Abstract
Objective
The purpose of this pilot study was to evaluate the feasibility of testing an intervention protocol and measuring the immediate effects of a rib mobilization technique (RMT) and a diaphragm release technique (DRT) on the autonomic nervous system of patients with chronic obstructive pulmonary disease (COPD).
Methods
This was a pilot study of a randomized controlled trial. Fourteen individuals were evaluated. Eligibility criteria were being a sedentary person with a diagnosis of COPD, age between 50 and 72 years, and being clinically stable. Exclusion criteria were heart disease, other respiratory comorbidities, and body mass index above 30kg/m2. Participants first underwent cardiorespiratory evaluation and were then allocated into 2 groups: the RMT + DRT group and the DRT group. Clinical assessments were performed immediately before and after the intervention. Statistical analysis was carried out through a paired-sample Wilcoxon test, and the comparison between groups was performed using the Mann-Whitney test.
Results
All randomized participants completed the assessment and intervention protocol. Sample size was estimated at 24 individuals per group. The DRT group decreased resting heart rate by 5 bpm (P = .03) and increased variance (P = .04) and mean R-R interval (P = .03). The RMT + DRT group decreased mean R-R interval (P = .02).
Conclusion
The design for this study appears to be feasible for evaluating manual-therapy intervention in the nonmusculoskeletal function of patients with COPD. It was possible to determine the sample size for future studies. Preliminary data show that the diaphragm release technique may reduce mean resting heart rate and increase heart-rate variability immediately after the intervention.
Key Indexing Terms: Autonomic Nervous System; Pulmonary Disease, Chronic Obstructive; Heart Rate
Introduction
Chronic obstructive pulmonary disease (COPD) is a systemic disease that adversely affects the cardiovascular autonomic system.1,2 Changes in pulmonary mechanics have the effect of increasing respiratory work, leading to stimulation of local mechanoreceptors and metaboreceptors with sympathetic hyperactivation.3 Increasing sympathetic tonus in the lungs induces an increase in pulmonary vascular resistance of the pathogenic factors in the development of pulmonary hypertension and cor pulmonale.4 Studies have evidenced that individuals with COPD present autonomic dysfunction with an increase in mean resting heart rate (RHR) in addition to lower heart-rate variability (HRV).5,6
Heart-rate variability is a noninvasive measure that describes the oscillation of the intervals between consecutive heartbeats (R-R intervals), which are related to influences of the autonomic nervous system (ANS) on the sinus nodes. The sympathetic branch of the ANS induces an increase in heart rate, with shorter intervals between heartbeats. On the other hand, the parasympathetic branch reduces the heart rate, resulting in larger intervals between heartbeats.7 An autonomic dysfunction with sympathetic-predominance modulation can reduce HRV and increase RHR. A heart rate above 78 bpm can be considered a risk factor for several cardiac dysfunctions.8,9
According to some authors, stretching the respiratory muscles by rib mobilization techniques (RMTs) can influence the sympathetic outflow via the anatomical position of the sympathetic trunk and paravertebral ganglia, involving mobility of the costovertebral and costotransverse joints as well as the rib cage.10,11 Other studies have demonstrated reduced sympathetic excitability as a result of respiratory muscle stretching.3,12 Among the previously studied techniques, the diaphragm release technique (DRT) has shown positive effects on diaphragmatic mobility and inspiratory capacity.13 However, little is known about the effects of such techniques on the autonomic nervous system of patients with COPD who have altered respiratory mechanics.
The purpose of this pilot study was to assess the feasibility of measuring the effect of RMT and DRT on the sympathetic and parasympathetic autonomic nervous system in patients with COPD. The hypothesis was that interventions with manual techniques may modulate the autonomic nervous system in individuals with COPD.
Methods
Design
This was a pilot randomized controlled trial with blind allocation in which participants were unaware of the intervention and the therapist was unaware of what was being evaluated. Participants were advised regarding the evaluation procedures and potential risks and benefits of the research, and agreed to participate by signing a statement of informed consent. This study was conducted in compliance with the ethical standards established by the Declaration of Helsinki, approved by the Ethics and Research Committee of the Health Sciences Center of the Universidade Federal de Pernambuco under protocol number 1 662 521 and registered on ClinicalTrials.gov under protocol number NCT 03022942.
Participants
Participants were recruited from several pulmonology centers or by telephone from waiting lists of physiotherapy reference centers in the metropolitan region of Recife, Pernambuco. The evaluation and intervention were performed at the Laboratory of Cardiopulmonary Physiotherapy of the Physiotherapy Department of the Universidade Federal de Pernambuco.
Eligibility Criteria
Eligible participants were male and female individuals, aged between 50 and 75 years, who presented a diagnosis of COPD (based on spirometric criteria: baseline forced expiratory volume in the first second < 80%, and ratio < 0.7 of forced expiratory volume in the first second to forced vital capacity), led a sedentary lifestyle, and were clinically stable without any acute exacerbation episodes in the previous 6 weeks, in addition to not undertaking any other physiotherapeutic treatment. Exclusion criteria were rheumatic or orthopedic diseases; heart disease or anatomical deformities or abnormalities; rib fracture episode within the past year; other respiratory comorbidities; history of thoracic or abdominal surgery within the past year; osteoporosis; and body mass index above 30 kg/m2. Twelve of the 28 candidates selected were excluded.
Randomization
The randomization was executed in blocks using the website Randomization.com. The sequence of treatment modalities was coded and its allocation was transferred to opaque and numbered black envelopes, which were sent to the therapist in charge of the treatment to be opened right before beginning the session. The participants were assigned into 2 groups: the RMT + DRT group received both techniques, whereas the DRT group received only the diaphragm release technique. Primary outcomes were HRV and mean RHR.
Experimental Protocol
Participants initially gave an anamnesis with a focus on the symptoms, current history of the disease, medications, and comorbidities. Next they underwent an anthropometric evaluation to calculate their body mass index. Lastly, a cardiorespiratory screening was carried out in order to assess peripheral oxygen saturation, heart rate, blood pressure, respiratory rate, spirometry, and manovacuometry.
All evaluated participants were advised to abstain from caffeine and any stimulant or alcoholic beverages, as well as to avoid moderate or excessive effort the day before the tests and keep taking their usual medication. Participants were comfortably accommodated in an air-conditioned room on the day of the intervention, where the temperature ranged from 22°C to 24°C, and relative humidity was maintained between 50% and 60%. Data collection occurred individually from 1:00 pm to 2:00 pm. All evaluation and intervention methods were explained to the participants. Next, an elastic band was settled at the level of the lower third of the sternum, and a heart-rate monitor (Polar V800, Polar Electro Oy, Kempele, Finland) was placed on the wrist. Participants were maintained in dorsal decubitus position and remained breathing spontaneously for 10 minutes. Soon afterward, the elastic band was removed and the intervention was performed in accordance with the participant's group allocation. Immediately after the intervention, the elastic band and heart-rate monitor were replaced and the participant was repositioned in the dorsal position and instructed to continue breathing spontaneously for 10 minutes. Respiratory rate, blood pressure, and peripheral oxygen saturation were checked at the beginning and at the end of HRV capture for monitoring purposes.
Based on the study by Sima et al,14 we considered a change of 3 bpm in mean RHR to be clinically important in individuals with COPD, because this measurement presents good variability and reliability (coefficient of variation, 4.3; intraclass correlation coefficient, 0.93; 95% confidence interval, 80%-98%).
Rib Mobilization Technique and Diaphragm Release Technique (RMT + DRT) Group
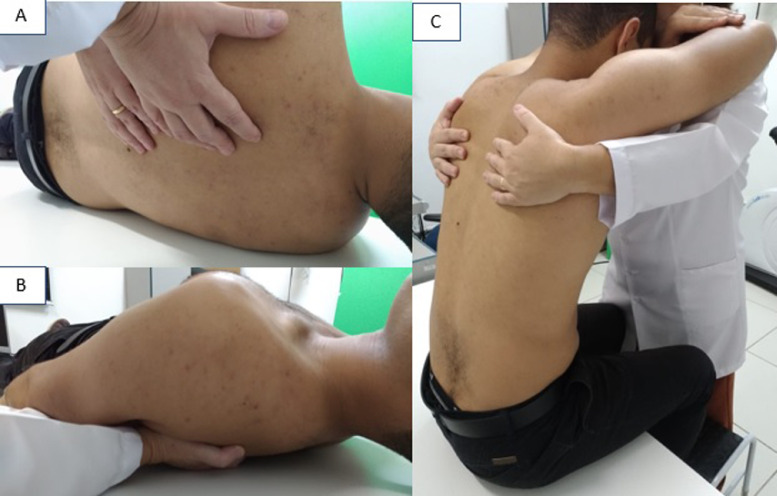
The RMT, adapted from Henderson et al10 and Abdelaal et al,15 was carried out in 2 different participant positions: supine and seated. In the supine position, the therapist was placed next to the participant and positioned the last 4 fingertips of both hands at the rib angles. The therapist mobilized the costal angles in the posteroanterior direction accompanying the participant's normal inspiration (Fig 1). The movement was performed in 2 series of 10 respiratory cycles in each hemithorax, with a 1-minute interval between sets.
Fig 1.
Rib mobilization technique: hand positions (A), technique in supine position (B), technique in seated position (C).
In the seated position, the participants remained seated on the stretcher, keeping the feet on the floor, while the therapist stood in front of him or her. The participant's head (frontal region) was positioned over his or her overlapping arms, which were placed on the therapist's trunk (Fig 1). The therapist then positioned his or her fingertips at the costal angles (bilaterally), moving from the lateral region to the anterior midline throughout the participant's inspiration and returning to the initial position on expiration. The therapist's fingers were then placed 1 level below the rib, repeating this procedure until his or her fifth finger reached the 12th rib. This technique was then carried out toward the second rib, completing a treatment cycle. Another cycle was conducted after a 1-minute rest period.
The DRT was performed according to the protocol described by Rocha et al.13 In this protocol, the participant remains in the supine position so that the therapist is able to maintain manual contact with the bottom edge of the rib cage (Fig 2). During inspiration, the therapist exerts traction after the natural rib-cage movement, then deepens the manual contact and maintains the resistance exerted in the previous phase throughout exhalation. The technique was applied in 2 series of 10 deep respiratory cycles, with a 1-minute interval between the series, under the therapist's verbal command.
Fig 2.
Diaphragm release technique.
Diaphragm Release Technique (DRT) Group
Participants received only the DRT, following the protocol already described.
Heart-Rate Variability Analysis
The RR interval (RRi) sequence length (n = 256 beats) with the greatest stability was selected for comparison before and after intervention. The same sequence was used for time- and frequency-domain analyses. The time-domain variables that were calculated were the mean RRi and the variance.
Heart-rate variability analysis for the frequency domain contributes to the understanding of autonomic control of RRi fluctuations in the heart-rate record and has been recommended for short-term measurements of HRV.16 This analysis has also been called the most accurate tool to obtain an assessment of autonomic function in both experimental and clinical settings.17
All sampling RRi periods were examined, and the most stable segment where no noise (ie, no ectopic beats, arrhythmic events, missing data, or artifacts) was detected was selected, encompassing 256 points. The power spectral density was calculated for each RRi series. The spectral components obtained were low frequency (LF; 0.03-0.15 Hz) and high frequency (HF; 0.15-0.4 Hz). They were expressed in absolute units (ms2) and normalized units (nu). The low frequency occurs owing to the combined action of vagal and sympathetic components on the heart, with sympathetic predominance. On the other hand, HF corresponds to respiratory modulation and stands as an indicator of vagal activity on the heart, expressed in normalized units.18 The LF/HF ratio was calculated to verify the sympathetic-vagal balance of the heart.19
Sample-Size Determination
In the absence of published data to guide the sample size, we performed a pilot study. We used the mean R-R intervals to calculate the sample size, considering a power (1-β) of 80% and an α of 5% through GPower 3.1 software. We used data from the first 7 participants of the RMT + DRT group and 7 participants from the DRT group, yielding 865 ms (SD, 125 ms) and 770 ms (SD, 95 ms), respectively. The sample size was estimated at 24 individuals per group for future clinical trials.
Statistical Analysis
Statistical analysis was carried out through SPSS version 20.0 (SPSS Inc, Chicago, Illinois). The data did not exhibit a normal distribution according to the Shapiro-Wilk test. The Wilcoxon paired test was used to assess potential changes in the continuous variables in relation to the baseline. Data were presented as median and interquartile range (25%-75%), and P < .05 was considered statistically significant. Comparison between groups was performed using the Mann-Whitney test.
Feasibility
The design for this study proved to be feasible. One hundred percent of the randomized participants completed the assessment and intervention protocol to which they were allocated. All data on HRV were analyzed successfully.
Results
Participant Characteristics
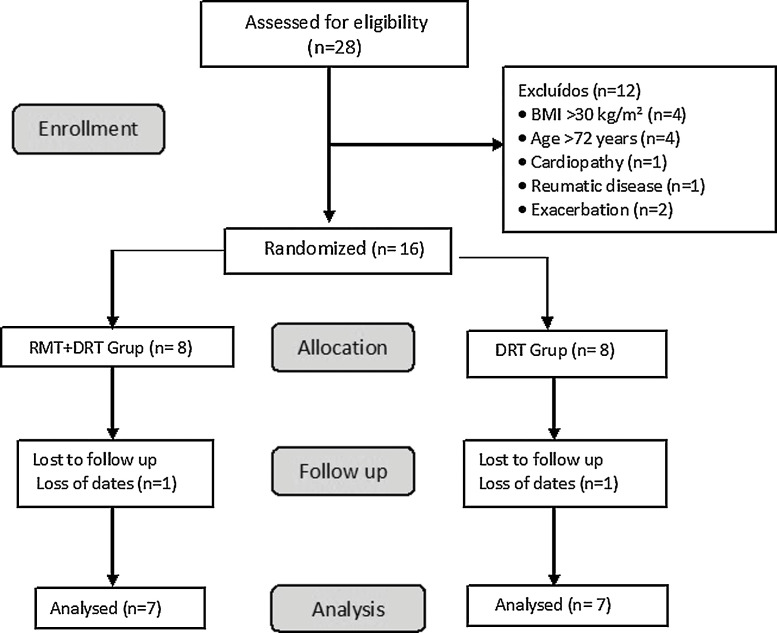
We randomized 16 participants; 2 losses occurred owing to equipment failure during data collection, and thus no data from these participants were captured. The flowchart of the participants is shown in Figure 3. The initial characteristics of the participants are presented in Table 1. Regarding medication use, all participants were under the effects of β2 agonists, and none of the patients used β-blockers.
Fig 3.
Participant flowchart.
Table 1.
Baseline Characteristics of Participants
| Characteristic | DRT Group (n = 7) | RMT + DRT Group (n = 7) | Pa |
|---|---|---|---|
| Sex (male/female) | 4/3 | 4/3 | — |
| Age (y) | 70 (69-72) | 64 (58-70) | .11 |
| BMI (Kg/m2) | 24 (19-27) | 26 (23-27) | .65 |
| FVC (% predicted) | 61 (48-73) | 70 (64-73) | .20 |
| FEV1 (% predicted) | 49 (30-67) | 53 (44-56) | .9 |
| RHR (bpm) | 79 (76-93) | 68 (67-84) | .11 |
| Mean RRi (ms) | 755 (641-789) | 878 (713-896) | .07 |
| Variance (ms2) | 270 (30-600) | 660 (310-1700) | .23 |
| LFnu | 58 (5-64) | 49 (14.5-57) | .75 |
| HFnu | 41.6 (36-100) | 49.5 (43-85.5) | .86 |
| LF/HF | 0.06 (0.03-1.4) | 1 (0.17-1.3) | .25 |
Data are presented as median and interquartile range (25%-75%).
BMI, body mass index; DRT, diaphragm release technique; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HF, high frequency; LF, low frequency; nu, normalized units; RHR, resting heart rate; RRi, RR intervals; RMT, rib mobilization technique.
P value between groups.
Heart Rate
A decrease in RHR of 5 bpm was observed in the DRT group (P = .03), whereas the RMT + DRT group had a 3-bmp reduction (P = .07) immediately after intervention (Table 2). There was no significant difference between groups.
Table 2.
Data Before and After Intervention
| DRT Group (n = 7) |
RMT + DRT Group (n = 7) |
Difference Between Groups | |||||
|---|---|---|---|---|---|---|---|
| Outcome | Pre | Post | P | Pre | Post | P | P |
| RHR (bpm) | 79 (77-93) | 74 (71-89) | .03a | 68 (67-84) | 68 (67-84) | .07 | .06 |
| Mean RRi (ms) | 755 (641-789) | 814 (670-837) | .03 | 878 (713-896) | 882 (715-989) | .02a | .07 |
| Variance (ms2) | 270 (30-600) | 580 (150-2730) | .04a | 650 (310-1700) | 800 (300-5370) | .13 | .52 |
| LF/HF | 0.060 (0.03-1.4) | 0.05 (0-1.2) | .45 | 0.99 (0.17-1.32) | 0.69 (0.05-3.64) | .46 | .08 |
Data are presented as median and interquartile range (25%-75%).
DRT, diaphragm release technique; HF, high frequency; LF, low frequency; RHR, resting heart rate; RRi, RR intervals; RMT, rib mobilization technique.
Statistically significant difference (P < .05).
Heart Rate Variability
There was an increase in the variance (P = .04) and mean RRi (P = .03) in the DRT group immediately after the intervention. The RMT + DRT group demonstrated an increase in mean RRi (P = .02). No discrepancies were found between groups in LFnu, HFnu, or the sympathetic-vagal relationship (Table 2).
Discussion
This study evaluated the feasibility of measuring an approach to COPD through manual therapy and evaluating the immediate effects of the rib mobilization technique and the diaphragm release technique on heart-rate variability and mean resting heart rate. In addition, as a pilot study it determined the appropriate sample size for future clinical research. We hypothesized that the mobilization of costotransverse joints and the diaphragm could modulate the autonomic nervous system. Preliminary results from the study suggest that the diaphragm release technique may promote an immediate reduction in mean resting heart rate resulting in an increase in HRV. The association of the diaphragm release technique with the rib mobilization technique also may reduce the mean resting heart rate in patients with COPD.
The rib mobilization technique is used in clinical practice to increase the mobility of the rib cage and to modulate the ANS. Some authors10,20,21 affirm that the rib mobilization technique affects ANS activity through the activation of the proximal ganglia of the thoracic sympathetic chain in the costotransverse joint; however, there is no consistent evidence in the literature regarding its effects in patients with COPD. Likewise, there are no studies on the influence of the diaphragm release technique on the ANS.
A recent systematic review affirms that the impairment of HRV in the time domain, baroreceptor sensitivity, and muscular sympathetic nerve activity demonstrate a strong level of evidence for being factors that influence autonomic function in patients with COPD. The decrease in HRV indicates a higher risk of mortality from cardiac events than in healthy individuals.22
In individuals with COPD, sympathetic activation through the stimulation of metaboreceptors and local mechanoreceptors can reduce HRV.3 Chronic pulmonary hyperinflation in COPD results in an increase in respiratory work, with a consequent increase in the tension of the musculoskeletal system of the thoracoabdominal region. The products of ischemic metabolism generated during muscle contraction stimulate local receptors and may lead to increased heart rate, blood pressure, and sympathetic activity.23 Also, sympathetic hyperactivity in COPD may be associated with skeletal-muscle dysfunction or even respiratory-pump dysfunction, as increased respiratory work leads to sympathetic activation through stimulation of local metaboreceptors.4 Our results show that manual techniques in the rib cage and the diaphragm can have immediate effects on the autonomic nervous system of patients with COPD, demonstrating the relationship between the musculoskeletal and autonomic nervous systems.
The relationship between the degree of disease severity and autonomic dysfunction is still not well defined in the literature. Camillo et al report that autonomic function in individuals with COPD is related not necessarily to the severity of the disease but to the level of physical activity in daily life, muscle dysfunction, and quality of life.5 Van Gestel et al also emphasize the role of autonomic cardiac dysfunction in impaired health-related quality of life in individuals with COPD.24 However, according to Janssens et al, mean RHR increases with the severity of lung dysfunction in COPD and helps better mortality prognosis, so heart rate may be a target for intervention in COPD.25
In the preliminary results, the DRT group showed a 5-bpm decrease in mean RHR immediately after application of the technique, and the RMT + DRT group presented a decrease of 3 bpm. In a recent study, a change of 3 bpm in individuals with COPD was considered clinically important, with good measurement variability and reliability (coefficient of variation, 4.3; intraclass correlation coefficient, 0.93; 95% confidence interval, 80%-98%).14 In general, a lower RHR implies higher HRV and can be interpreted as representing a well-balanced autonomic nervous system; as the heart rate increases, there is less time between heartbeats for variability to occur, and HRV decreases.26 Therefore, individuals who presented a decrease of 5 bpm in RHR may be benefiting from increased HRV. According to Cole et al, a reduction in HRV reflects an imbalanced autonomic nervous system that can reduce regulation capacity and adaptive response to physiological challenges, such as exercise.27
In our pilot study, HRV increased immediately after intervention in the DRT group. The RMT + DRT group did not present a change in HRV. Our hypothesis is that stretching the muscle fibers of the diaphragm through the diaphragm release technique favors reducing sympathetic excitability and parasympathetic activation in these patients. Additionally, increased tissue viscoelasticity can potentiate contractile-muscle capacity with less effort and reduce stress on musculoskeletal receptors.14 It is also possible that some mechanoreceptors trigger a predominantly parasympathetic response when stimulated by myofascial maneuvers.28 According to Farinatti et al, 10 minutes of stretching exercises acutely affects the sympathetic-vagal balance in individuals with low flexibility, especially by increasing vagal poststretching modulation.29
In a systematic review, Kingston et al claim that there is convincing evidence that the sympathetic response to spine mobilizations is excitatory in nature at the mobilized spine level.11 According to Borges et al, the influence of manipulation in the spine on the autonomic nervous system depends on the site and type of stimulation: a greater parasympathetic response is found from stimulation performed in the cervical and lumbar regions, while a greater sympathetic response is found from stimulation performed in the thoracic region.30 Thus, rib mobilization in the RMT + DRT group in our study may have promoted sympathetic arousal.
Changes in LFnu, HFnu, and the LF/HF ratio were not statistically significant. The short intervention time was probably not sufficient to generate a change in these outcomes.
Conclusion
The protocol performed to assess the immediate effects on mean resting heart rate and heart-rate variability was shown in this study to be feasible. With the data obtained, it was possible to calculate the sample size for future studies. The results of the present pilot study suggest that manual-therapy intervention may alter nonmusculoskeletal function in individuals with COPD. Preliminary data show that the diaphragm release technique may reduce the mean resting heart rate, resulting in an increase in HRV immediately after the intervention.
Funding Sources and Conflicts of Interest
This study received financial support from the Foundation for the Support of Science and Technology of the State of Pernambuco (FACEPE): APQ 0154-4.08/15, IBPG1599-4.08/15, and CAPES/PROCAD 88881.068409/2014-01. No conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): H.M.R., H.C.M.Z., A.D.A.
Design (planned the methods to generate the results): H.M.R., H.C.M.Z., R.V., V.R.N.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): H.M.R., H.C.M.Z., V.R.N., A.D.A.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): H.M.R., R.V.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): H.M.R., H.C.M.Z., V.R.N.
Literature search (performed the literature search): H.M.R., H.C.M.Z., R.V.
Writing (responsible for writing a substantive part of the manuscript): H.M.R., H.C.M.Z.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): H.M.R., H.C.M.Z., R.V., V.R.N., A.D.A.
Practical Applications.
-
•
This study evaluated whether manual techniques could possibly be used for nonmusculoskeletal outcomes.
-
•
We assessed the feasibility of measuring the effects of a diaphragm release technique on mean resting heart rate and heart-rate variability immediately after intervention in individuals with chronic obstructive pulmonary disease.
-
•
This study seems to be feasible for performance on a larger scale.
Alt-text: Unlabelled box
References
- 1.van Gestel A, Steier J. Autonomic dysfunction in patients with chronic obstructive pulmonary disease (COPD) J Thorac Dis. 2010;2(2):215–222. doi: 10.3978/j.issn.2072-1439.2010.02.04.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carvalho TD, Pastre MC, Rossi CR, Abreu L, Valenti V, Marques VL. Geometric index of heart rate variability in chronic obstructive pulmonary disease. Rev Port Pneumol (2006) 2011;17(6):260–265. doi: 10.1016/j.rppneu.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Paulin E, Brunetto A., Carvalho C. Effects of a physical exercises program designed to increase thoracic mobility in patients with chronic obstructive pulmonary disease. J Pneumol. 2003;29(5):287–295. [Google Scholar]
- 4.Heindl S, Lehnert M, Crieé C-P, Hasenfuss G, Andreas S. Marked sympathetic activation in patients with chronic respiratory failure. Am J Respir Crit Care Med. 2001;164(4):597–601. doi: 10.1164/ajrccm.164.4.2007085. [DOI] [PubMed] [Google Scholar]
- 5.Camillo C, Pitta F, Possani H, Barbosa M, Marques D, Cavalheri V. Heart rate variability and disease characteristics in patients with COPD. Lung. 2008;186(6):393–401. doi: 10.1007/s00408-008-9105-7. [DOI] [PubMed] [Google Scholar]
- 6.Volterrani M, Scalvini S, Mazzuero G. Decreased heart rate variability in patients with chronic obstructive pulmonary disease. Chest. 1994;106(5):1432–1437. doi: 10.1378/chest.106.5.1432. [DOI] [PubMed] [Google Scholar]
- 7.Pumprla J, Howorka K, Groves D, Chester M, Nolan J. Functional assessment of heart rate variability: physiological basis and practical applications. Int J Cardiol. 2002;84(1):1–14. doi: 10.1016/s0167-5273(02)00057-8. [DOI] [PubMed] [Google Scholar]
- 8.Fagundes JE, Castro I. Predictive value of resting heart rate for cardiovascular and all-cause mortality. Arq Bras Cardiol. 2010;95(6):713–719. doi: 10.1590/s0066-782x2010005000149. [DOI] [PubMed] [Google Scholar]
- 9.Palatini P. Elevated heart rate: a “new” cardiovascular risk factor? Prog Cardiovasc Dis. 2009;52(1):1–5. doi: 10.1016/j.pcad.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Henderson AT, Fisher JF, Blair J, Shea C, Li TS, Bridges KG. Effects of rib raising on the autonomic nervous system: a pilot study using noninvasive biomarkers. J Am Osteopath Assoc. 2010;110(6):324–330. [PubMed] [Google Scholar]
- 11.Kingston L, Claydon L, Tumilty S. The effects of spinal mobilizations on the sympathetic nervous system: a systematic review. Man Ther. 2014;19(4):281–287. doi: 10.1016/j.math.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 12.Wada JT, Borges-Santos E, Porras DC. Effects of aerobic training combined with respiratory muscle stretching on the functional exercise capacity and thoracoabdominal kinematics in patients with COPD: a randomized and controlled trial. Int J Chron Obstruct Pulmon Dis. 2016;11(1):2691–2700. doi: 10.2147/COPD.S114548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rocha T, Souza H, Brandão D. The manual diaphragm release technique improves diaphragmatic mobility, inspiratory capacity and exercise capacity in people with chronic obstructive pulmonary disease: a randomised trial. J Physiother. 2015;61(4):182–189. doi: 10.1016/j.jphys.2015.08.009. [DOI] [PubMed] [Google Scholar]
- 14.Sima C, Inskipa JA, Sheel AW, van Eeden SF, Reid WD, Camp PG. The reliability of short-term measurement of heart rate variability during spontaneous breathing in people with chronic obstructive pulmonary disease. Rev Port Pneumol (2006) 2017;23(6):338–342. doi: 10.1016/j.rppnen.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Abdelaal A, Ali M, Hegazy M. Effect of diaphragmatic and costal manipulation on pulmonary function and functional capacity in chronic obstructive pulmonary disease patients: randomized controlled study. Int J Med Res Health Sci. 2015;4(4):841–847. [Google Scholar]
- 16.Malik M, Bigger JT, Camm AJ. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Eur Heart J. 1996;17(3):354–381. [PubMed] [Google Scholar]
- 17.Acharya N, Joseph K, Kannathal N, Lim C, Suri J. Heart rate variability: a review. Med Biol Eng Comput. 2006;44(12):1031–1051. doi: 10.1007/s11517-006-0119-0. [DOI] [PubMed] [Google Scholar]
- 18.Montano N, Porta A, Cogliati C. Heart rate variability explored in the frequency domain: a tool to investigate the link between heart and behavior. Neurosci Biobehav Rev. 2009;33(12):71–80. doi: 10.1016/j.neubiorev.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Porta A, Guzzetti S, Montano N. Entropy, entropy rate, and pattern classification as tools to typify complexity in short heart period variability series. IEEE Trans Biomed Eng. 2001;48(11):1282–1291. doi: 10.1109/10.959324. [DOI] [PubMed] [Google Scholar]
- 20.Noll DR, Degenhardt BF, Johnson JC, Burt SA. Immediate effects of osteopathic manipulative treatment in elderly patients with chronic obstructive pulmonary disease. J Am Osteopath Assoc. 2008;108(5):251–259. [PubMed] [Google Scholar]
- 21.Wallace E, McPartland J, Jones J, Kuchera W, Buser B. Lymphatic system: lymphatic manipulative techniques. In: Ward RC, editor. Foundations for Osteopathic Medicine. 2nd ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2003. pp. 1064–1065. [Google Scholar]
- 22.Mohammed J, Meeus M, Derom E, Da Silva H, Calders P. Evidence for autonomic function and its influencing factors in subjects with COPD: a systematic review. Respir Care. 2015;60(12):1841–1851. doi: 10.4187/respcare.04174. [DOI] [PubMed] [Google Scholar]
- 23.Mark AL, Victor RG, Nerhed C, Wallin BG. Microneurographic studies of the mechanisms of sympathetic nerve responses to static exercise in humans. Circ Res. 1985;57(12):461–469. doi: 10.1161/01.res.57.3.461. [DOI] [PubMed] [Google Scholar]
- 24.Van Gestel A, Kohler M, Steier J, Teschler S, Russi EW, Teschler H. Cardiac autonomic dysfunction and health-related quality of life in patients with chronic obstructive pulmonary disease. Respirology. 2011;16(6):939–946. doi: 10.1111/j.1440-1843.2011.01992.x. [DOI] [PubMed] [Google Scholar]
- 25.Janssens L, Brumagne S, McConnell AK. Proprioceptive changes impair balance control in individuals with chronic obstructive pulmonary disease. PLoS One. 2013;8(3):e57949. doi: 10.1371/journal.pone.0057949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mccraty R, Shaffer F. Heart rate variability: new perspectives on physiological mechanisms, assessment of self-regulatory capacity, and health risk. Glob Adv Health Med. 2015;4(1):46–61. doi: 10.7453/gahmj.2014.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med. 1999;341(18):1351–1357. doi: 10.1056/NEJM199910283411804. [DOI] [PubMed] [Google Scholar]
- 28.Arroyo-Morales M, Olea N, Martinez M, Moreno-Lorenzo C, Daz-Rodrguez L, Hidalgo-Lozano A. Effects of myofascial release after high-intensity exercise: a randomized clinical trial. J Manipulative Physiol Ther. 2008;31(3):217–223. doi: 10.1016/j.jmpt.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Farinatti PTV, Brandão C, Soares PPS, Duarte AFA. Acute effects of stretching exercise on the heart rate variability in subjects with low flexibility levels. J Strength Cond Res. 2011;25(6):1579–1585. doi: 10.1519/JSC.0b013e3181e06ce1. [DOI] [PubMed] [Google Scholar]
- 30.Borges BLA, Bortolazzo GL, Neto HP. Effects of spinal manipulation and myofascial techniques on heart rate variability: a systematic review. J Bodyw Mov Ther. 2018;22(1):203–208. doi: 10.1016/j.jbmt.2017.09.025. [DOI] [PubMed] [Google Scholar]