Following the nationwide lockdown, private psychiatry outpatient departments (OPD) have almost completely shut. While the OPD services of government hospitals have continued, the attendance has been thin.1 Along with this—recent dwindling mental health services because of the lockdown, and also for protecting the available health care workers from getting infected, remote assessment and management of people with mental illness have become the best alternative. Telepsychiatry and telecounselling services in parts of India have been proved to be cost-effective and economical,2 and the service users have rated them as satisfactory.3 Sikkim, a hilly state, which frequently suffers landslides restricting the transportation of the mental health care service users, may be particularly helped with telepsychiatry. The timely release of the Telemedicine Practice Guidelines4 and the Telepsychiatry Operational Guidelines—2020 5 has motivated care providers in India to deliver much needed medical evaluation, diagnosis, and triage remotely during the current COVID crisis.
Telepsychiatry Practice in Sikkim Manipal Institute of Medical Sciences
Sikkim is a state in north-eastern India sharing borders with China and Bhutan. This least populous and second smallest state in India has 14 consultant psychiatrists and 5 psychiatry postgraduate trainees. As per the 2011 Indian census, Sikkim has a population of around 610,577.6 Based on the reliable population data, there are 2.3 psychiatrists per 100,000 in Sikkim, which is well above the national average of 0.75 per 100,000.7
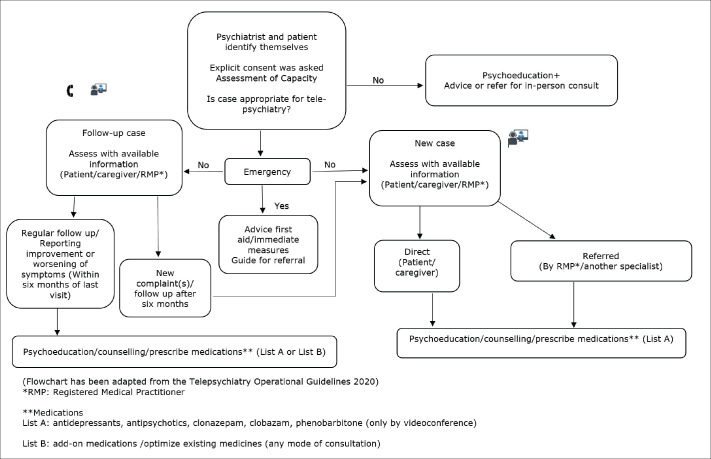
Telepsychiatry services from the Department of Psychiatry in our hospital, Sikkim Manipal Institute of Medical Sciences (SMIMS), began on March 25, 2020, at the commencement of the nationwide lockdown. Patients who have had their prior consultations with the psychiatrists at the hospital before the lockdown constitute the majority of those who sought telepsychiatry services. All five psychiatrists of the hospital were involved in the handling of telepsychiatry consultations for both new as well as follow-up cases. These patients have been calling or messaging their psychiatrists on their mobile numbers and also connecting with them on social media platforms. The new cases connected to the psychiatrist either by calling the hospital or through a person who has already visited or is known to these psychiatrists. All follow-up cases contacted the psychiatrist directly as they already had the contact numbers or obtained it from the hospital. The telepsychiatry consultations were done with the help of audio and video modes. Video mode was utilized for all new cases and, where List A medications like antipsychotic, antidepressant, etc.,5 needed to be prescribed for the first time (Figure 1). Most of the patients who sought telepsychiatry support from the consultant psychiatrists at SMIMS were residents of the state.
Figure 1. Flowchart Showing Steps of Telepsychiatry Consultations.
As of May 26, 2020, there have been a total of 78 teleconsultations (Table 1). Among these, 73 are residents of the state and 5 are from 2 other states. In terms of distance, the locations of the 73 patients residing within the state ranged from as near as 5 km from the hospital and to 130 km at the farthest. Duration of the calls varied from 15 minutes to 45 minutes, depending on whether it is a new case or a follow-up consultation. The language of communication between the psychiatrists and the patients were English, Hindi, or Nepali. Both audio and video calls were initiated by the patients or their caregivers, except for two cases where the calls were initiated by registered medical practitioners (from the patient’s end). The communication was synchronous. In the setting where registered medical practitioners referred cases, initially the audio mode was used and then the video mode. The prescriptions were sent as images, as personal messages through WhatsApp or Facebook Messenger, and the prescription format was followed as per the recommended guidelines. List A and List B medications as per the recommended guidelines were prescribed; however, no patient was prescribed injectables through teleconsultation. The hardcopies of the prescription are being kept in the department for record.
Table 1. Characteristics of Telepsychiatry Service Users.
| Caller’s Characteristics | Numbers |
|
|
|
|
|
|
We had six acute cases. For all of these, we guided the caregiver for a referral to a nearby hospital or to come to our institute. We received no cases of child and adolescent psychiatry for telepsychiatry consultation.
Challenges We Faced
Though an informal consent was taken before starting any consultation, it was difficult to get a formal written consent as suggested in the telepsychiatry guideline (Appendix 2, last part).5 The service users needed to be explained about the regulations of telepsychiatry. However, they were not very keen to listen about it during the initial stage of consultation, and, also, did not have the logistics to take a printout and send an image of the signed consent form. In some follow-up cases who were higher doses of the medications, refilling the doses without actual physical examination was a tricky affair. A routine OPD consultation gives the chance to build a relation, both for the attending psychiatrist and the patients as well as their caregivers; the virtual consultation may not have the same effect, especially for the new cases where the patients/caregivers are in contact with a stranger on a small screen and may not like disclosing everything about their life.
Future Considerations
For telehealth to be effective during the current COVID-19 pandemic and similar future events, it needs to be appropriately integrated into health service and treated as a “business as usual” modality, unless we want to experience the same failure as that of more developed countries who tried implementing it.8 To make telehealth a mainstream component of the health system, the authors propose the following measures:
Adequate education and training of all health professionals in telemedicine, even consider including it in the curriculum of the trainees.
Initiate telehealth accreditation for health professionals.
Adequate funding to cover the cost of delivering telehealth.
Restructure clinical models of patient care.
Support to all stakeholders with an effective communication and change management strategy
Ascertain systems to manage telehealth services on a regular basis.
Conclusion
The COVID-19 crisis and global pandemic may be the defining moment for digital mental health. One of the definite solutions to continue delivering mental health support within this pandemic from a safe distance is telepsychiatry. According to our preliminary experience, telepsychiatry services are realistically possible and apt to help patients and caregivers not only now during the pandemic but also in the future. This would help to decrease the inflow of regular OPD consultations and hence minimize exposure to novel corona virus now and save transportation and other logistic costs for the patients and their caregivers in the future too.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Mukherjee A, Bandopadhyay G, and Chatterjee SS.. COVID-19 pandemic: mental health and beyond—the Indian perspective [published online May 21, 2020]. Ir J Psychol Med; DOI:10.1017/ipm.2020.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moirangthem S, Rao S, Kumar CN, et al. Telepsychiatry as an economically better model for reaching the unreached: a retrospective report from South India. Indian J Psychol Med; 2017. May–Jun; 39(3): 271–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hazarika M, Das B, Das S, et al. Profile of distress callers and service utilisation of tele-counselling among the population of Assam, India: an exploratory study during COVID-19 [published online July 17, 2020]. Open J Psychiatry Allied Sci. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Board of Governors. In supersession of the Medical Council of India. Telemedicine practice guidelines. 2020. https://www.mohfw.gov.in/pdf/Telemedicine.pdf. Cited July 21, 2020.
- 5.Math SB, Manjunatha N, Kumar CN, et al. Telepsychiatry operational guidelines—2020. Bengaluru: NIMHANS, 2020. [Google Scholar]
- 6.Directorate of Census Operation Sikkim. Census of India 2011. Sikkim: Ministry of Home Affairs, 2011. https://censusindia.gov.in/2011census/dchb/1100_PART_B_DCHB_SIKKIM.pdf. Cited July 6, 2020. [Google Scholar]
- 7.Garg K, Kumar C N, and Chandra PS.. Number of psychiatrists in India: baby steps forward, but a long way to go. Indian J Psychiatry; 2019; 61: 104–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare; 2020. June; 26(5): 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]