Abstract
Objective.
To examine the survival of women with stage I non-endometrioid endometrial cancer with malignant peritoneal cytology.
Methods.
A retrospective observational cohort study was conducted to examine the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program from 2010 to 2016. Women with stage I serous, clear cell, carcinosarcoma, undifferentiated, and mixed endometrial cancer with known peritoneal cytology results at hysterectomy were examined (N = 4506). Propensity score inverse probability of treatment weighting was used to balance the measured covariates, and survival outcomes were assessed according to peritoneal cytology results.
Results.
Malignant peritoneal cytology was reported in 401 (8.9%) women. In multivariable analysis, older age, serous histology, and large tumors were associated with an increased likelihood of malignant peritoneal cytology (all, P < 0.05). In a propensity score weighted model, malignant peritoneal cytology was associated with a nearly two-fold increase in all-cause mortality risk compared to negative peritoneal cytology (5-year rates, 63.4% versus 80.2%, hazard ratio 2.18, 95% confidence interval 1.78–2.66). In sensitivity analyses, malignant peritoneal cytology was associated with decreased overall survival in old and young age groups, serous, clear cell, carcinosarcoma, and mixed histology groups, stage T1a disease, and staged and unstaged cases, but not for stage T1b disease. Difference in 5-year overall survival rates between the malignant and negative peritoneal cytology groups was particularly large among those with clear cell histology (24.0%), stage T1a disease (19.4%), aged >78 years(18.2%), and serous tumors (17.6%).
Conclusion.
Malignant peritoneal cytology can be prevalent in stage I non-endometrioid endometrial cancer. Our study suggests that malignant peritoneal cytology is a prognostic factor for decreased survival in stage I non-endometrioid endometrial cancer.
Keywords: Endometrial cancer, Non endometrioid, Serous, Malignant peritoneal cytology, Survival
1. Introduction
Endometrial cancer is the most common gynecologic malignancy in developed countries worldwide [1]. In 2012, 167,900 women were estimated to have this diagnosis and 34,700 women succumbed to the disease in Europe, Northern America, Australia/New Zealand, and Japan [1]. Tumors of endometrial cancer are traditionally classified as endometrioid and non-endometrioid histologies, and these two have discrete molecular and clinical characteristics and outcomes [2,3]. Non-endometrioid endometrial cancer consists of serous, clear cell, carcinosarcoma, undifferentiated, and mixed histology types, and is associated with poorer prognosis compared to the endometrioid type [3,4].
Endometrial cancer is commonly diagnosed at stage I disease [3,4]. The standard treatment approach for women with apparent stage I disease, irrespective of histology types, is a surgical treatment including hysterectomy, salpingo-oophorectomy, and additional lymphadenectomy for at-risk groups [5]. Surgical specimens are used to identify certain tumor characteristics that are associated with increased risk of disease relapse, and tailored postoperative therapy is recommended based on risk factors to improve survival outcome [5,6]. These prognostic tumor factors are generally incorporated into the cancer staging schema, such as depth of myometrial tumor invasion, cervical stromal tumor invasion, adnexal/uterine serosal tumor metastasis, and lymph node metastasis [7].
Malignant peritoneal cytology could be another important tumor factor. This was previously used as an element of the Fédération Internationale de Gynécologie et d’Obstétrique (FIGO) cancer staging system for endometrial cancer prior to the 2009 revision [7]. Malignant peritoneal cytology can be seen in approximately 5% of early-stage endometrial cancer, and the incidence seems higher in the non-endometrioid histological types [8–21]. Moreover, multiple studies have shown decreased survival in the setting of malignant peritoneal cytology, but studies specifically evaluating non-endometrioid types are limited [8–19].
To date, population-based statistics associated with malignant peritoneal cytology in stage I non-endometrioid endometrial cancer remain scarce. If malignant peritoneal cytology is to be considered a prognostic factor, its utility in clinical practice would be fairly substantial (e.g., survival stratification via cancer staging schema, and possible implications for postoperative treatment). The objective of this study was to examine the association between malignant peritoneal cytology and survival in women with early-stage non-endometrioid endometrial cancer.
2. Materials and methods
2.1. Data
A retrospective observational cohort study was conducted by examining the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program [22]. The SEER Program is the largest population-based tumor registry in the United States and has been in operation since 1973. The SEER Program covers ~35% of the U.S. population in the latest version, and 97% of cancer incidence is captured within the registry area. Patient identification, data accumulation and entry, and rigorous quality control for the SEER Program are managed by registered trained personnel [23]. The University of Southern California Institutional Review Board exempted this study due to the use of deidentified, publicly available data.
2.2. Study population
Women with stage I (T1/N0-x/M0-x) non-endometrioid endometrial cancer who underwent hysterectomy with available peritoneal cytology results from 2010 to 2016 were eligible for the study. The histology types for non-endometrioid tumors were limited to serous, clear cell, carcinosarcoma, undifferentiated, and mixed type tumors. This starting point was chosen because the FIGO revised the cancer staging schema in 2009 and the SEER Program has discrete information for peritoneal cytology testing results during the study period [24,25]. Patients with stage II-IV disease, an unknown tumor stage, with histology types other than those described above, a secondary cancer diagnosis, or who did not undergo hysterectomy were excluded from the analysis. Peritoneal cytology results recorded as suspicious were also excluded.
2.3. Exposure allocation
Surgically treated women with stage I non-endometrioid endometrial cancer who had malignant peritoneal cytology were compared to those who had negative peritoneal cytology. Collaborative Stage Site-Specific Factor 2 was used to interpret the peritoneal cytology result as malignant peritoneal cytology (code, 010) versus negative peritoneal cytology (code, 000) [24,25].
2.4. Clinical variables
Patient demographics, tumor characteristics, treatment type, and survival outcomes were abstracted from the SEER Program. Patient demographics included age (≤57, 58–60, 61–78, and >78), year of diagnosis (2010, 2011, 2012, 2013, 2014, 2015, and 2016), race/ethnicity (non-Hispanic white, black, Hispanic, Asian, and others), registry area (West, Central, and East), insurance status (yes versus no), and marital status (single, married, divorced, separated, widowed, and unmarried/domestic). Age cutoff points were determined per the regression-tree analysis described below.
Tumor characteristics included histology subtypes (serous, clear cell, carcinosarcoma, undifferentiated, and mixed), tumor differentiation (well, moderate, and poor), cancer stage (T1a versus T1b), tumor size (≤2.0, 2.1–4.0, 4.1–6.0, 6.1–8.0, and >8 cm), and peritoneal cytology results (malignant versus negative). Histology types were based on the International Classification of Diseases for Oncology 3rd edition/World Health Organization histological classification as described previously [26]. The American Joint Committee on Cancer staging classification schema was used for defining T stage [27].
Treatment types included hysterectomy type (simple, modified/radical, and supracervical), performance of pelvic lymphadenectomy (yes versus no) and para-aortic lymphadenectomy (yes versus no), and postoperative therapy modalities for chemotherapy and radiotherapy (whole pelvic irradiation [WPRT], vaginal brachytherapy [VBT], chemotherapy, chemotherapy/WPRT, and chemotherapy/VBT). Lymphadenectomy performance was verified with the study coding for “Regional Nodes”, which was introduced in 1988 and has not changed since.
2.5. Outcome measures
Overall survival (OS) and cause-specific survival (CSS) were assessed for outcome analysis.
OS was defined as the time interval between the endometrial cancer diagnosis and death from any cause. CSS was defined as the time interval between the endometrial cancer diagnosis and death due to endometrial cancer. Women who had no survival event at the last follow-up were censored. Survival status in the SEER Program is near-universally updated and is externally linked to the National Death Index for validation.
2.6. Statistical approach
The first step of the analysis was to identify the independent characteristics associated with malignant peritoneal cytology. Differences in the baseline characteristics were assessed with chi-square test for univariable analysis. Then, a binary logistic regression model was fitted, and all the pre-/intra-operative factors with a P < 0.05 in the univariable analysis were entered into the initial model, and a conditional backward method was used with a final stopping rule of P < 0.05. Multicollinearity was assessed with variance inflation factor (cutoff, 2.5). Hosmer-Lemeshow test was used to assess the goodness-of-fit in the final model, and a P > 0.05 was interpreted as a good-fit model.
In an attempt to identify the specific patterns for patient and tumor demographics for malignant peritoneal cytology, a recursive partitioning analysis was performed to construct a regression-tree model for risk patterns [28]. All independent factors for malignant peritoneal cytology were entered in the final analytic model, and the chi-square automatic interaction detector method was used for the model with stopping rule of three layers. Among the determined nodes in this analysis, incidences of malignant peritoneal cytology were estimated.
The second step of the analysis was to assess the outcome measures (OS and CSS) related to malignant peritoneal cytology. Propensity score inverse probability of treatment weighting was used to balance the measured covariates between the two groups [29]. The propensity score was computed by fitting a multivariable binary logistic regression model for the peritoneal cytology status (malignant versus negative) [30]. All measured covariates were entered into the model. The propensity score weighting approach assigned women with malignant peritoneal cytology a weight of 1/(propensity score) and women with negative peritoneal cytology a weight of 1/(1-propensity score), respectively. Stabilized weights were used for weighting, and the threshold technique was used at the 1st and 99th percentile of the weight distribution [29].
Size effect was assessed between the two groups in the weighted model, and a standardized difference (SD) of >0.20 was considered presence of size effect with clinical imbalance between the two groups [31]. The Kaplan-Meier method was used to plot survival curves, and a Cox proportional hazard regression model was fitted to estimate hazard ratio (HR) with 95% confidence interval (CI) for malignant peritoneal cytology. Proportional hazard assumption was tested and satisfied without interaction over time. The difference in the 5-year survival rates was also calculated.
Multiple sensitivity analyses were performed to assess the robustness of the study findings. First, the association of peritoneal cytology results and survival outcome was examined, stratified by age (≤78 versus 78 years), histology (serous, clear cell, carcinosarcoma, and mixed), cancer stage (T1a versus T1b), and lymphadenectomy status (staged versus unstaged). Propensity score weighting was performed in each subcohort. Second, survival outcomes were assessed across postoperative therapy types and stratified by the peritoneal cytology results. Survival outcomes were compared between WPRT, chemotherapy/WPRT, and chemotherapy/VBT among serous, clear cell, and carcinosarcoma cases. This was based on the notion that multiple phase III trials have examined these treatment approaches in early-stage serous and clear cell tumors [32,33], and recent studies suggest a benefit of combination therapy in carcinosarcoma [34,35]. Third, doubly robust adjustment was used in the presence of size effect in the weighted model. Lastly, the survival outcome of women with stage I disease and malignant peritoneal cytology was compared to those with stage III disease. The rationale for this analysis is that malignant peritoneal cytology was a component of stage III disease on previous staging schema [7].
Two-sided hypotheses were used for statistical analysis, and a P < 0.05 was considered statistically significant. Statistical Package for Social Sciences (version 25.0, Armonk, NY, USA) and R version 3.5.3 (R Foundation for Statistical Computing, Vienna, Austria) were used for analyses. The STROBE guidelines were consulted to outline the results of this observational cohort study.
3. Results
Among 53,636 women in the database, 4506 women with stage I non-endometrioid endometrial cancer had peritoneal cytology results available and met the inclusion criteria (Fig. S1). Of those, malignant peritoneal cytology was reported in 401 (8.9%) women.
Women aged >78 years (14.4%) and aged 58–60 (11.6%), uninsured patients (10.4%), those with serous or clear cell histology types (both, 10.8%), those with stage T1b disease (10.6%) or tumor size of 4.1–6.0 cm (11.7%) had >10% incidences of malignant peritoneal cytology (Table S1). In the univariable analysis (Table 1), age, histology type, performance of para-aortic lymphadenectomy, and tumor size were significantly associated with malignant peritoneal cytology (all, P < 0.05). In multivariable analysis (Table 1), age >78 years (OR 1.95), serous histology (OR 1.55), and tumor size of 4.1–6.0 cm (OR 1.81) remained associated with an increased likelihood of malignant peritoneal cytology (all, P < 0.05).
Table 1.
Patient demographics per peritoneal cytology status (N = 4506).
| Characteristics | Negative | Malignant | P-value | aOR (95%CI) | P-value† |
|---|---|---|---|---|---|
| No. | n = 4105 | n = 401 | |||
| Age (yr) | <0.001 | <0.001* | |||
| ≤57 | 788 (19.2%) | 59 (14.7%) | 1 | ||
| 58–60 | 421 (10.3%) | 55 (13.7%) | 1.68 (1.14–2.48) | 0.010 | |
| 61–78 | 2517 (61.3%) | 223 (55.6%) | 1.06 (0.78–1.45) | 0.694 | |
| >78 | 379 (9.2%) | 64 (16.0%) | 1.95 (1.33–2.87) | 0.001 | |
| Year | 0.959 | ||||
| 2010 | 489 (11.9%) | 48 (12.0%) | |||
| 2011 | 528 (12.9%) | 49 (12.2%) | |||
| 2012 | 587 (14.3%) | 57 (14.2%) | |||
| 2013 | 615 (15.0%) | 65 (16.2%) | |||
| 2014 | 603 (14.7%) | 55 (13.7%) | |||
| 2015 | 638 (15.5%) | 58 (14.5%) | |||
| 2016 | 645 (15.7%) | 69 (17.2%) | |||
| Race/ethnicity | 0.164 | ||||
| White | 2581 (62.9%) | 275 (68.6%) | |||
| Black | 680 (16.6%) | 49 (12.2%) | |||
| Hispanic | 443 (10.8%) | 40 (10.0%) | |||
| Asian | 352 (8.6%) | 33 (8.2%) | |||
| Others | 28 (0.7%) | 1 (0.2%) | |||
| Unknown | 21 (0.5%) | 3 (0.7%) | |||
| Marital status | 0.426 | ||||
| Single | 669 (13.3%) | 70 (17.5%) | |||
| Married | 2033 (49.5%) | 215 (53.6%) | |||
| Divorced | 514(12.5%) | 36 (9.0%) | |||
| Separated | 48 (1.2%) | 5 (1.2%) | |||
| Widowed | 632 (15.4%) | 56 (14.0%) | |||
| Unmarried/domestic | 15 (0.4%) | 1 (0.2%) | |||
| Unknown | 194 (4.7%) | 18 (4.5%) | |||
| Insurance | 0.322 | ||||
| Yes | 3988 (97.1%) | 385 (96.0%) | |||
| No | 69 (1.7%) | 8 (2.0%) | |||
| Unknown | 48 (1.2%) | 8 (2.0%) | |||
| Registry area | 0.252 | ||||
| West | 2074 (50.5%) | 214 (53.4%) | |||
| Central | 770 (18.8%) | 62 (15.5%) | |||
| East | 1261 (30.7%) | 125 (31.2%) | |||
| Histology type | 0.011 | 0.004* | |||
| Serous | 1294 (31.5%) | 156 (38.9%) | 1.55 (1.20–2.00) | 0.001 | |
| Clear cell | 248 (6.0%) | 30 (7.5%) | 1.42 (0.92–2.17) | 0.111 | |
| Carcinosarcoma | 877 (21.4%) | 81 (20.2%) | 1.01 (0.75–1.38) | 0.931 | |
| Mixed | 1653 (40.3%) | 132 (32.9%) | 1 | ||
| Undifferentiated | 33 (0.8%) | 2 (0.5%) | 0.59 (0.14–2.50) | 0.472 | |
| Tumor differentiation | 0.073 | ||||
| Well | 434 (10.6%) | 28 (7.0%) | |||
| Moderate | 381 (9.3%) | 31 (7.7%) | |||
| Poor | 2289 (55.8%) | 242 (60.3%) | |||
| Unknown | 1001 (24.4%) | 100 (24.9%) | |||
| T stage | 0.115 | ||||
| IA | 3161 (77.0%) | 292 (72.8%) | |||
| IB | 823 (20.0%) | 98 (24.4%) | |||
| I NOS | 121 (2.9%) | 11 (2.7%) | |||
| Tumor size (cm) | 0.017 | 0.004* | |||
| ≤2.0 | 830 (20.2%) | 67 (16.7%) | 1 | ||
| 2.1–4.0 | 1191 (29.0%) | 121 (30.2%) | 1.32 (0.97–1.82) | 0.082 | |
| 4.1–6.0 | 711 (17.3%) | 94 (23.4%) | 1.81 (1.29–2.54) | 0.001 | |
| 6.1–8.0 | 284 (6.9%) | 31 (7.7%) | 1.54 (0.97–2.44) | 0.069 | |
| >8.0 | 205 (5.0%) | 19 (4.7%) | 1.35 (0.78–2.35) | 0.286 | |
| Unknown | 884(21.5%) | 69 (17.2%) | 1.00 (0.71–1.42) | 0.995 | |
| Hysterectomy type | 0.583 | ||||
| Simple | 3757 (91.5%) | 359 (89.5%) | |||
| Modified/radical | 201 (4.9%) | 25 (6.2%) | |||
| Supracervical | 20 (0.5%) | 2 (0.5%) | |||
| NOS | 127 (3.1%) | 15 (3.7%) | |||
| Pelvic lymphadenectomy | 0.456 | ||||
| No | 688 (16.8%) | 60 (15.0%) | |||
| Yes | 3394 (82.7%) | 340 (84.8%) | |||
| Unknown | 23 (0.6%) | 1 (0.2%) | |||
| Para-aortic lymphadenectomy | 0.049 | ||||
| No | 1829 (44.6%) | 157 (39.2%) | |||
| Yes | 2245 (54.7%) | 243 (60.6%) | |||
| Unknown | 31 (0.8%) | 1 (0.2%) | |||
| Postop therapy | <0.001 | ||||
| None‡ | 1705 (41.5%) | 108 (26.9%) | |||
| VBT/chemo | 800 (19.5%) | 100 (24.9%) | |||
| Chemo | 783 (19.1%) | 116 (28.9%) | |||
| VBT | 337 (8.2%) | 19 (4.7%) | |||
| WPRT/chemo | 279 (6.8%) | 38 (9.5%) | |||
| WPRT | 190 (4.6%) | 19 (4.7%) | |||
| RT NOS/chemo | 7 (0.2%) | 0 | |||
| RT NOS | 4(0.1%) | 1 (0.2%) |
Number (percentage per group) is shown. Percentage per row is shown in Supplemental Table S1. Chi-square test for univariable analysis. A binary logistic regression model for multivariable analysis. All the preoperative and operative covariates with P < 0.05 in univariable analysis were entered in the initial model, and conditional backward method with the stopping rule of P < 0.05.
including unknown cases.
P-value for multivariable analysis.
P-value for interaction. Hosmer-Lemeshow test shows P = 0.984 indicated a good-fit model. Abbreviations: aOR, adjusted-odds ratio; CI, confidence interval; NOS, not otherwise significant; VBT, vaginal brachytherapy; WPRT, whole pelvic radiotherapy; RT, radiotherapy; and chemo, chemotherapy.
Women with malignant peritoneal cytology were more likely to receive any type of postoperative therapy compared to those with negative cytology (73.1% versus 58.5%, P < 0.001; Table 1). Among those who received postoperative therapy, chemotherapy alone was the most common type of postoperative therapy (28.9% versus 19.1%) followed by chemotherapy/VBT (24.9% versus 19.5%).
In a regression-tree model with recursive partitioning analysis (Fig. S2), age was found to be the strongest factor to distinguish the peritoneal cytology pattern, followed by histology types. Women aged >78 with serous/undifferentiated tumors (representing 3.3% of the study population) possessed a disproportionally high incidence of malignant peritoneal cytology that exceeded >20% (21.5%).
Clinical demographics were more balanced after performing propensity score weighting (all 14 factors, SD ≤0.10; Fig. 1 and Table S2). 489 women with malignant peritoneal cytology were compared to 4116 women with negative peritoneal cytology for survival outcome measures (Fig. S1). The median follow-up time was 2.8 years, and there were 645 (14.0%) deaths including 491 (10.7%) deaths due to endometrial cancer.
Fig. 1.
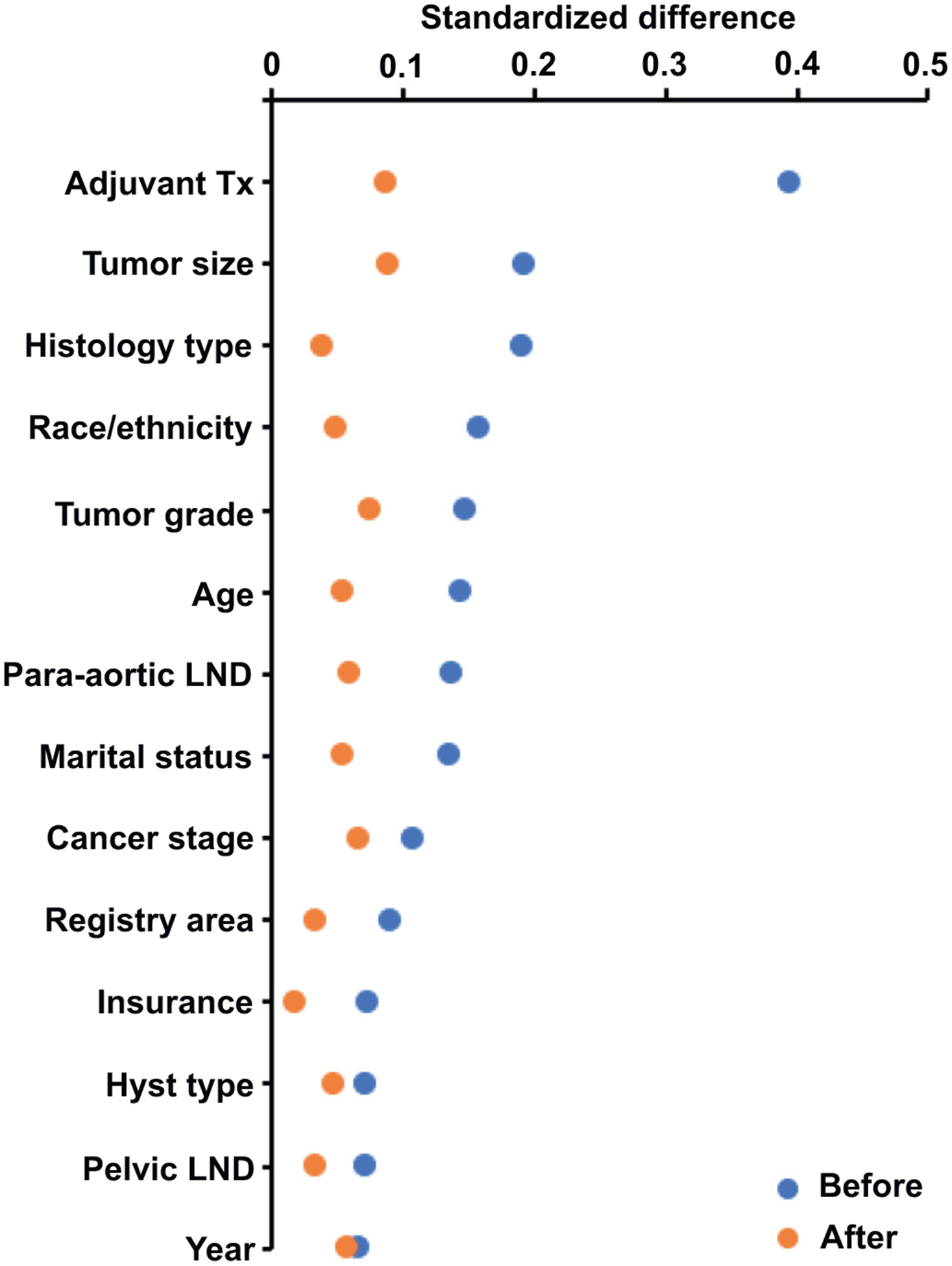
Standardized differences before and after PS-IPTW (whole cohort). Standardized difference of >0.2 indicates the presence of size effect with clinical imbalance. Abbreviations: PS-IPTW, propensity score inverse provability of treatment weighting; and LND, lymphadenectomy; and Tx, therapy.
In the weighted model, the 5-year OS rates were 63.4% (95%CI57.7–69.6) for women with malignant peritoneal cytology and 80.2% (95%CI 78.6–81.9) for those with negative peritoneal cytology (Fig. 2). The absolute difference in the 5-year OS rates was 16.8%. Malignant peritoneal cytology was associated with a nearly two-fold increased risk of all-cause mortality (HR 2.18, 95%CI 1.78–2.66, P < 0.001). Similar results were observed for CSS (5-year rates, 67.4% versus 84.8%, absolute difference 17.4%, HR 2.51, 95%CI 2.02–3.13, P < 0.001; Fig. S3).
Fig. 2.
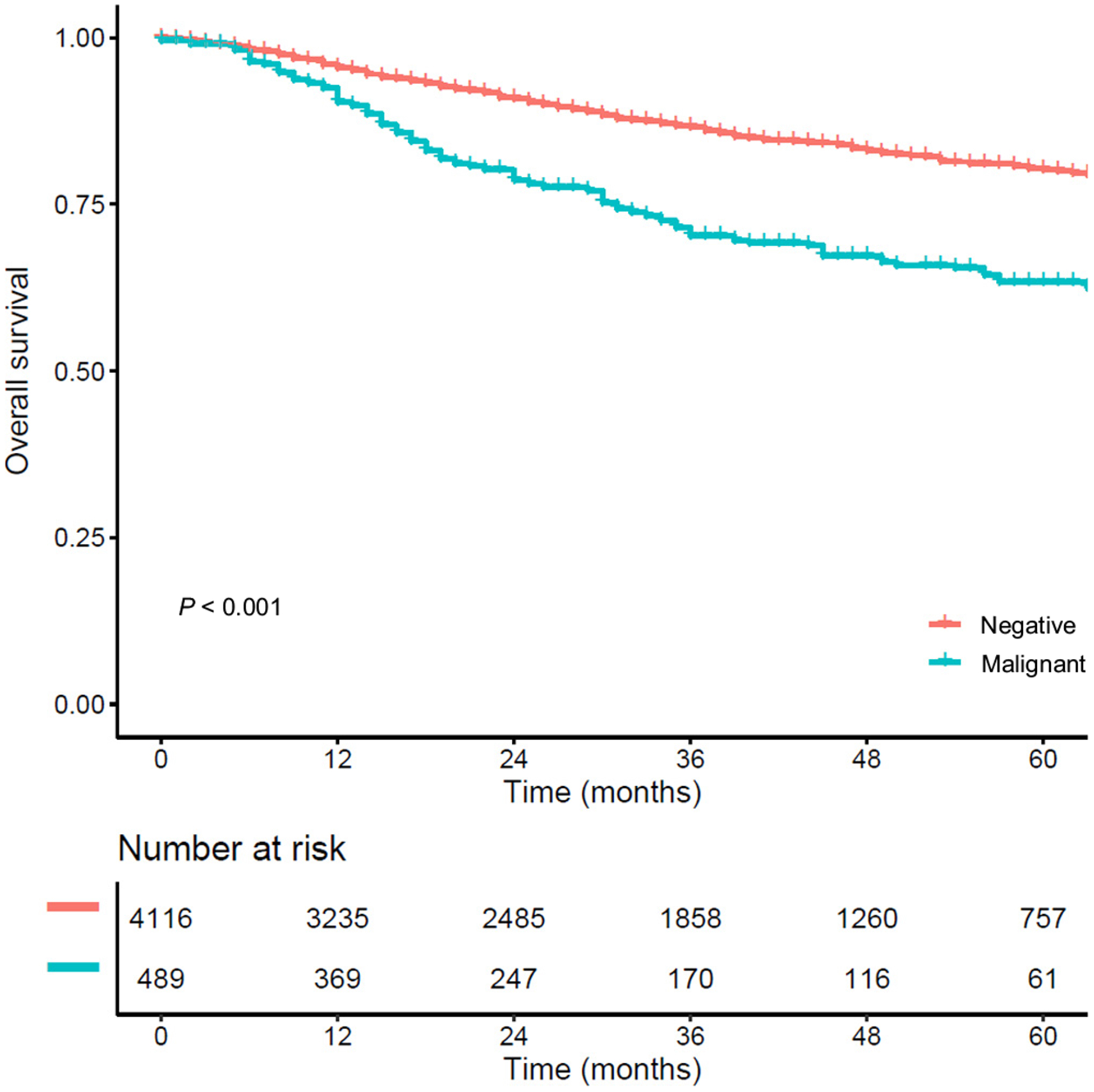
Survival curves based on peritoneal cytology results (whole cohort). Survival curves for overall survival are shown according to the peritoneal cytology status. Cox proportional hazard regression model for P-value. Abbreviations: Negative, no malignant cells in peritoneal cytology; and malignant, malignant cells in peritoneal cytology.
In sensitivity analyses (Figs. 3–4 and S4), malignant peritoneal cytology was associated with decreased OS in all the sub-cohorts including older age (>78 years, HR 2.75), serous (HR 2.12), clear cell (HR 2.80), carcinosarcoma (HR 1.84), stage T1a disease (HR 2.59), and unstaged cases (HR 2.32) compared to negative peritoneal cytology (all, P < 0.05), but not in stage T1b disease (HR 1.35, 95%CI 0.93–1.96, P = 0.112). The difference in 5-year OS rates between the malignant and negative peritoneal cytology groups was particularly large for serous (17.6%) and clear cell (24.0%) histology, stage T1a disease (19.4%), and age >78 years (18.2%). Similar trends were observed for CSS (Fig. S3).
Fig. 3.
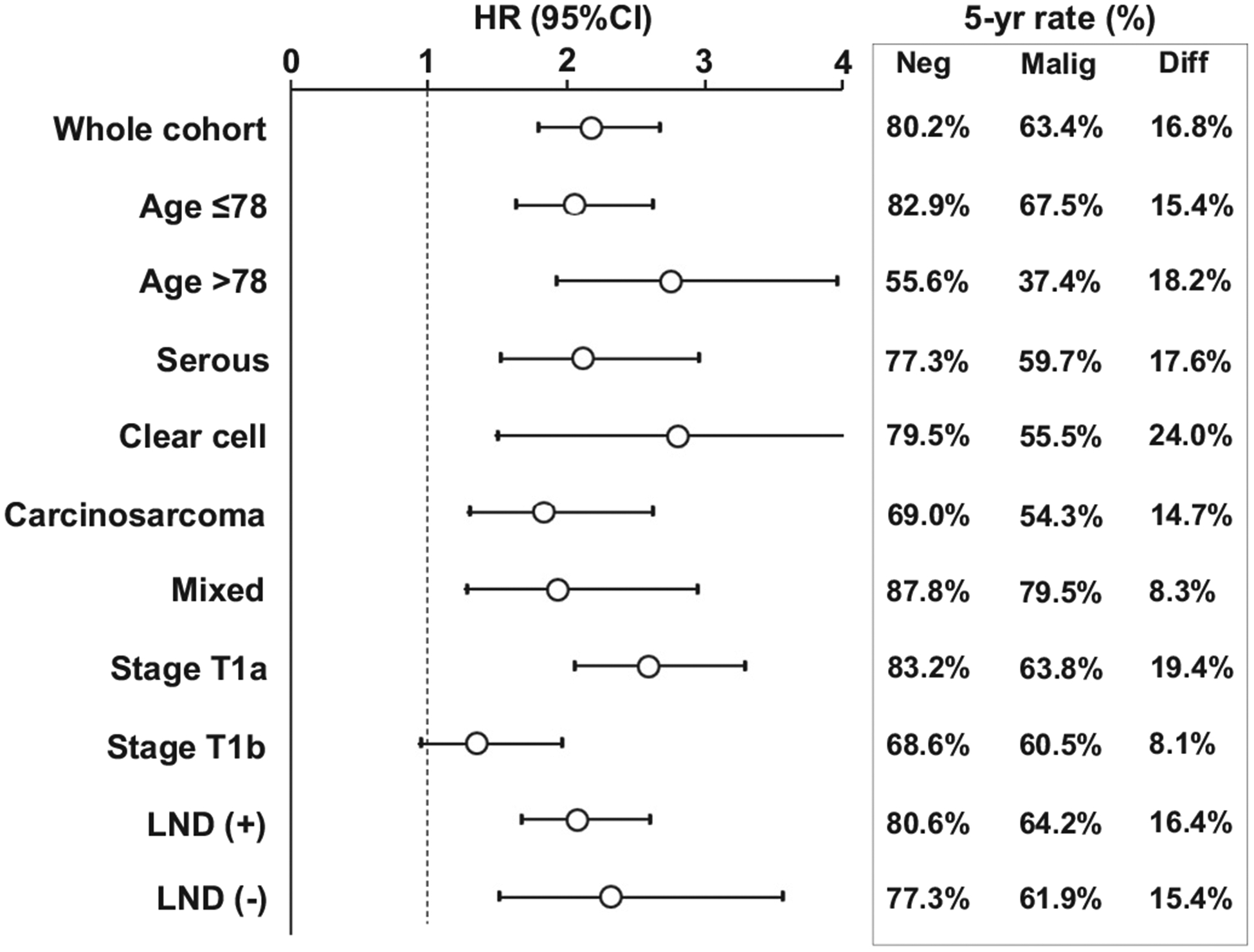
Forest plots for overall survival (weighted models). Association of peritoneal cytology (malignant versus negative) and overall survival was assessed with Cox proportional hazard regression in the weighted models. The 5-year survival rates and differences are shown. Circles represent HR, and bars represent 95%CI. Abbreviations: HR, hazard ratio; CI, confidence interval; LND, lymphadenectomy; Neg, negative peritoneal cytology; Malig, malignant peritoneal cytology; and Diff, difference in 5-year survival rate between the negative and malignant cytology groups.
Fig. 4.
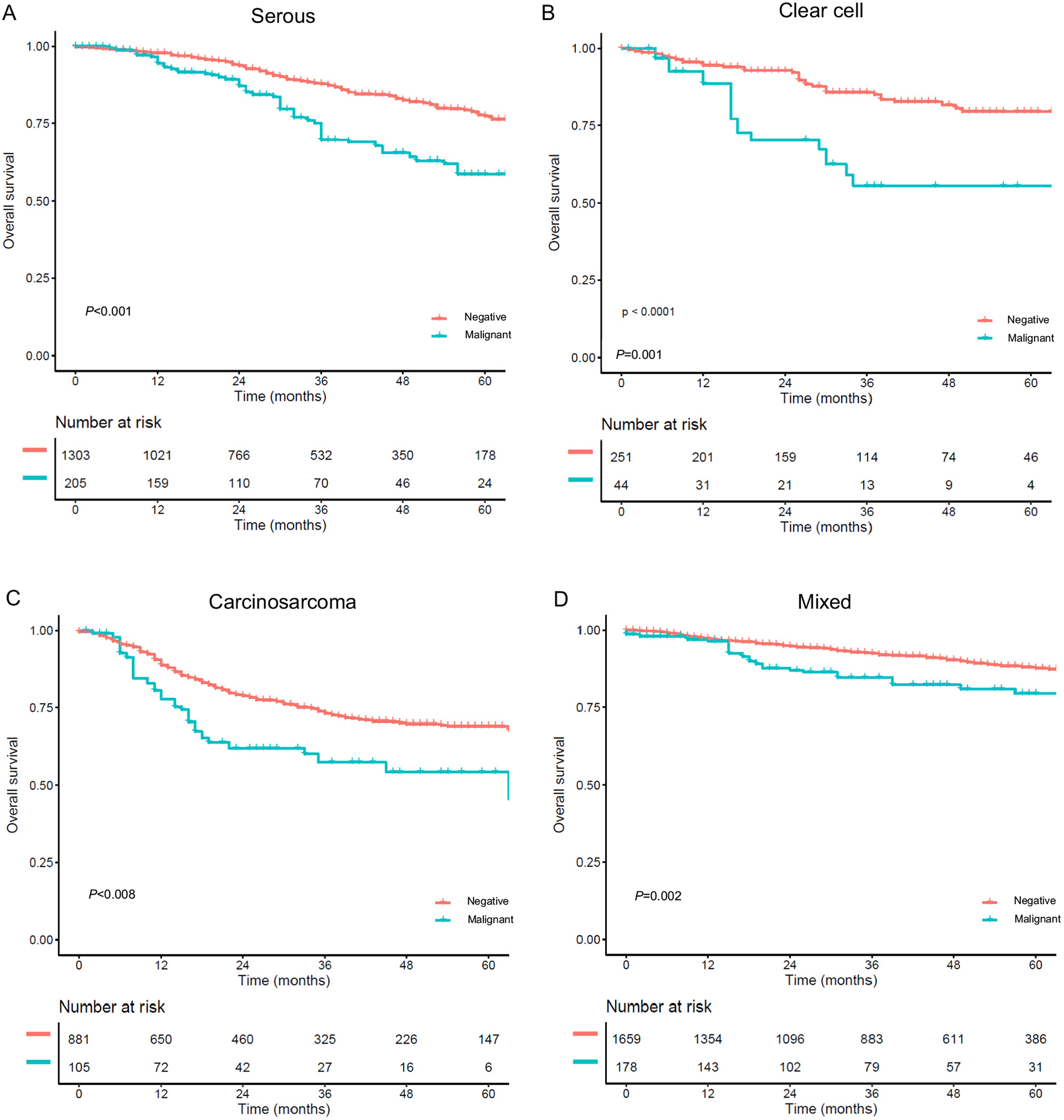
Sensitivity analysis for overall survival (histology type). Survival curves for overall survival are shown by peritoneal cytology status: (A) serous, (B) clear cell, (C) carcinosarcoma, and (D) mixed histology. Survival statistics are shown in Fig. 3.
The association between postoperative therapy and survival was examined based on the peritoneal cytology status among women with serous, clear cell, and carcinosarcoma histologies (Fig. S5). In the negative cytology cases, women who received chemotherapy-based postoperative therapy had higher 5-year OS rates compared to those received whole pelvic irradiation (79.6% for chemotherapy ± brachytherapy, 77.4% for chemotherapy with whole pelvic irradiation, and 56.9% for whole pelvic irradiation, P < 0.001). In contrast, OS was similar across the three modalities among malignant peritoneal cytology cases (P = 0.844).
Women with stage I disease and malignant peritoneal cytology had a higher 5-year OS rate compared to those with stage III disease: 62.3% for stage I disease with malignant peritoneal cytology, 50.5% for stage IIIA,31.5% for stage IIIB, 43.2% for stage IIIC1, and 37.5% for stage IIIC2 disease, respectively (P < 0.001, Fig. 5). Similar results were observed for CSS (66.1%, 54.2%, 36.9%, 46.4%, and 41.5%, respectively, P < 0.001).
Fig. 5.
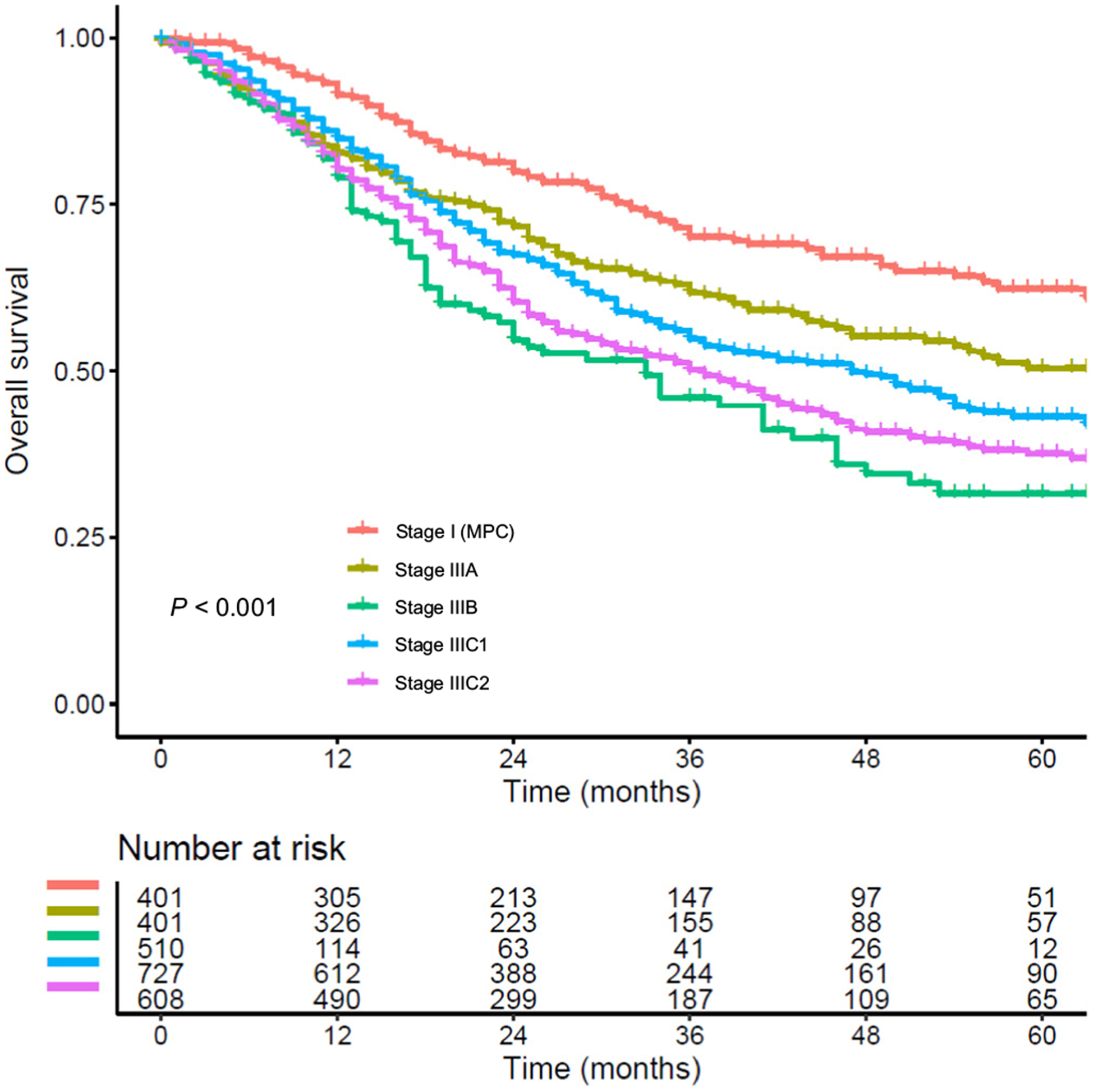
Survival curves based on cancer stages. Survival curves for overall survival are shown based on cancer stages. Abbreviations: MPC, malignant peritoneal cytology.
4. Discussion
Important findings from this study are that malignant peritoneal cytology was seen in ~9% of stage I non-endometrioid endometrial cancer and that malignant peritoneal cytology is associated with a two- to three-fold increased risk of all-cause death. Several points deserve further discussion.
Malignant peritoneal cytology is considered relatively common in stage I non-endometrioid endometrial cancer and was seen in approximately 9% of our study population, compared to 5.3–9.2% which has been reported in prior studies [15,36]. This is far more prevalent than in the endometrioid histology types, where the incidence of malignant peritoneal cytology is about half that of the non-endometrioid endometrial cancer types (2.8–4.8%) [11,15]. Therefore, recognition of malignant peritoneal cytology as a common tumor factor is necessary in early-stage non-endometrioid endometrial cancer.
Old age, serous histology, and larger tumor size were associated with increased risks of malignant peritoneal cytology. Older age was associated with a higher likelihood of having malignant peritoneal cytology, and women aged >78 years with serous or undifferentiated histology had the highest incidence of malignant peritoneal cytology, exceeding 20% in our study. The exact etiology of this increased incidence of malignant peritoneal cytology in older women is unknown, but it is speculated that the tumors of older women may be more aggressive than those in younger women.
One possible mechanism of malignant peritoneal cytology is the retrograde spread of tumor cells via the fallopian tubes. A recent study demonstrated that tubal ligation is associated with decreased risk of peritoneal tumor metastasis (GOG-210) [37]. The risk reduction is much higher in serous tumors (peritoneal metastasis rates for tubal ligation: yes versus no, 13.8% versus 37.2%) than in low-grade endometrioid tumors (23.8% versus 24.0%). Trans-tubal spread is therefore more common in non-endometrioid endometrial cancer, which could explain the higher incidence of malignant peritoneal cytology cases in non-endometrioid versus endometrioid tumors.
Our study demonstrated that malignant peritoneal cytology is a prognostic factor in stage I non-endometrioid endometrial cancer. This is congruent with the results of a prior study, but the larger sample size in our study enhances our findings [38]. As malignant peritoneal cytology is associated with other tumor factors such as lymph node metastasis [39], one may argue that decreased survival with the presence of malignant peritoneal cytology is due to micro-metastases in unstaged cases. However, sub-cohort analyses of women who did and did not undergo lymphadenectomy showed similar results, supporting the notion that malignant peritoneal cytology is likely an independent prognostic factor in stage I non-endometrioid endometrial cancer.
A striking finding is that the impact of malignant peritoneal cytology on survival is quite significant in the earliest cancer stages (Fig. 3). That is, the mortality risk is nearly tripled (HR 2.59) with a considerably large 5-year survival rate decrease (19.4%) when malignant cells were present in the peritoneal cytology in stage T1a disease. This finding suggests that (i) malignant peritoneal cytology may reflect the presence of more aggressive tumor characteristics which has an increased propensity to metastasis and (ii) has more impact on survival in early-stage disease when there is less tumor burden in non-endometrioid endometrial cancer.
The current National Comprehensive Cancer Network (NCCN) guidelines for postoperative therapy for stage I endometrial cancer do not have a histology type-specific recommendation [5]. Two recent trials compared radiotherapy-based postoperative therapy and a chemotherapy-based approach [32,33]. Both trials included a small fraction of women with early-stage non-endometrioid tumors with serous and clear cell histologies. Analyses of these sub-cohorts showed that overall survival was similar between the two treatment approaches. Notably, their trials did not assess the peritoneal cytology status, which may have possibly confounded the results. Our study suggests that a chemotherapy-based approach may be more beneficial over a radiotherapy-based approach in patients with stage I non-endometrioid endometrial cancer with negative peritoneal cytology results.
Malignant peritoneal cytology was removed from the FIGO cancer staging schema in 2009 [7]. This was most likely due to the lack of a prognostic impact shown in some studies [20,21], but these studies were limited either by small sample sizes or lack of stratification according to histology type or cancer stage. This revision in the cancer staging schema impacted practice patterns with a recent study showing a decrease in peritoneal cytology testing during hysterectomy for early-stage endometrial cancer [9]. However, our study emphasizes the importance of peritoneal cytology evaluation at hysterectomy, which is also strongly recommended by the NCCN guidelines [5]. The decrease in 5-year survival rate exceeding 15% found in this study as well as by others is clinically impressive and not negligible [15]. Therefore, our study team humbly suggests including malignant peritoneal cytology as a sub-group in stage I disease.
Strengths of the current study include that this is a population-based analysis with, to our knowledge, the largest sample size for non-endometrioid tumors in the literature to date. A homogenous study population restricted to stage I non-endometrioid tumors enhances the interpretation of the study results. The analytic approach with propensity score inverse probability of treatment weighting as well as exhaustive sensitivity analyses enriched the statistical rigor.
Possible limitations in this study are as follows: first, this study has a retrospective design, with inherent unmeasured bias. For example, details of surgical-pathological factors such as lympho-vascular space invasion, personal history of tubal surgery, use of diagnostic hysteroscopy prior to hysterectomy, and omental biopsy were not available in the SEER Program, but may affect the incidence of malignant peritoneal cytology as well as the oncologic outcomes. In particular, multiple studies suggested an increased risk of malignant peritoneal cytology with the use of diagnostic hysteroscopy [40,41]. In older women, cervical stenosis due to age-related change may make in-office endometrial sampling difficult, and diagnostic hysteroscopy may be used to achieve a tissue sample. The observed effect in our study may be to some degree biased by the lack of information about preoperative hysteroscopy. Nevertheless, the prognostic impact of malignant peritoneal cytology related to diagnostic hysterectomy remains understudied and needs further investigation.
Second, there is a possibility of lead-time bias in the study due to the relatively short follow-up time (median, ~3 years). Third, the accuracy of malignant cytology results is unknown due to the lack of central pathology review in the study. Fourth, as this study only examined the U.S. population, generalizability of our findings to other study populations needs to be examined. Fifth, complete oncological outcome analysis was not feasible due to lack of information on recurrence and its anatomical site in the SEER Program. Therefore, it is unknown if malignant peritoneal cytology is associated with distant recurrence and if systemic chemotherapy use reduces these recurrences as hypothesized by prior studies [32,33]. Likewise, extra caution is needed to interpret the result of exploratory analysis for malignant peritoneal cytology and postoperative therapy due to limited sample size in this subcohort.
Sixth, possible misclassification may exist in adjuvant therapy. Per the SEER Program definition, cases with no and unknown status are grouped together in chemotherapy or radiotherapy data. Lastly, details of chemotherapy (regimen and cycle) were not available in the SEER Program. It may therefore be possible that the lack of survival benefit in chemotherapy over radiotherapy among the malignant peritoneal cytology group was due to an insufficient number of administered cycles. For example, in a trial of high-risk early stage disease (GOG-249), patients in the chemotherapy-based arm received 3 cycles of post-operative chemotherapy whereas patients with stage III disease received 6 cycles of post-operative chemotherapy (GOG-258) [32,42].
In conclusion, our study suggests that malignant peritoneal cytology is a prognostic tumor factor associated with increased mortality risk in women with stage I non-endometrioid endometrial cancer. When cancer cells are present in the peritoneal cytology, 5-year survival rates drop by >15%, which is a substantial decrease. Together with our recent analysis of stage I endometrioid endometrial cancer demonstrating a similar association between malignant peritoneal cytology and decreased survival [43], this study re-visits the conversation as to whether or not malignant peritoneal cytology should be incorporated back into the cancer staging schema.
Supplementary Material
HIGHLIGHTS.
Examined survival effect of malignant peritoneal cytology in stage I non-endometrioid endometrial cancer
Malignant peritoneal cytology was seen in 8.9%.
Malignant peritoneal cytology was associated with nearly 2-fold increased mortality risk.
Similar association was seen in serous, clear cell, carcinosarcoma, and mixed types.
Acknowledgements
Funding support
Ensign Endowment for Gynecologic Cancer Research (K.M.).
Role of funding for the study
The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declaration of competing interest
Consultant, Clovis Oncology, research funding, Merck (J.D.W.); consultant, Quantgene (L.D.R.); honorarium, Chugai, textbook editorial expense, Springer, and investigator meeting attendance expense, VBL therapeutics (K.M.); research funding, MSD (S.M.); personal fees, non-financial supports, honoraria for lectures, advisory board, and travel support, AstraZeneca and Roche, non-financial support and travel support, Medac, personal fees, honoraria for lectures, and advisory board, Tesaro and Pharmamar, personal fees and honoraria for advisory board, Clovis and Lilly, personal fees and honoraria for lectures, Stryker, personal fees and honoraria for advisory board, Immunogen (H.P.); advisory board, Tesaro, GSK (M.K.); none for others.
Data availability statement
The data that support the findings of this study are openly available in The National Cancer Institute’s Surveillance, Epidemiology, and End Results Program at http://seer.cancer.gov/.
Footnotes
Ethical committee exemption
University of Southern California (HS-16-00481).
Transparency
The manuscript’s corresponding author (K.M.) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. Surveillance, Epidemiology, and End Result Program is the source of the de-identified data used; and the program has not verified and is not responsible for the statistical validity of the data analysis or the conclusions derived by the study team. Race/ethnicity was based on the program grouping.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ygyno.2020.07.010.
References
- [1].Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A, Global cancer statistics, 2012, CA Cancer J. Clin 65 (2015) 87–108. [DOI] [PubMed] [Google Scholar]
- [2].Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, Yau C, Laird PW, Ding L, Zhang W, Mills GB, Kucherlapati R, Mardis ER, Levine DA, Integrated genomic characterization of endometrial carcinoma, Nature. 497 (2013) 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E, Endometrial cancer, Lancet (London, England) 387 (2016) 1094–1108. [DOI] [PubMed] [Google Scholar]
- [4].Wright JD, Barrena Medel NI, Sehouli J, Fujiwara K, Herzog TJ, Contemporary management of endometrial cancer, Lancet (London, England) 379 (2012) 1352–1360. [DOI] [PubMed] [Google Scholar]
- [5].Uterine neoplasms. NCCN Clinical Practice Guidelines in Oncology, National Comprehensive Cancer Network https://www.nccn.org/professionals/physician_gls/. (Accessed 17 January 2020).
- [6].Meyer LA, Bohlke K, Powell MA, Fader AN, Franklin GE, Lee LJ, Matei D, Coallier L, Wright AA, Postoperative radiation therapy for endometrial cancer: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Society for Radiation Oncology Evidence-Based Guideline, J. Clin. Oncol 33 (2015) 2908–2913. [DOI] [PubMed] [Google Scholar]
- [7].Pecorelli S, Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium, Int. J. Gynaecol. Obstet 105 (2009) 103–104. [DOI] [PubMed] [Google Scholar]
- [8].Takahashi K, Yunokawa M, Sasada S, Takehara Y, Miyasaka N, Kato T, Tamura K, A novel prediction score for predicting the baseline risk of recurrence of stage I-II endometrial carcinoma, J. Gynecol. Oncol 30 (2019), e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Matsuo K, Yabuno A, Hom MS, Shida M, Kakuda M, Adachi S, Mandelbaum RS,Ueda Y, Hasegawa K, Enomoto T, Mikami M, Roman LD, Significance of abnormal peritoneal cytology on survival of women with stage I-II endometrioid endometrial cancer, Gynecol. Oncol 149 (2018) 301–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Tate K, Yoshida H, Ishikawa M, Uehara T, Ikeda SI, Hiraoka N, Kato T, Prognostic factors for patients with early-stage uterine serous carcinoma without adjuvant therapy, J. Gynecol. Oncol 29 (2018), e34. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Seagle BL, Alexander AL, Lantsman T, Shahabi S, Prognosis and treatment of positive peritoneal cytology in early endometrial cancer: matched cohort analyses from the National Cancer Database, Am. J. Obstet. Gynecol 218 (2018) (329.e321–329.e315). [DOI] [PubMed] [Google Scholar]
- [12].Scott SA, van der Zanden C, Cai E, McGahan CE, Kwon JS, Prognostic significance of peritoneal cytology in low-intermediate risk endometrial cancer, Gynecol. Oncol 145 (2017) 262–268. [DOI] [PubMed] [Google Scholar]
- [13].Shiozaki T, Tabata T, Yamada T, Yamamoto Y, Yamawaki T, Ikeda T, Does positive peritoneal cytology not affect the prognosis for stage I uterine endometrial cancer?: the remaining controversy and review of the literature, Int. J. Gynecol. Cancer 24 (2014) 549–555. [DOI] [PubMed] [Google Scholar]
- [14].Haltia UM, Butzow R, Leminen A, Loukovaara M, FIGO 1988 versus 2009 staging for endometrial carcinoma: a comparative study on prediction of survival and stage distribution according to histologic subtype, J. Gynecol. Oncol 25 (2014) 30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Garg G, Gao F, Wright JD, Hagemann AR, Mutch DG, Powell MA, Positive peritoneal cytology is an independent risk-factor in early stage endometrial cancer, Gynecol. Oncol 128 (2013) 77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bansal S, Buck AM, Herzog TJ, Deutsch I, Burke WM, Wright JD, Stage IIIA endometrial carcinoma: outcome and predictors of survival, Obstet. Gynecol 114 (2009) 100–105. [DOI] [PubMed] [Google Scholar]
- [17].Metindir J, Dilek G Bilir, Positive peritoneal cytology and its prognostic value in endometrioid adenocancer confined to the uterus, Oncologie. 10 (2008) 348–351. [Google Scholar]
- [18].Havrilesky LJ, Cragun JM, Calingaert B, Alvarez Secord A, Valea FA, Clarke-Pearson DL, Berchuck A, Soper JT, The prognostic significance of positive peritoneal cytology and adnexal/serosal metastasis in stage IIIA endometrial cancer, Gynecol. Oncol 104 (2007) 401–405. [DOI] [PubMed] [Google Scholar]
- [19].Saga Y, Imai M, Jobo T, Kuramoto H, Takahashi K, Konno R, Ohwada M, Suzuki M, Is peritoneal cytology a prognostic factor of endometrial cancer confined to the uterus? Gynecol. Oncol 103 (2006) 277–280. [DOI] [PubMed] [Google Scholar]
- [20].Tebeu PM, Popowski Y, Verkooijen HM, Bouchardy C, Ludicke F, Usel M, Major AL, Positive peritoneal cytology in early-stage endometrial cancer does not influence prognosis, Br. J. Cancer 91 (2004) 720–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kasamatsu T, Onda T, Katsumata N, Sawada M, Yamada T, Tsunematsu R, Ohmi K, Sasajima Y, Matsuno Y, Prognostic significance of positive peritoneal cytology in endometrial carcinoma confined to the uterus, Br. J. Cancer 88 (2003) 245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].National Cancer Institute’s The Surveillance, Epidemiology, and End Results (SEER) Program, http://seer.cancer.gov/. (Accessed 16 January 2020).
- [23].National Cancer Registrars Association, http://www.ncra-usa.org/i4a/pages/index.cfm?pageid=1%3e. (Accessed 16 January 2020).
- [24].Corpus carcinoma. CS site-specific factor 2 peritoneal cytology, http://web2.facs.org/cstage0205/corpuscarcinoma/CorpusCarcinoma_kpo.html. (Accessed 18 January 2020).
- [25].Jamison PM, Altekruse SF, Chang JT, Zahn J, Lee R, Noone AM, Barroilhet L, Site-specific factors for cancer of the corpus uteri from SEER registries: collaborative stage data collection system, version 1 and version 2, Cancer 120 (Suppl. 23) (2014) 3836–3845. [DOI] [PubMed] [Google Scholar]
- [26].Matsuo K, Machida H, Blake EA, Holman LL, Rimel BJ, Roman LD, Wright JD, Trends and outcomes of women with synchronous endometrial and ovarian cancer, Oncotarget. 9 (2018) 28757–28771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].American Joint Committee on Cancer, https://cancerstaging.org/Pages/default.aspx. (Accessed 18 February 2020).
- [28].Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R, Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials, Int. J. Radiat. Oncol. Biol. Phys 37 (1997) 745–751. [DOI] [PubMed] [Google Scholar]
- [29].Austin PC, Stuart EA, Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies, Stat. Med 34 (2015) 3661–3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hershman DL, Wright JD, Comparative effectiveness research in oncology methodology: observational data, J. Clin. Oncol 30 (2012) 4215–4222. [DOI] [PubMed] [Google Scholar]
- [31].Cohen J, Statistical Power Analysis for the Behavioral Sciences, 2nd ed Erlbaum, Hillsdale, NJ, 1988. [Google Scholar]
- [32].Randall ME, Filiaci V, McMeekin DS, von Gruenigen V, Huang H, Yashar CM, Mannel RS, Kim JW, Salani R, DiSilvestro PA, Burke JJ, Rutherford T, Spirtos NM, Terada K, Anderson PR, Brewster WR, Small W, Aghajanian CA, Miller DS, Phase III trial: adjuvant pelvic radiation therapy versus vaginal brachytherapy plus paclitaxel/carboplatin in high-intermediate and high-risk early stage endometrial cancer, J. Clin. Oncol 37 (2019) 1810–1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].de Boer SM, Powell ME, Mileshkin L, Katsaros D, Bessette P, Haie-Meder C, Ottevanger PB, Ledermann JA, Khaw P, D’Amico R, Fyles A, Baron MH, Jurgenliemk-Schulz IM, Kitchener HC, Nijman HW, Wilson G, Brooks S, Gribaudo S, Provencher D, Hanzen C, Kruitwagen RF, Smit V, Singh N, Do V, Lissoni A, Nout RA, Feeney A, Verhoeven-Adema KW, Putter H, Creutzberg CL, Adjuvant chemoradiotherapy versus radiotherapy alone in women with high-risk endometrial cancer (PORTEC-3): patterns of recurrence and post-hoc survival analysis of a randomised phase 3 trial, Lancet Oncol. 20 (2019) 1273–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Matsuo K, Takazawa Y, Ross MS, Elishaev E, Podzielinski I, Yunokawa M, Sheridan TB, Bush SH, Klobocista MM, Blake EA, Takano T, Matsuzaki S, Baba T, Satoh S, Shida M, Nishikawa T, Ikeda Y, Adachi S, Yokoyama T, Takekuma M, Fujiwara K, Hazama Y, Kadogami D, Moffitt MN, Takeuchi S, Nishimura M, Iwasaki K, Ushioda N, Johnson MS, Yoshida M, Hakam A, Li SW, Richmond AM,Machida H, Mhawech-Fauceglia P, Ueda Y, Yoshino K, Yamaguchi K, Oishi T, Kajiwara H, Hasegawa K, Yasuda M, Kawana K, Suda K, Miyake TM, Moriya T, Yuba Y, Morgan T, Fukagawa T, Wakatsuki A, Sugiyama T, Pejovic T, Nagano T, Shimoya K, Andoh M, Shiki Y, Enomoto T, Sasaki T, Fujiwara K, Mikami M, Shimada M, Konishi I, Kimura T, Post MD, Shahzad MM, Im DD, Yoshida H, Omatsu K, Ueland FR, Kelley JL, Karabakhtsian RG, Roman LD, Significance of histologic pattern of carcinoma and sarcoma components on survival outcomes of uterine carcinosarcoma, Ann. Oncol 27 (2016) 1257–1266. [DOI] [PubMed] [Google Scholar]
- [35].Rauh-Hain JA, Starbuck KD, Meyer LA, Clemmer J, Schorge JO, Lu KH, Del Carmen MG, Patterns of care, predictors and outcomes of chemotherapy for uterine carcinosarcoma: a National Cancer Database analysis, Gynecol. Oncol 139 (2015) 84–89. [DOI] [PubMed] [Google Scholar]
- [36].Mysona DP, Tran LKH, Tran PMH, Gehrig PA, Van Le L, Ghamande S, Rungruang BJ, Java J, Mann AK, Liao J, Kapp DS, Santos BD, She JX, Chan JK, Clinical calculator predictive of chemotherapy benefit in stage 1A uterine papillary serous cancers, Gynecol. Oncol 156 (2020) 77–84. [DOI] [PubMed] [Google Scholar]
- [37].Felix AS, Brinton LA, McMeekin DS, Creasman WT, Mutch D, Cohn DE, Walker JL, Moore RG, Downs LS, Soslow RA, Zaino R, Sherman ME, Relationships of tubal ligation to endometrial carcinoma stage and mortality in the NRG oncology/gynecologic oncology group 210 trial, J. Natl. Cancer Inst 107 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Han KH, Park NH, Kim HS, Chung HH, Kim JW, Song YS, Peritoneal cytology: a risk factor of recurrence for non-endometrioid endometrial cancer, Gynecol. Oncol 134 (2014) 293–296. [DOI] [PubMed] [Google Scholar]
- [39].Creasman WT, Ali S, Mutch DG, Zaino RJ, Powell MA, Mannel RS, Backes FJ, DiSilvestro PA, Argenta PA, Pearl ML, Lele SB, Guntupalli SR, Waggoner S, Spirtos N, Boggess JF, Edwards RP, Filiaci VL, Miller DS, Surgical-pathological findings in type 1 and 2 endometrial cancer: an NRG Oncology/Gynecologic Oncology Group study on GOG-210 protocol, Gynecol. Oncol 145 (2017) 519–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Chang YN, Zhang Y, Wang YJ, Wang LP, Duan H, Effect of hysteroscopy on the peritoneal dissemination of endometrial cancer cells: a meta-analysis, Fertil. Steril 96 (2011) 957–961. [DOI] [PubMed] [Google Scholar]
- [41].Polyzos NP, Mauri D, Tsioras S, Messini CI, Valachis A, Messinis IE, Intraperitoneal dissemination of endometrial cancer cells after hysteroscopy: a systematic review and meta-analysis, Int. J. Gynecol. Cancer 20 (2010) 261–267. [DOI] [PubMed] [Google Scholar]
- [42].Matei D, Filiaci V, Randall ME, Mutch D, Steinhoff MM, DiSilvestro PA, Moxley KM, Kim YM, Powell MA, O’Malley DM, Spirtos NM, Small W Jr., K.S. Tewari, W.E. Richards, J. Nakayama, U.A. Matulonis, H.Q. Huang, D.S. Miller, Adjuvant chemotherapy plus radiation for locally advanced endometrial cancer, N. Engl. J. Med 380 (2019) 2317–2326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Matsuo K, Matsuzaki S, Nusbaum DJ, Machida H, Nagase Y, Grubbs BH, Roman LD, Wright JD, Harter P, Klar M, Malignant peritoneal cytology and decreased survival of women with stage I endometrioid endometrial cancer, Eur. J. Cancer 133 (2020) 33–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


