Abstract
Osteoma of the external auditory canal is a rare benign tumor with an estimated incidence of 0.05% of total otologic surgeries. In most cases, an osteoma in the external auditory canal does not cause symptoms because the tumor grows slowly and does not occlude the ear canal. However, if the mass grows to occlude the external auditory canal, several symptoms can occur, including conductive hearing loss, aural fullness, and keratin debris accumulation. We present two cases of this rare tumor in a 23-year-old woman and a 19-year-old man. The mass was surgically excised at the level of the peduncle under local anesthesia with microscope assistance. The base of the excised mass was drilled with a diamond burr to remove all osseous lesions. Histopathologic findings showed spongiotic osteomas. In these cases, patients had symptoms of aural fullness, although the osteomas did not completely occlude the external auditory canal, and the symptoms improved after surgical excision without recurrence.
Keywords: Osteoma, spongiotic osteoma, external auditory canal, ear canal, pathology
Introduction
Osteoma is slow growing benign tumor and can occur in all regions of temporal bone including the external auditory canal (EAC), mastoid portion, squamous portion, middle ear, Eustachian tube, petrous apex, internal auditory canal, zygomatic process, glenoid fossa, and styloid process.1–3 Among them, EAC is the most common area of temporal bone osteoma.1–5 Osteoma of the EAC is a rare benign tumor with an estimated incidence of 0.05% of total otologic surgeries.4–7
Osteoma is a slow growing mass and usually produces no symptoms.2,3,6,8–10 However, a mass in the EAC that is suspicious for osteoma should be carefully evaluated, because a large osteoma can cause symptoms. Conductive hearing loss and aural fullness can occur when the canal is obstructed.4,6 Furthermore, complications such as EAC cholesteatoma can arise due to EAC obstruction by the osteoma.5,9
Several cases of osteomas in the EAC have already been reported regarding their associated complications and management. Nonetheless, considering the clinical significance of symptoms and complications resulting from EAC osteoma, we present two cases of this rare tumor of the spongiotic type seen in histopathology.
Case reports
Case 1
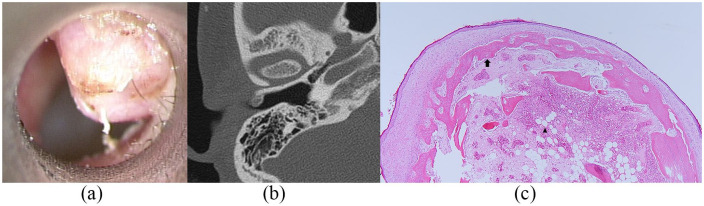
A 23-year-old woman visited our otorhinolaryngology clinic with symptoms of aural fullness in the right ear for several months. She had no history of repeated cold water irritation to the ear. On physical examination, an ovoid hard mass was observed in the right EAC (Figure 1(a)). Temporal bone computed tomography revealed a 0.5 cm × 0.5 cm anterior-based, pedunculated, bony mass originating from the tympanosquamous suture line (Figure 1(b)). Because the tumor was of bone origin, surgical excision was planned.
Figure 1.
(a) A 0.5 cm × 0.5 cm anterior-based, pedunculated, bony mass was observed in the right external auditory canal; (b) temporal bone computed tomography revealed a 0.5 cm × 0.5 cm anterior-based, pedunculated, bony mass originating from the tympanosquamous suture line, and (c) histopathologic image showed stratified squamous epithelium overlying the mass of trabeculae of mature lamellar bone (arrow) with a variable amount of fibrofatty marrow tissue (arrowhead) (hematoxylin-eosin, ×40).
With microscope assistance, the mass was surgically excised at the level of the peduncle via transcanal approach with the patient under local anesthesia. The pedunculated mass was broken easily with curette and alligator forceps. The base of the excised mass was drilled with a diamond burr to further remove all osseous lesions. The tympanic membrane was intact and there were no other lesions such as cholesteatoma medial to the excised osteoma. After excision, skin graft was not necessary because the skin defect was minimal, and the EAC was packed with gelfoam.
Histopathologic findings showed lamellated bone covered with stratified squamous epithelium with a variable amount of fibrofatty marrow tissue, consistent with spongiotic osteoma (Figure 1(c)). Two years and eight months after surgery, the patient is without symptoms and has not experienced any tumor recurrence.
Case 2
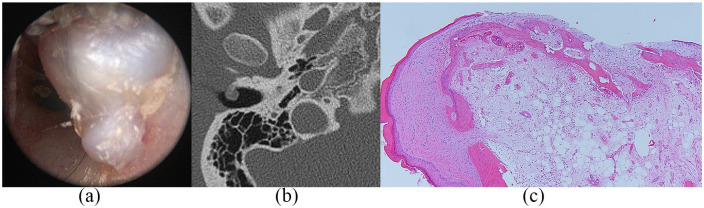
A 19-year-old man visited our otorhinolaryngology clinic with a known mass in the right EAC. He had reported mild symptoms with aural fullness for several years. On physical examination, an ovoid hard mass was observed in the right EAC (Figure 2(a)). Temporal bone computed tomography revealed a 0.6 cm × 0.5 cm anterior-based, pedunculated, bony mass originating from the tympanosquamous suture line (Figure 2(b)). Because the tumor was of bone origin, surgical excision was planned.
Figure 2.
A 0.6 cm × 0.5 cm anterior-based, pedunculated, bony mass was observed in the right external auditory canal: (a) transcanal view, (b) temporal bone computed tomography, and (c) histopathologic image.
As in Case 1, surgery was performed, and pathology revealed a spongiotic osteoma (Figure 2(c)). Two years and five months after surgery, the patient is without symptoms and there has been no tumor recurrence.
Discussion
Osteoma is a mesenchymal, osteoblastic, well-differentiated, mature tumor that usually grows slowly.1 Osteoma in the temporal bone is rare, and the most common site in the temporal bone is the EAC.1,2,4 The postulated osteoma etiologies include trauma, surgery, radiotherapy, chronic infection, and glandular factors such as pituitary dysfunction, but the precise etiology remains unknown.2–4,7 Similarly, EAC osteoma epidemiology is uncertain due to its low incidence. EAC osteoma affects patients from the second decade of life with an uncertain sex preponderance.11
EAC osteoma presents as a single, unilateral, pedunculated hyperdense mass originating from the tympanosquamous or tympanomastoid suture lines in computed tomography. T1-weighted magnetic resonance imaging may reveal a high signal intensity due to bone marrow within the mass.11 Histopathologically, osteoma has the characteristics of dense lamella, Harversian canals, and intertrabecular stroma.1 There are three types of osteomas that include compact, spongiotic, and mixed.1-3,11 The compact type is common and contains Harversian systems, whereas the spongiotic type has trabecular bone with marrow.2,11 To our best knowledge, only two cases of spongiotic osteoma in the temporal bone have been reported to date in the English literature.
In most cases, an osteoma in the EAC does not cause symptoms because the tumor grows slowly and does not occlude the ear canal. However, if the mass grows to occlude the EAC, several symptoms can occur, including conductive hearing loss, aural fullness, and keratin debris accumulation. The major complication of osteoma in the EAC is EAC cholesteatoma, a cyst formed by epithelial migration secondary to canal occlusion.9
Therefore, excision of an osteoma in the EAC should be considered, despite its rarity. Thus, the recommended treatment for a symptomatic EAC osteoma is surgical excision.2,4,8–11 Post-excisional EAC osteoma recurrence has not been reported.
Osteoma of the EAC usually originates lateral to the isthmus of the EAC, and its base is usually located at the tympanosquamous or tympanomastoid suture line.4 In the two present cases, each of the EAC osteomas was located at the tympanosquamous suture line lateral to the EAC isthmus.
Additionally, the osteomas did not completely occlude the EAC, so observation was possible. However, the two patients had symptoms, although not severe, and surgical excision was considered. Hempel et al.12 reported that surgery for ear canal exostosis and osteoma can significantly improve patient health-related quality of life if the symptoms existed before surgery, and they concluded that surgery should be considered when a patient reports symptoms that are due to the EAC mass. Likewise, we considered surgery in the present cases because the patients were symptomatic. Each patient was informed of mass size and the potential for growth, and both patients wanted excision.
EAC osteoma is similar to exostosis, and they should be differentiated. Although there have been debates over differentiating the two diseases, they are histopathologically different.13 Osteoma is usually single, unilateral, and pedunculated while exostosis is usually multiple, bilateral, and broad-based.11,13 Occurring more frequently in middle-aged men, exostosis has an incidence of 0.6% and is more common than EAC osteoma.11 Chronic irritation, such as cold water, wind, and repeated otitis externa, is related to the development of exostosis.11,13
A slow growing mass in the EAC should also be differentiated from fibrous dysplasia and ossifying fibroma. However, those are rarer than osteoma in temporal bone. Fibrous dysplasia reveals a typical radiopaque ground glass, ill-defined appearance in computed tomography and occurs at younger than 30 years most commonly.14,15 Histopathologically, it shows bony trabeculae with woven bone without lamellar transformation.14 In contrast, ossifying fibroma reveals a radiolucent, well-defined appearance in computed tomography and occurs in the third and fourth decades of life. Histopathologically, it shows evenly spaced spicules of woven bone with lamellar transformation at the periphery.14 Thus, osteoma can be differentiated from those by using radiologic and histopathologic evaluations.
Conclusion
EAC osteoma is rare and can be observed without immediate therapy if there are no symptoms. However, excision should be actively considered in symptomatic patients for the following reasons: osteomas can grow, surgical excision is more difficult with larger masses, and EAC cholesteatomas can develop secondary to EAC obstruction.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval to report this case series was obtained from the Institutional Review Board of the National Health Insurance Service Ilsan Hospital (NHIMC 2019-04-029).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT) (No. 2019R1F1A1062649).
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Junhui Jeong  https://orcid.org/0000-0002-1592-261X
https://orcid.org/0000-0002-1592-261X
References
- 1. Jeong J, Choi YJ, Hong CE, et al. Giant osteoma in the mastoid of the temporal bone: complete excision of a rare tumor. Otol Neurotol 2018; 39(9): e894–e896. [DOI] [PubMed] [Google Scholar]
- 2. Abhilasha S, Viswanatha B. Osteomas of temporal bone: a retrospective study. Indian J Otolaryngol Head Neck Surg 2019; 71(Suppl. 2): 1135–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mahalle S. Osteoma of external auditory canal associated with external auditory canal cholesteatoma and exuberant granulation tissue in mastoid air cell system: a rare association. Indian J Otolaryngol Head Neck Surg 2019; 71(Suppl. 2): 1505–1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee DH, Jun BC, Park CS, et al. A case of osteoma with cholesteatoma in the external auditory canal. Auris Nasus Larynx 2005; 32(3): 281–284. [DOI] [PubMed] [Google Scholar]
- 5. Iaccarino I, Bozzetti F, Piccioni LO, et al. A case of external auditory canal osteoma complicated with cholesteatoma, mastoiditis, labyrinthitis and internal auditory canal pachymeningitis. Acta Otorhinolaryngol Ital 2019; 39(5): 358–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Salami A, Mora R, Dellepiane M, et al. Piezosurgery for removal of symptomatic ear osteoma. Eur Arch Otorhinolaryngol 2010; 267(10): 1527–1530. [DOI] [PubMed] [Google Scholar]
- 7. Gheorghe DC, Stanciu AE, Ulici A, et al. Bilateral external ear canal osteomas: discussion on a clinical case. J Med Life 2016; 9(4): 434–436. [PMC free article] [PubMed] [Google Scholar]
- 8. Bahgat M, Bahgat Y, Bahgat A, et al. External auditory canal osteoma. BMJ Case Rep 2012; 2012: bcr006745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ata N, Övet G, Alatas N, et al. External auditory canal osteoma with cholesteatoma and sinus thrombosis. J Craniofac Surg 2015; 26(7): 2234–2235. [DOI] [PubMed] [Google Scholar]
- 10. Chen CK, Chang KP, Chien CY, et al. Endoscopic transcanal removal of external auditory canal osteomas. Biomed J. Epub ahead of print 21 April 2020. DOI: 10.1016/j.bj.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carbone PN, Nelson BL. External auditory osteoma. Head Neck Pathol 2012; 6(2): 244–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hempel JM, Forell S, Krause E, et al. Surgery for outer ear canal exostoses and osteomata: focusing on patient benefit and health-related quality of life. Otol Neurotol 2012; 33(1): 83–86. [DOI] [PubMed] [Google Scholar]
- 13. Grinblat G, Prasad SC, Piras G, et al. Outcomes of drill canalplasty in exostoses and osteoma: analysis of 256 cases and literature review. Otol Neurotol 2016; 37(10): 1565–1572. [DOI] [PubMed] [Google Scholar]
- 14. Goh EK, Cho KS, Lee IW, et al. A case of isolated ossifying fibroma of the mastoid cavity of the temporal bones. Am J Otolaryngol 2006; 27(5): 358–361. [DOI] [PubMed] [Google Scholar]
- 15. Zhang K, Qu P, Wang B, et al. Management of the temporal bone fibrous dysplasia with external auditory canal stenosis and secondary cholesteatoma in an Asian population: a 11-case series. Ear Nose Throat J. Epub ahead of print 22 May 2020. DOI: 10.1177/0145561320927922. [DOI] [PubMed] [Google Scholar]