Abstract
Background
Effective promotion of exclusive breast-feeding (EBF) is needed to improve child nutrition and survival.
Objective
We explored barriers and facilitators to EBF in rural Tanzania and assessed parents’ willingness and ability to try specific recommended EBF practices plus strategies for men to support breast-feeding.
Methods
We conducted Trials of Improved Practices in 36 households with infants <6 months. Fathers participated in focus group discussions on ways to support breast-feeding. Fathers and mothers were individually interviewed 2 and 3 times, respectively, about their willingness to try and experience with selected new practices. We analyzed data thematically.
Results
Common barriers to EBF were (1) use of gripe water and traditional medicines for perceived symptoms of infantile distress; (2) mothers’ workloads and time away from infants, limiting availability for EBF; and (3) water given for perceived thirst. Although several mothers expressed concerns about breast-milk insufficiency, few were giving other foods. After counseling, most mothers reported breast-feeding more optimally. Some reported improved breast-milk supply. Fathers saw their roles as providing food to mothers to ensure sufficient breast-milk and encouraging new practices. Dominant gender roles and work away from home were barriers even if fathers were willing to help with household chores. Fathers mostly provided emotional support or encouraged others to help with chores.
Conclusion
Exclusive breast-feeding promotion needs to address concerns about infantile distress and help parents develop effective soothing techniques while avoiding nonprescribed medicines. Engaging men in EBF interventions could help change social norms and facilitate men’s involvement in improving breast-feeding practices.
Keywords: exclusive breast-feeding, Trials of Improved Practices (TIPs), behavior change, fathers, breast-feeding support, Tanzania
Introduction
Breast-feeding is critical to the development and survival of young children and to the well-being of mothers.1 Exclusive breast-feeding (EBF) reduces the risk of infant mortality resulting from diarrhea and lower respiratory infections, 2 major causes of mortality in young children.1 The World Health Organization recommends that for the first 6 months, infants receive only breast- milk without any other foods or drinks, including water, with the exception of medicines prescribed by a doctor or a nurse.2
The Tanzanian government has committed to improving EBF among other infant and young child feeding (IYCF) practices.3 The prevalence of EBF among all infants aged 0 to 6 months in Tanzania improved over the last 3 decades, from 26% in 1991 to 59% in 2015.4 Even in the first month after birth, however, some children are not breast-fed exclusively; reported EBF prevalence is 84% for infants aged 0 to 1 month, 59% for infants aged 2 to 3 months, and 27% of infants aged 4 to 5 months.4 In Tanzania and similar contexts, receipt of breast-feeding education at antenatal and postnatal care visits, place of delivery and general breast-feeding knowledge, together with several nonmodifiable sociodemographic variables such as parity, marital status, level of education, and place of residence, have been identified as influencing EBF behavior.5–8 Furthermore, perceived infant thirst and perception of having insufficient breast-milk have been reported as the most common reasons for disruption of EBF.8,9
Exclusive breast-feeding appears simple: give young infants breast-milk only, with no other foods or drinks. Exclusive breast-feeding is, however, a complex set of behaviors which, in addition to proscriptions, includes recommended practices that enable sufficient breast- milk production. For example, mothers are encouraged to breast-feed on demand and frequently and to allow the baby to finish one breast before offering the other to ensure sufficient breast-milk. These practices take place in the context of social, cultural, and economic environments that influence caregivers’ ability to practice these recommendations. A major challenge, therefore, is developing effective social and behavior change interventions that account for the complexities of EBF.
Using Trials of Improved Practices (TIPs), a qualitative, consultative methodology, we aimed to understand mothers’ and fathers’ willingness to try, use, and sustain recommended practices that promote and support EBF. The TIPs methodology was developed to test IYCF messages in low- income countries by allowing the target audience to actually try the recommendations and provide input from their experiences.10
In this study, we explored the following questions: What are the gaps between knowing about EBF and practicing it? Are women willing and able (measures of acceptability and feasibility, respectively) to adopt recommended EBF practices? Are men willing and able to support women to improve EBF practices? What motivates and challenges parents to adopt recommended strategies? How can challenges be addressed?
Methods
Study Context
This research was conducted in the context of the Addressing Stunting in Tanzania Early (ASTUTE) program, which aims to reduce the prevalence of stunting in 5 Lake Zone regions through changes in practices related to IYCF, water, sanitation, and hygiene and early childhood development. These regions have high prevalence of stunting and anemia and low prevalence of appropriate IYCF practices. This study was part of operations research to identify key facilitators and barriers to optimal IYCF and strategies for overcoming behavioral barriers.
Study Area
Two wards in each of 2 Lake Zone regions were purposively selected to maximize variation in population size, access to health-care facilities, and proximity to the district town center and to the lake. One village was randomly selected within each of the 4 wards.
Study Population
In each of the 4 villages, community health workers (CHWs) identified 13 to 25 mothers with infants aged 0 to 5 months. The research team screened these potential study participants for index child’s age and other demographic variables. Nine mothers were purposively selected to maximize variation in child’s age, parity, mother’s age and educational status, and average time spent away from the index child. Exclusion criteria were mothers <15 years old, not breastfeeding the index child, or not available for follow-up. After mothers consented to participate, their partners were asked to participate as well. To increase the range of perspectives included in initial focus group discussions (FGDs) exploring fathers’ potential roles, additional fathers were recruited to participate just in this component of the study.
Data Collection: TIPs
We visited mothers 3 times over a 16-day period on 2 consecutive days at the beginning plus a follow-up visit after 2 weeks (T1-T3; Table 1). In addition to semi-structured interviews, we conducted 7-day infant-feeding recalls at the first and last visits. Instead of individual interviews at T1, eligible fathers participated in FGDs moderated by male interviewers (Table 2). The FGDs explored gender norms and behaviors around IYCF, identified factors that enable fathers to support improved IYCF practices, and provided guidance for recommendations offered to fathers at T2.
Table 1.
Overview of Data Collection Visits With Mothers in Trials of Improved Practices (TIPs).
| T0—Intake (Day 0) |
T1—Assessment Visit (Day 1), N = 36 |
T2—Counselling Visit (Day 2), N = 36 |
T3—Follow-Up Visit (Day 16), N = 36 |
|
|---|---|---|---|---|
| What are the current feeding practices? What support is received from others? | What would you like to try and change? | Did you try? How did it go? Will you continue? |
||
| Women | • Screening • Demographics • Recruitment • Consenting |
• Dietary recall • Feeding practices • Breast-feeding history • Barriers/Facilitators • Social support • Demographics • Health history |
• Feedback on feeding practices • Counseling on recommended practices and strategies to implement them • Initial response and views on practices/strategies • Willingness to try strategies • Choice of strategy • Anticipated barriers and facilitators • Anticipated social support |
• Dietary recall • Experience with strategies • Strategies modifications • Others’ reactions • Experienced barriers and facilitators • Experienced social support • Adoption of practices |
Table 2.
Overview of Data Collection Visits With Fathers in Trials of Improved Practices (TIPs).
| T0—Intake (Day 0) |
T1—Focus Group Discussion (Day 1), N = 38 |
T2—Counselling Visit (Day 3), N = 30 |
T3—Follow-Up Visit (Day 17), N = 29 |
|
|---|---|---|---|---|
| How are men willing to support mothers? | What would you like to try and change? | Did you try? How did it go? Will you continue? |
||
| Men | • Screening • Demographics • Recruitment • Consenting |
• Focus Group Discussion | • Counseling on supportive strategies • Willingness to try strategies • Choice of strategy • Anticipated barriers and facilitators |
• Experience with strategies • Strategies modifications • Experienced barriers and facilitators • Adoption of practices |
Interviews and FGDs were conducted in Swahili by 3 female and 4 male interviewers who participated in a 10-day training. The interviewers and data collection were supervised by 2 nutritionists. Each participant was interviewed by the same interviewer at all 3 visits. We used standardized semi-structured interview guides (Supplementary Materials A) and debriefed with 2 nutritionists daily. With participant consent, all interviews were audio-recorded.
After each mother’s T1 interview, the interviewer had a debriefing meeting with 1 to 2 supervisors and the father’s interviewer to discuss the mother’s responses and determine which recommendations to offer the mother and father. Recommendations were selected for each family based on problems identified and a counselling guide (Supplementary Materials B) developed prior to the study.
At T2, participants were offered 2 to 8 recommendations (average 4) to improve EBF practices, and the interviewer asked them to select 1 to 2 to try over a 2-week period. Participants regularly selected more than 2 recommendations, often because of overlap of practices needed to support successful EBF. At T3, participants discussed their experiences with selected recommendations. Recommendations offered and selected were tracked as data collection progressed.
Data Analysis
We used Microsoft Excel to enter and analyze quantitative demographic and infant dietary recall data. Interviewers took detailed qualitative notes during T1 and T2 interviews. Later, they listened to their recordings, added to the notes, and translated them into English. A random subsample of notes was reviewed against audio-recordings to ensure all responses were captured accurately. An independent contractor transcribed T3 qualitative interviews verbatim in Swahili, before translating into English. Subsequently, English interview notes and transcripts were qualitatively coded using Atlas.ti version 8 (Scientific Software Development, Berlin, Germany). Data were analyzed using the constant comparative method of grounded theory11 to identify emergent themes around participants’ experiences across all recommendations. Four coders initially coded the same transcripts independently to capture diverse interpretations of the data in creating the codebook and to ensure consistent coding and interpretation of the data.12
Any discrepancies among the coders were resolved through a consensus discussion. Eventually, transcripts were coded by a maximum of 2 coders. Participants’ willingness, selection, actual trial, and willingness to continue practices were quantitatively tallied, based on yes/no responses.10 Frequency tallying allows comparison across recommendations to identify which were most commonly recommended to participants and regarded positively by them.
Ethical Approval
This study was approved by the Cornell University Institutional Review Board and the National Medical Research Institute in Tanzania. Prior to T1, all participants gave written informed consent.
Results
A total of 36 mothers and 30 partners/fathers participated in TIPs. Among the 6 mothers whose partners did not participate, half were not married, and the other half were not living with their partners. An additional 8 fathers participated only in the FGD; neither they nor their partners were invited to participate in individual TIPs interviews. Since recruitment and consent happened a few days before the first TIPs visit, 5 women and 3 men had changed their minds and dropped out when the interviewer arrived for this first TIPs visit, citing religious beliefs and skepticism of interviewers’ intentions. These were, however, replaced by selecting another participant with similar characteristics from the CHW’s list. Of the 36 mothers and 30 fathers who participated in TIPs, 1 father was lost to follow-up at the final visit. Sociodemographic characteristics of households enrolled in TIPs are reported in Table 3.
Table 3.
Sociodemographic Characteristics of Trials of Improved Practices Households.
| Characteristic | N = 36 |
|---|---|
| Mother’s age, years | |
| Mean (SD) | 27 (8.4) |
| Range | 17–45 |
| Mother’s education, n | |
| No education | 6 |
| Some primary education | 11 |
| Completed primary education | 16 |
| Completed secondary education | 3 |
| Mother’s primary employment, n | |
| Not working | 8 |
| Daily wage worker | 0 |
| Work in own farm | 26 |
| Business/shop keeper | 2 |
| Fishing | 0 |
| Father’s age, years | |
| Mean (SD) | 34 (9.7) |
| Range | 20–61 |
| Father’s education, n | |
| No education | 5 |
| Some primary education | 4 |
| Completed primary education | 19 |
| Completed secondary education | 2 |
| Father’s primary employment, n | |
| Not working | 0 |
| Daily wage worker | 1 |
| Work in own farm | 25 |
| Business/shop keeper | 3 |
| Fishing | 1 |
| Marital status, n | |
| Married | 33 |
| Not Married | 3 |
| Number of children (Parity) | |
| Mean (SD) | 4 (2.8) |
| Range | 1–10 |
| Primiparous, n | 8 |
| Multiparous, n | 28 |
| Place of delivery, n | |
| Health facility | 23 |
| Home | 13 |
| Time away from baby, n | |
| 0 hours | 25 |
| >0 hours (Range: 1–5 hours) | 11 |
| Child age, n | |
| <1 month | 8 |
| 1-<2 months | 7 |
| 2-<3 months | 8 |
| 3-<4 months | 7 |
| 4-<5 months | 5 |
| 5-<6 months | 1 |
| Child gender | |
| Female | 18 |
| Male | 18 |
Abbreviation: SD, standard deviation.
Knowledge and Feeding Practices at T1
In Swahili, EBF translates to “feeding mother’s milk only.” At the first visit, 8 of 36 mothers had heard about EBF; most learned about EBF from health workers, one from a CHW and another from her sister-in-law. All these mothers reported that a child has to be exclusively breast-fed for 6 months; most reported that EBF is ideal for growth, good health, or disease prevention.
Eight of 36 infants received only breast-milk in the previous week. Medicines not prescribed by a health worker were the most commonly reported other substances given to infants in our sample (Table 4). Regarding their intentions, 18 mothers planned to introduce other foods at 6 months, while most of the other mothers planned to introduce other foods earlier than 6 months, some as early as 2 months, and a few planned for 7 to 9 months. Mothers often reported infants crying, waking from sleep, and wetting diaper as signals to breast-feed children and said they knew the child was full when he or she stopped sucking and refused to take the breast again or slept.
Table 4.
Mothers’ 7-Day Recall of Infant-Feeding Practices at Visits 1 and 3.
| Food/Liquid | Given at T1, N = 36 | Given at T3, N = 36 |
|---|---|---|
| Plain water | 12 | 1 |
| Cow’s milk | 2 | 0 |
| Porridge | 1 | 0 |
| Other semi-solid foods (sweet potato) | 1 | 0 |
| Gripe water | 16 | 1 |
| Oral traditional medicine | 11 | 2 |
| Other commercial medicines not prescribed by a health worker | 3 | 4 |
| Commercial medicines prescribed by a health worker | 8 | 6 |
| Breast-milk onlya | 8 | 31 |
| Breast-milk, plus nonprescribed medicinesa | 16 | 4 |
| Breast-milk, plus water and/or other foodsb | 12 | 1 |
Could also have been given prescribed medicine.
Could also have been given prescribed and/or nonprescribed medicines.
Barriers to EBF at Tl
Home management of perceived infantile distress
At the first visit, 30 households reported giving babies medicines not prescribed by a health worker. In 5 of these households, fathers, but not their partners, reported their babies were given nonprescribed medicines. Because fathers did not complete a 7-day infant dietary recall, it was unclear when the babies received the medicines in these 5 cases. Gripe water (a nonprescription product marketed as a relief for colic, gas reflux, and other gastrointestinal problems in young children) was the most commonly given medication, followed by traditional medicines. Less frequently, other commercial medicines were given without a health worker prescription, including antibiotics and antihistamines.
Overwhelmingly, gripe water and/or traditional medicines were given to infants to prevent or treat infantile distress viewed as symptomatic of a condition called “mchango” Symptoms that parents associated with mchango included infants’ frequent, excessive or prolonged crying, and perceived abdominal pain. A few mothers reported additional mchango symptoms in the infant’s genital area or head and also difficulty with breathing because of chest pains, for which traditional medicines were administered. In a few cases, traditional medicines were administered topically. Providing gripe water and traditional medicines for mchango was widely accepted in the family and the community.
I give my baby gripe water because of mchango. When I give gripe water, the baby sleeps and stops crying. (Mother of 1 month old; Site 1)
Typically, gripe water was bought without instruction from a health worker, at a local shop. One mother reported that a hospital doctor gave her gripe water to treat mchango, and another mother was advised by a health worker that it is better to treat mchango with gripe water than with traditional medicine. Traditional medicines were usually acquired from or advised by other family members, neighbors, and other local mothers.
Women’s workloads and lack of support from others
Over half of mothers reported that heavy workloads, including, farming, and gardening limited their ability to breast-feed optimally. Long distances between the home and the farm, the physical demands of farm work, and other work requiring long periods of time away from the baby made it particularly challenging to breastfeed frequently, on-demand, or when the baby cried. Some mothers reported that during farm work they left the baby at home in the care of others for several hours at a time. Other mothers brought the baby to the farm with them, but they were unable to take time to breast-feed while farming. Some mothers reported that cooking and fetching water also inhibited breast-feeding.
During the night I don’t breastfeed because I feel tired and sometimes sleepiness can cause me to be unable to breastfeed the baby… (Mother of <1 week old; Site 4)
Only 5 mothers reported that they stopped all activities to breast-feed when needed or took time to breast-feed until the baby was full before continuing work.
At T1, almost half of mothers reported lack of support from fathers to reduce workload and increase time to breast-feed. Over half reported lack of support from other family members. Several mothers indicated a lack of partner support and strained relationships in polygamous marriages and felt that their husbands only supported their other wives.
The baby has a father but on taking care of him, it is like I am alone… fathers do not… want to be responsible for their babies, because you can find one man has many wives.. (Mother 4-month-old; Site 3)
Some mothers reported that child-care support, mainly from family members other than the father, helped them complete other activities. Mothers reported that the baby’s grandparents, aunts, uncles, and siblings, as well as neighbors, helped them by carrying or soothing the baby while they worked. Fathers also provided support for child care, but men’s willingness to do so was sometimes conditional on the baby not crying or the mother and other caregivers being away or sick. Some fathers were resistant to carrying the baby due to societal expectations and their own perceptions of masculinity:
Based on culture … it doesn’t look okay when husbands help their wives. Every man in our society wants to show the manhood. But I personally chose my wife and l do things for her out of love. (Father of 1-month-old; Site 2)
Perceived breast-milk insufficiency
More than a third of mothers were concerned about the sufficiency of their breast-milk, a concern echoed by most partners. Breast-milk insufficiency was a salient theme in 3 of the 4 men’s FGDs.
We do have one problem, and it is not questionable! Our wives have a problem of not having enough milk in their breasts … [so] we are forced to give [babies] porridge … this breastmilk problem is now a common one in our community. (FGD Site 2)
Mothers and fathers often presumed breast- milk was insufficient based on observation of infant behavior or developmental progress, and mothers also interpreted their own physical signs. Infant behavior reported to indicate breast-milk insufficiency included crying, even after having been breast-fed; sucking until the mother feels pain in her breast or becomes tired; struggling to suckle and appearing frustrated; not sleeping well because of perceived hunger; and perceived slow weight gain or poor growth. Signs related to mothers’ self-perceptions included breasts running out of milk; breasts looking skinny; and associating maternal dietary intake with breast- milk supply. Most parents’ concerns related to quantity rather than quality of breastmilk.
In addition to mothers who reported breast- milk insufficiency, some expected that their breast-milk supply would become insufficient and said they would need to start giving infants other food between 2 and 4 months. Some men reported it would be hard for their wives to EBF for 6 months, or for themselves to encourage their wives to do so, if they experienced challenges with breast-milk supply.
Only 9 mothers felt they had enough breast- milk for the infant, although one was concerned that her baby’s growth had slowed and suspected insufficient breast-milk as the reason why. Another mother anticipated giving porridge at 3 months due to low breast-milk supply. Five fathers thought their partners had enough breast-milk.
Other foods and drinks
In spite of concerns about insufficient breast-milk, only 4 infants were given additional “foods” to supplement breast-milk. More often, infants were given water (Table 4). Infants were generally given water for perceived thirst, although other reasons included giving when baby showed interest and to “support” medicine that was provided.
Acceptability and Feasibility of Recommended Practices at T2 and T3
Practices that were offered can be grouped broadly as those aimed at improving EBF practices by: (1) not giving medicines that are not prescribed by a health worker; (2) increasing frequency and duration of breast-feeding; (3)increasing mother’s time for breast-feeding; (4)stopping other “foods/drinks”; and (5) addressing breast problems in mothers.
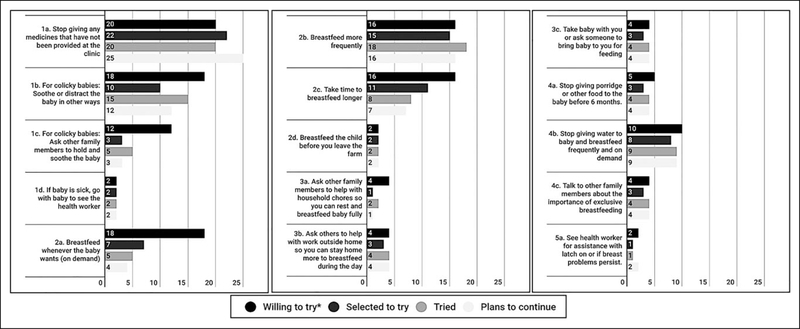
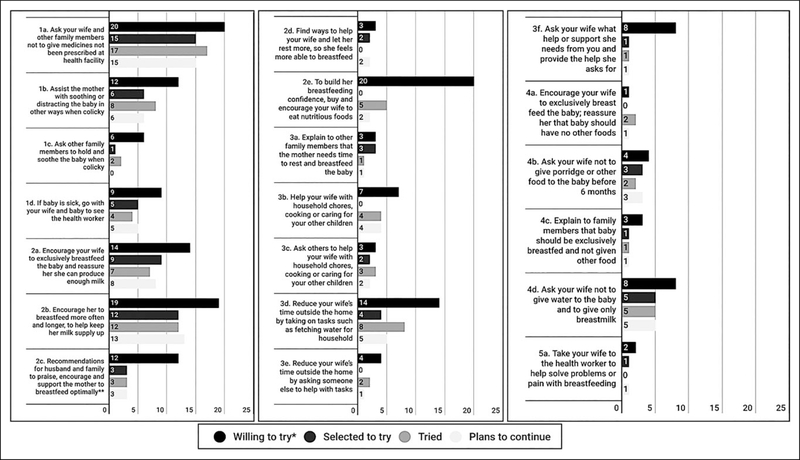
Each participant was offered 2 to 6 practices to try, based on challenges they were experiencing. With very few exceptions, participants were willing to try all practices offered, indicating high acceptability of recommended practices. Participants were, however, encouraged to select a smaller number of practices to actually try. When tallied (Figures 1 and 2), the total number of participants “willing to try” a recommendation included participants who were willing to attempt a new behavior in response to a recommendation and those who were already practicing this behavior.
Figure 1.
Women’s responses to recommended infant feeding practices to improve EBF practices.
* For women, the total number of participants willing to try a recommendation reflects how often the recommendation was offered, since participants did not report willingness to try any practices without prompting, and rarely mentioned that they were not willing to try or were already practicing a recommendation. This considered, shorter bars for willingness do not imply that participants were less willing to try the practice.
Figure 2.
Men’s responses to recommended infant feeding practices to improve EBF practices.
* For men, the total number of participants willing to try a recommendation is a combination of how often the recommendation was offered and how often it was reported as “already practicing”, since participants rarely mentioned that they were not willing to try. This considered, shorter bars for willingness do not imply that participants were less willing to try the practice.
** For men, 2c is an aggregate tally of four recommendations aimed at father and other family members providing mother with emotional support to breastfeed exclusively, on demand and from both breasts.
1. Response to recommendations related to not giving medicines that were not prescribed
Consequent to a large majority of infants being given nonprescribed medicines, recommendations to reduce this practice (1a-1d) were most common suggestions given to mothers and fathers. Mothers rarely selected and/or tried to ask family members to assist them by holding and soothing the baby. Relatedly, fathers primarily selected and reported trying to encourage their wives and other family members not to give the baby nonprescribed medicines and were less likely to select or actually try soothing the baby (although some did so) and much less likely to select asking other family members to help soothe the baby. One father was unwilling to accompany his wife to the clinic if their baby fell ill for reasons centered around gender norms and time availability.
… women are the ones who are responsible to go to the health facility to see health worker when the baby is sick. When the baby is not seriously sick, only my wife can go. The time that we might spend at the hospital is unpredictable. Sometimes we may spend the whole day at the hospital while we are living only two adults, that means that all of the other works at home will not be performed. (Father of 3-month-old; Site 2)
There was a marked decrease in the number of infants given gripe water or traditional medicines for mchango at T3 (Table 4). Only 1 mother reported giving her baby gripe water at T3 and that was because it was prescribed by a health worker.
Although she selected to try the practice, one mother reported that she was unable to stop giving her baby traditional medicine, because she felt doing so would “bring harm” to her child and planned to continue giving medicines as long as the baby had mchango. Another mother tried to not give her baby medicine for mchango but ended up giving both traditional medicine and gripe water because the baby was crying a lot on 2 occasions. In contrast, 2 mothers who were giving gripe water at T1 reported that their babies did not cry or show symptoms of mchango although they stopped giving medicines, which made it easier to continue avoiding gripe water, and was the reason why one did not use soothing techniques to calm the baby.
2. Response to recommendations related to frequency and duration of breast-feeding
Many mothers found it acceptable and feasible to breast-feed more frequently. The proportion of mothers who selected and actually tried breastfeeding more frequently was higher than any other practice. Furthermore, a few mothers reported breast-feeding their infants more frequently at T3, although they were not offered this practice at T2. Two mothers selected but did not try breast-feeding on-demand. Instead, they reported breast-feeding more frequently.
Four mothers categorized as not having tried breast-feeding their infants longer at each feed misinterpreted the recommendation; they took it to mean that the infant should be breast-fed on a schedule. It was not clear from our data whether this misinterpretation was by interviewers or by mothers. Some mothers, however, understood this recommendation.
All but 2 of the recommendations given to men involved providing emotional support to their wives (2a-2e). Many of the fathers opted to try at least 1 recommendation from this group or were already doing the practice. Two men were already encouraging their wives to breast-feed more often and longer, another 2 were already praising their wives for being good mothers, and 1 man was already encouraging his wife to EBF. Four men did not attempt recommendations (to improve frequency and duration of breast-feeding) that they had selected to try. One of these fathers had no intention of trying the recommendation at the time of interview nor in the future. Although his partner reported that she was breastfeeding more frequently at T3, he stated that he had asked her to prioritize other household activities and reduce time for breast-feeding:
I asked her to reduce breastfeeding time so that she can help meet other family needs … [instead] of staying home to look after the baby ‥ On that note we decided to ignore that procedure. (Father of 1- month-old; Site 2)
3. Response to recommendations related to mother’s time for breast-feeding
These recommendations were aimed at reducing mothers’ workloads so that they could have time to breast-feed optimally were offered less frequently to mothers. Generally, mothers who selected and tried these recommendations reported they were feasible and also positively received by other family members.
At T3, one mother had tried asking others to help with work outside the home (3b) although she had not selected to try this recommendation. Another mother was not willing to ask others to help with either domestic chores or other activities because they had their own work.
The recommendation to take the baby to the farm so that the mother could breast-feed was seemingly the most acceptable and feasible recommendation among those who committed to taking the time to breast-feed, for both mothers and fathers.
… I used to leave him for a long time … I [now] go with him and breastfed him whenever he cries. (Mother of 4-month-old; Site 1)
We go to the farm with the baby… when the baby cries she stops and breast-feeds. When the baby gets full we continue with work. (Father of 4-month-old; Site 1)
At T2, almost half of fathers reported that they were already reducing their wives’ time away from the home by helping with tasks such as fetching water and firewood and that their wives spent less or no time at all doing farming. These reports, however, were rarely corroborated by mothers when asked about support for breastfeeding they received from fathers. At T3, more fathers than those who chose the practice at T2 reported that they had helped their wives with fetching water or with farm work, and 2 of these fathers said they asked someone else to help with these activities. All the fathers who were willing to help with household chores, mostly cooking and child care, were either already doing this or reported their willingness spontaneously.
I support my wife by giving her more time to be with our baby. I do all household chores… I am feeling happier… helping my wife so that she can do some light works. (Father of 1-month-old; Site 2)
In the abovementioned case, the wife reported that she did not have any worries and that her husband encouraged her to breast-feed often. AtT3, one father reported that he started helping his wife with child care, although this was not offered to him at T2. His wife didnot say anything to corroborate this.
Yes, I do help her and sometimes I actually have to stay with the baby too … I never used to do it before … when she wants to cook, that can take a long time and therefore I stay with the baby as she does that… The baby is always happy, and also my wife feels happy too … I have actually learned how to carry a baby as I never knew before. (Father of 3mo. old; Site 2)
Among 9 fathers who were offered and were willing to ask their wives what help or support they needed to be able to breast-feed optimally, one was already practicing this recommendation and only one selected and tried the recommendation.
After trying related recommendations, several fathers and mothers perceived women having more time to breast-feed negatively. For example, one father reported that the baby was overfed and there were unmet work needs. Consequently, he and his wife developed a joint schedule so work and child-care activities were shared. Another mother reported her parents did not support increasing time for breast-feeding, as it led to unfinished work.
… they said they cannot come back to find all work not done because of this “feeding mother’s milk only”, or not going to the field just staying home and breastfeeding … [so] when I finish work I breastfeed him. Sometimes my young sisters help me to take care of him but some other time I carry him while doing work. (Mother of 3-month-old; Site 2)
At T3, some mothers reported receiving help with household work from other family members; however, 1 mother’s family was only willing to support “hard activities.”
I personally explained it to my family members and they agreed, although some [family members] may misunderstand and announce to the whole village that you are lazy and you don’t want to do house chores. But some understand and they help. (Mother of 5-month-old; Site 2)
Ultimately, time and resource opportunities enabled families to practice recommendations that reduced women’s workload and increased time for breast-feeding. Several mothers reported positive experiences with recommendation in this group. One mother positively reported she was able to spend more time with the child, and another reported family support gave her hope.
The thing I liked [about trying this recommendation]… for example, yesterday the child was crying my mother told me to stay with child and she went to fetch some water for me, so it gives me hope. (Mother of 2-month-old; Site 1)
4. Response to recommendations related to stopping other foods and liquids
Recommendations to not give infants other “foods or drink” (including plain water, cow’s milk, porridge, and sweet potato; 4a-4d) were not needed as much as other messages. However, the few parents who did report these nonideal practices were offered the recommendations to stop giving foods or drink to infants, and they found these recommendations particularly acceptable and feasible. At T3, no participants reported their infants were given other “foods,” and only 1 infant was given water.
At T2 and without prompting, more than half of the fathers reported they were already practicing the recommendation to purchase nutritious foods for their wife and encourage her to eat well (1 hour) or were willing to do so. This practice was often tied with fathers’ perceptions that the quantity and quality of food is essential for sufficient breast-milk supply. Fathers reported to be provided for mothers included enriched porridge, fish, fruits, vegetables, tea, and sugar.
5. Response to recommendations related to breast problems in mothers
Finally, 3 mothers reported breast problems that made it challenging to breast-feed; 2 had breast pain and the other reported that 1 nipple was blocked so she fed from only 1 breast. She was encouraged and chose to try breast-feeding from both breasts and reported an improvement in milk supply at T3. Both mothers who experienced breast pain cited distance and financial cost as challenges to getting assistance from a health facility. Only 1 mother reported that she did go to the dispensary, where she received advice from the health worker; her husband encouraged her to go.
Cross-Cutting Motivators, Facilitators, and Barriers to Adoption of Recommended Practices
Parents were motivated by the desire to realize optimal growth and health for their young children. Parents also reported observing improved health and accelerated growth as positive outcomes of these practices. Health was often described as when the infant was playful and happy, had a good appearance, and did not get sick frequently. To a lesser extent and citing “brain/mental growth” and intelligence, parents were also motivated by positive impact of breast-feeding on cognitive development.
As a result of trying out the recommendations, several parents, especially mothers, reported the infant slept well and more frequently and that crying was less intense and frequent. These positive outcomes allowed parents more time to focus on chores and other activities without being disturbed. In contrast, some parents reported children continuing to cry even when they tried to soothe them, a challenge that some participants overcame, but made it difficult for a few to avoid giving gripe water.
Several couples reported that as a result of the study, they spoke with their partners about child feeding and that doing so improved their communication, marital relationships, and family dynamics which, in turn, helped mothers practice the recommendations. Many couples reported more “cooperation,” less conflict, and greater joint decision-making related to feeding their child. At T1, one mother was particularly frustrated by the lack of any support from her polygamous husband, but at T3 said that her husband was now more involved with the family, helping with household activities and caring for their child.
I would like to thank you for coming to my house and visiting me. I worked on the recommendations which led to peaceful environment in my household. (Mother of 1-month-old; Site 1)
Another father reported that he was now helping his wife with chores, and she was breastfeeding more frequently: … there is now peace in the family… my wife she was thin but when we started with this process and I started helping her with her duties, she gained weight. She is now more beautiful that is why I am happy with these lessons. My wife is also happy. (Father of <1-week-old; Site 4)
Most participants were willing to attempt and reported trying recommended practices in spite of social and cultural norms. Participants often recounted negative commentary from others in the community but attributed this to their lack of knowledge of optimal feeding practices. Many mothers and fathers believed that if others received the same counseling, they would also be motivated to avoid nonprescribed medicines and support mothers to improve breast-feeding practices to achieve optimal growth and health for their children.
Knowledge and Feeding Practices at T3
Three-quarters of mothers planned to start giving other foods at 6 months, compared to half of mothers at the first visit. Virtually all infants were reported not to have been given any additional foods in the previous week. The exception was one infant who was given water. Ten participants, including 4 fathers, reported increased breast- milk supply and sufficiency for their babies. One mother was given medication by a doctor and encouraged to eat more pulses by a nurse to improve her breast-milk supply but reported that none of these suggestions helped.
Discussion
Global recommendations about breast-feeding should take into account local cultural beliefs, practices, and environments.13 This TIPs study explored mothers’ and fathers’ willingness to try recommended practices to improve EBF, providing program-relevant insights on context-specific barriers to EBF and acceptable and feasible strategies that parents can use to achieve optimal breast-feeding practices. Generally, strategies recommended to overcome barriers to EBF were acceptable and feasible, resulting in improved infant feeding practices and increased time for breast-feeding.
In this rural Tanzanian context, the most common barriers to EBF were the use of nonprescribed medicines and women’s heavy workloads. Parents were particularly concerned about mchango, a condition somewhat similar to infantile colic and most often associated with abdominal pain and excessive crying. Parents cited mchango as the most common reason for use of nonprescribed medicines. Parental concerns about mchango and colic in Tanzania have been reported elsewhere,5,14 although others have not found these concerns to be as salient as in the current study. This finding may be due to regional differences or lack of specific inquiry about mchango and use of nonprescribed medications.
Gripe water and traditional medicines were the most common substances given to alleviate or prevent mchango. Formulations of gripe water often contain bicarbonate of soda and dill, caraway, and spearmint oils as active ingredients that are dissolved in as much as 9% alcohol.15 Gripe water has been banned in the United States due to alcohol in most gripe water brands16 and limited only to formulations without alcohol in other high-income countries. Gripe water formulated with alcohol, however, is still readily available in many countries, including Tanzania, and used by mothers and other caregivers to treat symptoms related to colic,17–20 and mchango, in the case of Tanzania. In the current study, participants’ reports on the efficacy of gripe water were mixed. The soothing effects of alcohol in gripe water can also mask symptoms of other serious illnesses.21 Parents and health workers alike need to be educated on the lack of scientific evidence on the efficacy of gripe water and the potential risk of alcohol in its formulation.
The use of traditional herbal medicines to treat colic-like symptoms has been reported in South Africa and Zimbabwe.17,22 In South Africa, Bland and colleagues reported the use of oral traditional medicines in children <3 months which included remedies for capillary naevus, stomach pains (colic), and inyoni, a condition when an infant was perceived to be vulnerable to “supernatural elements which may cause illness,” specifically a sunken fontanelle and diarrhea, if left untreated.17 Mchango is also believed to have spiritual origin and, consequently, people tend to seek remedies from local traditional healers, as the condition is unresponsive to commercial medicines.23,24 Additionally, mchango, although the Swahili word literally translates to “worms,” is a complex construct that includes a variety of diseases not limited to infantile colic, including infertility, menstrual pains, epileptic fits in young children, and impotence in men.23 This perspective suggests why many parents perceive mchango as a serious condition and strongly desire to protect infants from it, exemplified by the mother in our study who feared that stopping nonprescribed treatment would “bring harm” to her infant.
Most mothers who were giving their infants only breast-milk and nonprescribed medicines reported that they were exclusively breast-feeding and had knowledge on EBF or planned to EBF up to 6 months, suggesting a disconnect between the knowledge mothers have on EBF and how it is translated into everyday practices. A similar phenomenon has been described in Zimbabwe, where “protective feedings” administered to infants for different ailments, including colic, were not considered to be interrupting EBF.22 Both the Zimbabwe study and ours suggest that programs need to tap into parents’ desire to nurture their infants and highlight the natural protective properties of breast-milk. Additionally, parents need to be assured that colic-like symptoms are common and that these typically resolve with age. Parents can comfort and soothe a colicky baby without resorting to nonprescribed medications. Programs can raise consciousness about the importance of being sensitive to how a crying baby can strain family relationships.25
Increasingly, the father’s role in breast-feeding is recognized. Mitchell-Box and Braun suggest that the traditional breast-feeding dyad of mother and infant should be replaced with the breast-feeding triad, which includes the father.26 Although fathers are often regarded as decision makers or influen- cers,27–29 the current study suggests that fathers can be involved directly in supporting and improving EBF behaviors. As noted earlier, caring for a colicky infant can induce maternal feelings of anxiety, guilt, disappointment, and failure.30 With mchango, fathers found it acceptable and feasible to assist their wives by carrying and soothing their fussy or inconsolable infant. This finding contrasts with the social expectation that fathers should not spend much time caring directly for infants. A change in fathers’ willingness to care for their babies can improve mothers’ mental well-being as well as EBF practices.
In many African contexts, parenting is patterned by strongly held traditional and cultural values. Traditional gender roles often dictate mothers’ and fathers’ roles in a family unit, with the fathering role seen as being the head and provider of the household and not very involved in childrearing.31,32 As a result, fathers tend to be excluded or to exclude themselves from child health programs and interventions.33 However, we found that fathers were pleased to be recognized as influential. We engaged participant fathers initially in FGDs that asked them to share their aspirations for their children and then suggest actions a father in a story could take to support his child’s health. The TIPs process offered each individual father a range of options and persuasive messages on how they could contribute to better child health outcomes, so even if recommendations seemed countercultural, men had a choice of how to participate. This and other considerations outlined by Panter-Brick and colleagues33—engaging fathers early on and as individuals rather than an extension of the mother and being flexible with the timing and location of meeting with the fathers—may have enhanced cooperation of fathers in this study. Not all fathers engaged in new practices to support EBF, and there is no way to gauge how long others would maintain new practices, but it was encouraging that some fathers responded positively and there were unexpected benefits for couple communication.
Emotional support can build mothers’ confidence with breast-feeding. However, instrumental support may be at least as important in ensuring that infants are breast-fed exclusively. Mothers reported their workloads made it difficult to breast-feed frequently, on demand and for long periods which ensures babies get both foremilk and hindmilk. This finding is consistent with reports from mothers in Uganda who found it challenging to balance their workloads with EBF.29 By the end of our study, mothers reported more time available for breast-feeding. However, this was often a result of instrumental support provided by others in the household, rather than fathers. Grandmothers and other senior women in the extended family often have dominant advisory and decision-making roles in the care of young children.34,35 In our study, fathers’ workloads and lack of time were salient barriers to supporting mothers with household tasks, and mothers rarely substantiated husbands’ claims to have helped to reduce their workload. Thus, actual practices are unknown. Fathers were more willing and able to support mothers emotionally and to encourage other family members to help the mother with household tasks.
Encouragingly, very few infants were given additional foods, despite mothers’ and fathers’ concerns about the sufficiency of breast-milk. This could reflect success of EBF educational outreach and promotion. Mothers intended to start giving other foods and drinks to their babies before 6 months, as a result of perceived or anticipated breast-milk insufficiency. Because mothers were concerned about their babies’ thirst, a large number of infants were given plain water. After the 2-week trial, a few mothers reported encouraging changes in their breast-milk supply, which highlights the positive potential of targeted lactational support from trained peers or facility- and community-based health workers, especially as this relates to parents’ confidence and perceptions of breast-milk sufficiency.36,37 Fathers commonly reported their role to be the provision of an adequate diet for their wives so that they could produce enough breastmilk. This tendency is likely tied to social norms around gender roles and masculinity, in that men are expected to provider for their families.38,39
Study Limitations
We relied on self-reported infant feeding histories and trial of selected practices. Both infant feeding histories and whether parents tried recommended practices are likely subject to social desirability bias, leading participants to give responses that would be acceptable to data collectors. However, data collectors were trained to build rapport and establish an environment conducive to honest conversation, aided by repeated visits to each household. Our small sample size, although ideal for the qualitative nature of TIPs, does not allow us to generalize about the frequency of additional foods and liquids given to infants. To quantify such data, future research on additional feedings given in the first 6 months should explore non-nutritive feedings, such as gripe water and traditional medicines. Although these findings are not generalizable beyond the Lake Zone of Tanzania, they provide an important contribution to our understanding of how men can support breast-feeding mothers, and how general EBF messages can be contextualized for more effective behavior change. Future TIPs research should also include other key influen- cers in the household, including grandmothers.
Conclusion
This study highlights the multiple challenges mothers face in their efforts to successfully adopt EBF behaviors. It also points to the importance of engaging men and other family members so that they provide more hands-on support and to improve spousal communication and relationship. Our study’s findings are now being used to improve training for CHWs and, in turn, program delivery through specific messages, including:
equipping parents with skills to soothe symptoms of mchango,
giving infants medications only when prescribed by a health worker,
building mothers’ confidence in their breastmilk supply,
reminding parents of the importance of optimal growth and health for their infants,
helping families support mothers to allow more time for breast-feeding, and
building on fathers’ roles by suggesting specific ways they can be involved in EBF.
These strategies were generally acceptable and feasible in this setting. Future research can be used to adapt recommendations to other contexts.
Supplementary Material
Acknowledgments
We are grateful for the support provided by the Tanzanian Government, through the Ministry of Health Community Development, Gender, Elderly and Children. We are also thankful for the research team, including research assistants and community health workers, for their hard work and dedication. Finally, we thank the communities in the Lake Zone regions, where this work was conducted, for welcoming us, and especially the study participants for sharing their experiences with us.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by UK Aid from the UK government, through the Addressing Stunting in Tanzania Early (ASTUTE) program.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Victora CG, Bahl R, Barros AJ, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016; 387(10017):475–490. [DOI] [PubMed] [Google Scholar]
- 2.WHO/UNICEF. Infant and Young Child Feeding: Global Strategy in Infant and Young Child Feeding Geneva: WHO; 2003. [Google Scholar]
- 3.Tanzania Food and Nutrition Center (TFNC). National Guidelines on Infant and Young Child Feeding Dar-es-Salaam, Tanzania: TFNC; 2013. [Google Scholar]
- 4.Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015–16 Dar es Salaam, Tanzania; Rockville, MD: MoHCDGEC, MoH, NBS, OCGS, and ICF; 2016. [Google Scholar]
- 5.Maonga AR, Mahande MJ, Damian DJ, Msuya SE. Factors affecting exclusive breastfeeding among women in Muheza District Tanga northeastern Tanzania: a mixed method community based study. Matern Child Health J. 2016;20(1):77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mgongo M, Mosha MV, Uriyo JG, Msuya SE, Stray-Pedersen B. Prevalence and predictors of exclusive breastfeeding among women in Kilimanjaro region, Northern Tanzania: a population based cross-sectional study. Int Breastfeed J. 2013;8(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nkala TE, Msuya SE. Prevalence and predictors of exclusive breastfeeding among women in Kigoma region, Western Tanzania: a community based cross-sectional study. Int Breastfeed J. 2011;6(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shirima R, Gebre-Medhin M, Greiner T. Information and socioeconomic factors associated with early breastfeeding practices in rural and urban Morogoro, Tanzania. Acta Paediatrica. 2001; 90(8):936–942. [PubMed] [Google Scholar]
- 9.Mgongo M, Hussein TH, Stray-Pedersen B, Van- gen S, Msuya SE, Wandel M. “We give water or porridge, but we don’t really know what the child wants:” a qualitative study on women’s perceptions and practices regarding exclusive breastfeeding in Kilimanjaro region, Tanzania. BMC Pregnancy Childb. 2018;18(1):323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickin K, Griffiths M, Piwoz E. Designing by Dialogue: A Program Planner’s Guide to Consultative Research for Improving Young Children Feeding Washington, DC: US Agency for International Development, Bureau for Africa, Office of Sustainable Development; 1997. [Google Scholar]
- 11.Corbin J, Strauss AL. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory Thousand Oaks, CA: Sage; 2008. [Google Scholar]
- 12.Creswell JW. Qualitative Inquiry and Research Design: Choosing Among Five Approaches 3rd ed. Thousand Oaks, CA: Sage; 2013. [Google Scholar]
- 13.Pelto GH, Martin SL, Liere MJ, Fabrizio CS. Perspectives and reflections on the practice of behaviour change communication for infant and young child feeding. Matern Child Nutr. 2016;12(2): 245–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leshabari SC, Koniz-Booher P, Astrom AN, de Paoli MM, Moland KM. Translating global recommendations on HIV and infant feeding to the local context: the development of culturally sensitive counselling tools in the Kilimanjaro Region, Tanzania. Implement Sci. 2006;1(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adhisivam B Is gripe water baby-friendly? J Pharmacol Pharmacother. 2012;3(2):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blumenthal I The gripe water story. JR Soc Med. 2000;93(4):172–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bland RM, Rollins NC, Broeck JVD, Coovadia HM. The use of non-prescribed medication in the first 3 months of life in rural South Africa. Trop Med Int Health. 2004;9(1):118–124. [DOI] [PubMed] [Google Scholar]
- 18.Jain K, GunaSeKaran D, VenKateSh C, SounDar- araJan P. Gripe water administration in infants 1–6 months of age-A cross-sectional study. J Clin Diagn Res. 2015;9(11):SC06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oshikoya KA, Senbanjo IO, Njokanma OF. Selfmedication for infants with colic in Lagos, Nigeria. BMC Pediatr. 2009;9(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aborigo RA, Moyer CA, Rominski S, et al. Infant nutrition in the first seven days of life in rural northern Ghana. BMC Pregnancy Childb. 2012; 12(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akkamamba B, Reddy NS. Impact of health education on the knowledge of mothers on newborn care practices- a study done in a tertiary care center. Journal of Evolution of Medical and Dental Sciences. 2017;6(82):5778–5782. [Google Scholar]
- 22.Desai A, Mbuya MNN, Chigumira A, et al. Traditional oral remedies and perceived breast milk insufficiency are major barriers to exclusive breastfeeding in rural Zimbabwe. J nutr. 2014; 144(7):1113–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen DR. Managing Motherhood, Managing Risk: Fertility and Danger in West Central Tanzania Ann Arbor: University of Michigan Press; 2004. [Google Scholar]
- 24.Oberlander L, Elverdan B. Malaria in the United republic of Tanzania: cultural considerations and health-seeking behaviour. Bull World Health Organ. 2000;78(11):1352–1357. [PMC free article] [PubMed] [Google Scholar]
- 25.Barr RG. The normal crying curve: what do we really know? Dev Med Child Neurol. 1990;32(4): 356–362. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell-Box K, Braun KL. Fathers’ thoughts on breastfeeding and implications for a theory-based intervention. J Obstet Gynecol Neonatal Nurs. 2012;41(6): E41–E50. [DOI] [PubMed] [Google Scholar]
- 27.Chary AN, Messmer SE, Rohloff PJ. Male influence on infant feeding in rural Guatemala and implications for child nutrition interventions. Breastfeed Med. 2011;6(4):227–231. [DOI] [PubMed] [Google Scholar]
- 28.Dearden KA, Quan LN, Do M, et al. Work outside the home is the primary barrier to exclusive breastfeeding in rural Viet Nam: insights from mothers who exclusively breastfed and worked. Food Nutr Bull. 2002;23(suppl 4):99–106. [PubMed] [Google Scholar]
- 29.Engebretsen IM, Moland KM, Nankunda J, Kara- magi CA, Tylleskar T, Tumwine JK. Gendered perceptions on infant feeding in Eastern Uganda: continued need for exclusive breastfeeding support. Int Breastfeed J. 2010;5(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Long T, Johnson M. Living and coping with excessive infantile crying. J Adv Nurs. 2001;34(2): 155–162. [DOI] [PubMed] [Google Scholar]
- 31.Amos PM. Parenting and culture-evidence from some African communities In: Parenting in South American and African contexts. InTech; 2013. [Google Scholar]
- 32.Ejuu G Celebrating African men’s role in child care and early childhood development programs. Childhood Educ. 2016;92(1):29–35. [Google Scholar]
- 33.Panter-Brick C, Burgess A, Eggerman M, McAllister F, Pruett K, Leckman JF. Practitioner review: engaging fathers-recommendations for a game change in parenting interventions based on a systematic review of the global evidence. J Child Psychol Psyc. 2014;55(11):1187–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kerr RB, Dakishoni L, Shumba L, Msachi R, Chirwa M. “We grandmothers know plenty”: breastfeeding, complementary feeding and the multifaceted role of grandmothers in Malawi. Soc Sci Med. 2008;66(5):1095–1105. [DOI] [PubMed] [Google Scholar]
- 35.Aubel J The role and influence of grandmothers on child nutrition: culturally designated advisors and caregivers. Matern Child Nutr. 2012;8(1): 19–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database Syst Rev. 2007;2007(1): CD001141. [DOI] [PubMed] [Google Scholar]
- 37.Tylleskar T, Jackson D, Meda N, et al. Exclusive breastfeeding promotion by peer counsellors in sub-Saharan Africa (PROMISE-EBF): a clusterrandomised trial. Lancet. 2011;378(9789):420–427. [DOI] [PubMed] [Google Scholar]
- 38.Richter L, Morrell R. Fathering: the role of men in raising children in Africa—holding up the other half of the sky In: Africa’s Future, Africa’s Challenge: Early Childhood Care and Development in sub-Saharan Africa. Washington, DC: The World Bank Location; 2008. [Google Scholar]
- 39.Mbekenga CK, Lugina HI, Christensson K, Olsson P. Postpartum experiences of first-time fathers in a Tanzanian suburb: a qualitative interview study. Midwifery. 2011;27(2):174–180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.