Abstract
Background
COVID-19 caused by SARS-CoV-2 virus emerged as an unprecedented challenge to discover effective drugs for its prevention and cure. Hyperinflammation-induced lung damage is one of the poor prognostic indicators causing a higher rate of morbidity and mortality of COVID-19 patients. Favipiravir, an antiviral drug, is being used for COVID-19 treatment, and we currently have limited information regarding its efficacy and safety. Thus, the present study was undertaken to evaluate the adverse drug events (ADEs) reported in the WHO pharmacovigilance database.
Methods
This study analyzed all suspected ADEs related to favipiravir reported from 2015. The reports were analyzed based on age, gender, and seriousness of ADEs at the System Organ Classification (SOC) level and the individual Preferred Term (PT) level.
Results
This study is based on 194 ADEs reported from 93 patients. Most frequent ADEs suspected to be caused by the favipiravir included increased hepatic enzymes, nausea and vomiting, tachycardia, and diarrhea. Severe and fatal ADEs occurred more frequently in men and those over the age of 64 years. Blood and lymphatic disorders, cardiac disorders, hepatobiliary disorders, injury poisoning, and procedural complications were more common manifestations of severe ADEs.
Conclusion
This study revealed that favipiravir appears to be a relatively safe drug. An undiscovered anti-inflammatory activity of favipiravir may explain the improvement in critically ill patients and reduce inflammatory markers. Currently, the data is based on very few patients. A more detailed assessment of the uncommon ADEs needs to be analyzed when more information will be available.
Keywords: favipiravir, usage, SARS-Cov-2, scrutiny, assumed, adverse drug events, described, World Health Organization, record
Introduction
“The COVID-19 created a health emergency that the world was not prepared for. Physicians had to repurpose previous drugs to supplement the standard medical management to maximize health outcomes.”1
COVID-19 originated in Wuhan, China, at the end of 2019 and was declared a global pandemic by WHO on 12-March-2020.2,3 It is caused by a virus identified as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).4 Over nine months since the first cases emerged, COVID-19 has caused a substantial increase in morbidity and mortality worldwide. As of 7-September-2020, there have been 27,032,617 confirmed cases and 881,464 deaths globally related to COVID-19.5
The current approaches to curbing the disease spread include maintaining hygiene, social distancing, quarantine, and sealing of containment areas.6–12 At present, there is no specific drug or vaccine available for SARS-CoV-2 infection.13 The researchers worldwide face daunting challenges of developing safe and effective vaccines and medicines for COVID-19. Over 190 vaccines are currently being tested for COVID-19, out of which 42 are being tested on humans in clinical trials.14 Based on experience, drug or vaccine discovery and development is risky and time-consuming, and effective regulation is required to ensure new drugs’ safety and efficacy.15 Thus, an estimation on when we will have an efficacious drug for the prevention or treatment of COVID-19 is surrounded by considerable uncertainty.
The researchers are working on repurposing existing antiviral therapies for the treatment of COVID-19. Hydroxychloroquine, remdesivir, lopinavir, ritonavir, and favipiravir are some existing drugs being explored for COVID-19 treatment.16 Nevertheless, the results of repurposing prevailing antiviral were not acceptable level in COVID-19 patients especially with diabetes mellitus, hypertension, CVS, renal failure, liver cirrhosis, stroke, and other co-morbidities.1 Before the emergence of SARS-CoV-2, six other family members Coronaviridae have been known to cause infections in humans, including the SARS-CoV infection, which was first reported in 2002, and the Middle East Respiratory Syndrome (MERS)-CoV infection in 2012.17,18 Since the genome sequence of SARS-CoV-2 is known to have about 75%–80% similarity with SARS-CoV, and even more so with some of the bat coronaviruses, significant efforts are indulged in testing the efficacy of existing antiviral drugs for SARS-CoV-2 infection treatment, including those with proven efficacy in other viral infections, such as ribavirin, lopinavir (ritonavir), interferon, and favipiravir.19
Favipiravir (IUPAC name: 5-fluoro-2-oxo-1H-pyrazine-3-carboxamide) is an antiviral prodrug with active metabolite favipiravir ribofuranosyl-5ʹ-triphosphate. It inhibits viral replication by arresting RNA polymerase.20 Although most of the preclinical safety and efficacy data for favipiravir are derived from the studies that have proven its antiviral activity against Ebola and influenza viruses, it has also shown efficacy against SARS-CoV-2 infection.16,21 A recent in vitro study performed by Wang et al revealed that, in Vero E6 cells, favipiravir virtually affects SARS-CoV-2 in 50% effective concentration of 61.88 μM/L.22 These preclinical and in vitro findings provide grounds for optimism concerning COVID-19 treatment with favipiravir on an emergency and compassionate use basis in many countries.16,22 Additionally, favipiravir’s overall safety profile is reasonably good, especially of total and severe ADEs. Nevertheless, safety apprehensions that remain with hyperuricemia, teratogenicity, and QTc prolongation have not yet been satisfactorily assessed. Researchers furthermore advised that although favipiravir should be utilized for the minimum duration for COVID-19 cases. Finally, this research advocated for more evidence is required to evaluate the longer-term effects of treatment because of yet limited data available regarding unsettled safety concerns. Hereafter, physicians need to be very careful and alert while utilizing favipiravir against COVID-19.23
Favipiravir (T-705) was first synthesized in 2005 by the chemical substitution of a pyrazine analog and initially tested in vitro for anti-influenza virus activity in cells. Subsequently, it was approved for clinical use in drug-resistant influenza strains.24 Favipiravir was approved for clinical use in Japan in 2014 to treat novel or re-emerging influenza virus infections, unresponsive or insufficiently responsive to existing antiviral agents.25 Favipiravir, which is a prodrug, is activated into favipiravir ibofuranosyl-5′-triphosphate (T-705-RTP) through intracellular modifications, such as ribosylation and phosphorylation. It blocks the RNA-dependent RNA polymerase (RdRp) action required to facilitate the virus’ transcription process by competing with purine nucleosides and incorporating into the viral RNA, hence halting the viral replication.26 The researchers investigated the efficacy of favipiravir in treating various pathogens, including Ebola, Lassa, and now SARS-Cov-2 viruses.20,26
Favipiravir has a well-established safety profile and has not been reported to possess any severe ADEs. A Spanish study reported favipiravir as a well-tolerated substance, without severe adverse effects even when used in high doses (50 mg/kg).27 Other studies demonstrated a lower proportion of grade 1–4 ADEs, gastrointestinal ADEs, serious ADEs, and a better overall safety profile of favipiravir than placebo. The most frequent adverse effects reported in clinical trials were increased serum uric acid level, diarrhea, decreased neutrophil count, and raised liver transaminases (AST and ALT).23 It has been documented that favipiravir manifests a good safety profile concerning the total and severe ADEs, and it might rarely induce drug-related psychotic symptoms.28 Due to the limited availability of the data, robust multicentric randomized controlled trials are warranted to establish the safety and efficacy of favipiravir against SARS-CoV-2. In the trials conducted until now, diarrhea, hyperuricemia, and liver toxicity are the typical adverse reactions of favipiravir.29 Despite being used in many countries on emergency grounds for COVID-19 management, the safety of favipiravir is still under investigation. Globally, the health professionals report ADEs encountered during the use of favipiravir for COVID-19 in the global database VigiBase® maintained by WHO.30
Consequently, it is essential to review ADEs’ current status associated with favipiravir reported by health professionals who prescribe favipiravir to their patients for COVID-19 management. Thus, the present study was undertaken to evaluate the ADEs of favipiravir used for COVID-19 treatment, as reported in the WHO pharmacovigilance database.
Materials and Methods
The authors used VigiBase for the study, which is a global database maintained by WHO. It contains individual case safety reports (ICSRs) of ADEs reported by health professionals. It is the most extensive database in existence since 1968, having over 20 million reports of suspected ADEs of medicines, reported by the member countries of the WHO Program for International Drug Monitoring.30 VigiBase is a repository of all ICSRs of ADEs collected by the national pharmacovigilance centers of over 130 countries.30,31 VigiBase contains reports in a structured form containing information regarding patient demographics (age, gender, continent, and country of residence), drugs (start date, end date, route of administration, and indication for use), suspected ADEs (date of onset, seriousness, causality, and outcome), and administrative data (a type of report and source of report). In this database, the medicines are coded according to the WHO Drug Dictionary Enhanced, including the Anatomical Therapeutic Chemical (ATC) classification.32 ADEs were coded according to the WHO Adverse Reaction Terminology and the Medical Dictionary for Regulatory Authorities (MedDRA).33 The International Council developed MedDRA for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH). It includes highly specific standardized medical terminology to facilitate the global sharing of uniform regulatory information for medical products used by humans.34 It consists of the five levels to the MedDRA hierarchy, which are arranged from very specific to very general levels: LTTs (Lowest Level Terms), PTs (Preferred Terms), HLTs (High-Level Terms), HLGTs (High-Level Group Terms), and SOCs (System Organ Classes).35
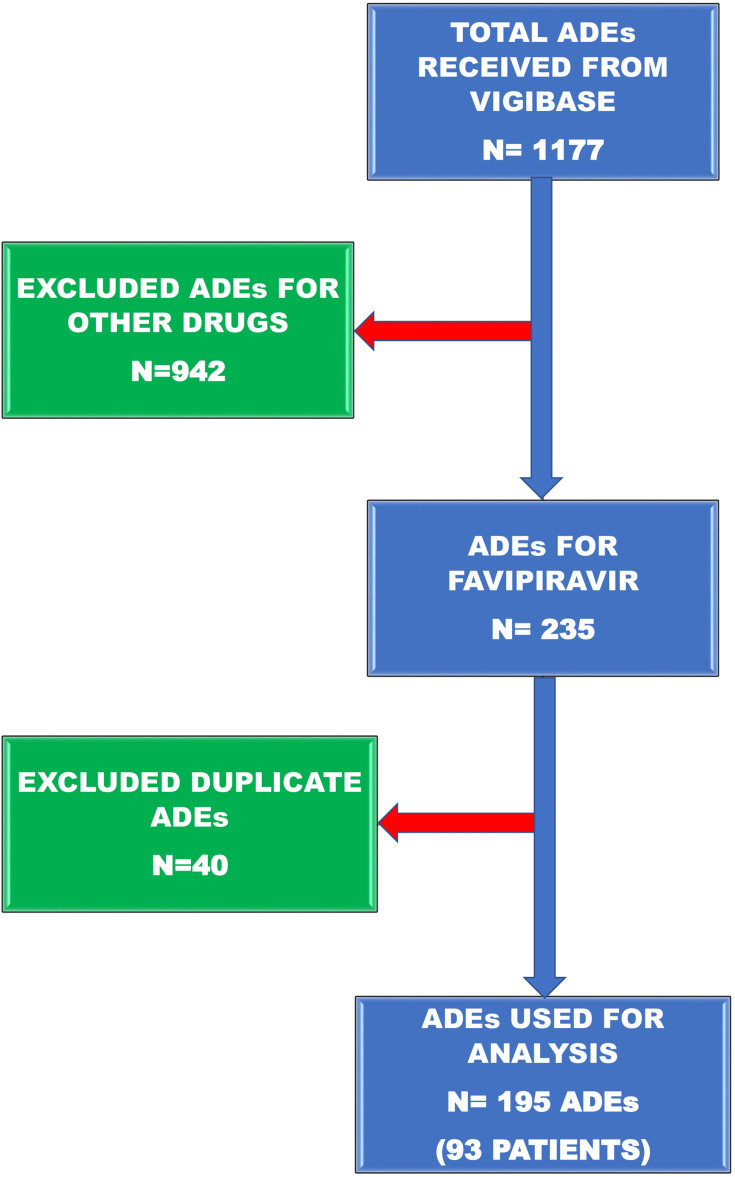
In the present analysis, we have used PT and SOC information. PTs are the specific terms for a particular symptom, disease, therapeutic indication, investigation, surgical or medical procedure, and medical social or family history characteristics.36 SOCs are the grouping of PTs as per etiology (eg, infections and infestations), manifestation sites (eg, gastrointestinal disorders), or purpose (eg, surgical and medical procedures). Besides, there is a SOC to contain issues related to products and one to contain social circumstances. This study included the analysis of all suspected ADEs of favipiravir notified when used to treat COVID-19. Each report in VigiBase refers to a single individual who may have encountered one or several ADEs simultaneously. As a result, the number of reported ADEs could be higher than the number of patients for whom the case reports were documented. ADEs was classified following the Medical Dictionary for Regulatory Authorities (MedDRA) and grouped at the SOC and individual PT levels. The schematic flowchart of ADEs selection is depicted in Figure 1.
Figure 1.
Schematic diagram of adverse drug events selection from Vigibase data used to filter the records.
Statistical Analysis
Descriptive statistics were reported in the form of frequency and percentages. Statistical Package for Social Science version 17 was used for the analysis.
Ethical Approval
This study was based on the WHO’s database and did not involve direct interaction with human participants; hence ethical approval was not required.
Results
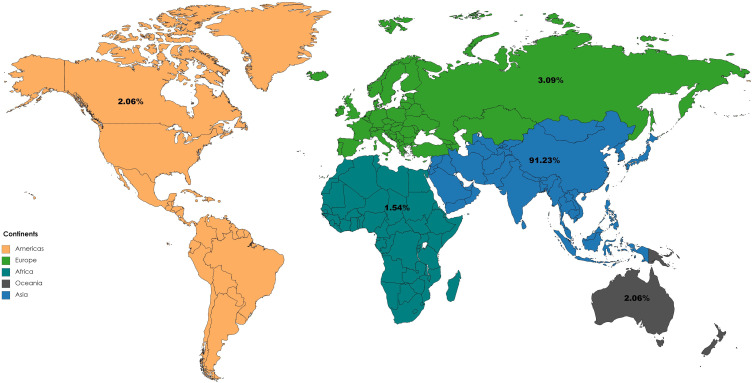
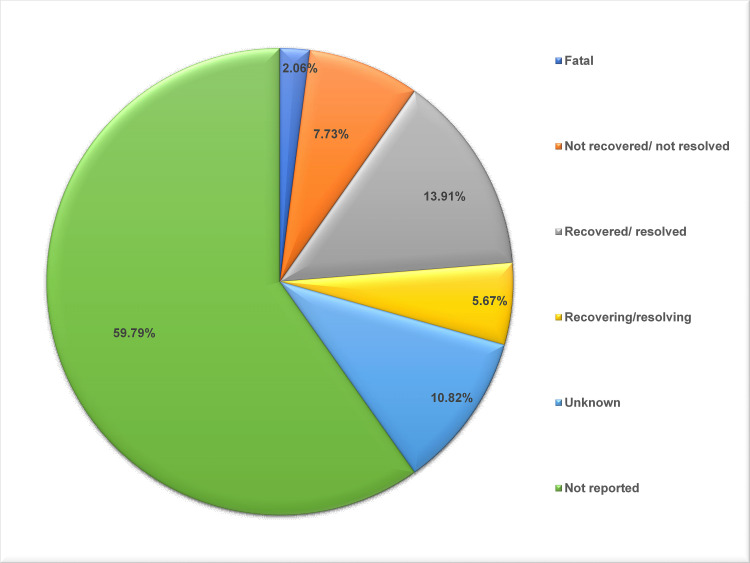
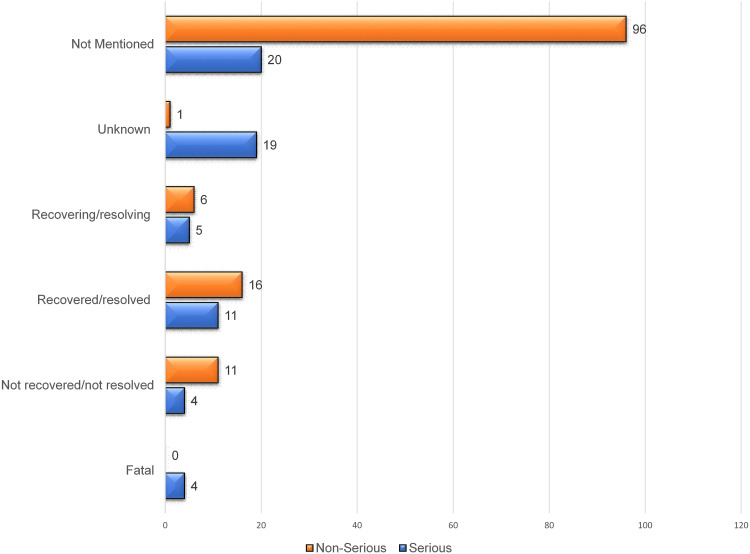
This study is based on 194 ADEs reported from 93 patients. In almost all cases, the drug was given to treat COVID-19. The male gender and age group of 18–64 years old made up the majority of cases. The majority of these ADEs were reported from Asia (N=177), followed by Europe (N=6), Americas (N=4), Oceania (N=4), and Africa (N=3) [Figure 2]. Around one-third of the ADEs were severe, and the drug was given predominantly through the oral route. On analyzing the outcomes of the ADEs, the majority were not reported (N=116) followed by recovered/resolved (N=27), unknown (N=21), not recovered/not resolved (N=15), recovering/resolving (N=11), and fatal in four cases [Figure 3]. Variables usually used for assessment of the causality were reported incompletely (Table 1). Most frequent adverse events suspected to be caused by the favipiravir were increased in the hepatic enzymes, nausea and vomiting, tachycardia, and diarrhea (Table 2).
Figure 2.
Distribution of Adverse Drug events reported with Favipiravir use in COVID-19 across continents in Vigibase.
Figure 3.
Adverse drug event outcomes of Favipiravir use in COVID-19.
Table 1.
Characteristics of Adverse Drug Events (194 ADEs Reported from 93 Individuals) Reported for Favipiravir in WHO Database
| Parameters | Frequency (%) | |
|---|---|---|
| Age (N = 194) | <18 Years | 2 (1.03) |
| 18–64 Years | 131 (67.52) | |
| ≥65 Years | 48 (24.74) | |
| Not reported | 13 (6.70) | |
| Gender (N = 194) | Female | 75 (38.66) |
| Male | 118 (60.82) | |
| Not reported | 1 (0.5) | |
| The seriousness of ADE (N =194) | Serious | 63 (32.47) |
| Non-Serious | 130 (67.01) | |
| Not reported | 1 (0.51) | |
| Route of Administration (N =194) | Oral | 182 (93.81) |
| Unknown | 8 (4.12) | |
| Not reported | 4 (2.06) | |
| Dechallenge Action (N =194) | Does not changed | 14 (7.21) |
| Drug has withdrawn | 29 (14.94) | |
| Unknown | 22 (11.34) | |
| Not reported | 129 (66.49) | |
| Dechallenge Outcome (N =194) | Fatal | 1 (0.51) |
| No effect observed | 7 (3.60) | |
| Reaction abated | 14 (7.21) | |
| Effect unknown | 19 (9.79) | |
| Not Reported | 153 (78.86) | |
| Rechallenge Action (N=194) | Rechallenge | 3 (1.54) |
| Not Reported | 191 (98.45) | |
| Rechallenge Outcome (N=194) | Effect unknown | 3 (1.54) |
| Not Reported | 191 (98.45) |
Table 2.
Adverse Drug Events Suspected to Be Caused by Favipiravir, as Reported in the WHO Database (N=93)
| Adverse Drug Events | Frequency |
|---|---|
| Intentional product use issue | 65 (69.89) |
| Hepatic enzyme increased | 22 (23.66) |
| Nausea and Vomiting | 13 (13.98) |
| Tachycardia | 9 (9.68) |
| Diarrhoea | 7 (7.52) |
| Electrocardiogram QT prolonged | 5 (5.37) |
| Headache | 5 (5.37) |
| Pruritus | 5 (5.37) |
| Rash | 5 (5.37) |
| Erythema | 4 (4.30) |
| Hepatotoxicity | 4 (4.30) |
| Thrombocytopenia | 4 (4.30) |
| Bradycardia | 3 (3.22) |
| Abdominal pain | 2 (2.15) |
| Abdominal pain upper | 2 (2.15) |
| Constipation | 2 (2.15) |
| Hypotension | 2 (2.15) |
| Rash maculopapular | 2 (2.15) |
| Anemia | 2 (2.15) |
| Acute kidney injury | 1 (1.07) |
| Arthritis | 1 (1.07) |
| Asthenia | 1 (1.07) |
| Atrial fibrillation | 1 (1.07) |
| Bronchospasm | 1 (1.07) |
| Colitis | 1 (1.07) |
| Cough | 1 (1.07) |
| Cystic fibrosis | 1 (1.07) |
| Death | 1 (1.07) |
| Dizziness | 1 (1.07) |
| Dyspnoea | 1 (1.07) |
| Hemorrhage | 1 (1.07) |
| Hair color changes | 1 (1.07) |
| Hepatic function abnormal | 1 (1.07) |
| Hyperglycaemia | 1 (1.07) |
| Hypersensitivity | 1 (1.07) |
| Hypertension | 1 (1.07) |
| Leukopenia | 1 (1.07) |
| Muscle contractions involuntary | 1 (1.07) |
| Musculoskeletal pain | 1 (1.07) |
| Nail discoloration | 1 (1.07) |
| Palpitations | 1 (1.07) |
| Purpura | 1 (1.07) |
| Pyrexia | 1 (1.07) |
| Respiratory distress | 1 (1.07) |
| Rhabdomyolysis | 1 (1.07) |
| Seizure | 1 (1.07) |
| Syncope | 1 (1.07) |
| Urticaria | 1 (1.07) |
| Vasculitis | 1 (1.07) |
| Visual impairment | 1 (1.07) |
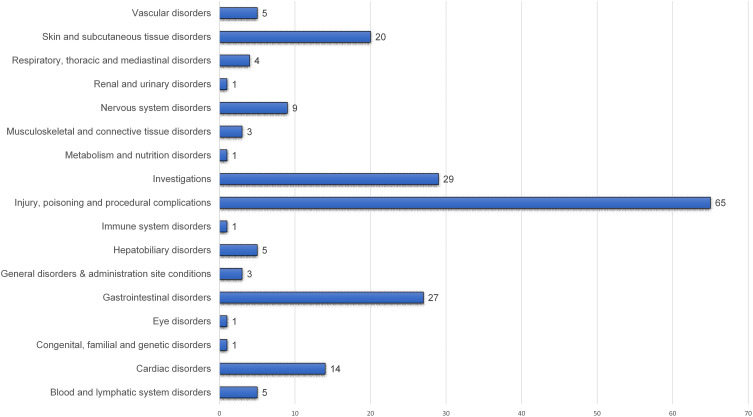
Serious ADEs were more common among those aged 64 and above than those aged below 64 (48% vs 26%, respectively). Skin and subcutaneous tissue disorders and gastrointestinal disorders were more prevalent, while blood and lymphatic disorders and nervous system disorders were less prevalent among those aged below 64 than among those aged 64 and above. The organ system-wise distribution of ADEs is presented in Figure 4. The probability of recovery was higher among patients aged below 64 than among those aged 64 and above (Table 3). Severe ADEs were more prevalent in males than females (68% vs 32%, respectively). Blood and lymphatic disorders, cardiac disorders, hepatobiliary disorders, injury poisoning, and procedural complications were more common in those with severe ADEs than those with non-serious ADEs (Table 4). All fatal ADEs were severe, and most non-serious ADEs were not mentioned [Figure 5].
Figure 4.
System-wise distribution of ADEs attributed to Favipiravir use in COVID-19.
Table 3.
Distribution of Characteristics of Different Adverse Drug Events Suspected to Be Caused by Favipiravir Between Age <64 and >64 Years
| Parameters | Age <64 (N=133) | Age 64 and Above (N = 48) | Age Unknown (N = 13) |
|---|---|---|---|
| Seriousness | |||
| Serious (N = 63) | 35 (26.31) | 23 (47.91) | 5 (38.46) |
| Non-serious (N = 130) | 98 (73.68) | 25 (52.08) | 7 (53.84) |
| ADE organ system | |||
| Blood and lymphatic system disorders (N=5) | 3 (2.25) | 2 (4.1) | 0 |
| Cardiac disorders (N=14) | 9 (6.76) | 3 (6.25) | 2 (15.38) |
| Congenital, familial and genetic disorders (N = 1) | 1 (0.75) | 0 | 0 |
| Eye disorders (N=1) | 1 (0.75) | 0 | 0 |
| Gastrointestinal disorders (N=27) | 20 (15.03) | 6 (12.5) | 1 (7.69) |
| General disorders and administration site conditions (N = 3) | 2 (1.50) | 0 | 1 (7.69) |
| Hepatobiliary disorders (N = 5) | 4 (3.0) | 1 (2.08) | 0 |
| Immune system disorders (N = 1) | 1 (0.75) | 0 | 0 |
| Injury, poisoning and procedural complications (N = 65) | 44 (33.0) | 18 (37.5) | 3 (23.0) |
| Investigations (N = 29) | 21 (15.78) | 7 (14.58) | 1 (7.69) |
| Metabolism and nutrition disorders (N = 1) |
1 (0.75) | 0 | 0 |
| Musculoskeletal and connective tissue disorders (N = 3) | 1 (0.75) | 2 (4.16) | 0 |
| Nervous system disorders (N = 9) | 5 (3.75) | 3 (6.25) | 1 (7.69) |
| Renal and urinary disorders (N = 1) | 0 | 1 (2.08) | 0 |
| Respiratory, thoracic and mediastinal disorders (N = 4) | 1 (0.75) | 3 (6.25) | 0 |
| Skin and subcutaneous tissue disorders (N = 20) |
18 (13.53) | 1 (2.08) | 1 (2.08) |
| Vascular disorders (N = 5) | 1 (0.75) | 1 (2.08) | 3 (23.07) |
| Outcomes | |||
| Fatal (N =4) | 1 (0.75) | 0 | 3 (23.07) |
| Not recovered/Not resolved (N =15) | 8 (6.01) | 6 (12.50) | 1 (7.69) |
| Recovered/Resolved (N =27) | 18 (13.53) | 7 (14.58) | 2 (15.38) |
| Recovering/Resolving (N =11) | 10 (7.51) | 1 (2.08) | 0 |
| Unknown (N =21) | 16 (12.03) | 3 (6.25) | 2 (15.38) |
| Not Reported (N =116) | 80 (60.15) | 31 (64.58) | 5 (38.46) |
Table 4.
Comparison of Serious and Non-Serious Adverse Drug Events Suspected to Be Caused by Favipiravir Among Various Study Characteristics (N = 194)
| Parameters | Serious (N = 63) | Non-Serious (N = 130) | |
|---|---|---|---|
| Gender | Male (N = 118) | 43 (68.25) | 74 (56.92) |
| Female (N = 75) | 20 (31.74) | 55 (42.30) | |
| Gender Not mentioned (N =1) | 1 (0.76) | ||
| The system involved in ADEs | Blood and lymphatic system disorders (N = 5) | 3 (4.76) | 3 (2.30) |
| Cardiac disorders (N = 14) | 12 (19.04) | 2 (1.53) | |
| Congenital, familial and genetic disorders (N = 1) | 1 (1.58) | 0 | |
| Eye disorders (N = 1) | 0 | 1 (0.76) | |
| Gastrointestinal disorders (N = 3) | 1 (1.58) | 2 (1.53) | |
| General disorders and administration site conditions (N = 3) | 1 (1.58) | 2 (1.53) | |
| Hepatobiliary disorders (N = 5) | 5 (7.93) | 0 | |
| Immune system disorders (N = 1) | 0 | 1 (0.76) | |
| Injury, poisoning and procedural complications (N = 65) | 13 (20.63) | 52 (0.40) | |
| Investigations (N = 29) | 10 (15.87) | 19 (14.61) | |
| Metabolism and nutrition disorders (N = 1) | 0 | 1 (0.76) | |
| Musculoskeletal and connective tissue disorders (N = 3) | 1 (1.58) | 2 (1.53) | |
| Nervous system disorders (N = 9) | 2 (3.17) | 7 (5.38) | |
| Renal and urinary disorders (N = 1) | 1 (1.58) | 0 | |
| Respiratory, thoracic and mediastinal disorders (N = 4) | 1 (1.58) | 3 (2.30) | |
| Skin and subcutaneous tissue disorders (N = 20) | 0 | 20 (15.38) | |
| Vascular disorders (N = 5) | 3 (4.76) | 1 (0.76) | |
Figure 5.
Comparison of serious and non serious adverse drug events outcomes of Favipiravir use in COVID-19.
Discussion
“Worldwide, millions of people are infected, and thousands of deaths are occurring due to the pandemic situation of 250COVID-19. The identification of effective strategies against SARS-CoV-2 is a major challenge. Currently, we are fighting a twenty-first-century disease with twentieth-century weapons.”37
This study was designed to review ADEs reported for favipiravir in the WHO database. It was observed that the majority of ADEs were reported from male subjects and subjects aged between 45 and 64 years. Most of events were reported from Asia. For almost all ADEs, the indication for use was COVID-19. Evidence shows that the increase in viral load of SARS-CoV-2 has a close association with risen IL-6 levels.38 Raised IL-6 levels with cytokine storm can worsen prognosis and have a poor outcome with higher mortality.38,39 Favipiravir, being a potent inhibitor of viral proliferation, possibly causes diminished cytokine production, ultimately saving the lung from inflammatory damage and fibrosis, hence preventing impending hypoxemia and poor prognosis.40,41 Accordingly, few studies showed an improvement in the chest imaging in patients administered with favipiravir, which possibly points towards its action to minimize hyperinflammatory state and improve respiratory function in these critically ill COVID-19 patients.42
Since favipiravir is a comparatively new drug, few randomized clinical trials have been conducted, with limited information available about its post-approval safety and efficacy. As per the existing evidence, most of the research related to favipiravir has been conducted for its use in Ebola and influenza virus infections; favipiravir for COVID-19 is used either on compassionate or emergency grounds and as of now, there is no concrete evidence of antiviral activity of Favipiravir.21 Although several studies assessing the safety and efficacy of favipiravir in COVID-19 were initiated, the results for most of them have not yet been published. The case reports published so far indicate that the higher doses of favipiravir are required to mellow down the higher viral loads.43 A pharmacokinetic study of Favipiravir performed on seven patients indicated that the favipiravir concentration was much less in critically ill SARS-CoV2 patients than in the healthy volunteers.21,44 This finding is crucial as dose optimization may lead to favorable results with favipiravir in COVID-19. The results of five published clinical trials show that the most common adverse effects of favipiravir are diarrhea, raised liver enzymes, hyperuricemia, and QT prolongation.23,29,38 Prolongation of QT interval by favipiravir is controversial; it is reported to be the outcome of drug interactions of favipiravir with concomitant drugs rather than favipiravir alone. Further studies are required to elucidate the association of Favipiravir with the occurrence of QT prolongation.45,46
The results of our study exhibited that the majority of the ADEs were related to the investigations (16%), which primarily included raised liver function tests (23.66%) and QT prolongation (5.37%), followed by skin and subcutaneous tissue disorders (15.4%). Favipiravir is metabolized in the liver mainly by the enzyme named aldehyde oxidase, and the xanthine oxidase metabolizes a minor portion.47 There is evidence that the rise in liver enzymes is documented in ≥1% of the patients, and <0.5% of the patients also showed raised serum bilirubin, which points towards the suspected liver injury by the drug.48 There was a roughly 2.1 fold rise and 6.3 fold rise in the Cmax and AUC, respectively, when favipiravir was given to patients with severe liver dysfunction (Child-Pugh classification C) compared to healthy participants, which warrants a cautious use of favipiravir in patients with liver dysfunction.48,49 Hypersensitivity reactions, such as rashes, have been reported by 0.5% to <1% of the patients.48
Previous studies reported that hyperuricemia was not present in the ADE database of WHO, which was used to evaluate ADEs related to favipiravir in the current study.23,29,48,50,51 Evidence shows that hyperuricemia was seen in 4.79% of the patients, and drug–drug interaction with the co-administered drug (pyrazinamide) might be a possibility of risen serum uric acid.48 It is essential to notice that the WHO database is based on reported ADEs, and the quality of reporting cannot be compared with the documentation of ADEs in clinical trials.
The present study also points out that favipiravir’s adverse metabolic effects as one patient with hyperglycemia were reported. Evidence shows that among the adverse metabolic effects, glycosuria was reported in 0.5% to <1% of the patients, and ≥1% of the patients were found to have raised serum triglycerides with favipiravir.48 Favipiravir is not recommended in pregnant patients and should be avoided, as early embryonic deaths and teratogenicity have been reported in the preclinical studies. Nevertheless, there is a lack of adequate documented evidence on human pregnancy outcomes.48
Limitations of the Study
This study’s data were obtained from “VigiBase, the WHO global database of ICSRs,” which in turn receives the data from numerous sources. Therefore, the probability that the suspected adverse effect is drug-related is not the same in all cases. Also, there were many missing values of indication or causality assessment criteria; hence, these could not be included in the analysis.
Conclusion
The overall picture drawn from the present analysis and other studies conducted on favipiravir for COVID-19 treatment appears to be a relatively safe drug. Since SARS-CoV-2 is a novice virus, researchers worldwide are still decoding the virus and the pattern of the human body’s biochemical and pathological changes brought about by SARS-CoV-2. Moreover, most of the safety data for favipiravir are derived from studies on subjects with Ebola and influenza infections. Since the drug–disease interactions may differ, the ADEs related to the drug in different diseases may vary. These crucial facts should be considered while evaluating the safety of favipiravir for COVID-19 in further clinical studies. The current analysis depicts the snapshot based on limited data on the use of favipiravir in COVID-19. More extensive evidence is required to assess the long-term and uncommon adverse effects of favipiravir. Finally, “the SARS-CoV-2 pandemic caught the world by surprise and the only way to keep fighting it is by learning more about it.”52
Recommendations
Clinicians using favipiravir should monitor the rise of hepatic enzymes, ECG changes, and plausible drug interactions during the treatment to avoid ADE and attain preferable clinical outcomes.
Key Messages
Favipiravir is one of the promising drugs for the treatment of COVID – 19.
It is crucial to evaluate the efficacy and safety of this new drug based on available data.
Based on the WHO pharmacovigilance data report, the most common ADEs reported for favipiravir were a rise in the hepatic enzymes, nausea and vomiting, and tachycardia.
Patients should be monitored for the rise in hepatic enzymes and ECG changes during the treatment with favipiravir.
Acknowledgment
We want to acknowledge ‘mapchart.net’ to prepare a map diagram for our study, a free service. The authors are grateful to Professor (Dr.) M. S. Razzaque, MBBS, Ph.D. of Lake Erie College of Osteopathic Medicine, Pennsylvania, USA, for reading the manuscript and providing useful suggestions.
Funding Statement
This paper was not funded.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work and declare that they do not have any financial involvement or affiliations with any organization, association, or entity directly or indirectly with the subject matter or materials presented in this article. This includes honoraria, expert testimony, employment, ownership of stocks or options, patents or grants received or pending, or royalties.
References
- 1.Kandimalla R, John A, Abburi C, Vallamkondu J, Reddy PH. Current Status of Multiple Drug Molecules, and Vaccines: an Update in SARS-CoV-2 Therapeutics. Mol Neurobiol. 2020;57(10):4106–4116. doi: 10.1007/s12035-020-02022-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Guan X, Wu P, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Accessed October2, 2020 https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. [Google Scholar]
- 4.Ghinai I, McPherson TD, Hunter JC, et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020;395(10230):1137–1144. doi: 10.1016/s0140-6736(20)30607-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard [Updated Oct 4, 2020]. Accessed October6, 2020 https://covid19.who.int/.
- 6.Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. 2020;4(4):Cd013574. doi: 10.1002/14651858.Cd013574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Y LZ N, Chua YX, Chaw WL, et al. Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore - January 2-February 29, 2020. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 2020;69:307–311. doi: 10.15585/mmwr.mm6911e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bedford J, Enria D, Giesecke J, et al. COVID-19: towards controlling of a pandemic. Lancet. 2020;395(10229):1015–1018. doi: 10.1016/s0140-6736(20)30673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Affairs. 2020;39(7):1237–1246. doi: 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- 10.Pradhan D, Biswasroy P, Kumar Naik P, Ghosh G, Rath GA. A Review of Current Interventions for COVID-19 Prevention.Arch Med Res. 2020;51(5):363–374. doi: 10.1016/j.arcmed.2020.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogunleye OO, Basu D, Mueller D, et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: successes, Challenges, and Implications for the Future. Front Pharmacol. 2020;11:1205. doi: 10.3389/fphar.2020.01205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. COVID-19 Strategic Preparedness and Response Plan - Operational planning guidelines to support country preparedness and response. 2020. Accessed October6, 2020 https://www.who.int/docs/default-source/coronaviruse/covid-19-sprp-unct-guidelines.pdf.
- 13.Holder K, Reddy PH, The COVID-19. Effect on the Immune System and Mitochondrial Dynamics in Diabetes, Obesity, and Dementia. Neuroscientist. 2020;1073858420960443. doi: 10.1177/1073858420960443 [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Draft landscape of COVID-19 candidate vaccines. Accessed October8, 2020 2020. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 15.Mullard ACOVID-19. COVID-19 vaccine development pipeline gears up. Lancet. 2020;395(10239):1751–1752. doi: 10.1016/s0140-6736(20)31252-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu R, Wang L, Kuo HD, et al. An Update on Current Therapeutic Drugs Treating COVID-19. Curr Pharmacol Rep. 2020:1–15. doi: 10.1007/s40495-020-00216-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. SARS (Severe Acute Respiratory Syndrome). https://www.who.int/ith/diseases/sars/en/. Accessed October8, 2020
- 18.World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV). Accessed October10, 2020 https://www.who.int/health-topics/middle-east-respiratory-syndrome-coronavirus-mers#tab=tab_1.
- 19.Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/s0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.PubChem. Favipiravir. Bethesda (MD): National Library of Medicine (US) https://pubchem.ncbi.nlm.nih.gov/compound/Favipiravir. Accessed October10, 2020. [Google Scholar]
- 21.Dauby N. Favipiravir as an antiviral agent in COVID-19: same script, different cast? Clinical Infectious Diseases. 2020;ciaa1600. doi: 10.1093/cid/ciaa1600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30(3):269–271. doi: 10.1038/s41422-020-0282-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilkington V, Pepperrell T, Hill A. A review of the safety of favipiravir – a potential treatment in the COVID-19 pandemic? J Virus Erad. 2020;6(2):45–51. doi: 10.1016/s2055-6640(20)30016-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Furuta Y, Takahashi K, Kuno-Maekawa M, et al. Mechanism of action of T-705 against influenza virus. Antimicrobial Agents and Chemotherapy. 2005;49(3):981–986. doi: 10.1128/aac.49.3.981-986.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hayden FG, Shindo N. Influenza virus polymerase inhibitors in clinical development. Current Opinion in Infectious Diseases. 2019;32(2):176–186. doi: 10.1097/qco.0000000000000532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Furuta Y, Komeno T, Nakamura T. Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proceedings of the Japan Academy, Series B. 2017;93(7):449–463. doi: 10.2183/pjab.93.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borobia AM, Mora-Rillo M, Ramírez Olivencia G, et al. High dose favipiravir: first experience in a patient with Ebola. Clinical Therapeutics. 2015;37(8):e15. doi: 10.1016/j.clinthera.2015.05.054 [DOI] [Google Scholar]
- 28.Ghasemiyeh P, Borhani-Haghighi A, Karimzadeh I, et al. Major Neurologic Adverse Drug Reactions, Potential Drug-Drug Interactions, and Pharmacokinetic Aspects of Drugs Used in COVID-19 Patients with Stroke: A Narrative Review. Ther Clin Risk Manag. 2020;16:595–605. doi: 10.2147/tcrm.S259152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cai Q, Yang M, Liu D, et al. Experimental Treatment with Favipiravir for COVID-19: an Open-Label Control Study. Engineering. 2020. doi: 10.1016/j.eng.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Uppsala Monitoring Centre: WHO Programme for International Drug Monitoring. VigiBase. Accessed October12, 2020 https://www.who-umc.org/vigibase/vigibase/.
- 31.Uppsala Monitoring Centre. VigiBase: signaling harm and pointing to safer use. Accessed October12 2020 https://www.who-umc.org/vigibase/vigibase/vigibase-signalling-harm-and-pointing-to-safer-use/.
- 32.World Health Organization. WHO Collaborating Centre for Drug Statistics Methodology. Accessed October12, 2020 https://www.whocc.no/.
- 33.Brown EG, Wood L, Wood S. The medical dictionary for regulatory activities (MedDRA). Drug Saf. 1999;20(2):109–117. doi: 10.2165/00002018-199920020-00002 [DOI] [PubMed] [Google Scholar]
- 34.International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). Medical Dictionary for Regulatory Activities(MedDRA). https://www.meddra.org/how-to-use/support-documentation/english/welcome. Accessed October14, 2020
- 35.International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH). MedDRA Hierarchy. Accessed October14, 2020 https://www.meddra.org/how-to-use/basics/hierarchy.
- 36.Uppsala Monitoring Centre. Glossary of pharmacovigilance terms. Accessed October14, 2020 https://www.who-umc.org/global-pharmacovigilance/publications/glossary/.
- 37.Bhatti JS, Bhatti GK, Khullar N, Reddy AP, Reddy PH. Therapeutic Strategies in the Development of Anti-viral Drugs and Vaccines Against SARS-CoV-2 Infection. Mol Neurobiol. 2020;57(11):4856–4877. doi: 10.1007/s12035-020-02074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen X, Zhao B, Qu Y, et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated With Drastically Elevated Interleukin 6 Level in Critically Ill Patients With Coronavirus Disease 2019. Clin Infect Dis. 2020;71(8):1937–1942. doi: 10.1093/cid/ciaa449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Medicine. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Takahashi H, Iwasaki Y, Watanabe T, et al. Case studies of SARS-CoV-2 treated with favipiravir among patients in critical or severe condition. Int J Infect Dis. 2020;100:283–285. doi: 10.1016/j.ijid.2020.08.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yamamura H, Matsuura H, Nakagawa J, Fukuoka H, Domi H, Chujoh S. Effect of favipiravir and an anti-inflammatory strategy for COVID-19. Crit Care. 2020;24(1):413. doi: 10.1186/s13054-020-03137-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Takahashi K, Furuta Y, Fukuda Y, et al. In Vitro and in Vivo Activities of T-705 and Oseltamivir against Influenza Virus. Antiviral Chemistry and Chemotherapy. 2003;14(5):235–241. doi: 10.1177/095632020301400502 [DOI] [PubMed] [Google Scholar]
- 43.Dauby N, Van Praet S, Vanhomwegen C, Veliziotis I, Konopnicki D, Roman A Tolerability of favipiravir therapy in critically ill patients with COVID-19: A report of four cases. J Med Virol. 2020. 1–3.doi: 10.1002/jmv.26488 [DOI] [PubMed]
- 44.Irie K, Nakagawa A, Fujita H, et al. Pharmacokinetics of Favipiravir in Critically Ill Patients With COVID-19. Clin Transl Sci. 2020;13(5):880–885. doi: 10.1111/cts.12827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chinello P, Petrosillo N, Pittalis S, Biava G, Ippolito G, Nicastri E. QTc interval prolongation during favipiravir therapy in an Ebolavirus-infected patient. PLoS Negl Trop Dis. 2017;11(12):e0006034. doi: 10.1371/journal.pntd.0006034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malvy D, Taburet AM, de Lamballerie X, Mentre F, Extramiana F. The safety profile of favipiravir should not be the first argument to suspend its evaluation in viral hemorrhagic fevers. PLoS Negl Trop Dis. 2020;14(6):e0008259. doi: 10.1371/journal.pntd.0008259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Madelain V, Nguyen TH, Olivo A, et al. Ebola Virus Infection: review of the Pharmacokinetic and Pharmacodynamic Properties of Drugs Considered for Testing in. Trials HE. Clin Pharmacokinet. 2016;55(8):907–923. doi: 10.1007/s40262-015-0364-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.AVIGAN. Favipiravir: prescribing information. 2017. Accessed October14, 2020 https://www.cdc.gov.tw/File/Get/ht8jUiB_MI-aKnlwstwzvw.
- 49.Li L, Wang X, Wang R, Hu Y, Jiang S, Lu X. Antiviral Agent Therapy Optimization in Special Populations of COVID-19 Patients. Drug Des Devel Ther. 2020;14:3001–3013. doi: 10.2147/dddt.S259058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen C, Zhang Y, Huang J, et al. Favipiravir versus Arbidol for COVID-19: A Randomized Clinical Trial. medRxiv. 2020;20. [Google Scholar]
- 51.Şimşek Yavuz S, Ünal S. Antiviral treatment of COVID-19. Turk J Med Sci. 2020;50(SI–1):611–619. doi: 10.3906/sag-2004-145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vallamkondu J, John A, Wani WY, et al. SARS-CoV-2 pathophysiology and assessment of coronaviruses in CNS diseases with a focus on therapeutic targets Biochim Biophys. Acta Mol Basis Dis. 2020;1866(10):165889. doi: 10.1016/j.bbadis.2020.165889 [DOI] [PMC free article] [PubMed] [Google Scholar]