf et al., 2017). This review has been performed on the basis of the 178 entries that could be allocated unequivocally. It is assumed that the loss of records is random and not concentrated in one particular SEG, and that any impact thereof on trends and conclusions is limited.
Identified cases “consistent with TDI-induced asthma”
Collins et al. (2017) reported seven cases that were described as “consistent with TDI-induced asthma.” These were identified by a consulting pulmonologist reviewing exposure and medical information of 31 participants who met certain criteria. Two additional cases were identified as “indeterminate regarding work-relatedness.” None of the asthma cases were clinically confirmed (Cassidy et al., 2017). For this reevaluation, the judgment of the pulmonologist involved in the original study was considered final.
In the anonymized data, seven cases were reported as consistent with asthma, only two of which were unequivocally marked as “work-related.” These seven cases could be allocated to a specific Plant/SEG so that the corresponding cumulative exposures could be calculated.
Workplace atmosphere measurements
It was noted from the recorded sampling durations that the three TDI plants used different work regimes. Workday or shift exposure durations therefore varied: “daytime” work either in a traditional 8-h system or in a system with mostly 9-h days in a 2-week cycle (“nine-eighties”), “maintenance” work regularly extending to 10 h per day (“eight-tens”), and both 8-h and 12-h shift systems. There was no indication of overtime or extended shifts, which are regular occurrences in shift work to cover for vacation or sick time. Although some shift rosters may inherently include overtime, it is unclear whether this was accounted for. For this evaluation, it was assumed that every participant worked a similar number of hours per year. By lack of more detailed information in the publications and in the data, it would be expected that the same assumption was made by Middendorf et al. (2017). This assumption may not necessarily be correct, and in particular may underestimate exposure for shift workers. A sensitivity analysis was performed to assess the potential impact thereof.
Additional background on job functions and how these affect exposure metrics that is based on the authors’ experience in chemical plants is given in Supplemental Information-4. This includes considerations about the potential contribution of dermal exposure. Middendorf et al. (2017) considered dermal contact to be only “sporadic,” and Supplemental Information-4 supports the view that—in the given chemical production environment—exposure by the dermal route is a minor contributor. It is worth repeating here that participants in support roles (bundled as Support-SEG) spend a larger portion of their time indoors (e.g. in control rooms, offices, or shops) and a smaller part in the plant near the TDI-containing processing equipment. They are usually not involved in direct line-breaking activities. Consequently, their risk of exposure is low since they rarely come into contact with “open” plant systems and are less likely to be near any incident or other event, should these occur in the facility.
The overall study rate of incidence of asthma “consistent with being TDI-induced” based upon actual person-years determined in this review was 0.89 per hundred person-years (= 7/785 × 100), which is in agreement with the value of 0.9 per hundred person-years determined by Collins et al. (2017). This is expected since the calculated numbers of person-years closely match and the number of cases is the same.
Data analysis
Gross cumulative exposure and relationship with incidence of cases consistent with TDI-induced asthma
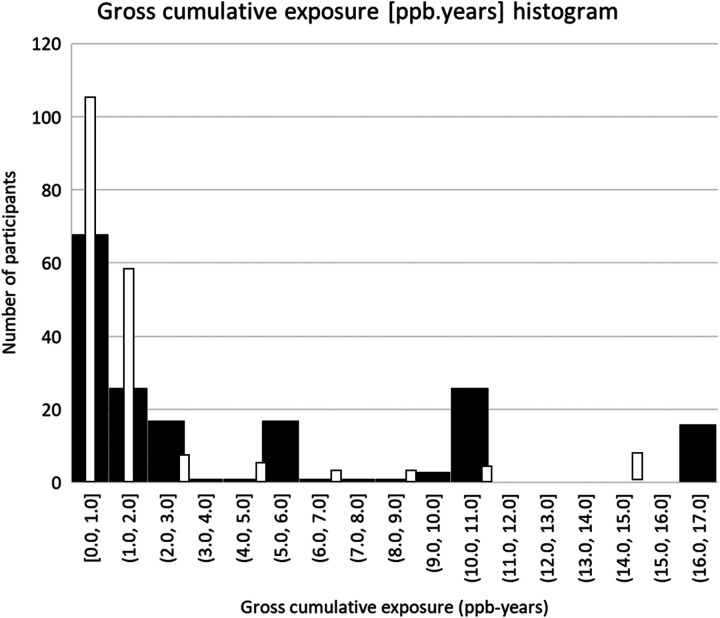
The histogram of number of participants in certain groups of gross cumulative exposure values is shown in Figure 1.
Figure 1.
Histogram of calculated gross cumulative exposure values. x-axis: intervals of gross cumulative exposure values (ppb-years); y-axis: number of participants. The open bars are a rendering of the histogram of cumulative exposure values of Middendorf et al. (2017). The full bars represent the histogram of cumulative exposure values obtained from this reanalysis.
The full bars in Figure 1 represent the histogram of cumulative exposure values obtained from this reanalysis. For 68 (38%) of the participants, gross cumulative exposure was less than 1 ppb-year. Large clusters occur between 5–7, 9–11, and 16–17 ppb-years. These correspond to the Plant/SEGs with higher average TWA values. The open bars in Figure 1 are a rendering of the histogram of cumulative exposure values as published by Middendorf et al. (2017). Compared to the results of Middendorf et al. (2017), the count in the lower cumulative exposure categories is markedly lower in the present analysis and there is evidently a higher number of participants associated with the higher cumulative exposure categories. Even when considering that exposure duration was limited to the duration of study participation, this result follows from the fact that the average TWA values were used in the present reanalysis instead of the geometric means.
Table 2 provides an overview of incidence of asthma “consistent with being induced by TDI” as a function of gross cumulative exposure categories derived from Figure 1.
Table 2.
Incidence of TDI-related asthma as a function of gross cumulative exposure categories derived from Figure 1.a
| Gross cumulative exposure (ppb-years) | <2 | 2–4 | 4–8 | 8–12 | >12 | |
|---|---|---|---|---|---|---|
| SEG | Support | Others | ||||
| Range of average TWA values (ppb) | 0.1 | 0.1–3.4 | 0.5–1.2 | 1.2–3.4 | 2.0–3.4 | 3.4 |
| Number of participants | 46 | 48 | 18 | 20 | 30 | 16 |
| Number of asthma cases | 0 | 2 | 1 | 1 | 2 | 1 |
| Participant-years | 190 | 201 | 86 | 84 | 144 | 80 |
| Incidence per hundred person-years | 0 | 1.00 | 1.17 | 1.20 | 1.39 | 1.25 |
SEG: Similar Exposure Group; TWA: time-weighted average; TDI: toluene diisocyanate.
a Incidence per hundred person-years of study participation. The overall incidence based on actual person-years is 0.9 per hundred person-years.
Incidence is much more evenly distributed over the range of gross cumulative exposures in the current analysis compared to what is implied by the model predictions of Collins et al. (2017), which show a steady increase of asthma risk with increasing cumulative exposure (see Table 1 for comparison). There is a lower incidence only among the participants in the category below 2 ppb-years of gross cumulative exposure (aggregate incidence in that category: 0.51). If Support-SEG data are broken out from the <2 ppb-years category, as it is presented in Table 2, an incidence rate of 1.00 per hundred person-years was obtained for the remainder of that category.
The 178 individual cumulative exposure data points together with their respective binary “asthma outcome” (0/1) were analyzed by logistic regression. The slope parameter was not significant (p = 0.37 for a linear model and p = 0.20 for a logarithmic model); neither was the goodness-of-fit (p = 0.40 and p = 0.19, respectively).
Sensitivities
Sensitivity analyses were made to investigate the effects of:
An assumed 30% overtime rate for shift workers (equivalent to multiplying study participation time by a factor of 1.3).
Replacing the average TWA values (μ A) with the values back-calculated from the log-transformed TWA distributions (μ T), which assumes the TWA values would be log-normally distributed (see Middendorf et al., 2017).
The results are reported in Supplemental Information-5. Neither alternative showed a significant relationship between asthma incidence and gross cumulative exposure.
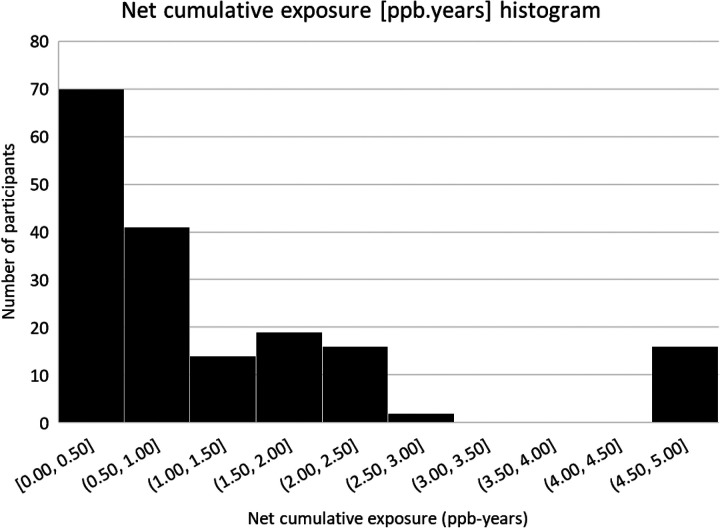
Net (respirator-adjusted) cumulative exposure and relationship with incidence of cases consistent with TDI-induced asthma
The histogram of number of participants in certain groups of net cumulative exposure values is shown in Figure 2.
Figure 2.
Histogram of calculated net (adjusted for the type of respiratory protective equipment used) cumulative exposure values. x-axis: intervals of net cumulative exposure values (ppb-years); y-axis: number of participants.
Table 3 provides an overview of incidence of asthma “consistent with being induced by TDI” as a function of net cumulative exposure categories derived from Figure 2.
Table 3.
Incidence of TDI-related asthma as a function of net (adjusted for the type of respiratory protective equipment used) cumulative exposure categories derived from Figure 2.a
| Net cumulative exposure (ppb-years) | <1 | 1–2 | 2–3 | >3 | |
|---|---|---|---|---|---|
| SEG | Support | Others | |||
| Number of participants | 46 | 65 | 33 | 18 | 16 |
| Number of asthma cases | 0 | 3 | 2 | 1 | 1 |
| Participant-years | 190 | 285 | 147 | 83 | 80 |
| Incidence per hundred person-years | 0 | 1.05 | 1.36 | 1.21 | 1.25 |
TDI: toluene diisocyanate; SEG: Similar Exposure Group.
a Incidence per hundred person-years of study participation. The overall incidence is 0.9 per hundred person-years.
Here too, incidence is evenly distributed over the range of net cumulative exposures. There is a lower incidence only among the participants in the category below 1 ppb-years of net cumulative exposure (aggregate incidence in that category: 0.63). The 178 data points were analyzed by logistic regression. The slope parameter was not significant (p = 0.36 for the linear model); neither was the goodness-of-fit (p = 0.39).
Discussion
The distributions of TWA values for the Plant/SEGs match well with the work of Middendorf et al. (2017) as is apparent from Table S3-1 (Supplemental Information-3). The anonymized workplace atmosphere data set used in the present reanalysis seems to be a reliable representation of the original data. The average (μ A) of these distributions was used to calculate cumulative exposure values for each participant.1 “Gross” cumulative exposure reflects the concentrations as measured by workplace atmosphere sampling; “net” cumulative exposure accounts for the reduction of actual exposure by the use of respiratory protection. The length of time a worker participated in the study was taken as a measure of exposure duration. The slope parameter of a logistic regression linking the rate of incidence of asthma “consistent with being induced by TDI” was found to be not statistically significant, indicating no significant relationship between exposure and asthma incidence. There appears to be almost a dichotomous response instead. No cases of asthma consistent with being induced by TDI were reported among participants in support roles (Support-SEG), who are only rarely exposed to plant systems that are intentionally (e.g. maintenance) or incidentally (e.g. releases) opened. For participants in other roles, asthma incidence was practically independent of gross cumulative exposure (Table 2). Sensitivity analyses confirmed that this observation also holds when another way of calculating average TWA-values is used or when potential overtime in shift work is considered. Similarly, the use of net (adjusted for the type of respiratory protection used) cumulative exposure as a basis did not affect the outcome.
Based upon the above considerations, there seems to be good agreement between the reanalyzed results of the ACC-NIOSH study with results from other cohorts, as presented in Table 1. The absence of a significant dose-response, as measured by asthma incidence, is also consistent with the results of Ott et al. (2000). Cumulative exposure values reported by Ott et al. (2000) ranged from 0 to 82 ppb-years with an average of approximately 20 ppb-years; asthma incidence was reported to be 1.06 per hundred person-years. The maximum cumulative exposure reported by Middendorf et al. (2017) was approximately 20 ppb-years; the corresponding asthma incidence reported by Collins et al. (2017) was 0.9 per hundred person-years. The results of Ott et al. (2000) do not compare favorably against the model of Collins et al. (2017) that predicts a steep increase in asthma incidence with cumulative exposure.
Review of other studies that met specific criteria (Supplemental Information-1) showed similar results. A more detailed scrutiny of the results reported by Weill et al. (1981) revealed that asthma incidence was actually higher in the “low cumulative exposure” group than in the “high cumulative exposure” group (see Table 1). Bodner et al. (2001) observed no difference in asthma risk as a function of cumulative exposure quartiles. Daftarian et al. (2000) determined that prevalence of work-related asthma symptoms was similar for the second, third and fourth exposure quartiles in their study. Prevalence was higher than in the first exposure quartile, however, the difference did not reach statistical significance. This picture is very similar to the results shown in Tables 2 and 3. Overall, and from a practical perspective, it can be concluded that cumulative exposure (whether gross or net) is not a good indicator of the risk of induction of TDI-related occupational asthma.
Average exposure values have decreased significantly between the 1970s and 1980s and the period of the ACC-NIOSH study, but asthma incidence rates from studies conducted in the two time periods are essentially the same. Diem et al. (1982) reported average TWA values of 1.6–6.8 ppb for their study population, and an overall asthma incidence rate of 1.0 per hundred person-years. Collins et al. (2017) reported an average asthma incidence rate of 0.9 per hundred person-years against average TWA values between 0.1 and 3.4 ppb. Daniels (2018) provides an extensive overview but did not include the results of Collins et al. (2017) (Supplemental Information-6). None of the exposure-response models evaluated by Daniels (2018) exhibited a significant slope parameter. This again is indicative that neither gross cumulative exposure nor the average study exposure (which usually are strongly correlated) are the main risk factors for the development of asthma consistent with being induced by TDI.
The present reanalysis of anonymized data of the joint ACC-NIOSH study of health effects associated with occupational exposure to TDI cannot overcome shortcomings that were already reported by the respective authors. With only seven cases identified as “consistent with TDI-induced asthma,” conclusions could be very dependent on their diagnosis. The workplace atmosphere data were shown to be a reliable representation of the data used in the original study. However, the anonymized records did not allow to allocate all 197 participants to the corresponding Plant/SEGs, which may have introduced an additional source of uncertainty in this reevaluation. To affect the trends and conclusions of this reevaluation, however, most of the 19 participants (among whom there were no asthma cases) for which it was not possible to allocate the corresponding exposure data would have to be associated with low gross cumulative exposure values. Looking at the data and Figure 1, however, even that would not compensate the large difference between geometric mean and average TWA-values. Hence, it appears far more likely that the way of calculating cumulative exposures had a more decisive influence on the results.
With this reanalysis of the ACC-NIOSH study, the weight-of-evidence from studies performed over three decades supports the conclusion that cumulative exposure is not a good indicator of the risk of developing asthma as a result of TDI exposure.
Supplemental material
Supplemental Material, Part_I-Supplemental_Information_1 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_2 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_3 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_4 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_5 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_6 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Acknowledgment
The authors acknowledge the support of the American Chemistry Council, acting on behalf of its Diisocyanates Panel, which granted access to the anonymized study data. The authors recognize Mr Robert J West of the International Isocyanate Institute, Inc. for support with the statistical analyses.
Note
Middendorf et al. (2017: S4) indicated the use of μ T but seem to have used the geometric mean instead (see Collins et al., 2017: S23). It was not possible to reconstruct figure 3 of Middendorf et al. (2017) based on μ T being used.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors are employed by the International Isocyanate Institute, Inc. The Institute is funded by producers of MDI and TDI.
Disclaimer: Any views expressed in this paper and any conclusions are those of the authors, not necessarily of the International Isocyanate Institute, Inc. or its member companies.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded with regular membership fees of the International Isocyanate Institute, Inc. There is no other funding to report.
ORCID iD: Patrick M Plehiers  https://orcid.org/0000-0002-4630-5016
https://orcid.org/0000-0002-4630-5016
Supplemental material: Supplemental material for this article is available online.
References
- Adams WGF. (1975) Long-term effects on the health of men engaged in the manufacture of toluene diisocyanate. British Journal of Industrial Medicine 32(1): 72–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner KM, Burns CJ, Randolph NM, et al. (2001) A longitudinal study of respiratory health of toluene diisocyanate production workers. Journal of Occupational and Environmental Medicine 43(10): 890–897. [DOI] [PubMed] [Google Scholar]
- Bruckner HC, Avery SB, Stetson DM, et al. (1968) Clinical and immunological appraisal of workers exposed to diisocyanates. Archives of Environmental Health 16(5): 619–625. [DOI] [PubMed] [Google Scholar]
- Bugler J, Clark RL, Hill H, et al. (1991) The acute and long-term respiratory effects of aromatic diisocyanates. A five year longitudinal study of polyurethane foam workers. Report no. 10848, Manchester: International Isocyanate Institute. [Google Scholar]
- Cassidy L, Doney B, Wang ML, et al. (2017) Medical monitoring for occupational asthma among toluene diisocyanate production workers in the United States. Journal of Occupational and Environmental Medicine 59(Suppl.12): S13–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark RL, Bugler J, McDermott M, et al. (1998) An epidemiology study of lung function changes of toluene diisocyanate foam workers in the United Kingdom. International Archives of Occupational and Environmental Health 71: 169–179. [DOI] [PubMed] [Google Scholar]
- Collins JJ, Anteau S, Conner PR, et al. (2017) Incidence of occupational asthma and exposure to toluene diisocyanate in the United States toluene diisocyanate production industry. Journal of Occupational and Environmental Medicine 59(Suppl.12): S22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daftarian HS, Roegner KC, Reh CM. (2000) Hazard evaluation and technical assistance report: HETA-98-0011-2801. Cincinnati: National Institute for Occupational Safety and Health. [Google Scholar]
- Daniels RD. (2018) Occupational asthma risk from exposures to toluene diisocyanate: a review and risk assessment. American Journal of Industrial Medicine 61(4): 282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diem JE, Jones RN, Hendrick DJ, et al. (1982) Five-year longitudinal study of workers employed in a new TDI manufacturing plant. The American Review of Respiratory Disease 126(3): 420–428. [DOI] [PubMed] [Google Scholar]
- Franzinelli A, Mariotti F, Innocenti A. (1978) Patologia respiratoria da isocianati in un’industria di frigoriferi. La Medicina del Lavoro 69(2): 163–171. [PubMed] [Google Scholar]
- Fuchs S, Valade P. (1951) Étude clinique et expérimentale sur quelques cas d’intoxication par le Desmodur T (diisocyanate de toluylène 1-2-4 et 1-2-6). Archives des Maladies Professionnelles 12(2): 191–196. [PubMed] [Google Scholar]
- Jones RN, Rando RJ, Glindmeyer HW, et al. (1992) Abnormal lung function in polyurethane foam producers: weak relationship to measured TDI exposures. The American Review of Respiratory Disease 146(4): 871–877. [DOI] [PubMed] [Google Scholar]
- Middendorf PJ, Miller W, Feeley T, et al. (2017) Toluene diisocyanate exposure: exposure assessment and development of cross-facility similar exposure groups among toluene diisocyanate production plants. Journal of Occupational and Environmental Medicine 59(Suppl.12): S1–12. [DOI] [PubMed] [Google Scholar]
- Ott MG, Klees JE, Poche SL. (2000) Respiratory health surveillance in a toluene di-isocyanate production unit, 1967-97: clinical observations and lung function analyses. Occupational and Environmental Medicine 57(1): 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters JM, Murphy RLH, Pagnotto LD, et al. (1968) Acute respiratory effects in workers exposed to low levels of toluene diisocyanate (TDI). Archives of Environmental Health 16(5): 642–647. [DOI] [PubMed] [Google Scholar]
- Plehiers PM, Chappelle AH, Spence MW. (2020) Practical learnings from an epidemiology study on TDI-related occupational asthma: Part II—Exposure without respiratory protection to TWA-8 values indicative of peak events is a good indicator of risk. Toxicology and Industrial Health (Submitted 14 May 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang ML, Storey E, Cassidy LD, et al. (2017) Longitudinal and cross-sectional analyses of lung function in toluene diisocyanate production workers. Journal of Occupational and Environmental Medicine 59(Suppl.12): S28–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegman DH, Pagnotto LD, Fine LJ, et al. (1974) A dose-response relationship in TDI workers. Journal of Occupational Medicine 16(4): 258–260. [PubMed] [Google Scholar]
- Weill H, Butcher B, Dharmarajan V, et al. (1981) Respiratory and immunologic evaluation of isocyanate exposure in a new manufacturing plant. NIOSH Technical Report Publication No. 81-125 Morgantown: National Institute for Occupational Safety and Health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Part_I-Supplemental_Information_1 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_2 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_3 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_4 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_5 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_I-Supplemental_Information_6 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part I—Cumulative exposure is not a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health