Abstract
Background:
The coronavirus disease (COVID-19) pandemic, associated with the economic consequences of non-pharmaceutical interventions such as lockdown, has led to mental health consequences among people worldwide. Protecting the mental well-being of populations is an imperative component of fighting the COVID-19 pandemic. This scoping review attempts to present an overview of the existing tools to measure COVID-19-related mental health problems.
Methods:
Literature search was conducted in the PubMed electronic database using developed key search terms. Reference lists of the identified eligible articles were reviewed to locate relevant articles missed from the electronic database search. Fifteen scales measuring COVID-19-associated mental health problems, validated among diverse populations across the world, were included in this review.
Results:
The majority of these scales were validated among middle-aged adults in Turkey. Only a few validated scales encompass the negative socioeconomic consequences of COVID-19. None of the available scales focused on the aspects of suicidal ideation or behavioral responses/coping strategies, neither were they inclusive of participants from diverse age, geographic, and COVID-19 exposure groups.
Conclusion:
This scoping review highlights the need for future research to develop and validate comprehensive psychometric tools to assess COVID-19-associated mental health problems. Also, in view of the vulnerable nature of healthcare professionals for developing mental health concerns in the course of providing services for COVID-19-affected individuals, future psychometric research needs to concentrate on the development of measures specific for these professionals.
Keywords: Clinical psychology, epidemiology, psychotherapy, qualitative
Key Messages:
Various validated tools are available to measure the mental health implications of COVID-19. The available psychometric instruments must be used in an informed manner in different settings to comprehend the psychological burden posed by COVID-19 on populations. Identification of COVID-19-associated mental health problems with an informed use of the available psychometric tools facilitates a thorough preparation of healthcare systems in dealing with the psychological aftermath of COVID-19.
Coronavirus disease (COVID-19) emerged as a devastating pandemic of unprecedented magnitude pushing the world into a looming health crisis. While the physical implications of this infectious disease are apparent, it is undeniable that the condition also holds the potential for mediating negative socioeconomic and psychological implications.1 Across the globe, it has substantially been established by now that the mental health problems are on the rise through the COVID-19 pandemic.2–7 Hossain et al. reviewed the mental health outcomes of nonpharmaceutical preventive interventions such as quarantine and reported depression, anxiety, insomnia, and mood disorders among isolated individuals.8 A few of the many stressors leading to mental health concerns among the general population in the COVID-19 era are fear of infection, financial depletion, deficient supplies, and stigmatization.9 Suicidal tendencies among COVID-19-affected individuals are also reported.10 Another important concern is the impact of COVID-19 on the psychological well-being of healthcare workers (HCW). Around the world, the health systems are under tremendous pressure catering to the needs of an ever-increasing number of COVID-19 cases. The situation demands HCW to work for longer periods in settings different from their regular work while staying away from their families and dealing with an infectious disease with a lot of uncertainties around. This context reflects the possibility of mental health concerns such as fear of infection, the guilt of providing suboptimal care, burnout, insomnia, anxiety, and depression among HCW.11–15 It has to be acknowledged here that mental health is a broad construct encompassing emotional, psychological, and social dimensions, making it an elusive construct to measure. Though diagnostic interviews were identified to be the gold standard and definitive diagnostic ways for appraisal of mental health status, the amount of time they consume precludes their application in conventional health settings, especially when the assessment has to be made at a mass level. It is for this reason that the reliance on screening tools for measuring mental health status has increased over the years.16 During the COVID-19 pandemic, new scales have been validated to assess the COVID-19-related mental health problems. A preliminary scan of the existing COVID-19 psychometric scales revealed that the focus predominantly had been placed on COVID-19-related fear and anxiety. However, drawing on the suggestions made by experts that the psychological implications of COVID-19 are manifold, tools that comprehensively capture COVID-19-related mental health concerns are warranted. The present scoping review, therefore, was conducted to address any existing knowledge gap and in order to provide a condensation of the available scales assessing COVID-19-related mental health problems.
Materials and Methods
This scoping review was conducted to examine the available psychometric tools to measure COVID-19-related mental health problems. While the primary purpose of a scoping review is to provide an overview of the available evidence by summarizing the available literature pertaining to a concept, there exists no concrete consensus on the indications for the conduct of a scoping review.17 Besides comprehending the fundamental characteristics of a phenomenon, identification and analysis of knowledge gaps, which forms the basis for this study, is purported to be one of the key indications of scoping reviews.18 The framework proposed by Arksey and O’Malley for scoping reviews was adopted in this study.19
Identification of the research question: Since the scoping review attempts to comprehensively document the existing literature, a broad question that facilitates the inclusion of different constructs relating to mental health are warranted. The research question for this review was identified as: In spite of a preliminary scan of the results showing predominant emphasis on the constructs of anxiety and fear, “What are the existing scales to measure COVID-19-related mental health problems?”.
Formulating the search strategy to identify relevant studies: A literature search was conducted in the PubMed electronic database after a series of consensus building among the investigators for identification of key search terms. The following key terms were included in the search for eligible studies: Coronavirus*, COVID-19, COVID, “COVID 19”, “SARS CoV-2”, “SARS CoV 2” for coronavirus disease; “mental health,” anxiety, fear, phobia, stress for mental health problems; and scale, tool, instrument, questionnaire for scale. The final search string was (Coronavirus* OR COVID-19 OR COVID OR “COVID 19” OR “SARS CoV-2” OR “SARS CoV 2”) AND (“mental health” OR anxiety OR fear OR depression OR stress OR phobia) AND (scale OR instrument OR questionnaire OR tool). Those studies measuring the constructs related to mental health specific to COVID-19, published in the English language in peer-reviewed journals in the year 2020, after the emergence of the COVID-19 pandemic, were included in the review. The search was inclusive of all the relevant publications available till June 10, 2020.
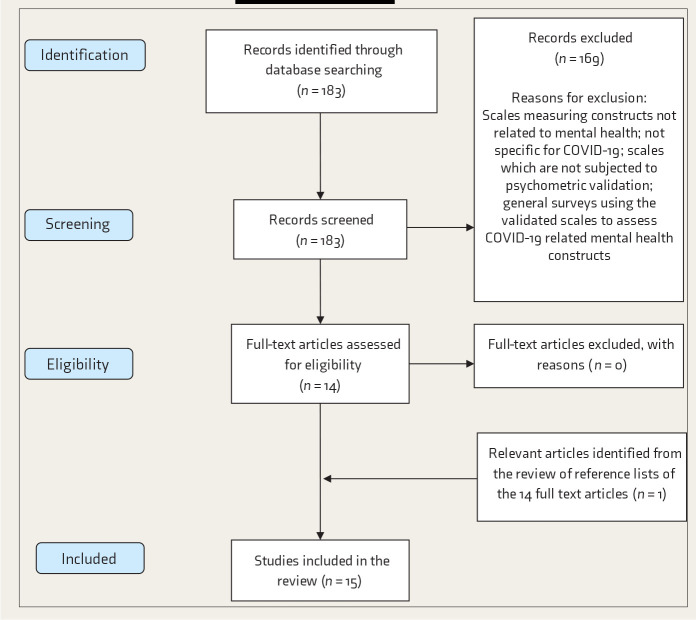
Selection of relevant studies: Figure 1 shows the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for the scoping review. The search strategy yielded 183 results. The EndNote bibliographic software package was used to import and manage all references. The title, abstracts, and key words of all the articles were independently reviewed by three investigators to check the relevance of these articles based on the selection criteria of the review. Scales measuring constructs not related to mental health and those that are not specific for COVID-19, scales which have not been subjected to psychometric validation, and general surveys using the validated scales to assess COVID-19-related mental health constructs were excluded from the review. The full texts of the 14 articles that were agreed upon by all the reviewers to be satisfying the study criteria after the initial review were reviewed. References from all these 14 articles were also reviewed to check if any relevant publications were missed in the electronic database search. The final review included 15 articles.20–34
Study charting and summarizing: All the 15 articles included in the final review were comprehensively charted and summarized. Summarization included details on the authors, journal, country, number of items, dimensionality, time of conduct of the study, and other psychometric properties of the scale. While summarizing the scales, the constructs and dimensions were identified based on the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition, DSM-5).35
Figure 1. PRISMA Flowchart of the Scoping Review.
Results
An overview of the existing scales measuring COVID-19-related mental health problems have been provided in Table S1. The majority of these scales were validated among middle-aged adults (range for mean age across scales: 26.5–49.8 years). There was a great variation in the sample size between the studies, ranging from 249 for the “Italian version of Fear of COVID-19 Scale” to 8550 for the “Bangla version of Fear of COVID-19 Scale.” Most of the scales, 4 of the 15 included in the review, were validated in Turkey, followed by 3 in the United States and 2 in Italy. The Fear of COVID-19 Scale (FCV-19S) was validated and available in seven languages (Farsi, Hebrew, Bangla, Turkish, Russian, Italian, Arabic), while the Coronavirus Anxiety Scale was available in English and Turkish. The majority of the studies included in this review (40%) were published in the International Journal of Mental Health and Addiction, followed by the Death Studies journal (20%). It is evident from Table S1 that a majority of scales were validated before the peak incidence was reached in the corresponding nations. “COVID Stress Scales” (CSS) was observed to be the lengthiest scale, with 36 items, and “Obsession with COVID-19 Scale” was the briefest scale, with only 4 items. Cronbach’s alpha was identified as the most common measure for internal consistency reliability, ranging from 0.73 to 0.93 among the 15 scales considered. Factor structure was presented for all the scales except the “Italian version of COVID-19 Peritraumatic Distress Scale.” A total of 10 out of the 15 scales were unidimensional with a single-factor solution. The majority of the scales were validated among the general population. Hospital Anxiety and Depression Scale (HADS), Perceived Vulnerability to Disease Scale (PVDS), Patient Health Questionnaire (PHQ), Brief Resilience Scale Turkish (BRS-T), Severity Measure for Specific Phobia-Adult (SMSP-A), self-rated mental health, Impact of Event Scale-Revised, and Depression Anxiety Stress Scales (DASS) were among the measures used for establishing of the scales included in this review.
Table S2 presents a detailed account of the items from the distinct instruments included in the review and the constructs and dimensions they measure; translated instruments are not included in this table to avoid repetition of content. “Obsession with COVID-19 Scale” is a brief four-item scale focusing on the cognitive dimension. Coronavirus Anxiety Scale is a five-item brief mental health screener with an emphasis on the physiological symptoms of COVID-19 anxiety. FCV-19S is a seven-item scale measuring the construct of fear and predominantly focuses on the emotional dimension, with representative items from physiological and cognitive dimensions. COVID-19 Phobia Scale (C19 P-S) had 19 items loaded on 4 factors representing corona phobia: psychological, psychosomatic, economic, and social. CSS demonstrated a five-factor solution focusing on danger and contamination, socioeconomic consequences, xenophobia, traumatic stress, and compulsive checking related to COVID-19; moderate to strong positive correlation (0.41–0.73) was observed between the five factors. COVID-19 Anxiety Scale is a seven-item scale with representative items from cognitive, physiological, and emotional dimensions of anxiety. COVID-19 Peritraumatic Distress Index (CPDI) is a 24-item scale measuring COVID-19-associated psychological distress on a 5-point Likert scale, with overall scores ranging from 0 to 100.
Discussion
It is evident from the literature that along with the general stressors, a fear of prolonged outbreak, fear of infection vulnerability, and exposure or close contact with COVID-19-affected individuals negatively influence the mental health and well-being.36 The psychiatric symptoms encompass depression, anxiety, somatic symptoms, panic attacks, psychosis, and suicidal tendencies.37, 38 CSS and C19 P-S consider the negative economic consequences of COVID-19 as contributing towards the COVID-19-associated mental health problems. Items relating to active search on the internet and social media for COVID-19 information are included in the CSS, along with practical concerns like worrying about cash transactions and future supplies of essentials, which makes CSS a comprehensive instrument among the available scales. However, CSS does not include behavioral responses to COVID-19, which found a place in C19 P-S, where items relating to avoidance of people who sneeze and spending extensive amounts of time on cleaning hands were included. Though it is not the aim of a scoping review to critically appraise/synthesize the findings, it is apparent that CSS, C19 P-S, and CPDI are more comprehensive measures compared to other scales included in this review. However, as the choice of an instrument depends on a lot of other factors such as feasibility and relevance and since all the validated scales demonstrated good psychometric properties, it is difficult to suggest the single best available instrument to measure COVID-19-related mental health problems.
According to American Psychiatric Association, concurrent validity is the extent to which one measurement is backed up by a related measurement obtained at about the same point in time, while criterion validity is reflective of the correlational nature of a measurement with an established standard of comparison. Convergent validity is defined as the extent to which responses on a test or instrument exhibit a strong relationship with responses on conceptually similar tests or instruments.39 However, these expressions do not have consistent interpretations in the literature and may overlap.30 For instance, it was reported that the concurrent validity of the Turkish version of FCV-19S was checked with Depression, Anxiety and Stress Scale-21 (DASS-21). DASS-21 is a short form of DASS-42 with three subscales: depression, anxiety, and stress.41 Since DASS-21 measures constructs of depression, anxiety, and stress, which are different from the construct of interest of FCV-19S, which is fear, and as there is a fine distinction between these constructs as evident from DSM-5, the expression “convergent validity” could have been preferred while referring to the correlation between the Turkish version of FCV-19S and DASS-21. Similar observations relating to overlapping use of the expressions of validity were made by us with regard to measuring concurrent validity of FCV-19S by comparing with DASS-21 and PVDS,42 which is a 15-item scale with two subscales of perceived infectability and germ aversion; assessment of concurrent validity of the Bangla version of FCV-19S with Bangla PHQ-9 depression measure43; checking criterion validity of FCVS-T with BRS-T,44 an instrument that assesses the ability to overcome difficult situations; assessment of concurrent validity of the Italian version of FCV-19S with HADS45 and SMSP-A46; assessing the concurrent validity of the Arabic version of FCV-19S with HADS-A, HADS-D, and HADS-T, which are the anxiety subscale, depression subscale, and combined scales, respectively.
Though it is an established notion that anxiety/fear may lead to suicidal tendencies and inclination towards substance use, there are no available scales that attempted to document these facets.47, 48 Also, none of the available scales included items on adopted coping strategies. It is noteworthy that the validatory sample for only a few scales was inclusive of the COVID-19-affected people. The mean age of the validatory samples across the scales ranged from 26.5 to 49.8 years; this finding is reflective of the necessity to consider population from different age groups in the validation process owing to the established contributory role of age in individuals’ progression towards severe disease.49 The time of validation of the scales in correspondence to the emotional epidemic curve does play a significant role in influencing the responses of the participants. All the scales were validated during the first peak of the emotional epidemic curve; therefore, validation studies during the dipping phase and second peak phase of this curve are warranted.50 A striking similarity between the majority of the scales in the present review was the predominant emphasis given to the somatic symptoms experienced by people on thinking about COVID-19. It is to be noted that the items on different scales included in the review concur to a considerable extent; this overlap must be understood in terms of the interchangeable use of the terms “anxiety,” “fear,” and “phobia” in common parlance despite the precise differences in meaning.39 C19P-S and CPDI are the two distinct scales that differ from the other scales by integrating items representative of the behavioral dimension. Except for the COVID-19 Anxiety Scale, which consisted of items on a semantic differential scale, all the other instruments chose Likert response options, which is an interesting observation in light of the potential acquiescence bias with Likert rating scales.51 COVID-19-imposed lockdown and quarantine measures may necessitate some individuals to stay away from their families. However, none of the available scales focused on separation anxiety. Failure to document the aspects of substance use and suicidal ideation is the other limitation observed in the existing scales, though these constructs were established to be possible consequences of fear and anxiety.47, 48 Another fundamental lapse identified was the inability of any of the existing scales to discern COVID-19-associated depression. Except for the OCS,52 CAS,20 and the Italian version of CPDI,33 all the remaining scales included in the review inquire about the current status of the subject but do not necessitate the patient to respond by reflecting on their experiences from the past few weeks. Because it has been six months since the identification of the first COVID-19 case, there is a necessity to focus on acute stress disorder and post-traumatic stress disorder associated with COVID-19 among the affected and recovered. A health-systems-related concern that could have an impact on the mental health of people is the unavailability or inaccessibility of healthcare facilities, which was not included in any of the validated scales included in this review. The aforementioned lapses in the scales considered in this review were discussed by us after thoroughly reviewing the catalogue of WHO psychiatric instruments53 and DSM-5.34 Moreover, drawing on the insights provided in the WHO Assessment Instrument for Mental Health Systems (WHO-AIMS), the following were identified to be the domains of mental health systems that require attention and close monitoring, learning lessons from COVID-19: the articulation of agencies for public education and awareness campaigns on mental health, development of community mental health services, development of mental health component in primary healthcare, active functioning of mental health mobile clinic teams, the increased proportion of undergraduate training hours devoted to psychiatry and mental-health-related subjects, and refresher training for HCW in mental health facilities.54 In line with these directives, Das discussed the need for telepsychiatry in active identification of individuals with psychological infirmity and provision of awareness education and psychological interventions in the Indian context.55 There is substantial literature available on the feasibility and effectiveness of online mental health services during the COVID-19 pandemic across the globe.56–58
Spoorthy et al.59 reported in their review that HCW across the globe had encountered a substantial degree of anxiety, stress, and insomnia in the course of the COVID-19 pandemic. Shanafelt et al.60 summarized the possible sources of fear and anxiety among HCW during the COVID-19 pandemic; they also discussed the conventional self-reliant nature of health fraternity as an important contributor to anxiety while dealing with a previously un-encountered disease that is outside the professionals’ area of clinical expertise. Despite the increased vulnerability of HCW in developing mental health concerns in the process of battling a pandemic the health systems are not prepared for, none of the available scales were exclusively developed for HCW. The following are a few of the concerns that render HCW more vulnerable with regard to COVID-19 impact on mental health: limited availability of personal protective equipment, necessity to work for longer durations, fear among HCW about the possibility of transmitting the infection to family members, reports on COVID-19-associated deaths of HCW around the globe, possible discrimination out of fear of infectability from society owing to the involvement of these professionals in the care provision of COVID-19-affected, etc.60–62 Given these concerns, it is also imperative that psychometric tools meant to assess COVID-19-posed mental health concerns among HCW be developed and validated.
FCV-19S was observed to be the most commonly translated and cross-culturally adapted instrument, which is available in seven languages. The probable reason for this instrument to be preferred for cross-cultural adaptation in different countries was the fact that this is the earliest available COVID-19-related psychometric tool, published on March 27, 2020. The next psychometric tool20 assessing coronavirus anxiety was published only three weeks later. Though CPDI was published on March 6, 2020, the full instrument was not made available in the publication.33 The 7-item COVID-19 Anxiety Scale was observed to be the only COVID-19 psychometric tool validated in the Indian context.31 While the adaption of validated measures developed in other countries is possible with a simple translation of the instruments to regional language, it is advisable to verify if the items in these tools meet the intended needs of Indian population, owing to the possible difference in psychological aspects between the populations.63 Even within the country, rural and urban people can psychologically be different with regard to their COVID-19-related mental health problems; therefore, scale validatory samples must include participants from diverse geographical regions so that differences in item responses across different geographic categories may be determined. Also, checking the psychometric and dimensional stability of translated measures is warranted.
The limitations of this review include confinement to the English language and the PubMed database. Nevertheless, an overview of the existing scales and identification of the knowledge gap in the evaluation of the desired constructs provides a direction for future psychometric research with regard to COVID-19-related mental health problems.
The directives for future studies include the development of more comprehensive measures to document mental health problems posed by COVID-19 pandemic by incorporation of the aspects of suicidal ideation, post-traumatic distress, coping strategies, etc. These studies must also aim for representation from diverse age, geographic, and COVID-19 exposure groups.
Conclusion
This scoping review identifies that majority of the existing scales are heavily biased towards the somatic symptoms of COVID-19-imposed mental health problems. C19 P-S, CPDI, and CSS are among the scales which attempted to capture COVID-19-associated mental health problems comprehensively. FCV-19S, while being a unidimensional scale with only seven items, offers an opportunity for screening in busy healthcare settings and also allows cross-country comparisons, owing to its validation and availability in multiple languages worldwide. The seven-item COVID-19 Anxiety Scale was identified as the only psychometric measure validated in the Indian context and could be adapted in other Indian languages.
Supplemental Material
Supplemental Material for Measuring the Impact of COVID-19 on Mental Health: A Scoping Review of the Existing Scales by Viswa Chaitanya Chandu, Yamuna Marella, Gnana Sarita Panga, Srinivas Pachava, Viswanath Vadapalli in Indian Journal of Psychological Medicine
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19 [published online ahead of print, May 27, 2020]. Diabetes Metab Syndr; 2020; 14 doi:10.1016/j.dsx.2020.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal K, Chauhan P, Chhikara K, Gupta P, and Singh MP.. Fear of COVID 2019: First suicidal case in India! Asian J Psychiatr; 2020; 49: 101989. doi:10.1016/j.ajp.2020.101989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lei L, Huang X, Zhang S, et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in outhwestern China. Med Sci Monit; 2020; 26 Published Apr 26, 2020. doi:10.12659/MSM.924609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mamun MA and Griffiths MD.. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies [published online ahead of print, Apr 7, 2020]. Asian J Psychiatr; 2020; 51 doi:10.1016/j.ajp.2020.102073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang W, Hu T, Hu B, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students [published online ahead of print, May 13, 2020]. J Affect Disord; 2020; 274 doi:10.1016/j.jad.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China [published online ahead of print, Apr 13, 2020]. Brain Behav Immun; 2020; 87 doi:10.1016/j.bbi.2020.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu J, Sun L, Zhang L, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry; 2020; 11 Published Apr 29, 2020. doi:10.3389/fpsyt.2020.00386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hossain MM, Sultana A, and Purohit N.. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiol Health; 2020; doi:10.4178/epih.e2020038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet; 2020; 395 (10227). doi:10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic [published online ahead of print, May 18, 2020]. Lancet Psychiatry; 2020; 7 doi:10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li G, Miao J, Wang H, et al. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: A cross-sectional study [published online ahead of print, May 4, 2020]. J Neurol Neurosurg Psychiatry; 2020. doi:10.1136/jnnp-2020-323134 [DOI] [PubMed] [Google Scholar]
- 12.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis [published online ahead of print, May 8, 2020]. Brain Behav Immun; 2020. doi:10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang Y and Zhao N.. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res; 2020; 288 doi:10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study [published online ahead of print, Mar 30, 2020]. Brain Behav Immun; 2020. doi:10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walton M, Murray E, and Christian MD.. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care; 2020; 9(3). doi:10.1177/2048872620922795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beidas RS, Stewart RE, Walsh L, et al. Free, brief, and validated: Standardized instruments for low-resource mental health settings. Cogn Behav Pract; 2015; 22(1). doi:10.1016/j.cbpra.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levac D, Colquhoun H, and O’Brien KK.. Scoping studies: advancing the methodology. Implement Sci; 2010; 5(1). doi:10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol; 2018; 18(1). Published Nov 19, 2018. doi:10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arksey H and O’Malley L.. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol; 2005; 8(1). doi:10.1080/1364557032000119616 [Google Scholar]
- 20.Lee SA. Coronavirus anxiety sale: A brief mental health screener for COVID-19-related anxiety [Epub Apr 16, 2020. PMID: 32299304]. Death Stud; 2020; 44(7). doi:10.1080/07481187.2020.1748481 [DOI] [PubMed] [Google Scholar]
- 21.Ahorsu DK, Lin CY, Imani V, et al. The Fear of COVID-19 Scale: Development and initial validation [Epub ahead of print. PMID: 32226353; PMCID: PMC7100496]. Int J Ment Health Addict; 2020. Mar 27 doi:10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.TzurBitan D, Grossman-Giron A, Bloch Y, et al. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population [Epub ahead of print. PMID: 32425276; PMCID: PMC7227556]. Psychiatry Res; 2020. May 15; 289 doi:10.1016/j.psychres.2020.113100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakib N, Bhuiyan AKMI, Hossain S, et al. Psychometric validation of the Bangla Fear of COVID-19 Scale: Confirmatory factor analysis and Rasch analysis [Epub ahead of print. PMID: 32395096; PMCID: PMC7213549]. Int J Ment Health Addict; 2020. May 11 doi:10.1007/s11469-020-00289-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haktanir A, Seki T, and Dilmaç B.. Adaptation and evaluation of Turkish version of the Fear of COVID-19 Scale [Epub ahead of print. PMID: 32469627]. Death Stud; 2020. May 29 doi:10.1080/07481187.2020.1773026 [DOI] [PubMed] [Google Scholar]
- 25.Arpaci I, Karataş K, and Baloğlu M.. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S) [Epub ahead of print. PMID: 32394993; PMCID: PMC7211675]. Pers Individ Dif; 2020. May 11; 164 doi:10.1016/j.paid.2020.110108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reznik A, Gritsenko V, Konstantinov V, et al. COVID-19 fear in Eastern Europe: Validation of the Fear of COVID-19 Scale [Epub ahead of print. PMID: 32406404; PMCID: PMC7217343]. Int J Ment Health Addict; 2020. May 12. doi:10.1007/s11469-020-00283-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satici B, Gocet-Tekin E, Deniz ME, and Satici SA.. Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey [Epub ahead of print. PMID: 32395095; PMCID: PMC7207987]. Int J Ment Health Addict; 2020. May 8 doi:10.1007/s11469-020-00294-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Soraci P, Ferrari A, Abbiati FA, et al. Validation and psychometric evaluation of the Italian version of the Fear of COVID-19 Scale [Epub ahead of print. PMID: 32372892; PMCID: PMC7198091]. Int J Ment Health Addict; 2020. May 4 doi:10.1007/s11469-020-00277-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alyami M, Henning M, Krägeloh CU, and Alyami H.. Psychometric evaluation of the Arabic version of the Fear of COVID-19 Scale [Epub ahead of print. PMID: 32427217; PMCID: PMC7229877]. Int J Ment Health Addict; 2020. May 16 doi:10.1007/s11469-020-00316-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor S, Landry CA, Paluszek MM, et al. Development and initial validation of the COVID Stress Scales [Epub 2020 May 4. PMID: 32408047; PMCID: PMC7198206]. J Anxiety Disord; 2020. May; 72 doi:10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandu VC, Pachava S, Vadapalli V, and Marella Y.. Development and initial validation of the COVID-19 Anxiety Scale [PMID: 32496255]. Indian J Public Health; 2020. Jun; 64(suppl). doi:10.4103/ijph.IJPH_492_20 [DOI] [PubMed] [Google Scholar]
- 32.Evren C, Evren B, Dalbudak E, Topcu M, and Kutlu N.. Measuring anxiety related to COVID-19: A Turkish validation study of the Coronavirus Anxiety Scale [Epub ahead of print. PMID: 32490730]. Death Stud; 2020. Jun 3 doi:10.1080/07481187.2020.1774969 [DOI] [PubMed] [Google Scholar]
- 33.Costantini A and Mazzotti E.. Italian validation of CoViD-19 peritraumatic distress index and preliminary data in a sample of general population [PMID: 32489191]. Riv Psichiatr; 2020. May–Jun; 55(3). doi:10.1708/3382.33570 [DOI] [PubMed] [Google Scholar]
- 34.American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders (DSM-5). Washington, DC: American Psychiatric Publishing, 2013. [Google Scholar]
- 35.Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations [published correction appears in Gen Psychiatr 2020 Apr 27; 33(2): e100213corr1]. Gen Psychiatr; 2020; 33(2). Published Mar 6, 2020. doi:10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hossain M, Tasnim S, Sultana A, et al. Epidemiology of mental health problems in COVID-19: A review. PsyArXiv; 2020. https://doi.org/10.31234/osf.io/q8e5u [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hall RC, Hall RC, and Chapman MJ.. The 1995 Kikwit Ebola outbreak: Lessons hospitals and physicians can apply to future viral epidemics. Gen Hosp Psychiatry; 2008; 30(5). doi:10.1016/j.genhosppsych.2008.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sim K, Huak Chan Y, Chong PN, Chua HC, and WenSoon S.. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res; 2010; 68(2). doi:10.1016/j.jpsychores.2009.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Psychological Association. APA dictionary of psychology. Washington, DC: American Psychological Association, 2007. [Google Scholar]
- 40.University of York Department of Health Sciences. Measuring health and disease—the validity of measurement methods [Internet], https://www-users.york.ac.uk/~mb55/msc/clinimet/week8/validity.pdf (accessed June 8, 2020).
- 41.Henry JD and Crawford JR.. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol; 2005; 44(Pt 2). doi:10.1348/014466505X29657 [DOI] [PubMed] [Google Scholar]
- 42.Duncan LA, Schaller M, and Park JH.. Perceived vulnerability to disease: Development and validation of a 15-item self-report instrument. Pers Individ Differ; 2009; 47(6): 541–546. [Google Scholar]
- 43.Chowdhury AN, Ghosh S, and Sanyal D.. Bengali adaptation of brief patient health questionnaire for screening depression at primary care. J Indian Med Assoc; 2004; 102(10): 544–547. [PubMed] [Google Scholar]
- 44.Haktanir A, Lenz AS, Can N, and Watson JC.. Development and evaluation of Turkish language versions of three positive psychology assessments. Int J Adv Couns; 2016; 38(4): 286–297. [Google Scholar]
- 45.Costantini M, Musso M, Viterbori P, et al. Detecting psychological distress in cancer patients: Validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer; 1999; 7(3). doi:10.1007/s005200050241 [DOI] [PubMed] [Google Scholar]
- 46.Knappe S, Klotsche J, Strobel A, et al. Dimensional anxiety scales for DSM-5: Sensitivity to clinical severity. Eur Psychiatry; 2013; 28(7). doi:10.1016/j.eurpsy.2013.02.001 [DOI] [PubMed] [Google Scholar]
- 47.Killgore WDS, Cloonan SA, Taylor EC, et al. Suicidal ideation during the COVID-19 pandemic: The role of insomnia [published online ahead of print, May 27, 2020]. Psychiatry Res; 2020; 290 doi:10.1016/j.psychres.2020.113134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sher L. The impact of the COVID-19 pandemic on suicide rates [published online ahead of print, Jun 15, 2020]. QJM; 2020. doi:10.1093/qjmed/hcaa202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu K, Chen Y, Lin R, and Han K.. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect; 2020; 80(6). doi:10.1016/j.jinf.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ransing R, Adiukwu F, Pereira-Sanchez V, et al. Mental health interventions during the COVID-19 pandemic: A conceptual framework by early career psychiatrists [published online ahead of print, Apr 14, 2020]. Asian J Psychiatr; 2020; 51 doi:10.1016/j.ajp.2020.102085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Park M and Wu AD.. Item response tree models to investigate acquiescence and extreme response styles in Likert-type rating scales. Educ Psychol Meas; 2019; 79(5). doi:10.1177/0013164419829855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee SA. How much “Thinking” about COVID-19 is clinically dysfunctional? [published online ahead of print, Apr 27, 2020]. Brain Behav Immun; 2020; 87 doi:10.1016/j.bbi.2020.04.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Janca A and Chandrashekar CR. Catalogue of WHO psychiatric assessment instruments. 2nd ed. Geneva: World Health Organization, https://apps.who.int/iris/handle/10665/62036 (July 26, 2020). [Google Scholar]
- 54.World Health Organization. iWorld Health Organization Assessment Instrument for Mental Health Systems (WHO-AIMS). Version 2.2. Geneva: World Health Organization, 2005, www.who.int/mentalhealth/evidence/AIMSWHO22.pdf [Google Scholar]
- 55.Das N. Psychiatrist in post-COVID-19 era: Are we prepared? [published online ahead of print, Apr 7, 2020]. Asian J Psychiatr; 2020; 51 doi:10.1016/j.ajp.2020.102082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry; 2020; 7(4). doi:10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ifdil I, Fadli RP, Suranata K, Zola N, and Ardi Z.. Online mental health services in Indonesia during the COVID-19 outbreak [published online ahead of print, May 5, 2020]. Asian J Psychiatr; 2020; 51. doi:10.1016/j.ajp.2020.102153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.D’Agostino A, Demartini B, Cavallotti S, and Gambini O.. Mental health services in Italy during the COVID-19 outbreak. Lancet Psychiatry; 2020; 7(5). doi:10.1016/S2215-0366(20)30133-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spoorthy MS, Pratapa SK, and Mahant S.. Mental health problems faced by healthcare workers due to the COVID-19 pandemic: A review [published online ahead of print, Apr 22, 2020]. Asian J Psychiatr; 2020; 51 doi:10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shanafelt T, Ripp J, and Trockel M.. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic [published online ahead of print, Apr 7, 2020]. JAMA; 2020. doi:10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- 61.Ing EB, Xu QA, Salimi A, and Torun N.. Physician deaths from corona virus (COVID-19) disease [published online ahead of print, May 15, 2020]. Occup Med (Lond) 2020. doi:10.1093/occmed/kqaa088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Greenberg N. Mental health of health-care workers in the COVID-19 era [published online ahead of print, Jun 19, 2020]. Nat Rev Nephrol; 2020. doi:10.1038/s41581-020-0314-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Menon V and Praharaj SK.. Translation or development of a rating scale: Plenty of science, a bit of art. Indian J Psychol Med; 2019; 41(6). Published Nov 11, 2019. doi:10.4103/IJPSYM.IJPSYM_418_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Measuring the Impact of COVID-19 on Mental Health: A Scoping Review of the Existing Scales by Viswa Chaitanya Chandu, Yamuna Marella, Gnana Sarita Panga, Srinivas Pachava, Viswanath Vadapalli in Indian Journal of Psychological Medicine