Abstract
Background.
U.S. research examining the illicit drug supply remain rare even though the information could help reduce overdoses. Relatively little is known regarding how often opioids are found in stimulants and whether temporal and geographic trends exist. We examined trends in fentanyl-cocaine and fentanyl-methampheatmine combinations in the national illicit drug supply.
Methods.
We analysed serial cross-sectional data from the National Forensic Laboratory Information System (NFLIS) collected between January 2011 and December 2016. We restricted the analysis to cocaine (N=1,389,968) and methamphetamine (n=1,407,474) samples and calculated proportions containing fentanyl (including 23 related analogs) over time.
Results.
The combined presence of fentanyl and cocaine steadily increased nationally between 2012-2016 (p=0.01), and the number of such samples tripled from 2015-2016 (n=423 to n=1,325). Similarly, the combined presence of fentanyl and methamphetamine increased 179% from 2015-2016 (n=82 to n=272). Patterns varied widely by state; in2016, fentanyl-cocaine samples were most common in New Hampshire (7.2%), Connecticut (5.4%), Ohio (2.6%) and Massachusetts (2.1%), whereas fentanyl-methamphetamine samples were most often in New Hampshire (6.1%), Massachusetts (5.6%), Vermont (2.4%) and Maine (1.2%).
Conclusions.
Although relatively uncommon, the presence of fentanyl in the stimulant supply increased significantly between 2011 and 2016, with the greatest increases occuring between 2015 to 2016; the presence of these products were concentrated in the U.S. Northeast. Given these trends, strengthening community-based drug checking programs and surveillance within the public health infrastructure could help promote timely responses to novel threats posed by rapid shifts in the drug supply that may lead to inadvertent exposures.
Keywords: substance use, overdose, opioids, fentanyl, stimulants
1. BACKGROUND
Despite the concerted efforts of many stakeholders, the opioid epidemic continues to result in enormous morbidity and mortality in the U.S., with 67,367 drug overdose deaths occurring in 2018, the majority involving opioids (Hedegaard et al., 2020). While overdoses in previous decades were largely attributable to prescription opioids and heroin, fentanyl now drives the majority of deaths (Ciccarone, 2017; O’Donnell et al., 2018). Between 2013 and 2018, deaths involving fentanyl and other similar synthetic opioids rose by tenfold (Hedegaard et al., 2020).
Less acknowledged is the role of stimulants in opioid deaths even though co-use of opioids and stimulants (e.g., ‘speedball’) elevate overdose risk (Jones et al., 2020; Martins et al., 2015). In the first half of 2018, many fentanyl deaths co-involved cocaine (40%) and methamphetamine (11%) (Gladden et al., 2019; Jones et al., 2020). National overdose mortality co-involving stimulants and synthetic opioids rose more than 30% from 2016 to 2017 across all age and sex groups (Kariisa et al., 2019). These trends are corroborated by a national toxicology study, which showed that emergency room visits involving cocaine with synthetic opioids increased by 9% between 2016 to 2017 (Hoots et al., 2020). These trends pose a substantial public health challenge given that interventions for stimulant use disorder and overdose remain underdeveloped (Gladden et al., 2019).
Polysubstance use is a common overdose risk factor among people who use drugs (PWUD) (Al-Tayyib et al., 2017; Connor et al., 2014; Park et al., 2018; Schneider et al., 2020). According to data from 2015 to 2017, methamphetamine use tripled from 9% to 30% among those reporting recent heroin use (Ellis et al., 2018; Strickland et al., 2019). The association between speedball use and overdose is established (Coffin et al., 2003; Darke et al., 2005; Seal et al., 2001). These data provide insights to the role of stimulants in the opioid epidemic, but leave several questions unanswered. For example, it is not clear whether morbidity and mortality trends are virtually all due to polysubstance use, or if accidental exposure to mixed or contaminated drugs is playing a substantial role (Amlani et al., 2015; Green and Gilbert, 2016). Research suggests that there may be a discordant relationship between perceived and actual fentanyl exposure (Armenian et al., 2019; Kenney et al., 2018) given that PWUD typically rely on subjective assessments and word-of-mouth to determine the contents of their illicitly-obtained drugs (Carroll et al., 2017; Mars et al., 2018a, b; Park et al., 2018; Rouhani et al., 2019). Elucidating the drug supply could inform public health interventions, and ultimately save lives.
As a starting point, information is needed regarding the extent to which opioids and stimulants are combined in the drug supply. We addressed this question using data from the U.S. Drug Enforcement Administration (DEA) National Forensic Information Laboratory System (NFLIS), a data repository that aggregates drug chemistry results of samples collected by the criminal justice system across all states and territories. According to the CDC, levels of fentanyl seizures have been shown to be correlated with synthetic opioid deaths, demonstrating the predictive potential of this underutilized data source (Gladden et al., 2016). We focused on examining the proportion of stimulants that contained fentanyl and fentanyl analogs (FFA), and how the combined presence of FFA and stimulants varied across states and by time, as well as their relation to overdose.
2. METHODS
2.1. NFLIS Data
A Freedom of Information Act (FOIA) was used to obtain drug seizure information from NFLIS (2011-2016); the methods are described elsewhere (Zoorob, 2019). The full dataset is available at https://dataverse.harvard.edu/dataset.xhtml?persistentId=doi:10.7910/DVN/B3GUAE. Readers may contact the corresponding author for further details on the FOIA process. The NFLIS is the most comprehensive database available on the U.S. illicit drug supply and includes drug chemistry data from all criminal cases requiring drug testing for prosecution. This includes personal drug possession cases as well as large seizures. Jurisdictions report data to NFLIS at the sample level or in aggregate by month; some states report both. In addition to information about the state/territory and date of the seizure, the NFLIS also contains information regarding overall sample weight, purity, and up to eight substances detected per seizure though there is substantial missingness.
2.2. Vital Statistics Data
We extracted 2016 vital statistics data denoting the national rank in age-adjusted opioid overdose rates of each state from the National Center for Health Statistics for comparison to the NFLIS trends.
2.3. Analysis
Our primary interest was in modeling the physical presence of FFA in cocaine and methamphetamine samples. To do so, for states reporting aggregate-1 eve I seizure records, we expanded the rows based on the number of samples to create a dataset that has one sample per row, similar to the structure of the individual sample-level dataset. FFA such as acetyl-fentanyl and furanyl fentanyl were combined into the “FFA” category. The full range of FFA in the dataset were identified based on a public DEA report (NFLIS Public Resource Library) and are listed in eTable1 Cocaine and Methamphetamine were analyzed as labeled.
eTable 1:
List of fentanyl analogs included in the analysis
| Fentanyl analogs |
|---|
| 3-Methylfentany |
| 3-Methylfentanyl |
| 4-Fluoroisobutyryl fentanyl |
| 4-methoxy-butyryl fentanyl |
| Acetyl fentanyl |
| Acetyl-alpha-methylfentanyl |
| Acryl fentanyl |
| Alpha-methylfentanyl |
| ANPP |
| Butyryl fentanyl |
| Carfentanil |
| cis-3-methylfentanyl |
| Fluorofentanyl |
| Fluoroisobutyryl fentanyl |
| Furanyl fentanyl |
| o-Fluorofentanyl |
| p-Fluorobutyryl fentanyl |
| P-Fluorofentanyl |
| Remifentanil |
| β hydroxythiofentanyl |
| Tetrahydrofuranfentanyl |
| trans-3 Methylfentanyl |
| Valeryl fentanyl |
The total proportion of cocaine and methamphetamine samples also containing Fentanyl were tabulated by state/territory and year. Trends over time were assessed using the Mann-Kendall non-parametric trend test. Lastly, Spearman’s rank-order correlations were used to assess the correlation between the ranked list of states by each outcome and the state’s rank in drug overdose rates. P-values < 0.05 indicated statistical significance.
3. RESULTS
Our analytic dataset contained 9,861,156 drug seizure records and was subsequently restricted to samples containing cocaine (n=1,389,968) or methamphetamine (n=1,407,474). Table 1 depicts the number and proportion of stimulant samples containing FFA and by state where such samples were detected. Figure 1 depicts state-level trends in the number of such samples detected by year.
Table 1.
Proportion of cocaine and methamphetamine law enforcement seizure samples containing fentanyl or fentanyl analogues in the United States using data from the National Forensic Laboratory Information System (NFLIS), 2011-2016.
| 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | Drug overdose mortality ranking, 2016* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| States | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Cocaine (n=1,389,968 samples) | |||||||||||||
| All states | 2 | 0.0 | 2 | 0.0 | 17 | 0.0 | 155 | 0.1 | 423 | 0.2 | 1,325 | 0.6 | -- |
| New Hampshire | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 9 | 1.3 | 44 | 6.3 | 62 | 7.2 | 3 |
| Connecticut | 0 | 0.0 | 0 | 0.0 | 1 | 0.3 | 1 | 0.3 | 3 | 0.7 | 22 | 5.4 | 11 |
| Ohio^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 96 | 0.6 | 189 | 1.1 | 548 | 2.6 | 2 |
| Massachusetts^ | 2 | 0.0 | 0 | 0.0 | 1 | 0.0 | 18 | 0.2 | 55 | 0.8 | 169 | 2.1 | 7 |
| Kentucky | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 33 | 1.1 | 55 | 1.9 | 5 |
| Maine | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 5 | 1.6 | 10 |
| Virgin^ | 0 | 0.0 | 0 | 0.0 | 12 | 0.1 | 10 | 0.1 | 27 | 0.3 | 114 | 1.5 | 32 |
| Vermont | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.4 | 3 | 1.1 | 2 | 1.0 | 20 |
| Pennsylvan^ | 0 | 0.0 | 1 | 0.0 | 4 | 0.0 | 1 | 0.0 | 19 | 0.2 | 90 | 0.7 | 4 |
| Florida^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 6 | 0.0 | 25 | 0.1 | 136 | 0.7 | 16 |
| Methamphetamine (n=1,407,474 samples) | |||||||||||||
| All states | 3 | 0.0 | 1 | 0.0 | 3 | 0.0 | 14 | 0.0 | 82 | 0.0 | 272 | 0.1 | -- |
| New Hampshire | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.1 | 18 | 6.4 | 28 | 6.1 | 3 |
| Massachusetts^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.6 | 15 | 9.4 | 13 | 5.6 | 7 |
| Vermont | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 2.4 | 20 |
| Maine | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 1.2 | 10 |
| Maryland^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 1.0 | 6 |
| Ohio^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 0.1 | 19 | 0.3 | 72 | 0.9 | 2 |
| Pennsylvan^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 0.1 | 20 | 0.7 | 4 |
| New Jersey^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 0.6 | 0 | 0.0 | 4 | 0.6 | 18 |
| Kentucky | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 4 | 0.1 | 30 | 0.3 | 5 |
| Virgin^ | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.0 | 1 | 0.0 | 11 | 0.2 | 32 |
Note: Values in cells represent total number of seized samples per state per year (N) and the proportion of these samples testing positive for fentanyl or a fentanyl analogue (%); top ten states based on 2016 proportions are depicted.
Data are from the Multiple Cause of Death Files, 1999-2018, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10.html on February 13, 2020.
Data reported to NFLIS at sample level
Figure 1:
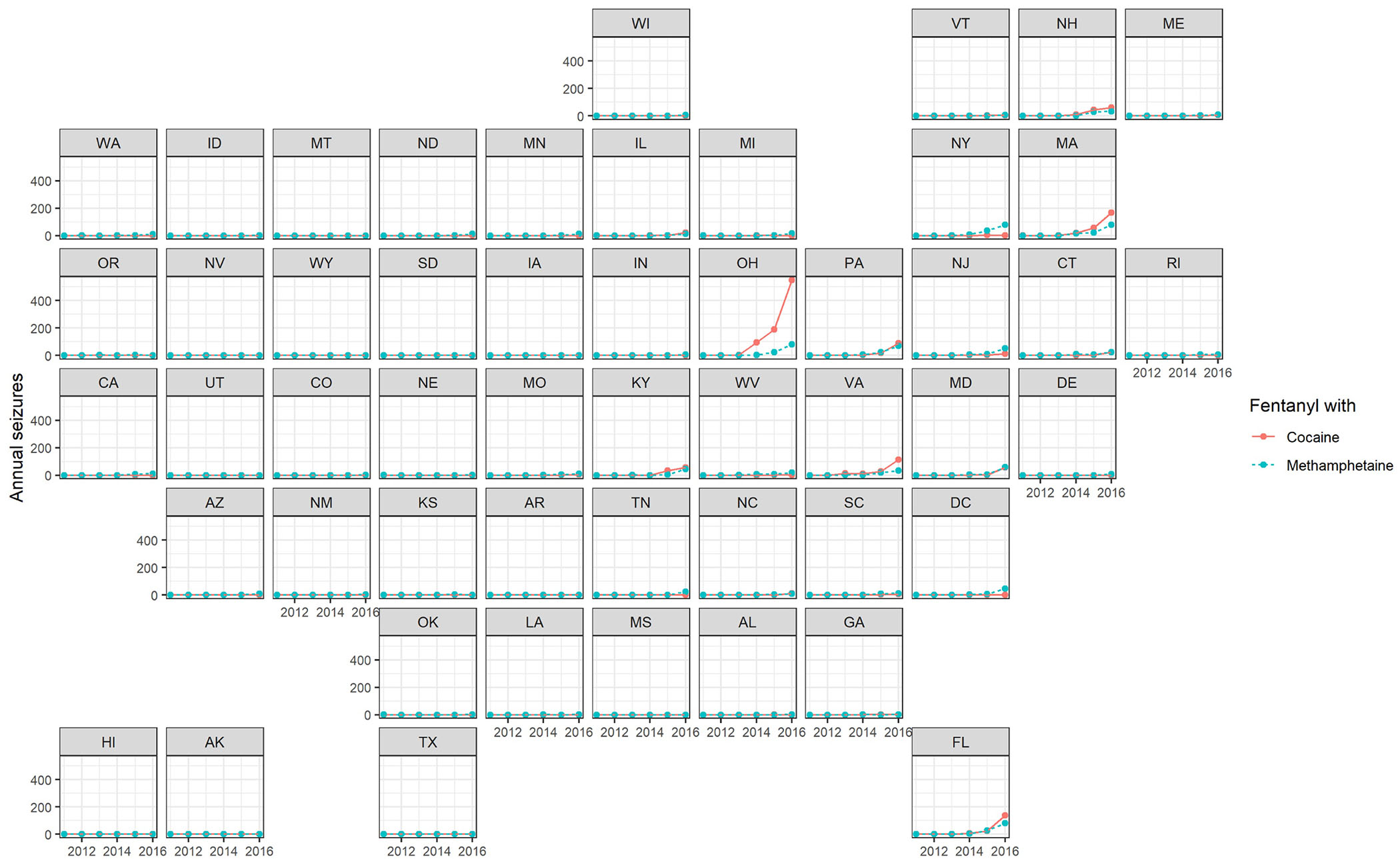
Fentanyl-Stimulant Seizures in the the National Forensic Laboratory Information System (NFLIS), 2011-2016
Between 2011 and 2013, few cocaine samples in any state contained detectable FFA, whereas between 2014 and 2016, increasing FFA within the cocaine seizures was noted, reaching approximately 0.6% (ISM,325) of all cocaine seizures by 2016. There was a statistically significant non-parametric trend for the FFA in cocaine seizures over time (p=0.01). A small proportion of states accounted for the majority of such samples (7 states accounted for 88.6% of FFA-cocaine seizures in 2016), led by New Hampshire (7.2% of cocaine samples containing FFA), Connecticut (5.4%), Ohio (2.6%) and Massachusetts (2.1%).
Similar patterns were observed when examining seized samples of methamphetamine, although overall rates of contamination were lower. For example, in 2016, across all states, 0.1% of seized methamphetamine samples contained FFA, and four states exceed 1% of samples with such mixing in 2016. The temporal trend of FFA/methamphetamine seizures was of borderline statistical significance (p = 0.06).
There was a moderate state-level correlation between the overall prevalence of FFA in stimulants and age-adjusted opioid overdose mortality rates (rcocaine=0.46; rmethamphetamine=0.46). For example, although Florida and Virginia were placed in the top ten in the nation for FFA-cocaine prevalence, they ranked 25th and 26th in the country respectively in opioid overdose mortality (see Table 1).
4. DISCUSSION
Despite gains in addressing the opioid epidemic (Hedegaard et al., 2020), enormous ramifications continue to accrue, and the COVID-19 pandemic has introduced further concerns (Alexander et al., 2020; Wakeman et al., 2020). In this analysis, we examined one important component of the opioid epidemic as it has continued to evolve – the physical combination of FFA with cocaine and methamphetamine. The co-presence of FFA increased significantly between 2011 and 2016, and all indications suggest that the increases may be accelerating in some states. In addition, the presence of FFA in cocaine tended to be concentrated in states that have been disproportionately impacted by fentanyl. These findings are important because of the continued availability, and persistent lethality, of FFA, as well as the dynamic nature of use patterns among PWUD. While our study was not designed to assess the degree to which these findings are an artifact of drug preparation or polysubstance use, these findings underscore the importance of reaching stimulant users through overdose prevention and response initiatives, particularly in states where the combination of fentanyl and stimulants is more widespread.
The geographic variability of the drug combinations that we found is noteworthy, and consistent with prior work examining the distribution of FFA across the U.S. (Hedegaard et al., 2019; Zoorob, 2019). Our findings also corroborate results from Ohio, where the presence of fentanyl/carfentanyl doubled in both cocaine and methamphetamine samples from between 2016 and 2017; these combinations were more common in smaller seizures (i.e., at the personal possession level), posing a risk of overdose to PWUD. We found that FFA was less commonly physically combined with methamphetamine than cocaine. This may be in part due to the ease in which the substances can be combined, given that both fentanyl and cocaine are often sold as white powders particularly in the Northeast and Midwest, compared to methamphetamine, which is often available as pressed pills or crystals.
Our findings also add to a growing literature characterizing the vast and changing illicit drug supply, and they complement national trends reported by the DEA with state-level detail (U.S. Drug Enforcement Administration, 2018). We also found only a small correlation between overdose trends and the physical presence of FFA in stimulants. As such, our data demonstrate that monitoring trends at state and local levels is required to enhance overdose prevention efforts; such information is likely to be of value to PWUD, healthcare professionals and outreach workers.
These findings are subject to limitations. Whether the presence of FFA in stimulants contribute to accidental overdose will need to be further examined. There are inherent issues (e.g., validity, missing data, timeliness, ethics) to relying on NFLIS data; states vary in the breadth of chemicals tested and instruments used. We also noted high levels of missing data (e.g., purity), which would be useful for developing health messages. The NFLIS albeit comprehensive may provide a biased representation of the drug supply given that the data originate from criminal cases; the majority of seized drugs are not analyzed, and drug criminalization laws disproportionately target low-income communities of color (Alexander, 2012; Cooper, 2015; Park et al., 2020a). In light of these challenges, as well as the harms associated with criminalizing PWUD and the ethics of relying on such data, there have been calls to strengthen public health systems to monitor the drug supply (Green et al., 2020; Palamar et al., 2020; Sherman et al., 2019).
Community-based drug checking programs (DCP) should be implemented to provide real-time information, in addition to other evidence-based harm reduction and treatment services, including overdose prevention sites and opioid agonist treatment (Park et al., 2020b). DCP permit PWUD to submit drugs for rapid chemical analysis and are effective in alerting communities of lethal combinations and novel toxic substances to encourage the adoption of safety behaviors (Barratt et al., 2018; Green et al., 2020; Harper et al., 2017; Tupper et al., 2018). While DCPs are established in Europe and Canada, it is a relatively new endeavor in the U.S. even though these programs are shown to be accepted among PWUD (Sherman et al., 2019) and service providers (Glick, 2018) and could facilitate service engagement and encourage the development of a safer drug supply. Building a new national drug surveillance system tailored for public health, consisting of a coordinated network of high-precision DCP with standardized testing and reporting could help to minimize heterogenity. Modifications to the Controlled Substances Act will be necessary, which currently impedes community-based collection of drug samples. The funding of implementation research and data sharing initiatives will also be critical in maximizing effectiveness.
CONCLUSION
As the overdose crisis continues to evolve, abatement strategies must follow suit. Our findings demonstrate that close and ongoing monitoring of the drug supply could help reduce the risks posed by the evolving drug supply. The integration of DCP and surveillance activities within the public health infrastructure could help promote timely responses to novel threats. While this analysis focused on physical combination of fentanyl with stimulants, such investments may have benefits beyond this particular instance by supporting the expansion of data-driven approaches to overdose reduction.
Highlights.
Fentanyl-stimulant combinations increased between 2015 and 2016 in the U.S.
The number and proportion of fentanyl-stimulant combinations varied by region
Subpopulations of stimulant users may benefit from overdose prevention interventions
Acknowledgments
Author disclosures
Dr. Park has served as a consultant to the Maryland Opioid Operational Command Center and the Delaware Department of Health and Social Services through funding from the Bloomberg American Health Initiative. Dr. Sherman is an expert witness for plaintiffs in opioid litigation. Dr. Alexander is past Chair of FDA’s Peripheral and Central Nervous System Advisory Committee; has served as a paid advisor to IQVIA; is a co-founding Principal and equity holder in Monument Analytics, a health care consultancy whose clients include the life sciences industry as well as plaintiffs in opioid litigation; and is a member of OptumRx’s National P&T Committee. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. ER, KF and MZ have no disclosures to declare.
Funding
Dr. Park is supported in part by a Faculty Development Award from the Johns Hopkins University Center for AIDS Research (1P30AI094189). Michael acknowledges support from the James M. and Cathleen D. Stone PhD Scholarship in Inequality and Wealth Concentration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None to declare.
REFERENCES
- Al-Tayyib A, Koester S, Langegger S, Raville L, 2017. Heroin and Methamphetamine Injection: An Emerging Drug Use Pattern. Subst Use Misuse 52(8), 1051–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GC, Stoller KB, Haffajee RL, Saloner B, 2020. An Epidemic in the Midst of a Pandemic: Opioid Use Disorder and COVID-19. Ann Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander M, 2012. The new Jim Crow: Mass incarceration in the age of colorblindness. The New Press. [Google Scholar]
- Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA, 2015. Why the FUSS (Fentanyl Urine Screen Study)? A cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduct J 12, 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armenian P, Whitman JD, Badea A, Johnson W, Drake C, Dhillon SS, Rivera M, Brandehoff N, Lynch KL, 2019. Notes from the Field: Unintentional Fentanyl Overdoses Among Persons Who Thought They Were Snorting Cocaine - Fresno, California, January 7, 2019. MMWR Morb Mortal Wkly Rep 68(31), 687–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barratt MJ, Kowalski M, Maier LJ, Ritter A, 2018. Global review of drug checking services operating in 2017, Drug Policy Modelling Program Bulletin. National Drug and Alcohol Research Center, UNSW, Sydney, Australia. [Google Scholar]
- Carroll JJ, Marshall BDL, Rich JD, Green TC, 2017. Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: A mixed methods study. Int J Drug Policy 46, 136–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, 2017. Fentanyl in the US heroin supply: A rapidly changing risk environment. Int J Drug Policy 46, 107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K, 2003. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction 98(6), 739–747. [DOI] [PubMed] [Google Scholar]
- Connor JP, Gullo MJ, White A, Kelly AB, 2014. Polysubstance use: diagnostic challenges, patterns of use and health. Current opinion in psychiatry 27(4), 269–275. [DOI] [PubMed] [Google Scholar]
- Cooper HL, 2015. War on drugs policing and police brutality. Substance Use & Misuse 50(8–9), 1188–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Darke S, Williamson A, Darke S, Williamson A, Ross J, Darke S, Williamson A, Ross J, Teesson M, 2005. Non-fatal heroin overdose, treatment exposure and client characteristics: findings from the Australian treatment outcome study (ATOS). Drug and Alcohol Review 24(5), 425–432. [DOI] [PubMed] [Google Scholar]
- Ellis MS, Kasper ZA, Cicero TJ, 2018. Twin epidemics: The surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend 193, 14–20. [DOI] [PubMed] [Google Scholar]
- Gladden RM, Martinez P, Seth P, 2016. Fentanyl Law Enforcement Submissions and Increases in Synthetic Opioid-Involved Overdose Deaths - 27 States, 2013-2014. MMWR Morb Mortal Wkly Rep 65(33), 837–843. [DOI] [PubMed] [Google Scholar]
- Gladden RM, O’Donnell J, Mattson CL, Seth P, 2019. Changes in Opioid-Involved Overdose Deaths by Opioid Type and Presence of Benzodiazepines, Cocaine, and Methamphetamine - 25 States, July-December 2017 to January-June 2018. MMWR Morb Mortal Wkly Rep 68(34), 737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick J, Christensen T, Park JN, McKenzie M, Green TC, Sherman SG, 2018. Stakeholder Perspectives on Implementing Fentanyl Drug Checking - Results from a Multi-Site Study. Drug Alcohol Depend In press. [DOI] [PubMed] [Google Scholar]
- Green TC, Gilbert M, 2016. Counterfeit Medications and Fentanyl. JAMA Intern Med 176(10), 1555–1557. [DOI] [PubMed] [Google Scholar]
- Green TC, Park JN, Gilbert M, McKenzie M, Struth E, Lucas R, Clarke W, Sherman SG, 2020. An assessment of the limits of detection, sensitivity and specificity of three devices for public health-based drug checking of fentanyl in street-acquired samples. Int J Drug Policy 77, 102661. [DOI] [PubMed] [Google Scholar]
- Harper L, Powell J, Pijl EM, 2017. An overview of forensic drug testing methods and their suitability for harm reduction point-of-care services. Harm Reduct J 14(1), 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Minino AM, Warner M, 2019. Urban-rural Differences in Drug Overdose Death Rates, by Sex, Age, and Type of Drugs Involved, 2017. NCHS data brief(345), 1–8. [PubMed] [Google Scholar]
- Hedegaard H, Minino AM, Warner M, 2020. Drug Overdose Deaths in the United States, 1999-2018. NCHS data brief(356), 1–8. [PubMed] [Google Scholar]
- Hoots B, Vivolo-Kantor A, Seth P, 2020. The rise in non-fatal and fatal overdoses involving stimulants with and without opioids in the United States. Addiction 115(5), 946–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Bekheet F, Park JN, Alexander GC, 2020. The Fourth Wave of the Overdose Epidemic: Synthetic Opioids and Rising Stimulant-Related Harms. Epidemiologic Review, In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariisa M, Scholl L, Wilson N, Seth P, Hoots B, 2019. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential - United States, 2003-2017. MMWR Morb Mortal Wkly Rep 68(17), 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Anderson BJ, Conti MT, Bailey GL, Stein MD, 2018. Expected and actual fentanyl exposure among persons seeking opioid withdrawal management. J Subst Abuse Treat 86, 65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Ondocsin J, Ciccarone D, 2018a. Sold as Heroin: Perceptions and Use of an Evolving Drug in Baltimore, MD. Journal of psychoactive drugs 50(2), 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Ondocsin J, Ciccarone D, 2018b. Toots, tastes and tester shots: user accounts of drug sampling methods for gauging heroin potency. Harm Reduct J 15(1), 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Sampson L, Cerdá M, Galea S, 2015. Worldwide prevalence and trends in unintentional drug overdose: a systematic review of the literature. American journal of public health 105(11), e29–e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NFLIS Public Resource Library, Table 3: State Counts for Fentanyl and Fentanyl Related Compounds. https://www.nflis.deadiversion.usdoj.gov/Resources/NFLISPublicResourceLibrary.aspx. Accessed 06/03/20.
- O’Donnell J, Gladden RM, Mattson CL, Kariisa M, 2018. Notes from the Field: Overdose Deaths with Carfentanil and Other Fentanyl Analogs Detected - 10 States, July 2016-June 2017. MMWR Morb Mortal Wkly Rep 67(27), 767–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Salomone A, Barratt MJ, 2020. Drug checking to detect fentanyl and new psychoactive substances. Current opinion in psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JN, Rouhani S, Beletsky L, Vincent L, Saloner B, Sherman SG, 2020a. Situating the Continuum of Overdose Risk in the Social Determinants of Health: A New Conceptual Framework. Milbank Quarterly, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JN, Rouhani S, Beletsky L, Vincent L, Saloner B, Sherman SG, 2020b. Situating the Continuum of Overdose Risk in the Social Determinants of Health: A New Conceptual Framework. Milbank Q 98(3), 700–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JN, Weir BW, Allen ST, Chaulk P, Sherman SG, 2018. Fentanyl-contaminated drugs and non-fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduct J 15(1), 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouhani S, Park JN, Morales KB, Green TC, Sherman SG, 2019. Harm reduction measures employed by people using opioids with suspected fentanyl exposure in Boston, Baltimore, and Providence. Harm Reduct J 16(1), 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider KE, O’Rourke A, White RH, Park JN, Musci RJ, Kilkenny ME, Sherman SG, Allen ST, 2020. Polysubstance use in rural West Virginia: Associations between latent classes of drug use, overdose, and take-home naloxone. Int J Drug Policy 76, 102642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Krai AH, Gee L, Moore LD, Bluthenthal RN, Lorvick J, Edlin BR, 2001. Predictors and prevention of nonfatal overdose among street-recruited injection heroin users in the San Francisco Bay Area, 1998–1999. American journal of public health 91(11), 1842–1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Morales KB, Park JN, McKenzie M, Marshall BDL, Green TC, 2019. Acceptability of implementing community-based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. Int J Drug Policy 68, 46–53. [DOI] [PubMed] [Google Scholar]
- Strickland JC, Havens JR, Stoops WW, 2019. A nationally representative analysis of “twin epidemics”: Rising rates of methamphetamine use among persons who use opioids. Drug Alcohol Depend 204, 107592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tupper KW, McCrae K, Garber I, Lysyshyn M, Wood E, 2018. Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug Alcohol Depend 190, 242–245. [DOI] [PubMed] [Google Scholar]
- United States Drug Enforcement Administration, 2018. 2018 National Drug Threat Assessment. https://www.dea.gov/sites/default/files/2018-11/DIR-032-18%202018%20NDTA%20final%20low%20resolution.pdf. Accessed 06/03/20.
- Wakeman SE, Green TC, Rich J, 2020. An overdose surge will compound the COVID-19 pandemic if urgent action is not taken. Nature Medicine 26(6), 819–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoorob M, 2019. Fentanyl shock: The changing geography of overdose in the United States. Int J Drug Policy 70, 40–46. [DOI] [PubMed] [Google Scholar]


