Abstract
The anonymized data of an epidemiology study on the incidence of toluene diisocyanate (TDI)-related occupational asthma in three US-based TDI production facilities have been reanalyzed to identify where to best focus exposure reduction efforts in industrial practice in order to reduce the risk of sensitization to TDI. In Part I, it was demonstrated that cumulative exposure is not a good indicator of the risk of developing TDI-related occupational asthma. In this Part II, an alternative model was developed based on net exposure parameters (i.e. samples taken when no respiratory protection was used). A statistically significant relationship was determined between asthma incidence and the frequency of exposure to TDI levels indicative of peak events that are expressed as time-weighted average-8 (TWA-8) values greater than 3 ppb during which no respiratory protection was used. This relationship suggests a threshold to induction of TDI-related asthma. The findings also highlight the importance of a comprehensive program for controlling workplace atmosphere in the plant by technical measures (e.g. selection of equipment, cleaning procedures) and controlling exposure by organizational measures and situational awareness (e.g. training, use of in-the-field direct reading indicators) during high potential exposure scenarios (e.g. line breaking, spills) to encourage or enforce the appropriate use of respiratory protection.
Keywords: Toluene diisocyanate (TDI), occupational asthma, peak exposure, threshold, respiratory protection, modeling, risk indicator
Introduction
Toluene diisocyanate (TDI) is a known respiratory sensitizer and has been studied in numerous epidemiological studies. However, it is difficult to derive from these studies targeted exposure reduction measures aimed at minimizing the risk of acquiring occupational asthma. The joint study investigating health effects of exposure to TDI in three US-based TDI production facilities conducted between 2007 and 2012 by the American Chemistry Council (ACC) and the US National Institute for Occupational Safety and Health (NIOSH) offers an opportunity to investigate this in more detail. Results were published in a series of four articles (Cassidy et al., 2017; Collins et al., 2017; Middendorf et al., 2017; Wang et al., 2017) and were summarized in Supplemental Information-2 of Part I (Plehiers et al., 2020).
Plehiers et al. (2020) recalculated cumulative exposures and demonstrated that neither gross nor net cumulative exposure are reliable indicators of the risk of acquiring asthma “consistent with being induced by TDI.” This was shown to be consistent with the results of several other epidemiology studies of TDI-related occupational asthma.
Part II explores other potential factors influencing the induction of TDI-related occupational asthma. For instance, behavioral aspects such as consistent use of respiratory protection may play a role, and others have suggested that peak exposure levels could be considered as a key factor for closer evaluation (Ott et al., 2000, 2003; Weill et al., 1981). However, peak, average, and cumulative exposure values are typically strongly correlated, as noted by Middendorf et al. (2017) and in a different context by Pronk et al. (2007). Differentiating between cumulative and peak exposure is very difficult on a purely statistical basis but can be done by combining the way time-weighted average (TWA) values are distributed with practical considerations from experience in plant operations. For instance, Cummings and Booth (2002) have shown that TWA values can be predictive for peak exposure if the actual operational time in the workday is considered.
Three important considerations allow for building an alternative model to link asthma incidence with exposure parameters. Firstly, while logistic regression models are powerful tools, they also have important limitations. At low probabilities (incidence less than 1 per hundred person-years in the case at hand), where the odds p/(1 − p) can be approximated by the probability p, the models reduce to either an exponential (linear model) or power (logarithmic model) probability function. Both are increasing monotonically but to a very different extent. Hence, it is worth validating such models against data that were not used to derive them. Secondly, it is important to note that in the ACC-NIOSH cohort, whenever respiratory protection was worn, it was of highest protective level (self-contained breathing apparatus, SCBA) (see Middendorf et al., 2017). This makes it plausible and likely that “net” (meaning taking into account the exposure reduction effect of respiratory protection used) rather than “gross” exposure parameters would need to be considered. In other words, “net exposure” rather than “workplace atmosphere” could be the determining factor driving TDI-related asthma incidence, because it is more representative of what workers have actually breathed. The third point relates to the fact that TDI production plants are large, continuously operating facilities that usually run without interruption for one to several years. Being a closed process, “background” work atmosphere concentrations in modern TDI production plants are normally a result of only the diffuse emissions from process equipment and piping flanges. Referring to the TWA distributions obtained by Middendorf et al. (2017), this is reflected by the very high number of measurements below the Limit of Detection and the narrow distribution of TWA values for support and maintenance roles. Hence, TWA values above background level mainly occur as a result of opening of the process system, whether planned (e.g. during plant “turnarounds”), intentional (e.g. maintenance, sampling) or incidental (e.g. leaks), or when making connections to other systems (e.g. truck loading). In many instances, engineering and administrative controls, such as closed sampling systems, system flushes, operating procedures, and so on are in place to mitigate exposure potential. Regardless of precautions, exposures from process stream and residual product leaks do occur as single events that are recorded as part of the TWA value. As an integral value over time, the TWA value does not provide direct information about the intensity (peak height) or the duration of events.
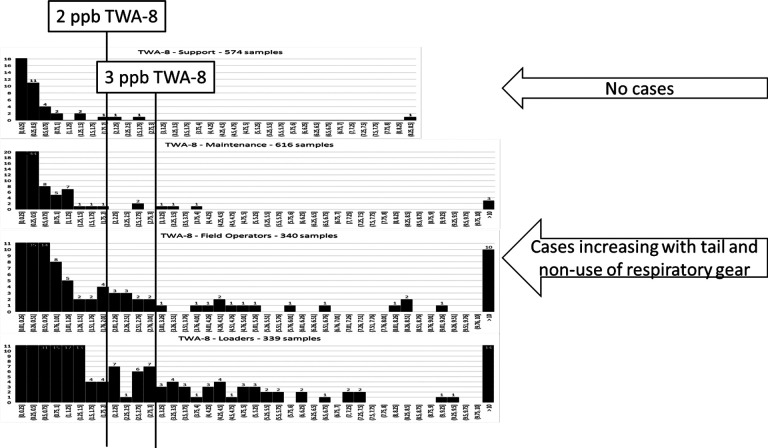
However, in a low-background environment like that of the ACC-NIOSH study, TWA-8 values of 2-3 ppb or higher are indicative of either conditions that approach the short-term exposure limit (STEL) allowances in force when the study was conducted (4 exposures at 20 ppb for 15 min averaged over an 8-h period correspond to a contribution of 2.5 ppb to the TWA-8) or the occurrence of large single events. A TWA-8 limit of 2–3 ppb also seems to represent a natural break between background and incident-related levels (see Figure 1).
Figure 1.
TWA-8 distributions, and indications of incidence of asthma cases “consistent with being induced by TDI” and non-use of respiratory protective equipment. The 2–3 ppb values were selected as potential breaks between “normal” background and task-related samples to the left and samples that are indicative of exceptional situations to the right. In a low-background environment, TWA-8 values of 2–3 ppb signal approaching STEL-allowances in force at the time of the study. TDI: toluene diisocyanate; STEL: short-term exposure limit; TWA: time-weighted average.
The measured TWA values from the ACC-NIOSH study show that, depending upon the job type, up to 7.1% of the TWA-8 samples represent conditions whereby the 8-h weighted value exceeded 3 ppb and no respiratory protection was worn (see “Results” section).
The considerations brought forward above are illustrated in Figure 1, which hints at a potential correlation between the occurrence of asthma cases and TWA-8 values above 2–3 ppb. This finding was taken as a lead to investigate potential correlations between asthma incidence and readily available TWA workplace atmosphere data that could reflect peak-type exposures.
Access to the anonymized study records was granted by the ACC, one of the data owners. A data use agreement with ACC is in effect. The protocol for and the report of the current study were reviewed and approved by the Human Studies Review Board of The Dow Chemical Company (Ref. 2019-HSRB-207).
It is recommended that the reader first read Part I (Plehiers et al., 2020) and its Supplemental Information for a complete understanding of the data grouping descriptions used in Middendorf et al. (2017) and this reanalysis (e.g. Plant/SEG, Support-SEG, etc.).
Methods
Workplace atmosphere measurements, TWA values, TWA-8 values and their averages were calculated as described in Plehiers et al. (2020).
The approach in this Part II was to correlate asthma incidence with a readily available indicator of peak exposures in the form of TWA-8 values above 3 ppb.
Frequency of TWA-8 values above 3 ppb without respiratory protection (“UnProtected (UP-3)-frequency”)
The Plant/SEG (Similar Exposure Groups as defined by Middendorf et al., 2017) TWA measurements were used to determine the frequency of occurrence of TWA-8 values above 3 ppb, whereby respiratory protection was either indicated as “None” or “Blank.”
All TWA-8 samples were taken into account. This includes samples taken under non-routine conditions (“Start-up,” “Upset,” and “Turnaround”), since these are the circumstances that would typically contribute to peak or unexpected exposures.
UP-3-frequencies for the Plant/SEGs were determined by fitting a Lomax-type distribution to the cumulative distribution of TWA-8 samples during which no respiratory protection was used. The percentage of samples above 3 ppb was then ratioed to the total number of TWA-8 samples for the Plant/SEG.
For Support-SEG (support groups), an UP-3-frequency of 0.15% was determined; for Maintenance-SEG (maintenance and laboratory functions), the UP-3-frequency was 0.8%. Wherever possible, separate values were determined for the other Plant/SEGs. In absence of a sufficient number of TWA-measurements, an UP-3-frequency of 0.8% was used as a conservative assumption.
Sensitivity analyses were performed to test different limit values (limits set at 1 ppb and 2 ppb instead of 3 ppb) and the potential impact of the abovementioned assumptions. Details are reported in Supplemental Information-1. For all sensitivity analyses, intercept and slope parameters as well as goodness-of-fit remained significant. Therefore, the UP-3 frequency as defined above was used for the further analyses in this review.
Data processing
In general, calculations and data analysis were performed using Excel (Microsoft Corp., Redmond, WA, USA). On the basis of this data analysis, the hypothesis for a potential alternative model was developed. This hypothesis was then tested against the individual exposure data points and their respective binary “asthma outcome” by means of logistic regression. The JMP statistics software package (v13.2.1; SAS Institute Inc., Cary, NC, USA) was used to perform the logistic regression and sensitivity analyses reported in the main text and in Supplemental Information-1.
The resulting prediction models were evaluated based on the standard criteria included in the JMP output:
A Wald-χ 2-test is used to evaluate whether either intercept or slope parameters were zero (null-hypotheses). A model was determined to be significant only if the probability values associated with both intercept and slope parameters were below 5% (p < 0.05).
The whole model evaluation is based on a χ 2-test for the difference of the full (including both intercept and slope parameters) and reduced (excluding the slope parameter) models. A model was concluded to provide a significant prediction of the outcome variable only if the probability of achieving a higher χ 2-value with the reduced model compared to the full model was less than 5% (p < 0.05).
Results
Potential alternative model
The potential alternative model makes use of the UP-3-frequency as a net exposure indicator. Table 1 shows that 46 of the 178 participants that could unequivocally be assigned to a Plant/SEG were in Support roles, which had an UP-3-frequency of 0.15%. The 132 others performed functions with higher risk of exposure, as is illustrated by UP-3-frequencies up to 7.1%.
Table 1.
Summary of incidence information using UP-3-frequency as a net exposure indicator.
| UP-3-frequencya (%) | 0.15 | 0.8 | 3.4 | 7.1 |
|---|---|---|---|---|
| SEG | Support | Others | ||
| Number of participants | 46 | 85 | 20 | 27 |
| Number of asthma cases | 0 | 3 | 1 | 3 |
| Participant-years | 190 | 405 | 85 | 105 |
| Incidence per hundred person-years | 0 | 0.8 | 1.2 | 2.8 |
a Percentage of all (routine and non-routine) samples, adjusted to 8-h values, that exceeded 3 ppb and for which no respiratory protection was used.
Table 1 also shows how the cases identified as “consistent with TDI-induced asthma” were distributed, together with the corresponding incidence rates. It indicates a clear relationship between UP-3-frequency and incidence of asthma consistent with being induced by TDI. No cases were observed when the UP-3-frequency was 0.15%. Incidence gradually increased up to 2.8 per hundred person-years with increasing UP-3-frequency.
The 178 individual data points together with their respective binary “asthma outcome” were analyzed by logistic regression models. Both a linear and a logarithmic model were evaluated. For both types of model, both the intercept and the slope parameters reached significance (p < 10−4 and p < 0.05 respectively). Both passed the goodness-of-fit test, with a slight advantage for the logarithmic model (p = 0.027 versus 0.047). For this data set, the ln(odds) of acquiring TDI-related asthma over the study duration could in principle be represented by either equation (1) (linear model) or equation (2) (logarithmic model):
| 1 |
| 2 |
Based solely upon the data of the study under consideration, a further discrimination between the two models would not be possible.
Discussion
The study by Bugler et al. (1991), published in part by Clark et al. (1998), is the only reference we could identify that has explicitly taken into account the use of respiratory protection to calculate (cumulative) exposure.1 However, air-purifying respirators were used and the exposure reduction was estimated to be no more than 50%. Compared to this and other studies conducted in the 1970s–1990s (Ott et al., 2000; Weill et al., 1981), the set of workplace atmosphere data evaluated here is unique in that it allows differentiation between TWA values that were measured while respiratory protection was used or not. This is a key strength that can be used beneficially to derive more meaningful correlations between the incidence of asthma “consistent with being induced by TDI” and net exposure rather than workplace atmosphere (gross exposure) characteristics.
A potential link between asthma incidence and high peak exposures (e.g. spills) was reported by Bugler et al. (1991), Ott et al. (2000), and Weill et al. (1981). Collins et al. (2017) too found a significant (p = 0.03) link between peak exposure, defined as the 95-percentile of the TWA values, and asthma incidence. In this reanalysis, a significant link was established between asthma incidence and the percentage of TWA-8 samples exceeding 3 ppb without respiratory protection being used (UP-3-frequency). This UP-3-frequency was selected as a better marker for net exposure than workplace atmosphere (gross exposure) measurements. It was also shown that, in this particular study, TWA-8 values above 3 ppb are more indicative of peak exposure events than of background levels. The established correlation between asthma incidence and UP-3-frequency makes clear that there is a significant link between asthma and (frequency of) “unprotected” peak exposure events.
Table 2 translates this observation into industrial practice by comparing four anonymized Plant/SEGs that cover a range of atmosphere and exposure control parameters. The +/− signs in Table 2 indicate situations that are better or worse than study average. “Control of atmosphere” is an indication of frequency of high TWA-8 values: “+” indicates less than 5% of all TWA-8 samples being above 3 ppb, and “−” indicates more than 10% of all TWA-8 samples being above 3 ppb. In practice, this parameter is an indication of the effectiveness of engineering controls. “Control of exposure” is a similar indication of UP-3-frequency: “+” indicates an UP-3-frequency below 1%, and “−” indicates an UP-3-frequency above 3%. In practice, this parameter is an indication of awareness regarding the need for respiratory protection in a given situation.2
Table 2.
Comparison of some relevant parameters for four anonymized Plant/SEGs that cover a range of atmosphere and exposure control parameters.
| Plant/SEG | A | B | C | D |
|---|---|---|---|---|
| Control of atmosphere | − | + | − | + |
| Control of exposure | − | − | + | + |
| Incidence rate compared to study average | −− | − | + | ++ |
+/−: performing better/ worse than study average; SEG: Similar Exposure Group.
Groups B and D both show a low frequency of elevated TWA-8 values (expressed by “+” for “Control of atmosphere”). They differ by their UP-3-frequencies (expressed by the “−” and “+” for “Control of exposure”). Whereas asthma incidence for D was far better (lower) than study average, incidence for B was worse (higher) than study average. Groups A and C both show a high frequency of elevated TWA-8 values (expressed by “−” for “Control of atmosphere”). They too differ by their UP-3-frequencies. By good “Control of exposure,” incidence remained better than study average for C, whereas A had an incidence rate far worse than study average. Table 2 suggests that relying solely on engineering measures to control the workplace atmosphere may not be sufficient to achieve low incidence rates. Should events occur that could result in brief TDI peak exposures, a program to quickly assess the need to don protective equipment seems to be equally important. Simple tools that can be used in-the-field (e.g. colorimetric indicator tape or badge, hand-held measurement device) are available to support such assessment.
It is reasonable to ask if the conclusions for TDI production plants could be applied to facilities consuming TDI. Whereas this may be the case for the general link with net exposure to high event concentrations, additional factors may have to be considered (Supplemental Information-2).
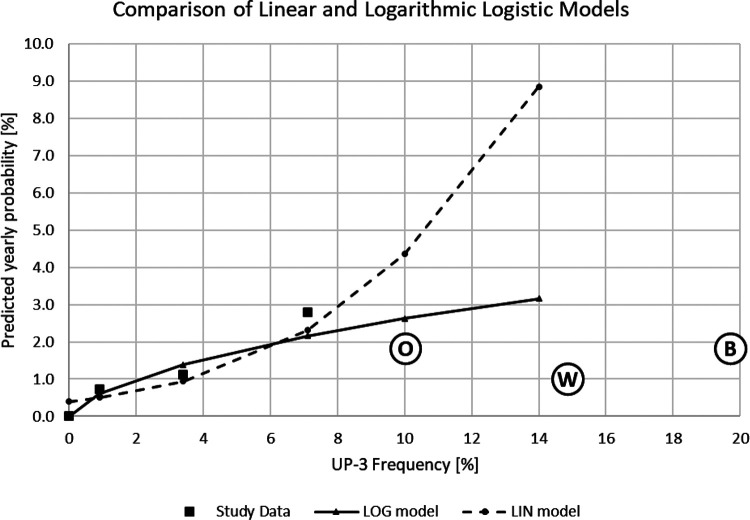
As mentioned under “Results” section, discrimination between the linear and logarithmic models (equations (1) and (2)) is not possible solely on the basis of the evaluated data set and statistical analysis. However, comparison of the extrapolated predictions of the linear and the logarithmic logistic regressions to data that were not used to develop the models does allow to do so, as is shown in Figure 2.
Figure 2.
Comparison between predicted probabilities of the linear (equation (1)) and logarithmic (equation (2)) logistic regression models. x-axis: frequency (%) of TWA-8 samples above 3 ppb (above 5 ppb for Ott et al. (2000) and Weill et al. (1981)) without respiratory protection (UP-3-frequency); y-axis: models: predicted yearly probability (%) of asthma consistent with being induced by TDI; study data: incidence rate per hundred person-years. The circled letters represent data from other studies: B = Bugler et al. (1991); O = Ott et al. (2000); W = Weill et al. (1981).
Excessive asthma incidence rates would be predicted from applying the linear model expressed in equation (1) to the group of employees that had spent 10–15% of their time even above 5 ppb (Ott et al., 2000: circled letter “O” in Figure 2; Weill et al., 1981: circled letter “W” in Figure 2). Reported incidence rates were between 0.7 and 1.8 per hundred person-years. For the “exposed” group in the work of Bugler et al. (1991), 7.5% of full-shift TWA samples were above 5 ppb, an estimated 20% were above 3 ppb, and incidence (43 cases, 521 participants, 4.3 years average participation) was 1.9 per hundred person-years (circled letter “B” in Figure 2). The monotonic and exponential “growth” that is implicit in the linear logistic model may have a limited range of applicability. While the estimate is conservative, more moderate incidence rates are predicted from applying the logarithmic model expressed in equation (2). Upon extrapolation, the logarithmic model thus seems to provide a prediction that is more in line with the results of other studies, and hence deserves preference. Inherently, it suggests the existence of a threshold below which induction of TDI-related asthma is not expected to occur.
It is also worth noting that the distribution of TWA values is very different in this data set versus what has been reported previously: a very low background with peaks in the study under consideration here, versus a background of 1.6–6.8 ppb as an arithmetic average with peaks reported by Weill et al. (1981). Both studies have very similar rates of asthma incidence (0.9 and 1.0 per hundred person-years, respectively), suggesting that, in the given range of exposure concentrations, the average TWA value (which does not take into account whether respiratory protection was used or not) does not represent the main factor influencing asthma incidence.
To conclude, it was determined (alternative model) that the incidence of asthma “consistent with being induced by TDI” is significantly related to the frequency of exposure to TWA-8 values above 3 ppb without respiratory protection being used. The limit of 3 ppb by itself as well as the preferred logarithmic logistic model (equation 2) both suggest the existence of a threshold. In this particular data set, the 3 ppb level is indicative of events rather than of general background concentrations. Another learning (Table 2) is that it is important to control both the “workplace atmosphere” under normal operation conditions as well as the “exposure” when the plant is intentionally or incidentally opened. The former is driven by technical measures to control the tightness of the plant. The latter is driven by situational awareness and organizational measures to encourage or enforce the appropriate use of respiratory protection.
Supplemental material
Supplemental Material, Part_II_-_Supplemental_Information_1 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part II—Exposure without respiratory protection to TWA-8 values indicative of peak events is a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_II_-_Supplemental_Information_2 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part II—Exposure without respiratory protection to TWA-8 values indicative of peak events is a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Acknowledgements
The authors acknowledge the support of the American Chemistry Council, acting on behalf of its Diisocyanates Panel, which granted access to the anonymized study data. The authors recognize Mr Robert J West of the International Isocyanate Institute, Inc. for support with the statistical analyses.
Notes
Middendorf et al. (2017) did calculate cumulative exposure values adjusted for the type of respiratory protective equipment used but didn’t use them for further analysis.
Remarkably, above average UP-3 frequencies correlate strongly with the percentage of new hires in the respective groups (data not shown).
Footnotes
Disclaimer: Any views expressed in this paper and any conclusions are those of the authors, not necessarily of the International Isocyanate Institute, Inc. or its member companies.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors are employed by the International Isocyanate Institute, Inc. The Institute is funded by producers of MDI and TDI.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded with regular membership fees of the International Isocyanate Institute, Inc. There is no other funding to report.
ORCID iD: Patrick M Plehiers  https://orcid.org/0000-0002-4630-5016
https://orcid.org/0000-0002-4630-5016
Supplemental material: Supplemental material for this article is available online.
References
- Bugler J, Clark RL, Hill H, et al. (1991) The Acute and Long-Term Respiratory Effects of Aromatic Diisocyanates. A Five Year Longitudinal Study of Polyurethane Foam Workers. Report no. 10848, Manchester: International Isocyanate Institute. [Google Scholar]
- Cassidy LD, Doney B, Wang ML, et al. (2017) Medical monitoring for occupational asthma among toluene diisocyanate production workers in the United States. Journal of Occupational and Environmental Medicine 59(Suppl.12): S13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark RL, Bugler J, McDermott M, et al. (1998) An epidemiology study of lung function changes of toluene diisocyanate foam workers in the United Kingdom. International Archives of Occupational and Environmental Health 71: 169–179. [DOI] [PubMed] [Google Scholar]
- Collins JJ, Anteau S, Conner PR, et al. (2017) Incidence of occupational asthma and exposure to toluene diisocyanate in the United States toluene diisocyanate production industry. Journal of Occupational and Environmental Medicine 59(Suppl.12): S22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings BJ, Booth KS. (2002) Industrial hygiene sampling for airborne TDI in six flexible slabstock foam manufacturing facilities in the United States: A comparison of the short-term and long-term sampling data. Applied Occupational and Environmental Hygiene 17(12): 863–871. [DOI] [PubMed] [Google Scholar]
- Middendorf PJ, Miller W, Feeley T, et al. (2017) Toluene diisocyanate exposure: Exposure assessment and development of cross-facility similar exposure groups among toluene diisocyanate production plants. Journal of Occupational and Environmental Medicine 59(Suppl.12): S1–S12. [DOI] [PubMed] [Google Scholar]
- Ott MG, Diller WF, Jolly AT. (2003) Respiratory effects of toluene diisocyanate in the workplace: A discussion of exposure-response relationships. Critical Reviews in Toxicology 33(1): 1–59. [DOI] [PubMed] [Google Scholar]
- Ott MG, Klees JE, Poche SL. (2000) Respiratory health surveillance in a toluene di-isocyanate production unit, 1967-97: Clinical observations and lung function analyses. Occupational and Environmental Medicine 57(1): 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plehiers PM, Chappelle AH, Spence MW. (2020) Practical learnings from an epidemiology study on TDI-related occupational asthma. Part I—Cumulative exposure is not a good indicator of risk. Toxicology and Industrial Health (Submitted 08 May 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk A, Preller L, Raulf-Heimsoth M, et al. (2007) Respiratory symptoms, sensitization, and exposure response relationships in spray painters exposed to isocyanates. American Journal of Respiratory and Critical Care Medicine 176(11): 1090–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang ML, Storey E, Cassidy LD, et al. (2017) Longitudinal and cross-sectional analyses of lung function in toluene diisocyanate production workers. Journal of Occupational and Environmental Medicine 59(Suppl.12): S28–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weill H, Butcher B, Dharmarajan V, et al. (1981) Respiratory and Immunologic Evaluation of Isocyanate Exposure in a New Manufacturing Plant. NIOSH Technical Report Publication No. 81-125 Morgantown: National Institute of Occupational Safety and Health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Part_II_-_Supplemental_Information_1 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part II—Exposure without respiratory protection to TWA-8 values indicative of peak events is a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health
Supplemental Material, Part_II_-_Supplemental_Information_2 for Practical learnings from an epidemiology study on TDI-related occupational asthma: Part II—Exposure without respiratory protection to TWA-8 values indicative of peak events is a good indicator of risk by Patrick M Plehiers, Anne H Chappelle and Mark W Spence in Toxicology and Industrial Health