Abstract
Background
Duchenne muscular dystrophy is a genetic disease characterized by gradual loss of motor function, respiratory failure and cardiomyopathy. During the time of the global coronavirus pandemic, maintenance of social distancing and self-isolation might complicate regular multidisciplinary care of patients with Duchenne muscular dystrophy but on the other hand may lead to new medical care telehealth solutions. The aim of the study was to investigate patients’ situation regarding rehabilitation in the pandemic, to establish an online rehabilitation program and motor assessment and to determine the needs of telerehabilitation in this group.
Methods
The project involved 69 boys with Duchenne muscular dystrophy. The rehabilitation program was presented during online workshops for patients and caregivers. The same program was recorded on video and published in the internet. The online motor assessment tool consisted of six motor tests, caregivers were asked to perform the tasks and share a photograph of the patient’s posture using a designed app.
Results
In the nonambulant group the emphasis was placed on chest physiotherapy, stretching of upper extremities, positioning and wheelchair ergonomics. The program for the ambulant group focused on lower extremities stretching and full body exercises. Response rate for the workshops for ambulant patients was 29.7%, and only 9.0% for nonambulant patients. Videos showing exercises were displayed 132 times within a month.
Conclusion
With the physiotherapist guidance (online communication or video) patients with caregivers’ help can continue home based rehabilitation. Online videos/instructions/video guidelines are more acceptable by parents/caregivers of patients with Duchenne muscular dystrophy than live workshops.
Keywords: Neuromuscular disease, Digital rehabilitation, Home-based exercise, Motor assessment, Physical therapy
Introduction
Duchenne muscular dystrophy (DMD) is one of the most severe and commonly diagnosed neuromuscular dystrophies. The etiology of this congenital X‑linked disease affecting 1 in 3500–6000 boys, are mainly deletions, duplications or point mutations of the dystrophin gene. Its product, dystrophin protein, in healthy individuals is responsible for creating muscular structure of an internal fibre cytoskeleton. In the clinical course of DMD, patients develop gradual loss of motor function, gait abnormalities, progressive respiratory failure and cardiomyopathy [1].
Currently, there is no documented evidence of a higher incidence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection among DMD patients; however, characteristic features of advanced DMD stages, such as chest or diaphragm muscle weakness, kyphoscoliosis, impaired cough reflex and airway clearance, deterioration of cardiac function, obesity and steroids intake altogether may predispose to the severe course of coronavirus disease 2019 (COVID-19). It may manifest as pneumonia, acute respiratory distress syndrome, cardiomyopathy and, finally, may lead to death [2, 3].
The DMD patients and their families should follow the World Health Organization (WHO) recommendations applicable for the general population, such as regular and thorough cleaning the hands with soap and water or alcohol-based specific products, social distancing and self-isolation. Adherence to the abovementioned regulations might complicate regular multidisciplinary care of DMD patients but on the other hand, it may lead to new medical care telehealth solutions [3].
It is well documented that rehabilitation with glucocorticosteroid treatment slows down the disease progress; it prolongs ambulation, delays respiratory function deterioration and decreases the prevalence of serious deformations caused by contractures or severe scoliosis. Maintaining optimal function and participation will be possible by implementing such interventions as management of contractures (stretching, positioning, standing frames and standers), orthotic interventions, exercises that improve strength and endurance, postural re-education, respiratory management, mobility and upper limb support devices.
International guidelines emphasize the necessity of regular physical, occupational, and speech therapy in DMD management. These interventions should be provided in outpatient and school settings together with extended home preventive stretching program [4]. The pandemic (COVID-19 outbreak) has resulted in discontinuation of many rehabilitation services. In this distinctive situation DMD patients face the risk of deterioration of functional status. Moreover, social isolation associated with quarantine can also be the catalyst for many mental health abnormalities, such as acute stress disorders, irritability, insomnia, emotional distress and mood disorders. Prolonged distancing with high stress level may induce depressive symptoms, panic and anxiety [5].
Purpose
The purpose of this study was 3‑fold. First, we aimed to investigate DMD patients’ situation regarding rehabilitation in the pandemic. The second purpose was to establish an online rehabilitation program and motor assessment for ambulant and non-ambulant DMD patients that can be safely performed in the time of limited access to institutional rehabilitation services. Third, to determine the needs regarding rehabilitation: what kind of rehabilitation service DMD patients prefer: online workshops, videos with exercise instructions or individual online consultations.
Methods
The study included 69 DMD boys with a mean age of 9.41 years (range 1.5–18 years; SD 4.13 years). Inclusion criteria for the study were confirmed DMD diagnosis (genetic testing and/or muscle biopsy, together with biochemical and clinical findings described by pediatricians). From the total of 72 patients 3 were excluded because of missing technical requirements at home.
The study was performed as a part of the Multidisciplinary Care Program for Patients with Duchenne Muscular Dystrophy performed by the Rare Disease Centre (RDC), University Clinical Centre, Medical University of Gdańsk, Poland. The University Clinical Centre is a member of the TREAT NMD Alliance Neuromuscular Network.
Informed consent was obtained from patients and/or their parents prior to enrolment in the study. The study was approved by the ethics committee and assigned the number NKBBN/105/2018.
Study design
The current situation regarding rehabilitation in the time of isolation was assessed by the online Google form questionnaire. The information about the survey was sent via an e‑mail to all DMD patients under the care of the RDC (n = 69). An informed consent was placed on the first page of the study questionnaire. It emphasized the confidentiality of the filled-out information (no identifying information was obtained through the questionnaire) and provided the affiliation of the researchers. Multiple choice, single answer questions were included. The survey consisted of 14 questions. The questions were grouped into three parts. The first part concerned the physical therapy before COVID-19 pandemic and its continuation in the time of social distancing. In the second part caregivers were asked about added burdens (remote working, home responsibilities, helping children with e‑learning) at the time of the pandemic. The third part consisted of questions about expectations from the telerehabilitation project.
Following the online survey, we implemented workshops for ambulant (group 1) and nonambulant (group 2) boys separately (single workshop for each group).
The patient was identified as ambulant (assigned to group 1) when having the ability to walk at least indoors independently, with or without leg braces. Training program was prepared in accordance to DMD care considerations from 2018 [4], as well as the clinical experience of physical and rehabilitation medicine (PRM) specialists and physiotherapists working in the RDC. During the workshops all exercises were presented by a physiotherapist with the use of a physical therapy manikin (the videos were recorded in the time of social distancing, therefore it was not possible to prepare the material with the proper DMD patient). The access to the workshops was possible via communication tool (Skype) for all Rare Disease Centre DMD patients. The workshops lasted 60 min each. Patients/caregivers used their private devices (laptops/tablets/mobile) to get access to the meeting.
Secondly, we published the video online with the same exercise program as it was presented during the workshops. The link to the webcasts was e‑mailed to all DMD patients involved.
The last intervention was to establish motor assessment tool based on the medical data management system (MDMS; P-System, Gdańsk, Poland). Patients and their caregivers were asked once a month to perform 6 tests using the MDMS app and note as described in Table 1.
Table 1.
Home motor assessment tasks
| Task | Testing details | |
|---|---|---|
| 1 | Climbing and descending 4 stairs | Time measurement |
| 2 | Standing up from the chair | Quality of the movement: able to stand up with arms folded/to stand up with help or altered starting position/unable to stand up |
| 3 | Rising up from the floor | Time measurement and quality of the movement: standing up without Gower’s maneuver/presents at least one of the Gower’s components/a need of external support or unable to perform |
| 4 | Lifting head from supine position | Chin moves to chest/head is lifted but through side flexion or with no neck flexion (protraction)/unable to lift head |
| 5 | Bringing plastic cup to mouth | Full/empty/unable to perform |
| 6 | Picking up 6 coins to one hand | Time measurement |
Notes: Tasks 2, 3 and 4 performed according to North Star Ambulatory Assessment (NSAA) manual [25]; Families were also asked to share a photograph of patient’s posture (undressed) while standing/sitting in 3 projections (anterior, posterior and lateral view), as well as a photograph of passive ankle dorsiflexion lying prone. All parents received video with the instructions of how the assessments should be performed
Families were also asked to share a photograph of a patient’s posture (undressed) while standing/sitting in 3 projections (anterior, posterior and lateral view), as well as a photography of passive ankle dorsiflexion lying prone. All caregivers received video with the instructions of how the assessments should be performed. The results of motor and postural assessment are still under investigation and will be published/presented in due time.
Data from this assessment was automatically transferred to the clinical database (MDMS) and was available for all RDC specialists involved in DMD patient care. The MDMS dedicated for rare disease patients was firstly adjusted for DMD patients. The information communications technology (ICT) platform is used as a database of specific DMD patient information that could not be collected via regular hospital information system, and is also used as an telehealth product facilitating the contact, monitoring and help for DMD patients.
Results
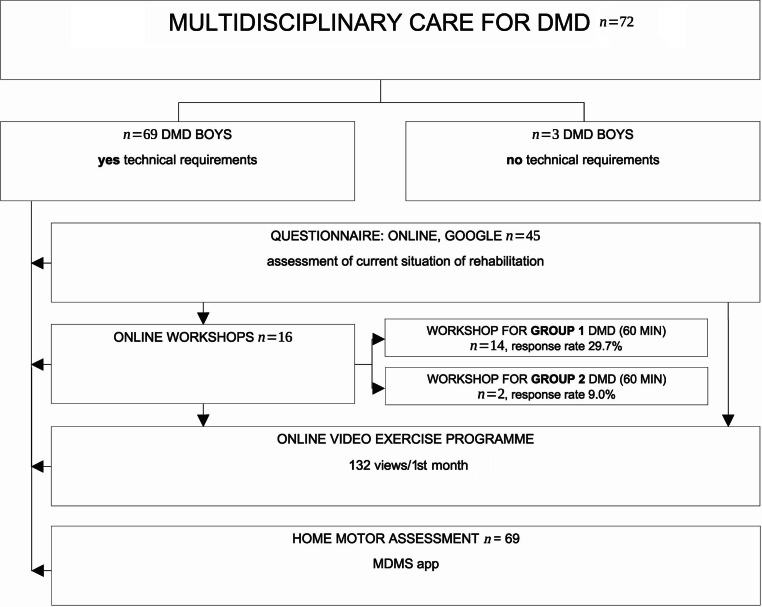
The first group (1 ambulant) consisted of 47 boys (mean age 7.38 years; SD 3.06 years), and the second group (2; nonambulant) 22 boys (mean age 13.74 years; SD 2.44 years). All study interventions, with the numbers of participants included, are presented in Fig. 1.
Fig. 1.
Flowchart showing study interventions with numbers of participants
The online questionnaire was filled in by 45 respondents (response rate 65.2%) and 44 of them received rehabilitation services before the pandemic. Most respondents (n = 43) stopped attending physical therapy sessions due to the recommendations of social distancing; 36 of them (83.7%) declared to continue rehabilitation at home.
Analyzing answers of rehabilitation intervention expectations, 27 (60.0%) respondents declared the need of telerehabilitation. Details of telerehabilitation expectations (with type of exercises) are presented in Fig. 2.
Fig. 2.
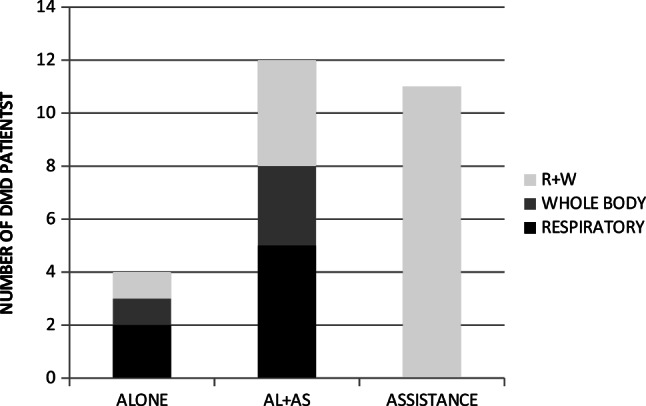
Bar chart showing telerehabilitation expectations. ALONE patient performs all exercises by himself, AL + AS patient performs some of exercises alone and some with caregiver’s assistance, ASSISTANCE patient exercises with caregiver’s assistance, RESPIRATORY respiratory exercises, WHOLE BODY whole body exercises including stretching, R + W respiratory and whole body exercises including stretching
We received 44 valid answers concerning remote working and 45 concerning e‑learning. From all respondents 22 caregivers (50%) did not work at all, 9 respondents (20.5%) declared to be overloaded with remote work. A total of 26 (57.8%) DMD patients felt overloaded with home schooling responsibilities.
Moreover, 23 (51.1%) caregivers confirmed the knowledge of how to perform exercises with their sons and, as far as it was possible, did it at home.
Characteristics of physical therapy with frequency of sessions and additional interventions (beside standard treatment) before the pandemic are illustrated in Table 2. Only standard physical therapy was declared by 10 patients (22.7%), 16 (36.4%) had one additional intervention, and 18 (40.9%) patients declared 2 or more types of additional interventions.
Table 2.
Frequency of physical therapy sessions and additional rehabilitation interventions
| Frequency of physical therapy | n = 44 (%) | Additional rehabilitation interventions | n = 44(%) |
|---|---|---|---|
| Everyday | 1 (2.2) | Hydrotherapy | 26 (57.8) |
| 4–6/week | 12 (27.2) | Massage | 20 (44.4) |
| 2–3/week | 25 (56.8) | Hippotherapy | 8 (17.8) |
| 1/week | 6 (13.6) | Horse riding simulator | 1 (2.2) |
Only 2 boys from the group 2 participated in the workshops (9.0%), whereas from the group 1 14 boys with caregivers (29.7%) participated in the workshops (the amount of logged in participants).
Videos showing exercises consisted of the same components as the workshops. Within 1 month the videos were displayed 132 times.
There were no requests for individual video consultations.
Physical therapy workshops for caregivers and patients from both groups consisted of three parts. The details of workshops for each group are presented in Table 3. The first part concerned respiratory and chest physiotherapy. This part was more detailed for group 2. In the second part the physiotherapist showed stretching and autostretching techniques. In the group 1 more attention was paid to lower extremities, for group 2 to upper extremities. The third part consisted of full body exercises in 3 sequences according to movement ontogenesis (prone, supine and side lying). For group 2 this part specifically included wheelchair exercises and standing assist devices. At the end of both workshops there was a time for questions from caregivers and patients.
Table 3.
Details of physical therapy workshops for group 1 and group 2
| Group 1 | Group 2 | ||
|---|---|---|---|
| Part I | Respiratory and chest physiotherapy | Breathing exercises, breathing with resistance, facilitation of breathing patterns, autogenic airways drainage | Breathing exercises, breathing with resistance, facilitation of breathing patterns, autogenic airways drainage, additional respiratory muscles exercisers, chest vibration, chest mechanoreceptors stimulation, intercostal muscles activation |
| Part II | Stretching and autostretching | Hip flexors and ankle dorsiflexors | Shoulder girdle, elbow flexors, extensors, forearm rotators, as well as wrist and fingers flexors |
| Part III | Full body exercises | Exercises in prone, supine and side lying, quadruped position or kneeling on one knee | Exercises in prone, supine, side lying, exercises while sitting on the wheelchair, ergonomics and positioning of the body in the wheelchair, upper extremities activity, standing frames and standers |
Discussion
The COVID-19 pandemic forced reorganization of the multidisciplinary healthcare system for DMD. For this time telehealth solutions seem to be the most optimal way for providing rehabilitation care.
The World Confederation for Physical Therapy (WCPT) and the International Network of Physiotherapy Regulatory Authorities (INPTRA) in 2020 published a report concerning digital physical therapy. In this document digital practice is defined as “health care services, support, and information provided remotely via digital communication and devices”. This document describes the advantages of telerehabilitation, its limitations and current evidence base as well as implications for the future and recommendations. Authors present the need of creating a culture of digital practice with interprofessional collaboration [6]. Our program is an attempt to respond to this need, particularly by digital assessment collected in an MDMS database and available for all RDC specialists. Some of the limitations reported by WCPT were insurance and funding. Currently in Poland telerehabilitation for DMD patients is not recognized for remuneration and insurance purposes; however, the National Health Fund is working on these regulations. The authors of the document also mention that poor or absent internet connectivity may impact the ability to deploy digital practice options [6]. Because of that limitation three participants were excluded from our study.
In spite of abovementioned barriers there are preliminary promising findings that telerehabilitation in musculoskeletal problems, cardiac, respiratory conditions and in neurological dysfunctions is effective in pain reduction as well as in functional and quality of life improvement [7, 8].
There are several studies reporting the feasibility and reliability of digital physiotherapy assessment and treatment in joint replacement, multiple sclerosis and postsurgical conditions. As benefits for patients, the authors report reduction of the number and length of hospital admissions, no costs of travel and access to the same level of service regardless of the distance [6, 9, 10]. Current systematic reviews and meta-analyses suggest that benefits from telerehabilitation can be gained not only by patients but also by physical therapists who have unique opportunity to educate patients in the home environment and to continuously supervise and monitor patient progress. Increasing accessibility of service may also shorten waiting lists [11, 12]. In spite of these advantages, only a few publications describe home-based rehabilitation programs dedicated to DMD patients [13, 14].
All studies cited above confirm the relevance of telerehabilitation program implementation for DMD patients.
The DMD patients should be particularly cautious in complying with recommendations of self-isolation in the time of the pandemic. The Parent Project Muscular Dystrophy Poland (PPMD) foundation remains in contact with majority of Polish DMD patients. Boys and their families are regularly provided with current status of COVID-19 pandemic and its effect on DMD. The PPMD Poland representatives participate in online webinars conducted by international DMD organizations and afterwards translate and disseminate their suggestions and recommendations of DMD care management throughout the DMD community.
Our results show that almost all patients stopped institutional physical therapy due to the national recommendations of social isolation and the majority of them continued physical therapy at home. Therefore, we have decided to prepare specific support for these patients. To date, there have been only a few published recommendations of digital rehabilitation showing the opportunities and perspectives for patients with disabilities in the COVID-19 pandemic [3, 11, 15, 16]; however, to our knowledge this is the first article to present a specific concept of telerehabilitation for DMD patients in this new challenging reality.
The first step of the telerehabilitation program was to share online workshops performed by physical therapists experienced in the management of DMD patients. We observed a low response rate for online workshops, which could be explained with the overload of daily responsibilities (over 50% of caregivers declared everyday overburden) and/or school tasks (almost 60% of respondents claimed to have too much home schooling activities). Facing the low response rate on the workshops, we decided to publish videos with training instructions for parents/caregivers that could be displayed any time if needed. The higher response rate indicated that this solution was far more acceptable.
All DMD families who were included in the program were offered individual online consultations with DMD specialists (pediatrician, neurologist, cardiologist, endocrinologist, pulmonologist, rehabilitation team, dietician). During the pandemic we noted 10 requests for neurology consultations (corticosteroids prescriptions), 4 pediatric (prescriptions) and one request for orthopedic consultation due to deterioration of foot deformation (clubfoot) and bruising in the ankle area. There were no rehabilitation consultations needed.
To our knowledge this is the first one to describe the remote rehabilitation support for DMD patients in the pandemic.
According to the international recommendations, rehabilitation programs should be individualized according to the patient’s functional status: joint contractures, posture, strength, function, quality of life, and participation in activities of everyday life [4].
The DMD patients in the time of social distancing lack physical activity outdoors, spend hours in a sitting position in front of the computer during home schooling. Due to this distinctive situation, the main goal of rehabilitation, that is entirely shifted onto the patient’s family, is to prevent worsening of patient’s functional status, especially caused by increasing contractures and deterioration of endurance. In the time of restricted participation in recreational activities the emphasis should also be focused on the respiratory function. Impaired respiratory muscles, with ineffective cough reflex and decreased ventilation may lead to pneumonia and respiratory insufficiency. In the previous studies the efficacy of respiratory muscle training in DMD was not fully proven [17]; however, some authors have suggested that lung volume recruitment techniques may help to slow down the rate of decline of pulmonary function [18, 19].
One of the most important elements of home rehabilitation is stretching. Contractures of hip flexors, knee flexors, and ankle plantar flexors are most common in DMD patients. It is known that the loss of range of motion becomes severe when there is deterioration of ambulatory function [20]. A daily preventive home stretching program should begin before the loss of passive range of motion. Study results of contracture management in DMD support the need of an individualized approach of optimal positioning, splinting, standing devices, serial casting, custom seating and power positioning components in mobility devices [21, 22].
The physiology of muscles in neuromuscular diseases differs from normal. The DMD patient’s response to exercise training vary from a healthy individual. It is important to maintain the equilibrium of physical activity as no exercises lead to muscle wasting but too much activity may hasten muscle breakdown. Previous studies suggested that high-intensity, high-volume, eccentric muscle contractions exacerbate the disease pathology. Moreover, lower intensity exercises may preserve and improve functional status of DMD patients [23, 24]. Due to the specific and not fully recognized response to physical activity, it is crucial to adapt the training intensity to the patient’s current condition.
To evaluate functional status related to the disease progression, consistent and reproducible clinical assessments of motor function should be performed regularly by trained practitioners [4]. In the RDC multidisciplinary assessments are systematically conducted. During these consultations, besides motor outcomes, the rehabilitation team reviews the current rehabilitation program and modifies it if needed. In the time of the pandemic all scheduled assessments were cancelled. Therefore, to monitor patients’ condition, we decided to provide tests that could be easily performed by the caregivers.
The COVID-19 pandemic changed everyday management of billions of human beings. It is especially important to maintain multidisciplinary care of patients in the safest way possible.
This innovative project might be applicable for many different patients who cannot obtain regular physical therapy and assessments performed by neuromuscular specialist due to limited mobility and long distances from the medical center. This easily accessible, free of charge and disease-adapted telerehabilitation program may also be a support to maintain the daily routine of home training.
Access to the online videos is available through YouTuBe https://youtu.be/ZJLaJcM-UeY.
Conclusion
In the time of the pandemic the majority of responsibilities regarding physical therapy have been transferred from institutions to caregivers. With the physiotherapist guidance (online communication or video) patients with caregivers’ help can continue home-based rehabilitation of respiratory physiotherapy, stretching, and strengthening exercises. Online videos/instructions/video guidelines are more acceptable by parents/caregivers of DMD patients than live workshops. The home rehabilitation program should be organized with respect to the individual family situation and other responsibilities experienced by patients and their caregivers.
Due to the fact that the epidemic situation in Europe is still unstable, the need of implementing telerehabilitation that is well planned, organized and focused on patients’ and caregivers’ abilities and needs should be the priority of the complex treatment of DMD patients.
Implications for future research
Motor assessment results performed by the caregivers will be presented in due time.
This rehabilitation program is a pilot study for a larger strategy of telehealth services for DMD patients. A further survey is being planned to determine patients’ and caregivers’ opinion about the program relevance, clarity of instructions given in the workshops and video, its strengths and weaknesses, as well as comprehensibility and feasibility in home conditions according to ambulatory status.
Acknowledgments
Funding
Medical Data Management System (P-System, Poland) was partially funded by Digital Poland Operational Programme: e‑Pioneer—supporting talented IT specialists in order to solve identified social or economic problems.
Compliance with ethical guidelines
Conflict of interest
A. Sobierajska-Rek, Ł. Mański, J. Jabłońska-Brudło, K. Śledzińska, A. Ucińska, and J. Wierzba declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mosqueira M, Zeiger U, Förderer M, Brinkmeier H, Fink R. Cardiac and respiratory dysfunction in Duchenne muscular dystrophy and the role of second messengers. Med Res Rev. 2013;33:1174–1213. doi: 10.1002/med.21279. [DOI] [PubMed] [Google Scholar]
- 2.World Muscle Society. Covid-19 and people with neuromuscular disorders: World Muscle Society position and advice. 2020. https://www.worldmusclesociety.org/news/view/150. Accessed 20 May 2020.
- 3.Veerapandiyan A, Wagner KR, Apkon S, et al. The care of patients with Duchenne, Becker, and other muscular dystrophies in the COVID-19 pandemic. Muscle Nerve. 2020;62(1):41–45. doi: 10.1002/mus.26902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17(3):251–267. doi: 10.1016/S1474-4422(18)30024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Usher K, Bhullar N, Jackson D. Life in the pandemic: social isolation and mental health. J Clin Nurs. 2020;29(15-16):2756–2757. doi: 10.1111/jocn.15290. [DOI] [PubMed] [Google Scholar]
- 6.Lee A, Finnin K, Holdsworth L, et al. Report of the WCPT/INPTRA Digital Physical Therapy Practice Task Force. 2020. https://world.physio/news/report-sets-out-future-digital-physical-therapy-practice. Accessed 10 Oct 2020.
- 7.Mani S, Sharma S, Omar B, et al. Validity and reliability of Internet-based physiotherapy assessment for musculoskeletal disorders: a systematic review. J Telemed Telecare. 2017;23(3):379–391. doi: 10.1177/1357633X16642369. [DOI] [PubMed] [Google Scholar]
- 8.Appleby E, Gill ST, Hayes LK, et al. Effectiveness of telerehabilitation in the management of adults with stroke: a systematic review. PLoS One. 2019;14(11):1–18. doi: 10.1371/journal.pone.0225150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson MJ, Crossley KM, Bourke MG, et al. Telerehabilitation feasibility in total joint replacement. Int J Telerehabil. 2017;9(2):31–38. doi: 10.5195/ijt.2017.6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Egmond MA, Engelbert RHH, Klinkenbijl JHG, et al. Physiotherapy with telerehabilitation in patients with complicated postoperative recovery after esophageal cancer surgery: feasibility study. J Med Internet Res. 2020;22(6):1–12. doi: 10.2196/16056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turolla A, Rossettini G, Viceconti A, et al. Musculoskeletal physical therapy during the COVID-19 pandemic: Is telerehabilitation the answer? Phys Ther. 2020;100(8):1260–1264. doi: 10.1093/ptj/pzaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galea MD. Telemedicine in rehabilitation. Phys Med Rehabil Clin N Am. 2019;30(2):473–483. doi: 10.1016/j.pmr.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 13.Jansen M, de Groot IJ, van Alfen N. Physical training in boys with Duchenne muscular dystrophy: the protocol of the No Use is Disuse study. BMC Pediatr. 2010;10:55. doi: 10.1186/1471-2431-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Capelini CM, da Silva TD, Tonks J, et al. Improvements in motor tasks through the use of smartphone technology for individuals with Duchenne muscular dystrophy. Neuropsychiatr Dis Treat. 2017;13:2209–2217. doi: 10.2147/NDT.S125466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bettger JP, Resnik LJ. Telerehabilitation in the age of COVID-19: an opportunity for learning health system research. Phys Ther. 2020 doi: 10.1093/ptj/pzaa151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dantas LO, Barreto RPG, Ferreira CHJ. Digital physical therapy in the COVID-19 pandemic. Braz J Phys Ther. 2020;24(5):381–383. doi: 10.1016/j.bjpt.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva IS, Pedrosa R, Azevedo IG, et al. Respiratory muscle training in children and adults with neuromuscular disease. Cochrane Database Syst Rev. 2019;9:CD011711. doi: 10.1002/14651858.CD011711.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Topin N, Matecki S. Dose-dependent effect of individualized respiratory muscule training in children with Duchenne muscular dystrophy. Neuromuscul Disord. 2002;12(6):576–583. doi: 10.1016/S0960-8966(02)00005-6. [DOI] [PubMed] [Google Scholar]
- 19.Rodrigues MR, Carvalho CR, Santaella DF, et al. Effects of yoga breathing exercises on pulmonary function in patients with Duchenne muscular dystrophy: an exploratory analysis. J Bras Pneumol. 2014;40(2):128–133. doi: 10.1590/S1806-37132014000200005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi YA, Chun SM, Kim Y, et al. Lower extremity joint contracture according to ambulatory status in children with Duchenne muscular dystrophy. BMC Musculoskelet Disord. 2018;19(1):1–6. doi: 10.1186/s12891-018-2212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carroll K, de Valle K, Kornberg A, et al. Evaluation of serial casting for boys with Duchenne muscular dystrophy: a case report. Phys Occup Ther Pediatr. 2018;38(1):88–96. doi: 10.1080/01942638.2017.1280874. [DOI] [PubMed] [Google Scholar]
- 22.Nishizawa H, Matsukiyo A, Shiba N, et al. The effect of wearing night splints for one year on the standing motor function of patients with Duchenne muscular dystrophy. J Phys Ther Sci. 2018;30(4):576–579. doi: 10.1589/jpts.30.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jensen BR, Berthelsen MP, Husu E, et al. Body weight-supported training in Becker and limb girdle 2I muscular dystrophy. Muscle Nerve. 2016;54(2):239–243. doi: 10.1002/mus.25039. [DOI] [PubMed] [Google Scholar]
- 24.Kostek MC. Exercise Is an adjuvant to contemporary dystrophy treatments. Exerc Sport Sci Rev. 2018;46(1):34–41. doi: 10.1249/JES.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 25.Mazzone E, Martinelli D, Berardinelli A, et al. North star ambulatory assessment, 6-minute walk test and timed items in ambulant boys with Duchenne muscular dystrophy. Neuromuscul Disord. 2010;20:712–716. doi: 10.1016/j.nmd.2010.06.014. [DOI] [PubMed] [Google Scholar]