Abstract
Limited funding across health and social service programs presents a challenge regarding how to best match resources to the needs of the population. There is increasing consensus that differences in individual characteristics and care needs should be reflected in variations in service costs, which has led to the development of case-mix systems. The present study sought to develop a new approach to allocate resources among children and youth with intellectual and developmental disabilities (IDD) as part of a system-wide Medicaid payment reform initiative in Arkansas. To develop the system, assessment data collected using the interRAI Child and Youth Mental Health-Developmental Disability instrument was matched to paid service claims. The sample consisted of 346 children and youth with developmental disabilities in the home setting. Using automatic interactions detection, individuals were sorted into unique, clinically relevant groups (ie, based on similar resource use) and a standardized relative measure of the cost of services provided to each group was calculated. The resulting case-mix system has 8 distinct, final groups and explains 30% of the variance in per diem costs. Our analyses indicate that this case-mix classification system could provide the foundation for a future prospective payment system that is centered around stability and equitability in the allocation of limited resources within this vulnerable population.
Keywords: Case-mix, intellectual and developmental disability, children and youth, interRAI
Introduction
Due to limited funding across health care sectors, including mental health, there is an ongoing challenge of how best to match resources to the needs of the population.1,2 Historically, many service sectors fund based on a standard rate per client as opposed to the complexity of their needs.3 An unfortunate result of this funding structure is that it leaves some agencies underfunded, particularly those that serve resource-intensive clients. Over the past few decades, there has been increasing recognition within the healthcare field that variations in individual characteristics and complexity should be reflected through variations in service costs; this has led to the development of case-mix classification systems.
Case-mix modeling integrates assessment information (ie, combination of individual characteristics) and resource data, most commonly to group individuals together based on similar resource requirements.4 Hence, case-mix systems usually describe the comparative resource needs of various groups, with payment systems subsequently attaching a dollar value to the different case-mix groups.3 Utilizing a case-mix approach allows system planners and funders to ensure the allocation of resources are driven by the needs of service recipients, rather than numbers, thereby facilitating more equitable access to health services, and ultimately better care. The feasibility of a case-mix approach has been demonstrated in a number of healthcare settings, including acute care hospitals (eg, diagnosis-related groups, DRGs) and nursing homes (eg, Resource Utilization Groups [RUG-IV]).5-7 Notably, while case-mix is used in institutional settings for determining facility payment, in the community setting, case-mix is used to determine the allocation of resources (eg, determining level of service, such as the maximal number of hours) or funding (such as a voucher for services). As the latter is at the level of an individual, and as the availability of natural supports (eg, informal caregivers) can vary, case-mix assignment in community settings should allow for additional discretion in the actual allocation.8 For example, the dependent variable in the RUG-III system, which was developed for home care settings, used both weighted informal and formal support costs.9,10
Case-mix classification systems are generally categorized into 2 types, namely index or grouping systems.11 All the previously referred to systems are considered grouping systems because they designate individuals into relatively homogenous groups based on their anticipated resource needs. Every group is assigned a “case-mix index” (CMI), which represents its anticipated resource use in comparison to the population average. In contrast, index systems will assign specific weights or “points” to distinctive elements of a case, which produces a numerical value that denotes the expected level of resource use for that case.11 A notable drawback of this type of system is the difficulty exploring numerous, high-order statistical interactions, which are quite common within these systems; this occurs when a certain characteristic is only important for a particular client, but not for others. One potential way of resolving this issue is by utilizing classification analysis to develop groups, such as automatic interactions detection (AID), which also has the benefit of providing both clinically, real-world meaningful and distinct groups.12
There are a number of factors to consider when developing a case-mix classification system. In particular, past literature has suggested that these systems should meet 3 types of criteria, including statistical, clinical, and incentives.13,14 One of the most important statistical criterion is the system’s ability to describe resource use, as measured by the percentage of variance in resources explained by the classification. With respect to the clinical criterion, the case-mix system will only be practical if it makes clinical sense, such that individuals within a particular group share clinical characteristics. Lastly, it is recognized that when case-mix algorithms are used for funding (ie, in prospective payment or resource allocation systems), they have the potential to change behaviors of service providers by creating incentives and disincentives. Therefore, when developing a classification system, it is crucial to consider whether including a variable will influence service delivery, or the reporting of a condition on an assessment. For example, if using restraints on a patient was associated with higher payment, there would be more of an incentive to restrain individuals rather than address the underlying issues associated with restraint use, resulting in a problematic resource allocation system. Case-mix development should also take into consideration the potential ambiguity of a variable; for example, whether it results in more than one way to classify an individual.15 This is an important concern as ambiguity may incentivize providers to select the classification that maximizes funding.
The Arkansas Division of Developmental Disability Services (ARDDS) sought a case-mix system to inform resource allocation for children and youth with intellectual and developmental disabilities (IDD), as part of a system-wide payment reform initiative for Medicaid. The ARDDS was specifically interested in looking into home and community-based services because there is currently very little guidance within this particular realm due to extensive variability. The present study describes the development efforts of a case-mix system for this younger target population, which uses the same approach we employed to develop the classification system for adults.16
Method
Study sample
A statewide consensus on the needs and characteristics of present clients was undertaken by the ARDDS in 2013. A total of 346 children and youth with developmental disabilities were assessed, all living in private homes. It should be noted that the sample comprised of all children cared for in their home under this particular Arkansas program over a 2-year period (ie, represents 100% of the population receiving the above-mentioned services between 2011-2013). The dependent variable, or “cost” variable, in this case-mix analysis was derived by linking each assessment record with paid claims for specific home and community-based services. Medicaid paid service claims were linked to identified patient data, and the resulting data set was de-identified per approval by the University of Michigan Institutional Review Board; thus, all subsequent analyses were conducted using de-identified data. Furthermore, all 346 children and youth had useable claims, so they were all included in the derivation of the case-mix system. Finally, the data were collected as part of routine care provided by the State of Arkansas, therefore informed consent was not needed and there was no selection bias.
Instrumentation
The ARDDS used the interRAI Child and Youth Mental Health and Developmental Disability (ChYMH-DD) instrument to assess all service users.17 This instrument is part of the interRAI integrated suite of assessment instruments. interRAI is a non-profit collaborative that is composed of clinicians and researchers from over 35 countries who are committed to improving the support and lives of vulnerable persons across the lifespan (www.interrai.org). Notably, 26 US states have adopted various interRAI instruments primarily for clinical purposes, however, some also use it for case-mix allocation, level of care determination, or quality measurement.
The ChYMH-DD is a comprehensive functional assessment intended for young persons aged 4 to 20 years living in community or inpatient settings, who have comorbid developmental disability/disabilities and mental health concerns. It includes items related to major life domains, such as education and employment, functioning, communication, cognitive/executive functioning, behavior, strengths and resilience, natural supports (ie, unpaid caregivers, such as family and friends), and physical and mental health. Assessment data are gathered via a semi-structured interview format, using all available sources of information (eg, conversations with parents/guardians, the child/youth, and teachers; medical and education records; and clinical observations). The instrument is accompanied by a detailed manual that outlines the intent, definition, and coding rules for each item.17 All of these result in a comprehensive assessment that is both reliable and valid.
Furthermore, the ChYMH-DD includes multiple scales and algorithms comprised of particular items to capture the complexity of areas of need, such as the activities of daily living (ADL) and instrumental activities of daily living (IADL) scales. The ADL scale informs on a child or youth’s ability to perform ADL, such as personal hygiene, dressing, and bathing; the IADL scale informs on a child or youth’s ability to perform IADL, such as housework, using technology, and schoolwork. Evidence of strong validity and reliability of a number of the scales and algorithms incorporated into this tool is provided elsewhere.18-21
Resource use
Each ChYMH-DD assessment record was linked to Medicaid paid service claims over a 2-year period, from July 2011 to June 2013. A particular group of Medicaid state plan and waiver services were selected by ARDDS from the full spectrum of service types; notably, this comprised all major cost centers funded under the state’s waiver, as well as a few rare ones that were of particular interest to ARDDS. The vast majority of the costs (94.3%) were payments for “supportive living,” an umbrella service that includes a wide range of personal assistance and community supports, with the remainder including adaptive equipment, specialized medical supplies, environmental modifications (eg, house ramps, enlarged doors), respite, and consultation (please refer to the Appendix for more detail). Three of the service types represented quite rare cost centers (ie, environmental modifications, adaptive equipment [per service], and specialized medical supplies) and should ideally be excluded from a case-mix system, but were included at the request of the ARDDS. Subsequent analyses (not shown) demonstrated that their inclusion did not affect the results. The inclusion of the costs of unpaid caregivers (ie, natural supports from family and friends) was also considered; however, it did not improve the case-mix model. It should be noted that omission of natural supports from the model is in line with the intended purpose of the case-mix system, which is to inform formal care resource allocation based on an individual’s needs (ie, our best estimate of an individual’s needs based on past resource use). Furthermore, privately paid care services were also not included in the model for the same reason as just described, as the purpose of this system is to allocate state funds for state covered services.
Analytic Methods
The analysis employed the AID package within the SAS Enterprise Guide (Data Miner analytic package, Version 4.3), to develop the classification system (ie, to sort the children and youth into unique, clinically relevant groups) and calculate the CMIs (ie, a standardized relative measure of the cost of services provided to each group). AID is a type of cluster analysis in which a large sample is divided into smaller, homogenous subsets in order to best explain a dependent variable based on a given set of predictors. As such, all the data points within the assessment are used to divide the sample into smaller groupings using a recursive set of splits. In developing the current case-mix, each split was based on person characteristics (ie, values of an independent variable), selected to maximize the predictive ability of resource use (ie, the dependent variable). This approach is advantageous in that the resulting subgroups from the various splits reflect personal characteristics that are associated with resource use in different subpopulations. As all potential variables in the assessment data were considered at each split, AID helps the user to select measures that make “clinical sense” and to avoid the inclusion of those that could provide negative incentives. A number of different initial splits were tested and analyzed in the development of the present case-mix system, similarly to our previous work.16 Finally, we calculated the CMIs by norming the mean cost for all observations in a particular group to a relative value (ie, by dividing by the mean cost for a selected, numerous group). The resulting classification system was dubbed “Child and Youth Resource Index” (ChYRI).
Results
Selected characteristics of the overall sample population are presented in Table 1. The average age was approximately 13 years, and there were slightly more boys than girls within the sample. The majority of the parents of the children and youth were married (52%) and approximately 20% were separated or divorced. Over half of the sample population had both parents as their legal guardians, whereas 8% had a child protection agency. Further, approximately 20% had either been in 1 or multiple foster families, and just under 5% had experienced residential instability in the last 2 years.
Table 1.
Selected characteristics of sample population (N = 346).
| Mean age, y | 12.9 |
| % male | 63.9 |
| Marital status of parents | |
| Never married | 17.3% |
| Married | 52.0% |
| Partner or significant other | 0.6% |
| Widowed | 2.9% |
| Separated | 2.0% |
| Divorced | 17.1% |
| Marital status unknown | 8.1% |
| Guardianship | |
| Both parents | 57.5% |
| Mother only | 24.6% |
| Father only | 3.5% |
| Neither parents, but other relative(s) or non-relative(s) | 5.8% |
| Child protection agency | 8.1% |
| Public guardian | 0.6% |
| Youth responsible for self | 0.0% |
| History of foster placement | |
| None | 78.3% |
| 1 foster family | 8.7% |
| Multiple foster families | 13.0% |
| Residential instability over the last 2 y | 4.3% |
| Top diagnoses | |
| Autism spectrum | 26.0% |
| Learning disorder | 22.8% |
| Communication disorder | 15.9% |
| Substantial physical dysfunction | |
| Extensive assistance (in 1 + ADLs) | 81.0% |
| Maximal assistance (in 1 + ADLs) | 74.5% |
| Violence to others within the last year | 3.5% |
| Considered performing a self-injurious act within the last year (ie, self-injurious ideation or attempt) | 4.0% |
| Full paralysis | 2.3% |
| Fetal alcohol effects or syndrome | 1.7% |
The top 3 diagnoses amongst the sample were autism spectrum, learning disorder, and communication disorder, and just under 2% had a medical diagnosis of fetal alcohol effects or syndrome. Approximately 3.5% had engaged in violence towards others, and 4% had thought about or attempted self-injury within the last year. Finally, about 80% of service recipients required extensive assistance in 1 or more ADLs, whereas about 75% required maximal assistance; just over 2% were fully paralyzed. Table 2 provides more detail on the functioning of the sample population. Notably, service recipients required the most assistance with washing their hair, and the least assistance with locomotion.
Table 2.
Functioning of sample population (N = 346).
| ADL | % Maximal assistance | % Extensive assistance |
|---|---|---|
| Personal hygiene | 69.69 | 61.47 |
| Bathing | 67.71 | 60.06 |
| Washing hair | 75.92 | 68.56 |
| Dressing upper body | 54.39 | 45.33 |
| Dressing lower body | 57.79 | 48.16 |
| Locomotion | 27.76 | 25.78 |
| Eating | 33.14 | 29.18 |
| Toilet use | 63.17 | 56.37 |
| Transfer toilet | 38.2 | 36.26 |
| Stairs | 47.98 | 46.53 |
Abbreviation: ADL, activities of daily living.
Case-Mix Classification System
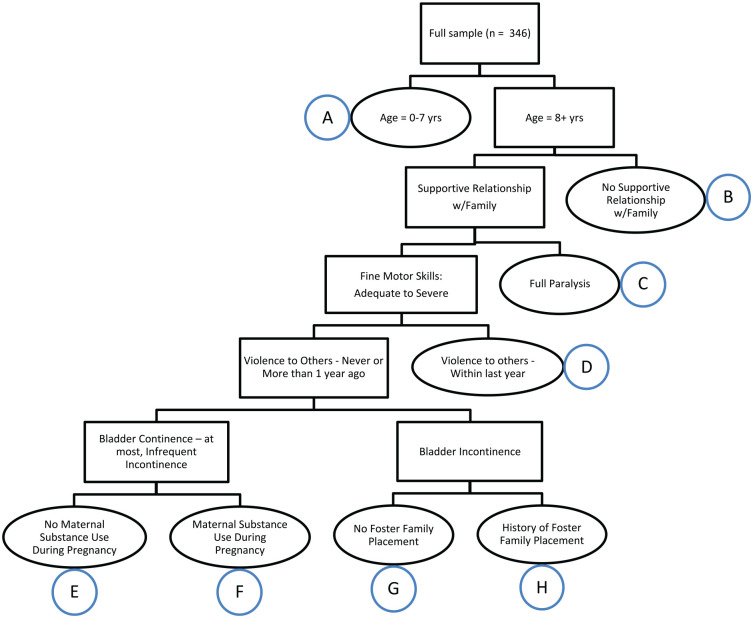
Various individual characteristics were modeled as initial “splits” when developing the classification system, such as age, level of functioning, and diagnosis. Through the modeling, age was found to be the most powerful predictor of costs. When split into 2 distinct categories, namely 0 to 7 years compared to 8-years and above (Figure 1), age explained 15.7% of the variance in per-diem costs.
Figure 1.
The case-mix groups for Children and Youth with Developmental Disabilities classification system.
Subsequent splits were made using individual-level characteristics that possessed both clinical and statistical significance, including familial factors (eg, supportive relationship with family, history of foster family placement), violence to others, and functional characteristics (eg, bladder continence). The final ChYRI system has 8 distinct final groups; sample size prevented examination of further splits. Overall, the ChYRI system explained 30% of the variance in total per diem costs.
Case-mix weights
CMIs were established by applying the system to the entire sample of 346 children and youth. Each group’s mean per diem costs was normalized by dividing by the mean cost for a numerous group with per diem cost close to the mean for the population. The per diem cost of the largest group was normalized to 1.00—that is, group “G,” with 134 individuals and a mean per diem cost of $88.95 (see the row in bold in Table 3). It is important to highlight that the selection of a normalization constant does not impact any payment system, or other use of CMIs, because these values are all relative.
Table 3.
ChYRI groups, CMIs, and CV.
| ChYRI | N | Mean per diem cost ($) | CV | CMI |
|---|---|---|---|---|
| A | 15 | 123.77 | 0.35 | 1.39 |
| B | 20 | 166.16 | 0.40 | 1.87 |
| C | 8 | 178.43 | 0.22 | 2.01 |
| D | 10 | 119.72 | 0.80 | 1.35 |
| E | 124 | 65.47 | 0.60 | 0.74 |
| F | 11 | 91.88 | 0.37 | 1.03 |
| G | 134 | 88.95 | 0.47 | 1.00 |
| H | 24 | 122.90 | 0.43 | 1.38 |
| Total | 346 | 91.91 | 0.59 | 1.03 |
Abbreviations: ChYRI, case-mix groups for Developmental Disability—Children and Youth; CMI, case-mix index; CV, coefficient of variation.
The CMIs had a 3-to-1 range. Individuals who were 8-years of age or older, had no supportive relationship with their family, and were fully paralyzed, were in the most expensive group (“C”, with CMI = 2.01). In contrast, individuals who were 8-years of age or older, had a supportive relationship with their family, were not fully paralyzed, had no history of violence in the last year, were bladder continent, and had no history of maternal substance use during pregnancy were in the least expensive group (“E”, with CMI = 0.74). Overall, the ChYRI system reduced the coefficient of variation (CV) for groups, a measure of dispersion of costs; only 2 groups had CVs larger than that of the total population.
Discussion
An unfortunate reality within the healthcare system is that when State Medicaid programs are searching for a case-mix system for child and youth services, they often apply some type of variation of a model developed for adults. This is a problematic practice because children and youth are significantly different to adult service users, for example, with respect to types of difficulty and relevant contextual factors. Notably, while we have previously developed a case-mix system for adults with developmental disabilities using the interRAI ID assessment tool,16 the present study used an assessment instrument specifically for children and youth, the ChYMH-DD, to develop a case-mix model for this younger population with IDD living in private homes.
The ChYRI case-mix classification system explains 30% of the variance in per diem costs for a particular set of community-based and home services. This percentage of variance explained is comparable to the findings from other case-mix systems developed for particular settings and populations.6,9 For example, our case-mix model for adults with DD explained 26% of the variance in costs.16 Specific to the child and youth population facing special health care challenges, a study conducted by Phillips22 used the interRAI Pediatric Home Care Assessment to develop a resource utilization system, namely, the Pediatric Home Care/Expenditure Classification Model (P/ECM). This model explained 41% of the variance in costs; however, children with IDD only accounted for a portion of the whole sample (ie, the sample population also included children and youth with medical, psychological, and developmental health conditions).
More recently, Phillips23 developed the Pediatric Personal Care Allocation Model for Home Care (PCAM), again for children and youth facing special health care challenges. This case-mix model was similar to the P/ECM, except the dependent variable used in this study was the number of Medicaid Personal Care Services (PCS) hours as opposed to Medicaid home care expenditures. The PCAM explained 27% of the variance in the allocation of PCS hours. Within their discussion of potential reasons that this model explained less variance compared to others, the author commented on the relatively low CV for CMIs within the PCAM (CV = 1.49); importantly, less variance (ie, lower CV) is typically associated with lower levels of explained variance in a model. Therefore, similar reasoning can be applied to the ChYRI, as its CV for CMIs is 0.59.
One somewhat obvious limitation of the present study is in regard to its generalizability. The case-mix groups and CMIs were derived based on a single Medicaid program in one state for a particular set of services; as previously noted, the ARDDS was specifically interested in looking into home and community-based services because of the lack of guidance within this particular domain due to extensive variability. Therefore, future research is needed to determine whether the results can be applied to different jurisdictions. However, governments could potentially derive their own CMIs using a different set of cost centers, while keeping the ChYRI grouping. It is important to note that the selection of which cost centers to include can be complicated, for example, there is debate on whether to include environmental modifications or natural supports. Another important limitation—one that is common to virtually all case-mix systems in the health arena—is that they can only tell us about differences in care received, not necessarily differences in care needed,4 which can be affected by state policy, practice patterns, and significant barriers to access services. Thus, a case-mix model does not identify the “optimal” amount of care or resources needed for each individual—it simply aids in the distribution of whatever resources are being provided under the assumption that the care provided is appropriate. Finally, sex and gender were considered as grouping measures, but were never found to be statistically significant in our sample. It is possible that such differences might be detected if there was a larger sample, therefore, this is another limitation of the study.
Despite these limitations, the case-mix system presented in this study provides a useful model for identifying and grouping children and youth who have similar service needs within a specific population. Overall, the ChYRI has a 3-to-1 range in costs, and is able to identify persons with expensive needs, albeit these individuals are quite rare. The model does so by using the ChYMH-DD assessment tool, which is specifically tailored to identify the needs of children and youth with IDD, and help plan for appropriate services. While this case-mix model is only the first step in the implementation of a case-mix-based prospective payment system, it is an important one.
Conclusion
Over the last several decades, case-mix systems have been a central part of the discussions around reimbursement for all types of health care services, effectively becoming an area where research and policy development intersect. Unfortunately, the mental health sector has lagged behind the general health sector in developing these types of systems. However, the present study, in conjunction with our previous work that developed a case-mix model for adults with DD, provide a small step forward within the broader movement toward “managed care” models, and away from “fee-for-service” reimbursement. Notably, our results indicate that the ChYRI classification system can be the foundation for a future case-mix approach to reimbursement that is centered around stability and fairness in how limited resources are allocated within this vulnerable group.
It is important to emphasize that the ChYRI is intended to be used as a guideline to aid with decision-making around allocation of resources. It should not be viewed as a strict prescription, and does not constitute the ultimate allocation cap for resources. Moreover, assignment for a specific CMI is surrounded by a “corridor” or buffer, meaning that the CMI of a group is simply the basis for a “presumptive” assignment and can be viewed as a starting point, but then moves up or down based on a number of other important factors, including the availability of natural supports.
It is also important to remember that the field of case-mix classification systems, particularly for children and youth with mental health challenges, is in its infancy. To aid in future research and development within this specific field, Martin et al24 have outlined areas of particular importance:
“(1) Completeness of cases: that providers collect and report information on all children seen.
(2) Completeness of records: that providers collect and record information on all key variables about the children they see.
(3) Connectedness: developing a facility to link episodes of care from the same patient across services and providers, such as between health, social, and school-based care.
(4) Standardization: encourage the use of standardized tools for data capture to ensure comparability of data.
(5) Comprehensiveness: extending the range of information collected to include information on diagnoses and aetiology.”
Notably, the interRAI suite of assessment tools address many of these areas deemed important to consider when developing future case-mix classification systems. For example, the interRAI ChYMH-DD is a comprehensive, standardized assessment instrument that collects health information across a number of major life domains (eg, education and employment, cognitive and behavioral functioning, natural supports, and physical and mental health). Moreover, its accompanying manual helps facilitate standardization, ensuring that assessments are valid and reliable. The ChYMH-DD can also be implemented as standard of care within mental health organizations, as has been done across agencies and certain provinces within Canada. Critically, the interRAI suite uses a common language across tools for the purpose of enhancing communication between health settings, and contributing to a continuity of care for individuals as they receive services across sectors.
Finally, an added advantage to using the interRAI assessment tools is that there is no need for additional assessment, in contrast with other case-mix and assessment systems. This means that a child or youth is not subjected to multiple assessment processes, which can oftentimes be overlapping, expensive, and potentially intrusive. Therefore, while the information generated from the ChYMH-DD can be used for multiple purposes–starting with support planning, but including measuring quality, screening, and policy analysis—the use for case mix is a key application to assist in allocating care resources for children and youth with intellectual and developmental disabilities.
Acknowledgments
The authors would like to sincerely thank the children, youth, and their families, along with the service providers within the agencies for their participation in the research.
Appendix
Appendix.
Cost center distributions.
| Per diem service payments | Mean | Percent of total |
|---|---|---|
| Supportive living | $86.68 | 94.3 |
| Respite care | $1.06 | 1.2 |
| Environmental modifications | $0.21 | 0.2 |
| Adaptive equipment | $0.22 | 0.2 |
| Consultation | $0.82 | 0.9 |
| Specialized medical supplies | $0.11 | 0.1 |
| Other | $2.81 | 3.1 |
| Total per diem payments | $91.91 | 100.0 |
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research was supported by the Arkansas Universal Assessment Project, Contract No. 4600031762 from the State of Arkansas to the University of Michigan. Nevertheless, the opinions expressed here are those of the authors and do not represent the official position of the State of Arkansas.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: The data used in this study were prepared by BEF. All authors were involved in evaluating the statistical analysis, writing, and reviewing the final manuscript.
ORCID iD: Angela Celebre  https://orcid.org/0000-0001-9994-7998
https://orcid.org/0000-0001-9994-7998
References
- 1. Hewlett E, Moran V. Making mental health count: the social and economic costs of neglecting mental health care. Published 2014. Accessed March 10, 2020 10.1787/9789264208445-en [DOI]
- 2. Knapp M. Economic evaluation and mental health: sparse past . . . fertile future? J Ment Health Policy Econ. 1999;2:163-167. [DOI] [PubMed] [Google Scholar]
- 3. Hirdes JP, Fries BE, Morris JN, et al. Integrated health information systems based on the RAI/MDS series of instruments. Healthc Manage Forum. 2000;12:30-40. [DOI] [PubMed] [Google Scholar]
- 4. Phillips CD. Case-mix adjustment. In: Mullner R, ed. Encyclopedia of Health Services Research, Vol. 1 Sage Publications; 2009: 129-132. [Google Scholar]
- 5. Vladeck BC, Kramer PS. Case mix measures: DRGS and alternatives. Annu Rev Public Health. 1988;9:333-359. [DOI] [PubMed] [Google Scholar]
- 6. Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a case-mix measure for nursing homes: resource utilization groups (RUG-III). Med Care. 1994;32:668-685. [DOI] [PubMed] [Google Scholar]
- 7. Centers for Medicare and Medicaid Services. MDS 3.0 for nursing homes and swing bed providers. Updated 2015. Accessed March 14, 2020 https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIMDS30.html
- 8. James ML, Fries BE, Goodell M, Wellens N. Design principles for HCBS case mix: a primer. Published June 2015. Accessed March 10, 2020 http://www.advancingstates.org/sites/nasuad/files/HCBS%20Case%20Mix%20Primer.pdf
- 9. Björkgren MA, Fries BE, Shugarman LR. A RUG-III case-mix system for home care. Can J Aging. 2000;19:106-125. [Google Scholar]
- 10. Poss JW, Hirdes JP, Fries BE, McKillip I, Chase M. Validation of resource utilization groups version III for home care (RUG-III/HC): evidence from a Canadian home care jurisdiction. Med Care. 2008;46:380-387. [DOI] [PubMed] [Google Scholar]
- 11. Costa AP, Poss JW, McKillop I. Contemplating case mix: a primer on case mix classification and management. Healthc Manage Forum. 2015;28:12-15. [DOI] [PubMed] [Google Scholar]
- 12. Morgan JN, Sonquist JA. Problems in the analysis of survey data, and a proposal. J Am Stat Assoc. 1963;58:415-434. [Google Scholar]
- 13. Schneider DP, Fries BE, Foley WJ, Desmond M, Gormley WJ. Case mix for nursing home payment: resource utilization groups, version II. Health Care Financ Rev. 1998;annual suppl:39-52. [PMC free article] [PubMed] [Google Scholar]
- 14. Fries BE. Comparing case-mix systems for nursing home payment. Health Care Financ Rev. 1990;11:103. [PMC free article] [PubMed] [Google Scholar]
- 15. Tran N, Poss KW, Perlman C, Hirdes JP. Case-mix classification for mental health care in community settings: a scoping review. Health Serv Insights. 2009;12:1178632919862248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fries BE, James ML, Martin L, Head MJ, Park PS. A case-mix system for adults with developmental disabilities. Health Serv Insights. 2019;12:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Stewart SL, LaRose L, Gleason K, et al. interRAI Child and Youth Mental Health – Developmental Disabilities (ChYMH- DD) Assessment Form and User’s Manual. Version 1. interRAI; 2015. [Google Scholar]
- 18. Lau C, Stewart SL, Saklofske DH, Tremblay PF, Hirdes J. Psychometric evaluation of the interRAI Child and Youth Mental Health Disruptive/Aggression Behaviour Scale (DABS) and Hyperactive/Distraction Scale (HDS). Child Psychiatry Hum Dev. 2018;49:279-289. [DOI] [PubMed] [Google Scholar]
- 19. Lau C, Stewart SL, Saklofske DH, Hirdes J. Scale development and psychometric properties of internalizing symptoms: the interRAI Child and Youth Mental Health internalizing subscale. Psychiatry Res. 2019;278:235-241. [DOI] [PubMed] [Google Scholar]
- 20. Stewart SL, Morris JN, Asare-Bediako Y, Toohey A. Examining the structure of a new pediatric measure of functional independence using the interRAI Child and Youth Mental Health assessment system. Dev Neurorehabil. 2019;23:526-533. [DOI] [PubMed] [Google Scholar]
- 21. Stewart SL, Hamza CA. The Child and Youth Mental Health Assessment (ChYMH): an examination of the psychometric properties of an integrated assessment developed for clinically referred children and youth. BMC Health Serv Res. 2017;17:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Phillips CD. The pediatric home care/expenditure classification model (P/ECM): a home care case-mix model for children facing special health care challenges. Health Serv Insights. 2015;8:35-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Phillips CD. The pediatric personal care allocation model for home care (PCAM): a personal care case-mix model for children facing special health care challenges. Health Serv Insights. 2018;11:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martin P, Davies R, Macdougall A, et al. Developing a case mix classification for child and adolescent mental health services: the influence of presenting problems, complexity factors and service providers on number of appointments. J Ment Health. 2017;29:1-8. [DOI] [PubMed] [Google Scholar]