Abstract
Introduction
Telemedicine has become part of mainstream medical practice. High quality virtual care is a skill that will be required of many physicians. Skills required for effective evaluation and communication during a video encounter differ from skills required at bedside, yet few rubrics for educational content and student performance evaluation in telemedicine training have been developed. Our objective was to develop, implement, and assess a training module designed to teach medical providers techniques to deliver professional, effective, and compassionate care during a telemedicine encounter.
Methods
We created a simulation-based, 8-hour modular curriculum using the PEARLS debriefing framework with video-based encounters focused on “web-side manner” as a critical corollary to traditional bedside manner. We recorded simulated cases for each student with standardized patients, guided debriefs, and incorporated small-group exercises to teach advanced communication and examination skills.
Results
Of medical students, 98 in their major clinical year participated in 2019. Of participants, 97% were enthusiastic about the course; 100% felt simulation was an effective mechanism for delivery of the educational material. After participation, 71% believed that telemedicine had the potential to become part of their future practice; 92% perceived an improvement in their comfort and ability to conduct video-based patient encounters.
Discussion
Teaching telemedicine using this methodology was well received by students, providing early exposure to this evolving aspect of medical practice. Qualitative comments were used for targeted improvements of the content and delivery for curriculum development. Objective assessment tools of students completing telemedicine encounters need to be created.
Keywords: Telemedicine, Standardized Patients, Simulation, Emergency Medicine, Flipped Classroom, Multimedia, Online/Distance Learning, Qualitative Research, Self-Assessment, Virtual Learning
Educational Objectives
By the end of this activity, learners should be able to:
-
1.
Describe the evolving importance of telemedicine in the current health care environment.
-
2.
Demonstrate the fundamentals of video-based complete history taking with a patient.
-
3.
Perform a physical exam over video, predicting the limitations of this method, and employing alternatives to ensure appropriate information is elicited to make a disposition decision.
-
4.
Use advanced communication and professionalism skills in “web-side manner” to build rapport with patients such that trust is established, and postvisit instructions are agreed upon and followed, particularly for patients that require escalation to in-person care.
Introduction
Telemedicine and virtual care, which includes a variety of technology formats that facilitate health care evaluation and communication, has moved from a low volume, niche service to an important component of mainstream medical care. Real-time audio/video interaction between providers and patients is a large part of the telemedicine landscape. Millions of patient-initiated visits with health care providers have now been performed over real-time audio and video, and currently 76% of US hospitals connect with patients and providers through this modality.1 Telemedicine is being used as a tool to reduce rural healthcare disparities,2,3 and as a mechanism to increase flexibility of the health care system in anticipation of a broader transition to value-based care payment strategies.4 Surveys of the United States population at large suggest patients are eager to have broader availability of telemedicine options for care.5 Employers are using telemedicine benefits as a means to decrease costs and increase worker productivity. Of employers with more than 50 workers, 67% say their largest insurance plan offers telemedicine.6 The majority of health care institutions are now offering or planning to offer this type of care,7,8 and major organizations such as the American Heart Association are making recommendations to increase the availability of telemedicine services.9
In 2020, the United States was struck by the novel coronavirus pandemic, throwing the health care system into uncharted territory in modern times. Telemedicine rapidly became instrumental in providing medical care to those who did not warrant or desire an in-person visit based on the redirection of resources and risks associated for transmission of the virus.10 Medical providers, out of necessity, started doing telemedicine visit encounters with patients with little to no training. Some of the larger academic medical centers who had previously existing telemedicine infrastructure rapidly were able to provide educational sessions to physicians and advanced practice providers (APPs).11 This event and change in the health care culture further demonstrates the importance of increasing preparedness in telemedicine across the country in the future.12
While today's medical students will encounter telemedicine in their clinical careers, medical education has not kept pace with the growing need for telemedicine education. It has been suggested that telemedicine may constitute the majority of practice for some current graduates, and in fact this is already the case for some behavioral health and neurology providers.13,14 However, little has been published regarding the mechanisms for teaching telemedicine skills.15 The American Medical Association has recommended that telemedicine training be incorporated into medical education,16 and core competencies for virtual health care have been identified.17 Educators in the field of dermatology, for example, have found teledermatology useful in both graduate and undergraduate education as a teaching tool.18 Neurology is another specialty that is embracing the need for education in this arena given the prevalence of telemedicine use in stroke evaluation, particularly in hospitals with limited access to an in-person neurologist.19,20 Recently telemedicine has begun to be included in residency training as part of clinical follow-up shifts in emergency medicine.19 The number of ACGME programs currently having implemented formalized teaching for these roles is limited, perhaps due to a lack of utilization of the technology at some institutions or the current lack of best practices in teaching this material.
Analogous to the GME arena, there is also limited data available regarding educational content in telemedicine for undergraduate medical students,14 and no published curricula related to development of the individual skills required to deliver effective care through telemedicine. Telemedicine training in the form of OSCEs has allowed learners to gain exposure to telemedicine in a safe simulated teaching environment and assesses medical student competencies.21 While the current medical students are often regarded as “digital natives” by virtue of their predominant age range,22 this does not automatically translate into an ability to convey warmth, empathy, and professionalism during a video encounter. There are specific skills required to move the clinical encounter from the bedside to “web-side,”17 and we currently have the opportunity to explore different strategies for education in this arena.
Our objective was to develop an innovative curriculum to prepare medical providers for the practice of telemedicine and virtual care, through real-time audio/video interaction with standardized patients (SPs) and a review of the telemedicine technical and regulatory landscape. Simulation was chosen as a feasible, safe, and effective teaching mechanism. In general, simulated patient encounters are often used to teach the face-to-face skills required to convey good bedside manner: verbal and nonverbal communication, professionalism, warmth, and empathy. Physical exam skills are both taught and assessed using simulation techniques. Of significant importance to medical students, the National Board of Medical Examiners issued Step 2 Clinical Skills, a standardized exam, using simulated encounters to ensure baseline competency for medical licensing in the United States.23 We developed an experiential curriculum using multiple formats to teach, in a collaborative learning environment, professional verbal and nonverbal techniques that are employed over video. We began with medical school students as our initial audience, described here, and are now expanding to graduate medical students (residents and fellows), APP students, and faculty.
Methods
Curriculum Development
This curriculum was developed by medical school faculty affiliated with a large, urban, quaternary care medical center and implemented in 2019. The medical school, with approximately 110 medical students per class, had a required primary care clerkship for students in their major clinical year. The leadership of this clerkship partnered with the department of emergency medicine to deliver core knowledge in telemedicine skills during the rotation. This curriculum encouraged students to explore the similarities and differences between in-person and video-based interactions. In order to more thoroughly convey physical exam technique training in our curriculum, we supplemented SP encounters via telemedicine with small-group tabletop exercises to discuss and emulate different approaches for conducting a virtual physical exam. We limited the traditional didactic lecture style to only deliver introductory and background content on telemedicine.
Using simulated encounters with SPs and tabletop exercises, a four-module curriculum was developed to address the following elements of a video-based encounter: (1) on-camera etiquette, (2) verbal and nonverbal communication skills during medical history taking, (3) physical exam skills, and (4) appropriate disposition planning to ensure patient safety and ongoing care.
The course was led by three faculty from the department of emergency medicine who were experienced in medical education and active clinical providers of telemedicine care, with facilitation by a course administrator. More specifically, one faculty member was the director of simulation education, fellowship-trained in simulation to oversee development and execution of the simulation exercises and debriefs for each course; one was the director of telemedicine, who founded our telemedicine program and oversees the telemedicine-based content delivered; and, one was the director of undergraduate medical education, with extensive experience in both undergraduate and graduate medical education to tailor content to each learner group. This faculty had facilitated training courses for many levels of providers including attending physicians, resident physicians, medical students, and advanced practice providers. Additional telemedicine faculty were present on an ad hoc basis to provide clinical perspectives at various stages of the course.
In 2019, as part of their required time during the primary care clerkship, all medical students took part in this 8-hour, in-person course in advanced communication skills and physical diagnosis via a video-based platform. However, beginning in January 2020, we varied the course length and distribution over 1 to 2 days, such as two 4-hour sessions, or modified course elements to fit a given time allotment. For example, we did a 4-hour virtual version using only the introductory material (Appendix A), homework assignment (Appendix B), and the tabletop exercises.
Requirements/Materials Needed
Each session ranged from eight to 16 students. The number of participants dictated the space needed and the length of the course depending on the number of SPs employed, as each participant had a 20-minute block with an SP one-on-one for each module.
Personnel requirements included two to three faculty (minimum of one comfortable with simulation and group debriefing; all faculty used telemedicine as part of their practice), audio/visual tech support (collated videos from sessions were stored in a shared folder, and facilitated access from the classroom computer for review during debriefings), and one coordinator (oversaw the scheduling and flow of students).
SPs were recruited by our Clinical Skills Center coordinator and trained in the four cases by both an SP educator from the Clinical Skills Center and our director of simulation education. The training consisted of an in-person, 2-hour workshop where they reviewed the cases, role-played the scenarios, and had time for questions and answers. The SPs were offsite during the course sessions, whether in their home or another quiet space to allow for a more realistic portrayal of patients calling in from their personal habitat via telemedicine. We did not specifically review the technology that the SPs were individually using other than to give them guidance about the software required, request that they have a high-speed, stable internet connection at the location where they would be for the session, and then allowed them to test it prior to their first encounter with our course coordinator if desired. The number of SPs scheduled per session was based upon the number of students enrolled in the course. For example, if there were 16 students enrolled in the course, we scheduled eight SPs to do the cases with both group A and group B. There was more than one SP playing the same role, and each SP did multiple modules, which minimized the overall time requirement for the course. All cases for the modules were built around a patient with the same gender and age for logistical reasons to be able to use the same SPs throughout the course. We varied the student-to-SP pairings for each module so that there was no transference from one case to the next.
Space requirements included one large classroom for didactics, debriefs, and wrap-up (sized to accommodate entire group attending course), and private spaces for each individual encounter with the SP to take place (same as the number of participants in the course or divided in half if a two-group format was used).
Technology requirements included laptops (one for each SP encounter as well as one in the large classroom for presentations and replaying videos during debriefs), and virtual meeting rooms for the web-based encounters to take place, with recording capability for videos to be downloaded to review during debriefing.
Course Structure
Prior to the start of the course, each student completed an initial homework exercise involving a self-recorded video submission of him/herself delivering instructions to a patient regarding RICE (rest, ice, compress, elevate) recommendations for a soft tissue ankle injury (Appendix B). The purpose of this exercise was to allow for students to become more comfortable on camera and simulate what it would be like to do a video session in their home setting. RICE was only pertinent in that it was our choice of topic. Any other type of instructions or assignment where the student provided an initial recording of themselves for a baseline assessment by the faculty would be fine. The videos of the homework exercise were uploaded by the students to a secure database (along with all the subsequent interactions with SPs) maintained by the medical school.
To begin the course, there was a 30-minute introductory lecture to telemedicine, including the breadth of current applications, delivery of care to resource limited settings, and anticipated growth of this modality in the near future (Appendix C). Basic information about technical specifications required for live audio/video communication, protection of patient privacy, and the regulatory landscape that applied to telemedicine care were also incorporated into the didactic. A live feed video interaction (using Zoom) with a practicing primary care physician who discussed the use of telemedicine in his daily practice was also part of the curriculum. This was optional depending on the setting and audience.
The didactic was followed by the first debriefing session about the homework video assignment submitted prior to arrival (Appendix K). During this debrief, students watched segments from the video submissions preselected by the faculty debriefer, to teach the basics of telemedicine visual preparedness including lighting, background, and setting. Subsequently, depending on the number of learners and SPs retained, the participants were split into two groups (Groups A and B) which rotated between completing simulations with SPs, debriefs, and tabletop exercises (Appendix A). Any group larger than 10 students should be split into two groups to increase engagement of learners in the tabletop sessions.
Group A started with the simulations. Prior to starting each case, each student in was given an introductory prompt sheet to outline the care setting into which the patient was calling (private office, virtual urgent care, etc.), basic information about the patient, and the goals of the interaction (Appendix D). The four cases provided to the students were as follows: (1) intake of a new patient to clinic with a history of hypertension who found in-person care logistically challenging (Appendix E), (2) same patient as the first encounter subsequently calling in as an established patient for an acute complaint of dyspnea that was likely to be a subacute presentation of new congestive heart failure (Appendix F), (3) a new patient calling for an urgent consult with flank pain symptoms and a history suggesting a complicated urinary tract infection (Appendix G), and (4) a new patient with self-diagnosed anxiety who was actually in alcohol withdrawal (Appendix H).
The students had 15 minutes of video time with the SP to complete each interaction via Zoom, but any video conferencing software could be used. When the simulated encounter started, the student was responsible for pressing the record button in order to capture video and the sound for their interaction (Figure). These video recordings were transferred into a cloud drive immediately following the encounter, collated by our audio/visual team into an accessible folder for the debriefer immediately, allowing for playback during the debrief portion of the module (Figure). There was no individual postencounter exercise.
Figure. Video playback as seen by the audience with the course participant on the left and the standardized patient on the right. (Author owned. Permission for use granted by both participants.).
While Group A completed the simulations, Group B completed the tabletop exercises (Appendix I). The primary facilitator for these sessions was the director of undergraduate medical education, with one to two additional faculty members from our telemedicine program. During these exercises, the students were asked to describe and mimic how they would conduct different elements of the physical exam over video, including obtaining vital signs and focus elements of the exam, based on the chief complaint. The exercises covered a remote cardiopulmonary exam with a case of dyspnea, a remote abdominal and genitourinary exam with a case of abdominal pain, a psychiatric assessment for depression and suicidality with a detailed social history, and pertinent observed exam features for a case involving a medication refill. The students were given immediate verbal feedback, direction, and demonstrations as appropriate by the faculty (Appendix J).
The debrief for the homework assignment was done for each group as the first SP case was taking place (Appendix K). The debriefs for simulations occurred with both groups together as the last stage of each the module (Appendices L, M, N, and O). The debriefing sessions were focused on addressing the course objectives, with content fostered by a group review of individual clips from videos taken of each session. The Promoting Excellence and Reflective Learning in Simulation (PEARLS) framework24 was used to guide a video-assisted discussion that focused on developing verbal and nonverbal communication skills required for telemedicine and an understanding of the conversion of bedside to “web-side” medical care. The four simulations allowed for a natural progression in the debriefing focus on the four stages of an encounter. Within the PEARLS framework, the faculty leading the debrief had multiple options for what debriefing technique to use, but relied mostly on advocacy-inquiry and directed feedback. SP checklists were initially built for this course, however were not used.
Program Evaluation and Data Analysis
Pre- and postcourse surveys (Appendices P and Q) were created by the course faculty prior to implementation and distributed to the participants. The goal of these surveys was twofold: (1) to assess the change between pre- and postcurriculum attitudes towards telemedicine, knowledge about the use of telemedicine in general, and self-assessed performance by the students; and, (2) to elicit suggestions for improvement to be applied in the iterative development of this curriculum. Feedback was assessed using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). Additional open-ended questions were asked for suggested improvements, revisions, and highlights of the program. Only aggregate evaluation data from students agreeing to involvement in the research was reported.
Study Protocol
Students consented to participate in the research related to this curriculum. By consenting, they agreed to allow the use of their pre- and postcourse surveys and video-recorded interactions with SPs for future educational research purposes. Research related to this curriculum development and implementation was approved by the Weill Cornell Medicine Institutional Review Board.
Results
There were eight sections of this course delivered in 2019, including 113 medical students during their major clinical year, of which 98 consented to participate in the study. This captured 1 full year of students rotating through the required primary care clerkship during their major clinical year. There was no difference in the educational experience delivered to those who did not consent.
Prior to taking the course, 78% of the learners had never performed a telemedicine encounter (simulated or real) and 85% had never received training in any capacity regarding telemedicine. There were 11 students (12%) who had received a lecture or workshop which included some telemedicine content. In the presurvey, only 24% felt prepared to conduct a video-based patient visit and 39% felt that telemedicine was going to be applicable to their future career.
In the postsurvey, 92% felt prepared to conduct a video-based patient visit and 71% felt that telemedicine would be incorporated into their future career.
Of the 98 learners who participated in the curriculum and agreed to have their data applied to research, 97% found the course to be useful and 100% felt simulation was an effective teaching strategy. Almost all learners found that the sessions provided insight into their communication, history taking, and physical exam skills. Similarly, almost all learners also concluded that the simulation sessions would alter their approaches to communicating with patients over a virtual medium going forward and influenced their remote history taking and physical exam skills.
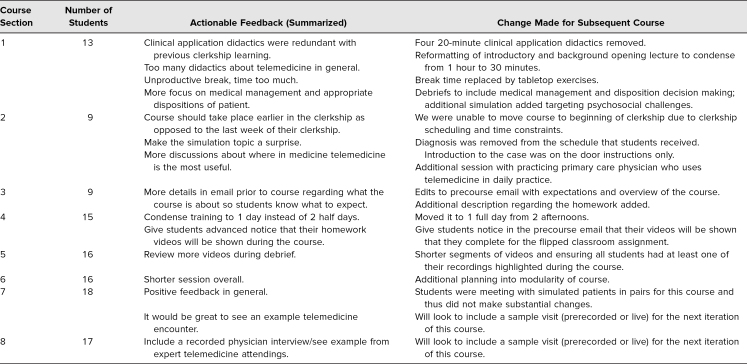
The open-ended questions on the survey informed changes to the structural and educational content of the course over time. The Table outlined the actionable feedback from each postcourse survey with the iterative change made to subsequent sections.
Table. Qualitative Feedback From Course Surveys With Actionable Items for Iterative Change.
Discussion
Iterative Design
After each session, the faculty and coordinator met to discuss improvements for the next course. The changes from the first to second delivery of the course were the most dramatic. They are discussed in further detail here to highlight why we have chosen the content presented in the final course and pitfalls to avoid for others who might implement a variation of this curriculum. Subsequent iterations of the course have had smaller, experimental differences to attempt to improve flow, or small structural changes to respond to differently sized groups. The educational content has stayed the same since the second iteration of the course based on positive feedback, and we will be adding a demonstrative telemedicine visit as an example in the future.
The initial iteration of the course for 13 students had three simulations and included four 20-minute didactic sessions targeting various clinical applications of telemedicine perceived to be useful in the primary care setting based on learning objectives from our primary care clerkship, adopted from the Family Medicine Clerkship Curriculum published by the Society of Teachers of Family Medicine.25 Clinical applications included: urinary tract infection management, dyspnea, suicidal ideation, and substance misuse. Feedback from the postcourse survey indicated that students considered these lectures repetitive and that this material was adequately covered elsewhere in the clerkship curriculum. Based on this feedback, the four 20-minute didactic clinical application sessions were removed in the second run of the course and a 30-minute web-based interactive session with a primary care physician who used telemedicine as a routine part of his practice was added.
Student feedback indicated that they appreciated understanding the scope of telemedicine care, the rural uses of telemedicine, and basic medicolegal implications, but that they were not as interested in the history of its development or our own institutional applications. In response, the introductory didactic component of the course was condensed and reformatted so that the history, current application, and future of telemedicine was changed from three 20-minute lectures to one 30-min introduction. To highlight individual practitioner involvement with telemedicine and given the fact that this course resided in the primary care clerkship at our institution, we added a real-time session with a primary care provider who called into the classroom via Zoom to discuss his current practice using telemedicine.
In the first iteration of the course, the students had break time when they were not doing the simulation while the other group completed their case. The faculty had anticipated students using this time to study for the shelf exam that occurred several days after the course. Students felt that this break time was unproductive, and they requested more teaching around physical exam and concrete management planning. In the second iteration of the course, we added the tabletop exercises instead of breaks and used these exercises to discuss virtual physical examination skills as well as concrete management options. We likewise made an effort in the simulation debriefs to include more discussion around disposition planning and specific treatment options. The reviews subsequently were very positive and none of the students requested additional break time.
With time gained from removing didactic components, we were able to add an additional simulation session to stimulate discussion about psychosocial challenges with telemedicine and safe disposition planning. The students found this case the most difficult to navigate.
Subsequent courses, of which there were seven, included a total of 100 students. The postcourse surveys did not indicate a need for changed content but rather smaller stylistic changes. Having a smaller group size was preferred by the facilitators, preferably with nine to 10 students per course. This allowed for a greater breadth of discussion in terms of the ability to move through the content and explore different aspects of the simulations. Fewer students also ameliorated logistical constraints such as timing of the course and physical space required.
Of note, we did have one iteration of the course in 2019 where, due to extenuating circumstances, we could not employ enough SPs to allow for the students to have one-on-one interactions for the simulations. The students were paired in their interview of the SP. While this was not our recommended method, the students' feedback was such that they felt they learned from their colleague and this was not perceived as detrimental to their experience as we had anticipated.
With the recent COVID-19 pandemic in spring 2020, we ran this course entirely remotely, using a separate Zoom meeting room as the classroom, and used two of the four SP modules along with the didactic material. This course was completed in 4 hours rather than 8 hours. We allowed six to eight participants per course so that there was only one group, and then were able to run a morning course and an afternoon course to accommodate all students. The students involved in these courses were not part of the study group reported here.
Outcomes
This course was designed to meet the stated educational objectives when completed in full. The introductory didactic was developed to teach students about the evolution of telemedicine and its growing role in the current health care environment. The simulations collectively have students practice history taking and physical exam skills with temporal observation and feedback from faculty. The debriefs and final tabletop exercise explicitly discussed building rapport with patients and appropriate disposition planning. We believed that there was enough overlap between the simulations that a modified course will likewise satisfy the educational objectives; however, this may require more strategic debriefing to move the discussion more quickly through all necessary components.
This course will hopefully to lead to long-term positive outcomes such as increased understanding of skills required for providing virtual care, confidence for learners in engaging with telemedicine delivery of care options, a reduction of medical errors, as well as a measurable and lasting improvement in video interaction skills as experienced by the patient (i.e., “web-side manner”) leading to increased patient satisfaction. We are aware that some of the outcomes we hope to achieve may prove difficult to tangibly measure.
Limitations
One limitation of this work was that our current outcome measurements were self-assessments made by learners. Such assessments are highly subjective and may not be an accurate reflection of performance improvement. Our outcome assessment would be stronger if we had made objective measures of performance before and after students took the course. Even more ideal than objective measures of student efficacy in simulated encounters would be if we could make objective measurements in a clinical environment with real patients. A second limitation was related to how our course content iteratively changed and judgments were initially made based on a small sample size. Although the core simulation and debrief portion of the course remained constant, we deemphasized lecture content and added tabletop exercises between the first and second iteration. There were fewer recommendations for changes in the second course iteration and afterwards, indicating improvement, but our sample size for each course was too small to determine the relative contribution of these changes to our outcomes.
We were limited by the time at which we could hold the course as part of the primary care clerkship. Ideally, we would have held the course at the beginning of the rotation so that students could use the clerkship to practice their skills rather than at the end when things were coming to a close and the students were anxious about the shelf exam. A potential option would be to run the course over several weeks in a modular format, so that the content is revisited over time as the simulations become more complex, introducing new concepts and thought processes. This might allow the students time to use these skills in clinical practice between sessions and stimulate more advanced conversations.
While having the four video encounters with the SPs and completing Kolb's experimental26 cycle for each was our current model, having a fewer number of simulations could potentially shorten the course. We think the course is strongest as a complete entity in our initial rollout, although we have delivered the content only using certain modules when time was limited and did so in an entirely virtual format. To date, we have not implemented comparable experiences over a significant enough duration to create judgments on the comparison. However, in the post-COVID-19 period of flexibility and creativity in reorganizing the curriculum, we may have an opportunity going forward. Depending on the resources available for other institutions in general, an abbreviated course is a viable option to pursue.
An additional limitation that may hinder the ability of a course to meet the educational objectives in general was the required level of training of different faculty members in simulation, education, and clinical telemedicine to successfully implement this course. This may be problematic at smaller institutions.
Future Directions
Using simulation and tabletop exercises, we were able to effectively teach students telemedicine specific communication and remote physical evaluation skills. These skills are becoming increasingly critical to patient care. Our next steps in this telemedicine educational research program included development and validation of measurement tools for the objective assessment of professionalism and communication during video-based encounters. We plan to evaluate the impact of our course on student performance during a telemedicine OSCE that is being incorporated in the OSCE testing curricula for our medical college, as well as being a way of testing skills acquired during the course going forward.
We also aim to create content on directive feedback that will be put into an online module in which students can participate prior to the course. Longer-term studies will be designed to measure the impact of our training on actual patient-centered outcomes and patient experience. Assessment of providers after completing individual modules and then caring for patients with that specific chief complaint may be a more targeted approach to objectively evaluate the content delivered.
We are currently expanding the scope of the course attendees to faculty, APPs, APP students, and trainees in GME programs. The content has been kept the same for these groups, with only a shift in the debrief content around complexities in medical management and disposition planning, as is appropriate for each level of learner. Future expansions to the course may include the nuances of provider-to-provider interactions when telemedicine is used as a consultation platform, with a goal of improved teamwork and patient care.
During the COVID-19 pandemic, we experienced a rapid rollout of telemedicine into many sectors that had not yet used this technology or mode of delivering care. One positive of this situation is that this was an unexpected test case for a more widespread dissemination of telemedicine and has subsequently convinced many of the future potential telemedicine provides. Thus, we anticipate the need for institutions across the country to employ a course such as this to train providers sooner than we would have otherwise expected in order to hopefully ease the burden of any future COVID-19 wave, or other infectious disease.
Appendices
- Course Schedules.docx
- Homework Assignment.docx
- Intro Didactic.pptx
- Door Instructions.docx
- SP Intake Simulation.docx
- SP CHF Simulation.docx
- SP UTI Simulation.docx
- SP ETOH Simulation.docx
- Tabletop Exercises.docx
- Tabletop Facilitator Guide.docx
- Homework Debriefing Guide.docx
- Intake Debriefing Guide.docx
- CHF Debriefing Guide.docx
- UTI Debriefing Guide.docx
- ETOH Debriefing Guide.docx
- Prequestionnaire.docx
- Postquestionnaire.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
None to report.
Prior Presentations
Mulcare M, Naik N, Greenwald P, et al. But what about the medical students? Developing a medical school telemedicine curriculum. Poster presented at: ATA 2020 Telehealth Virtual Conference & Expo; June 22–26, 2020.
Ethical Approval
The Weill Cornell Medical College Institutional Review Board approved this study.
References
- 1.Fact sheet: telehealth. American Hospital Association. February 2019. Accessed April 29, 2019. https://www.aha.org/system/files/2019-02/fact-sheet-telehealth-2-4-19.pdf
- 2.Mohr P, Attinson D, Lakhia A. PCORI-funded projects aim to use telehealth to address disparities. Patient-Centered Outcomes Research Institute. July 31, 2018. Accessed April 29, 2019. https://www.pcori.org/blog/pcori-funded-projects-aim-use-telehealth-address-disparities
- 3.Marcin J, Shaikh U, Steinhorn R. Addressing health disparities in rural communities using telehealth. Pediatr Res. 2016;79(1):169–176. 10.1038/pr.2015.192 [DOI] [PubMed] [Google Scholar]
- 4.Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood). 2014;33(2):194–199. 10.1377/hlthaff.2013.0992 [DOI] [PubMed] [Google Scholar]
- 5.Welch BM, Harvey J, O'Connell NS, McElligott JT. Patient preferences for direct-to-consumer telemedicine services: a nationwide survey. BMC Health Serv Res. 2017;17(1):784 10.1186/s12913-017-2744-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rae M, Cox C. More employers are paying for telemedicine, but enrollee take-up has been relatively low. Peterson-KFF Health System Tracker. October 3, 2018. Accessed April 29, 2019. https://www.healthsystemtracker.org/brief/more-employers-are-paying-for-telemedicine-but-enrollee-take-up-has-been-relatively-low/#item-start
- 7.Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375(2):154–161. 10.1056/NEJMra1601705 [DOI] [PubMed] [Google Scholar]
- 8.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585–1592. 10.1056/NEJMsr1503323 [DOI] [PubMed] [Google Scholar]
- 9.Schwamm LH, Chumbler N, Brown E, et al; American Heart Association Advocacy Coordinating Committee. Recommendations for the implementation of telehealth in cardiovascular and stroke care: a policy statement from the American Heart Association. Circulation. 2017;135(7):e24–e44. 10.1161/CIR.0000000000000475 [DOI] [PubMed] [Google Scholar]
- 10.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 11.Telemedicine training proves vital during Covid-19 crisis, increasing access to care. Weill Cornell Medicine. April 9, 2020. Accessed September 20, 2020. https://news.weill.cornell.edu/news/2020/04/telemedicine-training-proves-vital-during-covid-19-crisis-increasing-access-to-care
- 12.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health. 2020;26(5):571–573. 10.1089/tmj.2020.29040.rb [DOI] [PubMed] [Google Scholar]
- 13.Nochomovitz M, Sharma R. Virtual care as a specialty-reply. JAMA. 2018;319(24):2560 10.1001/jama.2018.5674 [DOI] [PubMed] [Google Scholar]
- 14.Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ. 2019;5(1):e12515 10.2196/12515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rutledge CM, Haney T, Bordelon M, Renaud M, Fowler C. Telehealth: preparing advanced practice nurses to address healthcare needs in rural and underserved populations. Int J Nurs Educ Scholarsh. 2014;11(1):1–9. 10.1515/ijnes-2013-0061 [DOI] [PubMed] [Google Scholar]
- 16.AMA encourages telemedicine training for medical students, residents. American Medical Association. June 15, 2016. Accessed April 20, 2019. https://www.ama-assn.org/ama-encourages-telemedicine-training-medical-students-residents
- 17.Sharma R, Nachum S, Davidson KW, Nochomovitz M. It's not just FaceTime: core competencies for the medical virtualist. Int J Emerg Med. 2019;12(1):8 10.1186/s12245-019-0226-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyers LN, Schultz A, Baceviciene R, et al. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health. 2015;21(4):312–314. 10.1089/tmj.2014.0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papanagnou D, Stone D, Chandra S, Watts P, Chang AM, Hollander JE. Integrating telehealth emergency department follow-up visits into residency training. Cureus. 2018;10(4):e2433 10.7759/cureus.2433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baruchin A. Professionalism: a proposed ACGME curriculum in telemedicine for neurology residents. NeurologyToday. 2017;17(16):22–23. 10.1097/01.NT.0000524435.61771.09 [DOI] [Google Scholar]
- 21.Cantone RE, Palmer R, Dodson LG, Biagioli FE. Insomnia telemedicine OSCE (TeleOSCE): a simulated standardized patient video-visit case for clerkship students. MedEdPORTAL. 2019;15:10867 10.15766/mep_2374-8265.10867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pathipati AS, Azad TD, Jethwani K. Telemedical education: training digital natives in telemedicine. J Med Internet Res. 2016;18(7):e193 10.2196/jmir.5534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Step 2 clinical skills. United States Medical Licensing Examination. Accessed June 2, 2020. https://www.usmle.org/step-2-cs/
- 24.Eppich W, Cheng A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc. 2015;10(2):106–115. 10.1097/SIH.0000000000000072 [DOI] [PubMed] [Google Scholar]
- 25.National Clerkship Curriculum: 2nd ed Society of Teachers in Family Medicine; 2018. Accessed June 2, 2020. https://www.stfm.org/media/1828/ncc_2018edition.pdf
- 26.Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Prentice Hall; 1984. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Course Schedules.docx
- Homework Assignment.docx
- Intro Didactic.pptx
- Door Instructions.docx
- SP Intake Simulation.docx
- SP CHF Simulation.docx
- SP UTI Simulation.docx
- SP ETOH Simulation.docx
- Tabletop Exercises.docx
- Tabletop Facilitator Guide.docx
- Homework Debriefing Guide.docx
- Intake Debriefing Guide.docx
- CHF Debriefing Guide.docx
- UTI Debriefing Guide.docx
- ETOH Debriefing Guide.docx
- Prequestionnaire.docx
- Postquestionnaire.docx
All appendices are peer reviewed as integral parts of the Original Publication.