Abstract
Current literature suggests that neuroticism is positively associated with maladaptive life choices, likelihood of disease, and mortality. However, recent research has identified circumstances under which neuroticism is associated with positive outcomes. The current project examined whether “healthy neuroticism”, defined as the interaction of neuroticism and conscientiousness, was associated with the following health behaviors: smoking, alcohol consumption, and physical activity. Using a pre-registered multi-study coordinated integrative data analysis (IDA) approach, we investigated whether “healthy neuroticism” predicted the odds of engaging in each of the aforementioned activities. Each study estimated identical models, using the same covariates and data transformations, enabling optimal comparability of results. These results were then meta-analyzed in order to estimate an average (N-weighted) effect and to ascertain the extent of heterogeneity in the effects. Overall, these results suggest that neuroticism alone was not related to health behaviors, while individuals higher in conscientiousness were less likely to be smokers or drinkers, and more likely to engage in physical activity. In terms of the healthy neuroticism interaction of neuroticism and conscientiousness, significant interactions for smoking and physical activity suggest that the association between neuroticism and health behaviors was smaller among those high in conscientiousness. These findings lend credence to the idea that healthy neuroticism may be linked to certain health behaviors and that these effects are generalizable across several heterogeneous samples.
Keywords: Healthy Neuroticism, Health Behaviors, Big Five, IALSA, Coordinated IDA
Introduction
Personality psychologists have long debated the notion of ‘healthy neuroticism’. The idea that, under certain circumstances, neuroticism can have a positive impact on health is one that has intrigued personality and health psychologists for decades. While most agree with the validity of healthy neuroticism as an idea, few have agreed on the precise ways that healthy neuroticism is related to health or whether it is related to health at all (i.e., is it really “healthy”?). The current project sought to pursue the following research goals: 1) to examine whether healthy neuroticism was associated with a number of health behaviors, and 2) to establish the robustness and replicability of these associations by comparing effects from pre-registered coordinated models across 15 independent longitudinal studies. The current work was completed as part of a larger, three-part paper series project examining whether healthy neuroticism is associated with health behaviors (the current project), chronic conditions, and mortality.
Neuroticism and Health
A growing body of literature suggests that high neuroticism is associated with poor health outcomes. However, there is some inconsistency in the effects. Some have proposed two major paths (Friedman, 2000) through which neuroticism might relate to health. On one hand, neuroticism could lead to poorer health via anxiety-provoked maladaptive behaviors. On the other hand, neuroticism could lead to better health due to anxiety-provoked vigilance. One approach to deepening our understanding of the neuroticism-health associations is to examine factors that influence the neuroticism-health associations. Some studies have found that conscientiousness moderates the associations between neuroticism and health, such that individuals who are high in neuroticism and also high in conscientiousness may experience more positive health outcomes compared to those who have high in neuroticism but low in conscientiousness (Turiano, Mroczek, Moynihan, & Chapman, 2013; Turiano, Whiteman, Hampson, Roberts, & Mroczek, 2012; Weston & Jackson, 2016). This combination of neuroticism and conscientiousness has thus been labeled “healthy neuroticism”, though evidence that the combination of traits leads to better health or health behaviors is inconclusive (Graham et al., 2018; Weston, Hill, Edmonds, Mroczek, & Hampson, 2018).
The health behavior model of personality posits that personality influences health and mortality indirectly through the specific behaviors that individuals at various levels of a given trait are more (or less) likely to engage in over their lifetimes (Murray & Booth, 2015). For example, individuals high in conscientiousness may have better health outcomes as they age due to regular doctor visits, healthy diet, and a consistent physical fitness routine. Several studies have found direct links between personality and various health behaviors such as smoking (Graham et al., 2017; Turiano, Chapman, Gruenewald, & Mroczek, 2015), alcohol consumption (Hopwood, Baker, & Morey, 2008; Hopwood et al., 2007; Turiano et al., 2015), and physical activity (Graham et al., 2018). Additionally, research using mediator models provides evidence that health behaviors serve as mediators between personality and health outcomes (Graham et al., 2018; Turiano et al., 2013, 2012; Weston & Jackson, 2016). The behaviors an individual engages in may influence health, which influences an individual’s life expectancy. Personality presumably influences each of these pathways independently. As such, we focused the current project on just one of these pathways, the personality-health behaviors association. More specifically, we focused on the moderating effects of conscientiousness on the associations between neuroticism and health behaviors.
Healthy Neuroticism?
The existence of healthy neuroticism has been debated for close to two decades, beginning with Friedman (2000, 2019) who introduced the idea that neuroticism, while often bad for health, could also be beneficial in some circumstances. An individual’s level of neuroticism, combined with their unique constellation of the other Big Five traits, can, in theory, contribute to healthy or unhealthy choices. The most common method of operationalizing healthy neuroticism is as an interaction between neuroticism and conscientiousness; in other words, the degree to which predictive effects of neuroticism are moderated by conscientiousness (Weston et al., 2018). A number of studies have found that at high levels of conscientiousness, high neuroticism is associated with lower odds of smoking after disease diagnosis (Weston & Jackson, 2015), lower odds of problematic alcohol consumption (Turiano et al., 2012), and lower levels of inflammatory biomarkers (interleukin-6) (Turiano et al., 2013). In contrast, further research suggests that high neuroticism paired with low conscientiousness is associated with greater odds of risky behaviors (Vollrath & Torgersen, 2002). “Healthy neuroticism” (Healthy N) has been defined in various ways in the literature. For example, one study, which operationalized healthy N using a neuroticism by socioeconomic status by gender interaction, found that high neuroticism was protective against cardiovascular disease among high socio-economic status women (Hagger-Johnson et al., 2012). Another, defining healthy N as the interaction of neuroticism and self-rated health, found that neuroticism was protective against mortality among individuals with lower self-rated health (Gale et al., 2017). However, based on a single sample and a variety of operationalizations of healthy neuroticism, Weston and associates (2018) found no evidence that healthy neuroticism is associated with health, health behaviors, or biological markers of health. Together, these findings suggest that neuroticism may lead to better health under some conditions, though evidence is mixed.
As described above, existing research has applied a variety of operational definitions of the healthy neuroticism construct, but no studies have examined the construct in relation to the same health outcomes, which limits the ability to evaluate the replicability of results. A more rigorous and systematic approach is needed to understand whether healthy neuroticism is predictive of health in adulthood. Coordinated integrative data analysis (IDA) can help resolve this issue and clarify the extent to which healthy neuroticism is related to behavior and health by testing for these associations in multiple independent studies simultaneously (Graham et al., 2017; Hofer & Piccinin, 2009).
The Current Project
The current study is the third in a series of three studies submitted together. These studies were the result of a single, coordinated project involving multiple principal investigators and research labs around the world. The goal of this project was to rigorously analyze the evidence for “healthy neuroticism,” narrowly defined as the significant moderation of the neuroticism-health relationship by conscientiousness. These analyses considered multiple components of health, specifically behaviors, development of chronic conditions, and mortality, following a lifespan trajectory. Despite the coordination and similarity of analyses among these three components of health, there were notable differences between the studies, including the datasets which could be used for the analysis, the quantitative models applied, and the theoretical rationale followed to link personality and health. Moreover, synthesizing this project in a single manuscript would have required over-simplification of critical details and decision points along the way. As a result, the three components were divided into three separate but linked manuscripts, allowing for the requisite detail to be included in each.
The current project focused on one pathway in the health behaviors model of personality: the association between traits and health behaviors. Our primary aim was to test the moderating effect of conscientiousness on the neuroticism-health behavior association, with a focus on smoking, alcohol consumption, and physical activity as outcomes. The outcome health behavior variables were selected because many studies assess these behaviors. A current theme across the psychological sciences involves the importance of research replicability (Condon, Graham, & Mroczek, 2017; Nelson, Simmons, & Simonsohn, 2018; Vazire, 2018); as discussed above, we acknowledge that while the idea of healthy neuroticism has face validity, existing published findings examining the construct may be inadvertently subject to publication bias. As such, in an effort to mitigate potential publication bias, the current project used a coordinated IDA approach to answer our key questions (Graham et al., 2017; Hofer & Piccinin, 2009). We identified 15 existing longitudinal samples that contained the appropriate data to test our hypotheses. Fitting identical models to each sample individually, then calculating meta-analytic summaries, provided the opportunity to address both the extent to which our hypotheses were supported, as well as the extent to which these answers were replicated across many large sample studies.
Research Questions and Hypotheses
The following overarching research questions were investigated: Is healthy neuroticism associated with health behaviors? Does a consistent pattern of results emerge across several longitudinal studies of aging? We hypothesized that the relationship between neuroticism and current smoking, drinking, or physical activity would vary as a function of conscientiousness.
Coordinated Analysis
Coordinated analysis is a form of IDA that compares identical models across multiple studies (Graham et al., 2017; Hofer & Piccinin, 2009). The methods and measures used in existing individual longitudinal studies are typically heterogeneous; therefore, direct replications are virtually impossible. As such, coordinated analyses are conceptual replications: instead of harmonizing across identical measures, coordinated analysis projects use harmonized models, thereby allowing the exact measurement of a given construct to vary. This approach lends itself to greater generalizability and credibility of results. Furthermore, variations in studies have long been considered a constraint on the generality of findings in longitudinal research (Simons, Shoda, & Lindsay, 2017). In coordinated analysis, these differences can be a strength: instead of regarding these study-level characteristics (e.g., cohort, measurement scale, country) as sources of error, researchers have the option to test these differences systematically as sources of heterogeneity.
Methods
Samples
We used the Integrative Analysis of Longitudinal Studies of Aging and Dementia (IALSA) network to identify existing data sets worldwide with the requisite data to test our hypotheses. The IALSA network promotes access among collaborating investigators to data that are not publicly available and facilitates data-sharing agreements among study sites. Studies with non-public data provided analyst support. In total, 15 longitudinal studies had appropriate data to address our research questions. See Table 1 for study level descriptions.
Table 1.
Descriptive Statistics.
| Study | Country | N | Year | Age Range | Personality Scale | Smokers(%) | Alcohol(%) | Physical Activity(%) |
|---|---|---|---|---|---|---|---|---|
| BASE-II | Germany | 1,613 | 2009 | 22-77 | BFI-S | 12.00 | 3.00 | 68.00 |
| EAS | U.S. | 799 | 2005 | 69-99 | IPIP-50 | 4.00 | 76.00 | 67.00 |
| ELSE | U.K. | 8,832 | 2002 | 29-99 | MIDI | 12.00 | 1.00 | 94.00 |
| HRS | U.S. | 19,242 | 2006 | 25-105 | MIDI | 15.00 | 6.00 | 94.00 |
| ILSE | Germany | 482 | 1994 | 60-64 | NEO-FFI | 21.00 | 25.00 | 50.00 |
| LBC1936 | U.K. | 962 | 2006 | 67-71 | IPIP | 11.00 | 87.00 | 69.00 |
| LBLS | U.S. | 1,361 | 1994 | 30-97 | NEO-PI-R | 9.00 | 64.00 | 45.00 |
| MAP | U.S. | 982 | 1997 | 56-100 | NEO-FFI | 1.00 | 1.00 | 87.00 |
| MAS | Australia | 879 | 2005 | 70-91 | NEO-PI-R | 4.00 | 88.00 | 84.00 |
| MIDUS | U.S. | 4,009 | 1994 | 30-84 | MIDI | 14.00 | 4.00 | 97.00 |
| NAS | U.S. | 899 | 1990 | 47-85 | Goldberg | 21.00 | 58.00 | 59.00 |
| OATS | Australia | 536 | 1997 | 65-90 | NEO-PI-R | 6.00 | 4.00 | 89.00 |
| ROS | U.S. | 1,394 | 1994 | 56-102 | NEO-FFI | 2.00 | 0.00 | 79.00 |
| SLS | U.S. | 1,194 | 2001 | 29-101 | NEO-PI-R | 4.00 | 9.00 | 87.00 |
| WLS | U.S. | 10,723 | 1993 | 33-75 | BFI | 17.00 | 55.00 | 94.00 |
The Berlin Aging Study II (BASE-II) consists of a subsample of younger adults (20-35 years of age) and a subsample of older adults (60-84 years of age) who were recruited from the greater metropolitan area of Berlin (Bertram et al., 2013; Gerstorf et al., 2016). Starting in 2009, participants completed at least one personality and health measure. For the current project, baseline was defined as the first occasion at which a participant had completed the personality measures. This ranged from 2009 to 2014, with the majority of participants starting in 2009. A total of 1,613 (Mage = 61.56, SDage = 16.58, 50% female) participants completed personality and health behavior measures.
The Einstein Aging Study (EAS) is an ongoing longitudinal cohort study of cognitive aging and dementia, beginning in 1993. Older adults who were at least 70 years of age, non-institutionalized, and English speaking were systematically recruited from an urban, multi-ethnic, community-dwelling population in Bronx County, NY. Participants receive comprehensive annual medical and neuropsychological evaluations (Katz et al., 2012).For the current project, baseline was defined as the first time at which participants completed the personality scales, ranging from 2005 to 2016. A total of 799 (Mage = 79.01, SDage = 5.36, 61% female) participants completed personality and health behavior measures.
The English Longitudinal Study of Ageing (ELSA) is an ongoing longitudinal cohort survey that collects multidisciplinary information on older adults living in England. Data collection began in 2002, and new participants were added at waves 3, 4, 6 and 7 to maintain size and representativeness (Marmot et al., 2017). Although recruitment and biennial testing occasions commenced in 2002, personality assessment was administered in 2010 (wave 5), which is defined as baseline for the purposes of this analysis. Face-to-face interviews, a computer assisted personal interview, and self-completed questionnaires were administered at every wave. A total of 8,832 (Mage = 66.31, SDage = 9.52, 56% female) participants completed personality and health behavior measures.
The Health and Retirement Study (HRS) is an ongoing longitudinal panel study that tracks retirement-age adults in the United States. Data collection began in 1992, with new cohorts added throughout the 1990s and 2000s (Sonnega et al., 2014). For this analysis, baseline was defined as the first time at which participants completed the personality scales, ranging from 2006 to 2014. Participants were assessed every two years regarding health information. A total of 19,242 (Mage = 66.27, SDage = 11.16, 59% female) participants completed personality and health behavior measures.
The Interdisciplinary Longitudinal Study of Adult Development and Aging (ILSE) is a multidisciplinary longitudinal study initiated in 1993 investigating the aging process of two German birth cohorts born between 1930-1932 and 1950-1952 (e.g., Aschwanden, Kliegel, & Allemand, 2018; Sattler et al., 2015). For the current analysis, individuals from the older cohort (i.e., born in 1930-1932) were included A total of 482 (Mage = 62.51, SDage = 0.96, 52% female) participants completed personality and health behavior measures.
The Lothian Birth Cohort 1936 (LBC) consists of surviving members of the 1947 Scottish Mental Health Survey cohort. The 1936 birth cohort was recruited between 2004 and 2007 by identifying individuals from the original 1947 survey cohort who were residing in Edinburgh and the surrounding areas (Taylor, Pattie, & Deary, 2018). In total, 1,091 participants entered the study. LBC baseline for the current analysis is defined as the first wave of personality assessment, which took place in 2006. A total of 962 (Mage = 69.50, SDage = 0.84, 51% female) participants completed personality and health behavior measures.
The Long Beach Longitudinal Study (LBLS) started in 1978 and consisted of an initial sample of 589 adults aged 28-84 from California. Additional cohorts were added in the second two waves of data collection (Zelinski & Kennison, 2008). Participants were surveyed in 1994-1995, 2000-2002, and 2008-2013. Personality was assessed in 1994/1995 and 2000/2001. LBLS baseline personality for the present study is the first time that the NEO-PI-R was completed. A total of 1,361 (Mage = 68.97, SDage = 13.35, 54% female) participants completed personality and health behavior measures.
The Memory and Aging Project (MAP) is a longitudinal, epidemiologic clinical-pathologic cohort study of common chronic conditions of aging with emphasis on decline in cognitive and motor function and risk of Alzheimer’s disease. Participants are older adults recruited from retirement communities and subsidized senior housing facilities throughout Chicagoland and northeastern Illinois. Participants, without known dementia at baseline, agreed to annual clinical evaluation, cognitive testing, and brain and other tissue donation after death (Bennett et al., 2018, 2012). Enrollment began in 1997 and is ongoing. Neuroticism was collected at baseline since study start; conscientiousness and extraversion were collected at baseline since 2008 (openness and agreeableness not collected). A total of 982 (Mage = 79.85, SDage = 7.14, 76% female) participants completed personality and health behavior measures.
The Sydney Memory and Ageing Study (MAS) is an ongoing longitudinal cohort study of brain aging and dementia in older individuals, who undertake medical, neuropsychological and psychosocial assessments biennially. Individuals without dementia aged 70-90 and living in the Australian community at baseline (between 2005-2007) were randomly sampled through the electoral roll (Sachdev et al., 2010). A total of 879 (Mage = 78.71, SDage = 4.78, 46% female) participants completed personality and health behavior measures.
The Midlife in the United States (MIDUS) Study is an ongoing nationally representative study of 7,108 participants in the U.S. that began in 1994/1995, and has since added two additional waves of data collection, in 2004/2005, and 2013/2014 (Brim, Ryff, & Kessler, 2004). A total of 4,009 (Mage = 56.19, SDage = 12.37, 55% female) participants completed personality and health behavior measures.
The Veterans Affairs Normative Aging Study (NAS) is a study of the medical and psychosocial aging among U.S. men that is funded by the U.S. Department of Veterans Affairs. The sample is based in the Greater Boston, MA metro area and consists of 2,280 men enrolled 1961-1970, who were on average 42 years old at enrollment (SD = 8, range = 21 - 81) (Bosse, Ekerdt, & Silbert, 1984). Surviving participants were examined every 3-5 years, depending on age (until 1984 men under 52 were seen every 5 years, and older men were seen every 3; since then all are seen every 3 years) for follow up examinations. Personality was assessed, by mail, for the current project, beginning in 1990. A total of 899 (Mage = 64.45, SDage= 7.38, 0% female) participants completed personality and health behavior measures.
The Older Australian Twins Study (OATS) is a multi-site longitudinal study of monozygotic (MZ) and dizygotic (DZ) twins aged ≥ 65 years, with a cohort of 623 participants assessed at baseline, and is one of the largest and most comprehensive studies of older twins in Australia (Sachdev et al., 2012). The study includes comprehensive psychiatric, psychological, cognitive, cardiovascular, metabolic, and neuroimaging assessments. A total of 536 (Mage = 71.40, SDage = 5.54, 65% female) participants completed personality and health behavior measures.
The Religious Orders Study (ROS) is a longitudinal, epidemiologic clinical-pathologic cohort study of aging and Alzheimer’s disease that enrolls older Catholic nuns, priests, and brothers from more than 40 groups across the United States. Participants do not have known dementia at baseline and agree to annual clinical evaluations, cognitive testing, and brain and other tissue donation after death (Bennett et al., 2018; Bennett, Schneider, Arvanitakis, & Wilson, 2012). Enrollment began in 1994 and is ongoing. NEO personality has been assessed at baseline since study start. A total of 1,394 (Mage = 75.95, SDage = 7.47, 71% female) participants completed personality and health behavior measures.
The Seattle Longitudinal Study (SLS) started in 1956 and has since collected data on close to 6,000 participants in a cohort sequential design (Schaie, Willis, & Caskie, 2004). Participants were sampled randomly from members of a large health maintenance organization in the Seattle, Washington area. A total of 1,656 participants aged 26 to 101 completed at least one personality assessment between 2001 and 2012. Baseline was defined as the first time at which a participant had completed the personality measures. For the health behavior and chronic conditions projects, the 2001 personality assessment could not be used because the corresponding health data were missing. For these analyses, the earliest possible baseline assessment was in 2005. A total of 1,194 (Mage = 66.45, SDage = 14.33, 55% female) participants completed personality and health behavior measures.
The Wisconsin Longitudinal Study (WLS) follows a cohort of men and women who graduated from Wisconsin high schools in 1957. Data from graduate participants (N = 10,317) span almost 60 years from the baseline assessment in 1957, with follow-up assessments collected in 1967, 1975, 1993, 2004, and most recently in 2011. In addition to the original cohort, subsequent assessments included randomly selected siblings and spouses of graduate participants (Herd, Carr, & Roan, 2014). Personality measures were first introduced in the WLS in 1993, which served as the baseline assessment for the present analyses. Health, demographic characteristics, and other information were collected in the 1993, 2004, and 2011 waves through in-person, mail, and telephone surveys. A total of 10,723 (Mage = 53.77, SDage = 4.52, 54% female) participants completed personality and health behavior measures.
Materials
Descriptive statistics for all studies/variables as well as descriptions of variable collection/construction can be found online.
Personality Traits
Each of the 15 samples included a baseline assessment of the Big Five personality traits (neuroticism, extraversion, openness to experience, conscientiousness, agreeableness). Seven studies used a version of the NEO (ILSE, ROS, MAP, LBLS, OATS, SLS, MAS) (Costa Jr & McCrae, 1985), three used the MIDI (MIDUS, HRS, ELSA) (Lachman & Weaver, 1997), two used a version of the IPIP (LBC1936 [IPIP50], EAS) (Goldberg et al., 2006), one used the Goldberg (1992) adjectives (NAS) and two (BASE-II, WLS) used the BFI (John & Srivastava, 1999). For inclusion in the current project, we required that studies had, at minimum, a baseline assessment of neuroticism and conscientiousness (not necessarily the full Big Five). Collectively, the measures of personality traits used covered a wide range of narrow constructs that are typically assessed by the broader Big Five model. It is worth noting some systematic differences between the scales. For example, the IPIP-50 measure of conscientiousness included items assessing responsibility, practicality, and thriftiness, but not self-discipline or efficiency; in addition, the BFI measures competency and achievement but not goal-striving. To some extent, the differences in trait coverage across scales is an asset to these analyses: a lack of notable differences in effects would suggest that estimated relationships are robust to type of scale, while significant differences may point to specific mechanisms (i.e., narrower traits) which may underlie and inspire investigation of causal mechanisms. We provide a table of content measurement by scale online and invite comparisons across these measures.
Health Behaviors
All health behaviors were assessed at baseline, which was defined as the initial assessment of personality in each individual study.
Smoking
The majority of studies assessed smoking behavior with a single self-report item asking whether the participant is a current smoker, with dichotomous response option (yes or no). Common phrasing for this item was “are you currently a smoker”, or “do you smoke cigarettes/pipes/cigars currently”. This item was used across studies to construct a smoking variable, assigning participants as either a current smoker (1) or not (0).
Alcohol Consumption
Alcohol consumption behavior was assessed with self-report items across all studies. Individual studies used different approaches to ascertaining whether the participant was currently a drinker. Some (HRS, ROS, MAP, ILSE) used a simple yes/no response item for whether the participant regularly consumed alcohol. Most (BASE-II, EAS, ELSA, NAS, SLS, WLS, MAS, OATS, LBLS) asked for the frequency with which participants regularly consumed specific sources of alcohol (e.g., wine, beer, liquor). For these studies, individuals were coded as being a current drinker if they consumed alcohol (or typically) consumed alcohol in the past week or year.
Physical Activity
For all studies, a physical activity variable was constructed that categorized participants as either regularly engaging in physical activity (1) or not (0). Studies varied on their method of assessing physical activity, but all were self-report. Studies typically asked participants about the frequency of physical activity (e.g., times per week), and many also asked about the types (e.g., jogging, gardening, home repairs) and intensity of activity (e.g., mild, moderate, vigorous).
Covariates
Models estimated for the current project were adjusted for age, education, gender, and the other personality traits as applicable. For all studies, age was z-standardized and centered at the baseline assessment of personality. Sex was coded as 1=Women, 0=Men (note, NAS was a male-only sample and as such did not adjust for gender). For most studies (BASE-II, EAS, HRS, ROS, MAP, LBLS), education was defined as the total number of years of education at baseline. Some studies employed an ordinal scale that assessed the highest degree earned (ELSA, ILSE, NAS, WLS). Education was z-standardized within study.
Data analysis
We used R (Version 3.6.2; R Core Team, 2018) for all our analyses and visualizations. Functions in the metafor package (Version 2.0.0; Viechtbauer, 2010) were used to estimate the overall effects and heterogeneity between studies, as well as to create forest plots. The sjPlot package (Version 2.6.1; Lüdecke, 2018) was used to calculate predicted values for each study and the ggplot2 package (Version 3.0.0; Wickham, 2009) was used to visualize effects. Analyses were pre-registered. While all data for this project were collected prior to analysis, the analytic plan was made prior to analysis of any data. The first author decided which health behaviors to use as outcomes and which variables to use as covariates. The second author, who has analyzed the HRS data in prior publications, then cleaned the HRS data, and created a randomly seeded subset for which to write code, evaluate the inferential models in R, and test for errors in both the individual study analysis scripts and the meta-analysis script. This R script created an output object containing meta-data, descriptive statistics, statistics from the inferential models and values predicted from the model for plotting. Analyses, including scripts, were pre-registered at this point. After pre-registration, individual data analysts downloaded the inferential script to fit the models to their dataset. Output objects were created and uploaded to OSF; the first author then used the meta-analysis scripts to estimate the average effect of healthy neuroticism on health behaviors using these output objects. Study level moderators were specified for the meta-analysis, including the personality scale used and country of origin. All scripts and data objects (not the data themselves, in order to comply with data sharing agreements) are [available on OSF](https://osf.io/y3mzb/](https://osf.io/y3mzb/?view_only=a70c7e4d189e4d39a5b0805652f9e9dc).
The results reported below are the second of two pre-registered versions of this project. The first, preliminary version, was completed as part of a coordinated analysis workshop in conjunction with the other papers in this series. The second, final version, was completed after the fact, due to a change in personnel. The original pre-registration can be found here and differs in the following ways: the MAP study was included, but no models included the chronic condition covariates. The second registration also contains more information for how the individual study- and meta- analyses would be completed. Preregistration and script development were conducted by the first and second authors, who had seen the results from the preliminary analyses. The pre-registration contains a few lines throughout where the individual study analysts had not yet identified the exact variable to be used for the analyses, and as such is listed as “TBD” in the pre-registration. This to-be-determined status was restricted to the specific variable a study was using, and in no way influenced the choice of construct measured or data coding. While we would like to assure readers that the results from the preliminary analyses did not inform any data analytic decisions for the second registration, we acknowledge that this is impossible to prove empirically and as such, the results reported below should be interpreted accordingly. Analyses and script development were designed to most closely mirror models used in the mortality and chronic conditions studies. All model output and scripts can be found at [OSF](https://osf.io/y3mzb/](https://osf.io/y3mzb/?view_only=a70c7e4d189e4d39a5b0805652f9e9dc); the OSF page also includes an archive folder containing all results and code from the preliminary analyses to allow readers to compare the results from this stage of analysis to the ones presented here.
Individual Study Analysis
Concurrent relationships between the interaction of neuroticism and conscientiousness and the likelihood of engaging in smoking, alcohol consumption, and physical activity were estimated using binary logistic regression. For each behavioral outcome, we constructed the following models: First (Model A), the predicted probability of behavior by neuroticism and conscientiousness (i.e., partialled main effects of these traits). Second Model B, the predicted probability of behavior by neuroticism and conscientiousness and the interaction of these traits. Third Model C, the predicted probability of behavior by neuroticism and conscientiousness and the interaction of these traits, controlling for age, gender, and education. Fourth Model D, prediction of odds of behavior by neuroticism and conscientiousness and the interaction of these traits, controlling for age, gender and education and the other Big Five personality traits (extraversion, agreeableness, openness). Fifth (Model E), prediction of odds of behavior by neuroticism, conscientiousness and age, and all possible two- and three-way interactions of these variables, controlling for gender and education and any other Big 5 personality traits (extraversion, agreeableness, openness). The following results focus on the main effects models for neuroticism and conscientiousness separately (Model A), then the fully adjusted models (Model D), and finally the models including age interactions (Model E) for smoking, drinking, and physical activity. The inferential decisions do not differ based on model choice, and in models B, C, and D the differences between estimates are all less than .02. We report Models D and E below, as they provide the most robust test of our hypotheses. All models used listwise deletion. Sample sizes for each model in each dataset are presented in the relevant figure or table.
Meta-Analysis
The individual study analyses were aggregated and summarized using random effects meta-analysis in the metafor package of R (Version 2.0.0; Viechtbauer, 2010). We estimated the average effect (weighted by N) of the neuroticism by conscientiousness interaction for each outcome. This calculation included an estimation of heterogeneity in the effects between studies. The forest plot shows the individual study effects, as well as the meta-analytic summaries.
Power Analysis
Given the anticipated sample size, we did not believe a power analysis was necessary with regards to our interaction coefficient estimate, or the coefficient estimates of neuroticism and conscientiousness. However, our power to detect significant heterogeneity in effect sizes between studies is unclear. We estimated our power using methods described by Hedges and Pigott (2004). Based on the within-study variability and number of studies, we estimate that we are sufficiently able (power > .90) to detect heterogeneity of at least a standard deviation (in odds ratios) of .05 (corresponding τ of .08). We note that the majority of psychology meta-analyses find between study variability between tau of 0 and .25 (Van Erp, Verhagen, Grasman, & Wagenmakers, 2017). See also here for the estimated power curves for each outcome.
Results
Figure 1 and 2 contain forest plots summarizing the individual study estimates (in odds ratios), and the average effect (weighted by N), and meta-analytic statistics (I2, Cochran’s Q) of the main effects of neuroticism and conscientiousness. Figure 3 contains a forest plot of the neuroticism by conscientiousness interaction. Model results were very similar when adjusted for demographics only (https://ialsaging.github.io/healthyn/behavior_forest_cov1.html) versus the models adjusted for demographics and the full Big Five. Below, we report the forest plots for the models containing all of the covariates.
Figure 1:
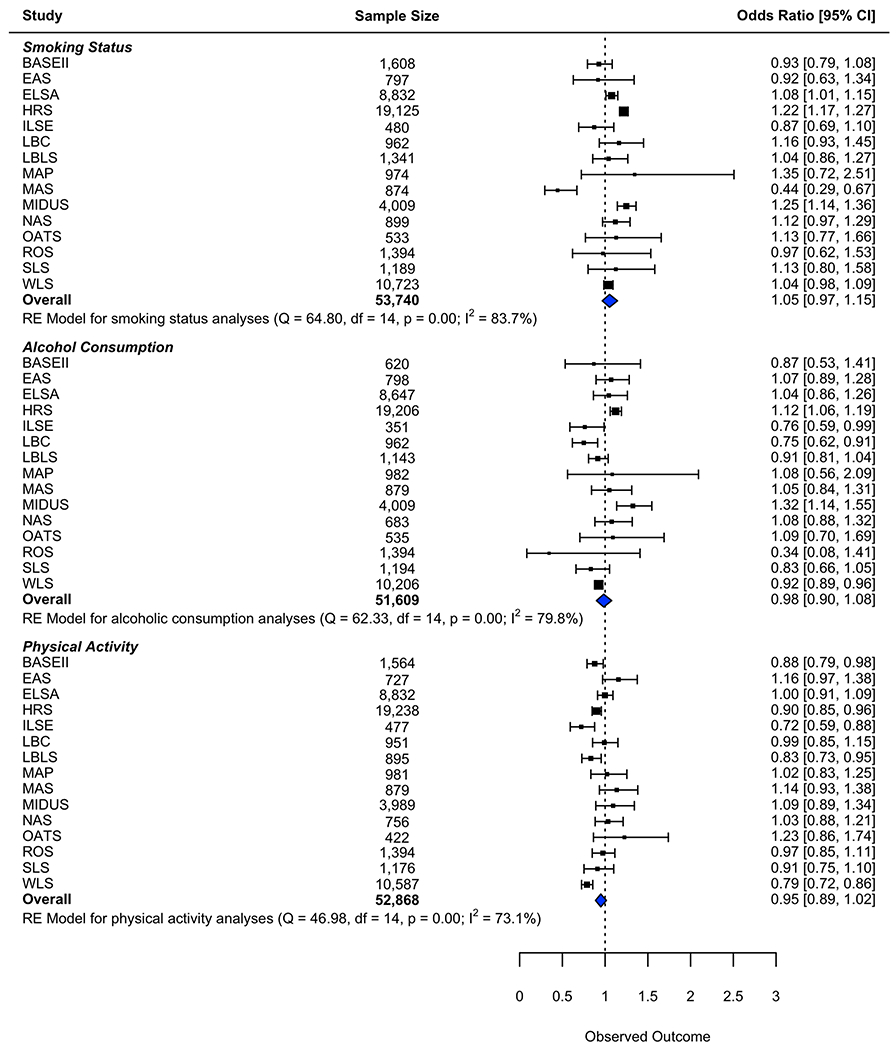
Forest Plot of Main Effect of Neuroticism, Associations with Smoking, Alcohol Consumption, and Physical Activity
Figure 2:

Forest Plot of Main Effect of Conscientiousness, Associations with Smoking, Alcohol Consumption, and Physical Activity
Figure 3:

Forest Plot of Neuroticism by Conscientiousness Associations with Smoking, Alcohol Consumption, and Physical Activity
Healthy Neuroticism and Smoking
The main effect models indicate that neuroticism was not associated with the odds of being a smoker (beta = 0.05, OR = 1.05, 95% CI = [0.97,1.15], p = .244). Higher conscientiousness was associated with lower odds of smoking (beta = −0.07, OR = 0.93, 95% CI = [0.90,0.96], p = <.001). The models with the interaction term indicated that the neuroticism by conscientiousness interaction was associated with odds of smoking. The average effect for the overall interaction terms was significant (beta = −0.04, OR = 0.97, 95% CI = [0.94,0.99], p = .002), (I2 = 0.00, Q = 8.90, df = 14, p =.838). The middle two columns of Figure 3 show the effect of neuroticism on odds of smoking for individuals who are +/−1 SD of conscientiousness. The association of neuroticism and odds of smoking appear to be lessened at the higher end of conscientiousness, indicating that being high in conscientiousness may be protective against the association of neuroticism and smoking. The low heterogeneity in the meta-analytic summary indicates that, in general, the studies are consistent in these effects. See Figure 4 to see the plotted predicted values of smoking at high and low conscientiousness. We also tested the three way interaction, to ascertain whether the healthy neuroticism interaction was moderated by age. The meta-analytic summary indicates that there is a small effect (beta = −0.05, OR = 0.95, 95% CI = [0.91,0.99], p =.017), and this was consistent across studies (I2 = 13.47, Q = 12.90, df = 14, p = .535). Given the lack of heterogeneity, we did not test study-level moderators of this effect. In Figure 5, it appears that the moderating effect of conscientiousness on the neuroticism-smoking association varies across age groups. The neuroticism by conscientiousness interaction becomes less pronounced with each increasing age group, indicating that the effect is primarily present among younger adults.
Figure 4:
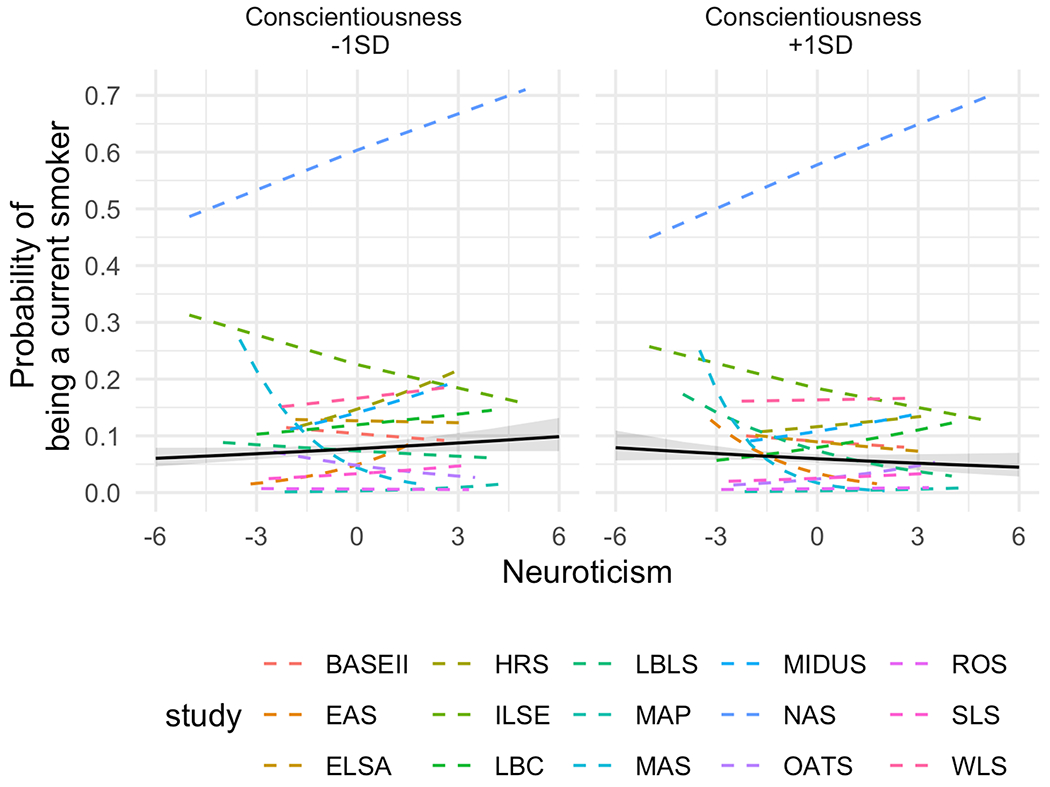
Associations between Neuroticism and Odds of Smoking, Moderated by Conscientiousness, black line is the cross-study average
Figure 5:
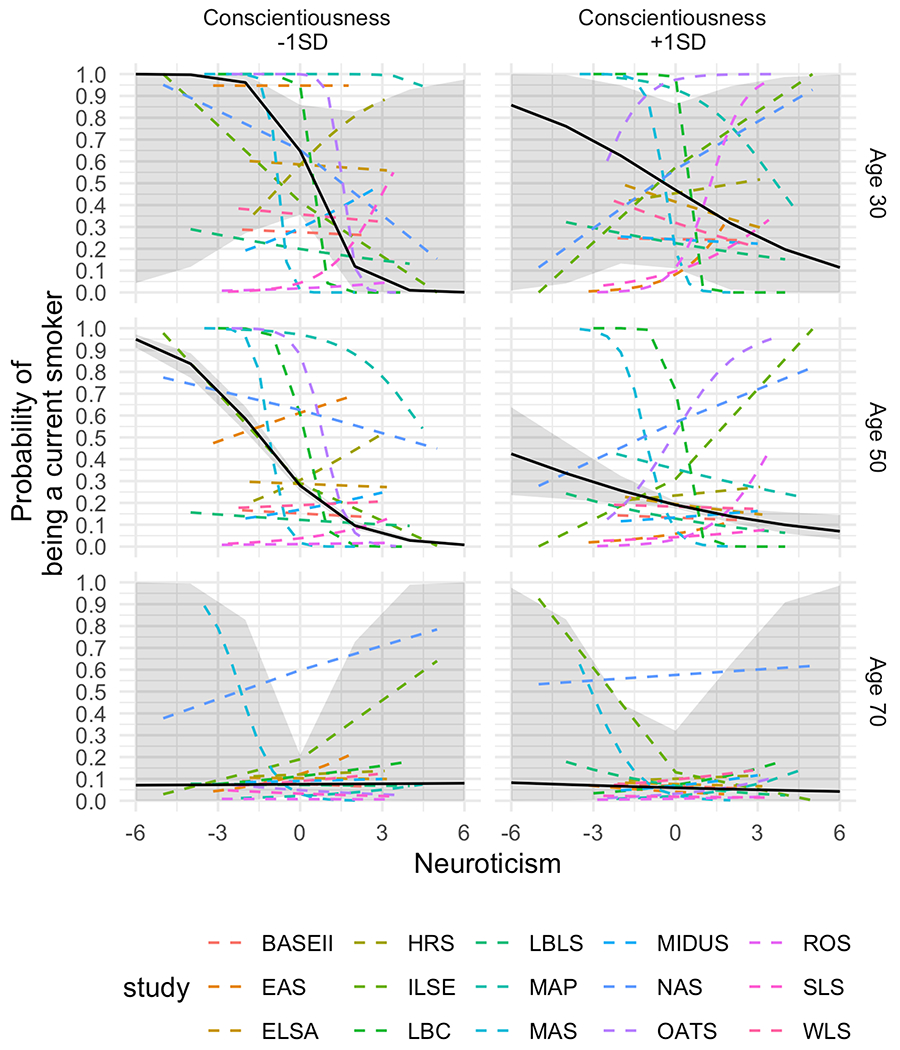
Associations between Neuroticism and Odds of Smoking, Moderated by Conscientiousness and Age (predicted probability), black line is the cross-study average
Healthy Neuroticism and Alcohol Consumption
The main effect models indicate that neuroticism is not associated with odds of alcohol consumption (beta = −0.02, OR = 0.98, 95% CI = [0.90,1.08], p = .722). Higher conscientiousness is associated with lower odds of alcohol consumption (beta = −0.07, OR = 0.93, 95% CI = [0.87,0.99], p = .028). The overall interaction effect for alcohol consumption (Figure 3, middle rows) suggests that there is not a neuroticism by conscientiousness interaction predicting alcohol consumption behavior (beta = 0.01, OR = 1.01, 95% CI = [0.95,1.08], p = .677). These effects are fairly consistent across studies (I2 = 58.23, Q = 25.28,, df = 14, p = .032). See Figure 6 for the plotted predicted values of alcohol consumption at high and low conscientiousness. Given the lack of heterogeneity, we did not test study-level moderators of this effect. We tested the three-way interaction with age, to ascertain whether the healthy neuroticism interaction was moderated by age, which it was not (beta = 0.03, OR = 1.01, 95% CI = [0.99,1.08], p = .096), and this was consistent across studies (I2 = 0.00, Q = 10.33, df = 14, p = .738).
Figure 6:

Associations between Neuroticism and Odds of alcohol consumption, Moderated by Conscientiousness (predicted probability), black line is the cross-study average
Healthy Neuroticism and Physical Activity
The main effect models indicate that neuroticism was not associated with odds of physical activity (beta = −0.05, OR = 0.95, 95% CI = [0.89,1.02], p = .131) Higher conscientiousness was associated with higher odds of physical activity (beta = 0.21, OR = 1.24, 95% CI = [1.12,1.36], p = <.001). The models for the interaction indicate that there was an overall neuroticism by conscientiousness interaction ((beta = 0.04, OR = 1.04, 95% CI = [1.01,1.07], p = .003), and this association is consistent across studies (I2 = 0.00, Q = 13.66, df = 14, p = .475). The middle two columns of Figure 1 show the effect of neuroticism on odds of physical activity for individuals who are +/−1SD of conscientiousness. At the lower end of the conscientiousness distribution (e.g., −1SD below the mean), neuroticism was associated with lower odds of being physically active (beta = −0.08, OR = 0.93, 95% CI = [0.86,0.99], p = .034). This suggests that being higher in neuroticism is associated with poorer health choices (e.g. sedentary lifestyle) among individuals who are also low in conscientiousness. At the higher end of conscientiousness, there is not an association between neuroticism and physical activity, suggesting that conscientiousness may ameliorate the negative impact of neuroticism on physical activity (and thus provides evidence for healthy neuroticism). The low heterogeneity in the meta-analytic summary indicates that, in general, the studies are consistent in these effects. Given the lack of heterogeneity, we did not test study-level moderators of this effect. See Figure 7 for the plotted predicted values of activity at high and low conscientiousness. The meta-analytic summary for the three-way interaction with age indicates that there is no effect (beta = −0.01, OR = 0.99, 95% CI = [0.94,1.04], p = .670), and this was consistent across studies (I2 = 0.00, Q = 7.52, df = 14, p = .913). This suggests that the neuroticism by conscientiousness interaction on physical activity is the same across age.
Figure 7:

Associations between Neuroticism and Odds of Physical Activity, Moderated by Conscientiousness (predicted probability), black line is the cross-study average
Discussion
This coordinated analysis found evidence that high neuroticism, when paired with high conscientiousness, is related to specific healthy behaviors. We found associations for smoking behavior and physical activity, but not for alcohol consumption. The current project conceptually replicated analyses using 15 longitudinal data sets with a total N of nearly 54,000 to investigate the associations between healthy neuroticism and health behaviors. Each study transformed their data identically to the extent possible and estimated the same models. Our goal was to ascertain whether the neuroticism by conscientiousness interaction could be detected using a very simple modeling paradigm based on cross-sectional data. We focused on baseline levels of both personality and health behaviors. We focused our results on the meta-analytic summaries, which provided an overall effect across the studies, and an estimate of the consistency (homogeneity) of these effects. The estimates of heterogeneity in each model were all quite small, indicating that the effects were relatively similar across studies.
Results indicate that at low levels of conscientiousness, odds of smoking increase and odds of being physically active decrease for individuals with higher levels of neuroticism. At high levels of conscientiousness, this pattern is not present, suggesting that higher conscientiousness ameliorates the negative impact that neuroticism has on smoking and activity behavior. A significant three-way interaction suggests that these effects are further moderated by age for smoking, but not for alcohol consumption or physical activity. The pattern of the interaction suggests that the effect of neuroticism on smoking behavior at higher levels of conscientiousness is strongest at younger ages. Among highly conscientious older adults, neuroticism is associated with decreased odds of smoking. From a lifespan perspective, the observed interaction with age could be related to the idea that older adults have typically outgrown the sense of immortality of youth and are more anxious of how their behaviors may impact their health (Shanahan, Hill, Roberts, Eccles, & Friedman, 2014), and make decisions about their health behaviors accordingly (as evidenced by the primarily negative sign in age effects on behaviors across studies).
Overall, the effects we detected were relatively small. Within each individual study, the estimates were all very close to null (1.00 in odds ratio terms). The aggregated effects were weighted by sample size, and were still relatively close to zero, but were statistically significant for smoking and physical activity. Since three outcome measures were used to test the overall hypothesis, we thus had three opportunities to reject the null hypothesis. In the case of the current results, we would make the decision to reject the null for two of the three outcomes. As a matter of prudence, using a more conservative alpha (e.g., .01) would help account for this multiple testing problem, and using this more conservative criterion leads to the same conclusion. Overall, we conclude that while the effects are small, healthy neuroticism does appear to be related to health behavior.
The coordinated analysis approach to IDA is an increasingly accepted form of establishing the replicability of effects using existing data (Graham et al., 2017; Hofer & Piccinin, 2009; Weston, Graham, & Piccinin, 2019). Our use of coordinated analysis attempted to overcome some of the limitations of inferences obtained from single-sample studies, including uncertainties with regard to effect size estimates, as well as the consistency and generalizability of obtained effects. Additionally, the coordination and planning of theoretically derived models prior to data analysis ensured that we did not make post-hoc analysis decisions based on results, but rather used a theory driven approach to planning and executing the statistical models. Our pre-registered data transformation and analysis plan ensured that we adhered to our pre-planned analysis.
While the current project used only a cross-sectional portion of the participating data sets, this project is one of a three-paper series, the others of which use longitudinal data to explore whether healthy neuroticism was associated with disease incidence and mortality. These three papers together provide compelling evidence regarding the role that healthy neuroticism plays in the health behavior model of personality. Namely, although healthy neuroticism may impact some health behaviors, there is not a direct effect of healthy neuroticism on disease incidence or mortality (see Weston et al., and Turiano et al., in this series).
We acknowledge several limitations of our project. One limitation is the variation in measurements across all variables. With different scales used to assess the Big Five, and different wording of items to assess smoking, alcohol consumption, and physical activity behavior, the current project is not a direct replication but rather a conceptual replication. However, variations in key features of datasets can reinforce results in a coordinated analysis (Hofer & Piccinin, 2009). Consistency in findings across datasets, in spite of measurement differences, suggests that the effect of healthy neuroticism on health behaviors is robust and is not limited to a single methodological approach. Detection of consistent effects across samples of varying ages, countries, and start year are further indications of the generalizability of these effects. The current project also limited analyses to baseline measurements of both the independent and outcome variables, resulting in the inability to make any longitudinal inferences. Next steps could test whether healthy neuroticism is longitudinally associated with incidence (e.g., starting smoking), maintenance (e.g., continuing a physical activity program), or cessation (e.g., quitting alcohol consumption) of health behaviors. Further, the current project defined healthy neuroticism as the interaction between neuroticism and conscientiousness. Future studies should also seek to understand healthy neuroticism using different operational definitions such as higher-order traits, the interaction between neuroticism and subjective health, or possibly trait by stimulus interactions.
Constraints on generality
The set of studies used in this coordinated analysis is not comprehensive. The included studies are largely WEIRD samples (i.e., Westernized, Educated, Industrialized, Rich, and Democratic; Henrich, Heine, & Norenzayan, 2010). As such, our results may not generalize to Eastern cultures or less-industrialized countries. Additionally, we also cannot confidently conclude that our results would generalize to disadvantaged populations within the cultures studied here. Results may also be limited to the health behaviors that we studied, and may not generalize to other health behaviors such as diet/nutrition, other drug use, or sleep behavior. We believe these results would generalize to measures of personality that were not used in the present study, as there was little evidence that the present scales yielded different conclusions from each other, and we have no reason to believe these scales vary in systematic ways from other scales. We also believe that these results are likely to generalize over time, as both the personality and health measurements varied across time within this project, and the behaviors studied hereare fairly stable over time (Greenfield & Kerr, 2003; Weinberger, Pilver, Mazure, & McKee, 2014); thus, these results would be expected in samples collected in the past and also the foreseeable future. Model generalizability is constrained by the fact of missing data in these models. For any longitudinal panel study, attrition causes bias in the results. Given that the first occasion of personality assessment did not always occur at the study’s initial measurement occasion, it may be the case that participants who become ill or die between waves may be missing, thus selecting out the most extremely ill cases. Additionally, certain personality characteristics (notably, agreeableness and openness; (Salthouse, 2013)) are associated with repeated participation in longitudinal studies, and so we may lose participants low in these traits from the sample over time.
The current study was limited by the data available. All measures were self-reported. The current study used binary coding to harmonize measures of health behaviors across studies. This choice was made to compare results across countries and measures of personality; however, we are unable to distinguish between different frequencies of use within a behavior (e.g., light vs. moderate vs. intense physical activity). It is possible that healthy neuroticism may explain differences in engaging in health behaviors, and also in the frequency of that behavior, and we would be unable to see this effect in the current analyses.
The current study, along with the others in this series, estimated population-level relationships between constructs through the coordinated analysis approach. One benefit of coordinated analysis is the ability to compare methods of data collection or cohorts to find the boundary conditions of an effect (Hofer & Piccinin, 2010). However, we found limited evidence of heterogeneity of effects across data sets. The observed effects of neuroticism and conscientiousness on health behaviors were similar across studies in different cultures, with different measures of personality, and across different time spans. This underscores our conclusion that the relationship of neuroticism to concurrent health behaviors is related to levels of conscientiousness.
Conclusion
Our results indicate that healthy neuroticism is associated with health behaviors. Individuals who were high in neuroticism and low in conscientiousness were more likely to engage in unhealthy behavior, but this association was ameliorated among individuals with higher conscientiousness. Neuroticism may, in some contexts, be related to lower odds of engaging in maladaptive behavior. The current study is the third of three studies rigorously testing the healthy neuroticism hypothesis. The conclusions of the current study stand in contrast to the prior two, which found that the relationship between neuroticism and mortality and the relationship between neuroticism and chronic condition status and development do not differ across levels of conscientiousness. Together, the three studies in this coordinated project suggest that while it may be true that so-called healthy neurotics engage in slightly better health behaviors, this effect is not substantial enough to impact overall health.
Acknowledgments
We would like to thank Brenton Wiernik who consulted on and wrote the R function to perform these analyses.
This project was made possible by funding from the NIA (P01AG043362, R01-AG1843, R01-AG067622, R01-AG064006, K01AG050823, R01AG017917, P30AG010161, R01AG10569, T32AG000037, P01AG03949, R01-AG032037, R29-AG07465, R01-AG-002287, R01AG055653, R01AG056486); Dietmar Hopp Stiftung; German Federal Ministry for Family, Senior Citizens, Women, and Youth (Grant Ref. 314-1722-102/16 and 301-1720-295/2); National Health and Medical Research Council (ID: 568969); NHMRC Australia (APP1100579); German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF) under grant numbers #16SV5536K, #16SV5537, #16SV5538, #16SV5837, #01UW0808; #01GL1716A; and #01GL1716B); Social Sciences and Humanities Research Council of Canada (SSHRC); Alzheimer Society Research Program (ASRP); Czap Foundation; Sylvia & Leonard Marx Foundation; Age UK; Medical Research Council; Biological Sciences Research Council (MR/K026992/1).
Footnotes
Competing interests: No competing interests exist.
Data accessibility: R scripts and meta-data (e.g., coefficients estimated from individual datasets) are available on osf.io/48fhe. Raw data can be obtained through the following websites or emailing the following researchers: - BASE-II: Swantje Müller (swantje.mueller@hu-berlin.de) - EAS: Ruixue Zhaoyang ((rzz12@psu.edu)[rzz12@psu.edu]) - ELSA: https://www.elsa-project.ac.uk/ - HRS: http://hrsonline.isr.umich.edu/ - ILSE: Damaris Aschwanden ((Damaris.Aschwanden@med.fsu.edu)[Damaris.Aschwanden@med.fsu.edu]) - LBC-1936: Tom Booth ((tbooth1@exseed.ed.ac.uk)[tbooth1@exseed.ed.ac.uk]) - LBLS: Kristi M. Wisniewski ((kwisniew@usc.edu)[kwisniew@usc.edu]) - MAP: Bryan D. James ((Bryan_James@rush.edu)[Bryan_James@rush.edu]) - MAS: Fleur Harrison ((f.harrison@unsw.edu.au)[f.harrison@unsw.edu.au]) - MIDUS: http://midus.colectica.org/ - NAS: Avron Spiro ((aspiro3@bu.edu)[aspiro3@bu.edu]) - OATS: Steven R. Makkar ((stevem@unsw.edu.au)[stevem@unsw.edu.au]) - ROS: Bryan D. James ((Bryan_James@rush.edu)[Bryan_James@rush.edu]) - SLS: Swantje Müller (swantje.mueller@hu-berlin.de) - WLS: https://www.ssc.wisc.edu/wlsresearch/
References
- Aschwanden D, Kliegel M, & Allemand M (2018). Cognitive complaints mediate the effect of cognition on emotional stability across 12 years in old age. Psychology and Aging, 33(3), 425–438. 10.1037/pag0000246 [DOI] [PubMed] [Google Scholar]
- Bennett DA, Buchman AS, Boyle PA, Barnes LL, Wilson RS, & Schneider JA (2018). Religious Orders Study and Rush Memory and Aging Project. Journal of Alzheimer’s Disease, 64(s1), S161–S189. 10.3233/JAD-179939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Arvanitakis Z, & Wilson RS (2012). Overview and Findings from the Religious Orders Study. Current Alzheimer Research, 628–646. 10.2174/156720512801322573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett DA, Schneider JA, Buchman AS, Barnes LL, Boyle PA, & Wilson RS (2012). Overview and findings from the Rush Memory and Aging Project. Current Alzheimer Research, 9(6), 646–663. 10.2174/156720512801322663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertram L, Bockenhoff A, Demuth I, Duzel S, Eckardt R, Li S-C, … Wagner GG (2013). Cohort profile: the Berlin aging study II (BASE-II). International Journal of Epidemiology, 43(3), 703–712. 10.1093/ije/dyt018 [DOI] [PubMed] [Google Scholar]
- Bosse R, Ekerdt D, & Silbert J (1984). The Veteran Administration Normative Aging Study In Mednick SA, Harway M, & Finello KM (Eds.), Handbook of longitudinal research vol. teenage and adult cohorts (pp. 273–289). New York. [Google Scholar]
- Brim OG, Ryff CD, & Kessler RC (2004). How Healthy Are We? A National Study of Well-Being At Midlife. Chicago: University of Chicago Press. [Google Scholar]
- Condon DM, Graham EK, & Mroczek DK (2017). On Replication Research In The Wiley-Blackwell encyclopedia of personality and individual differences: Vol. ii. research methods and assessment techniques. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Costa PT Jr, & McCrae RR (1985). The NEO Personality Inventory manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Friedman HS (2000). Long-Term Relations of Personality and Health: Dynamisms, Mechanisms, Tropisms. Journal of Personality, 68(6), 1–19. [DOI] [PubMed] [Google Scholar]
- Friedman HS (2019). Neuroticism and health as individuals age. Personality Disorders: Theory, Research, and Treatment, 10(1), 25–32. 10.1037/per0000274 [DOI] [PubMed] [Google Scholar]
- Gale CR, Čukić I, Batty GD, McIntosh AM, Weiss A, & Deary IJ (2017). When Is Higher Neuroticism Protective Against Death? Findings From UK Biobank. Psychological Science, 28(9), 1345–1357. 10.1177/0956797617709813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D, Bertram L, Lindenberger U, Pawelec G, Demuth I, Steinhagen-Thiessen E, & Wagner GG (2016). The Berlin Aging Study II - An overview. Gerontology, 62(3), 311–315. 10.1159/000441495 [DOI] [PubMed] [Google Scholar]
- Goldberg LR (1992). The development of markers for the Big-Five factor structure. Psychological Assessment, 4(1), 26–42. [Google Scholar]
- Goldberg LR, Johnson JA, Eber HW, Hogan R, Ashton MC, Cloninger CR, & Gough HG (2006). The international personality item pool and the future of public-domain personality measures. Journal of Research in Personality, 40(1), 84–96. 10.1016/j.jrp.2005.08.007 [DOI] [Google Scholar]
- Graham EK, Bastarache ED, Milad E, Turiano NA, Cotter KA, & Mroczek DK (2018). Physical activity mediates the association between personality and biomarkers of inflammation. SAGE Open Medicine, 6(9), 1–10. 10.1177/2050312118774990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham EK, Rutsohn JP, Turiano NA, Bendayan R, Batterham PJ, Gerstorf D, … Mroczek DK (2017). Personality predicts mortality risk: An integrative data analysis of 15 international longitudinal studies. Journal of Research in Personality, 70, 174–186. 10.1016/j.jrp.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield TK, & Kerr WC (2003). Tracking alcohol consumption over time. Alcohol Research & Health, 27(1), 30–38. [PMC free article] [PubMed] [Google Scholar]
- Hagger-Johnson G, Roberts B, Boniface D, Sabia S, Batty GD, Elbaz A, … Deary IJ (2012). Neuroticism and Cardiovascular Disease Mortality. Psychosomatic Medicine, 74(6), 596–603. 10.1097/PSY.0b013e31825c85ca [DOI] [PubMed] [Google Scholar]
- Hedges LV, & Pigott TD (2004). The power of statistical tests for moderators in meta-analysis. Psychological Methods, 9(4), 426–445. 10.1037/1082-989X.9.4.426 [DOI] [PubMed] [Google Scholar]
- Henrich J, Heine SJ, & Norenzayan A (2010). The weirdest people in the world? Behavioral and Brain Sciences, 33(2-3), 61–83. 10.1017/S0140525X0999152X [DOI] [PubMed] [Google Scholar]
- Herd P, Carr D, & Roan C (2014). Cohort profile: Wisconsin Longitudinal Study (WLS). International Journal of Epidemiology, 43(1), 34–41. 10.1093/ije/dys194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer SM, & Piccinin AM (2009). Integrative data analysis through coordination of measurement and analysis protocol across independent longitudinal studies. Psychological Methods, 14(2), 150–164. 10.1037/a0015566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofer SM, & Piccinin AM (2010). Toward an Integrative Science of Life-Span Development and Aging. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 65B(3), 269–278. 10.1093/geronb/gbq017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Baker KL, & Morey LC (2008). Personality and drugs of choice. Personality and Individual Differences, 44(6), 1413–1421. 10.1016/j.paid.2007.12.009 [DOI] [Google Scholar]
- Hopwood CJ, Morey LC, Skodol AE, Stout RL, Yen S, Ansell EB, … McGlashan TH (2007). Five-Factor Model Personality Traits Associated With Alcohol-Related Diagnoses in a Clinical Sample. Journal of Studies on Alcohol and Drugs, 68(3), 455–460. 10.15288/jsad.2007.68.455 [DOI] [PubMed] [Google Scholar]
- John OP, & Srivastava S (1999). The Big Five trait taxonomy: HIstory, measurement, and theoretical perspectives In Handbook of personality theory and research (pp. 102–138). New York: New York. [Google Scholar]
- Katz MJ, Lipton RB, Hall CB, Zimmerman ME, Sanders AE, Verghese J, … Derby CA (2012). Age-specific and sex-specific prevalence and incidence of mild cognitive impairment, dementia, and Alzheimer dementia in blacks and whites: A report from the Einstein Aging Study. Alzheimer Disease & Associated Disorders, 26(4), 335–343. 10.1097/WAD.0b013e31823dbcfc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, & Weaver SL (1997). The Midlife Development Inventory (MIDI) Personality Scales.
- Lüdecke D (2018). SjPlot: Data visualization for statistics in social science. 10.5281/zenodo.1308157 [DOI]
- Marmot MG, Oldfield Z, Clemens S, Blake M, Phelps A, Nazroo J, … Oskala A (2017). English Longitudinal Study of Ageing: Waves 0-7, 1998-2015.
- Murray AL, & Booth T (2015). Personality and physical health. Current Opinion in Psychology, 5, 50–55. 10.1016/j.copsyc.2015.03.011 [DOI] [Google Scholar]
- Nelson LD, Simmons J, & Simonsohn U (2018). Psychology’s Renaissance. Annual Review of Psychology, 69(1), 511–534. 10.1146/annurev-psych-122216-011836 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2018). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.R-project.org/ [Google Scholar]
- Sachdev PS, Brodaty H, Reppermund S, Kochan NA, Trollor JN, Draper B, … the Memory and Ageing Study Team. (2010). The Sydney Memory and Ageing Study (MAS): methodology and baseline medical and neuropsychiatric characteristics of an elderly epidemiological non-demented cohort of Australians aged 7090 years. International Psychogeriatrics, 22(08), 1248–1264. 10.1017/S1041610210001067 [DOI] [PubMed] [Google Scholar]
- Sachdev PS, Lammel A, Trollor JN, Lee T, Wright MJ, Ames D, … OATS research team. (2012). A Comprehensive Neuropsychiatric Study of Elderly Twins: The Older Australian Twins Study. Twin Research and Human Genetics, 12(06), 573–582. 10.1375/twin.12.6.573 [DOI] [PubMed] [Google Scholar]
- Salthouse TA (2013). Selectivity of attrition in longitudinal studies of cognitive functioning. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(4), 567–574. 10.1093/geronb/gbt046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattler C, Wahl H-W, Schröder J, Kruse A, Schönknecht P, Kunzmann U, & Zenthofer A (2015). Interdisciplinary Longitudinal Study on Adult Development and Aging (ILSE) In Pachana N (Ed.), Encyclopedia of geropsychology (pp. 1–10). [Google Scholar]
- Schaie KW, Willis SL, & Caskie GIL (2004). The Seattle Longitudinal Study: Relationship between personality and cognition. Aging, Neuropsychology, and Cognition, 11(2-3), 304–324. 10.1080/13825580490511134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan MJ, Hill PL, Roberts BW, Eccles J, & Friedman HS (2014). Conscientiousness, health, and aging: The Life Course of Personality Model. Developmental Psychology, 50(5), 1407–1425. 10.1037/a0031130 [DOI] [PubMed] [Google Scholar]
- Simons DJ, Shoda Y, & Lindsay DS (2017). Constraints on Generality (COG): A Proposed Addition to All Empirical Papers. Perspectives on Psychological Science, 12(6), 1123–1128. 10.1177/1745691617708630 [DOI] [PubMed] [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR (2014). Cohort Profile: the Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor AM, Pattie A, & Deary IJ (2018). Cohort Profile Update: The Lothian Birth Cohorts of 1921 and 1936. International Journal of Epidemiology, 47(4), 1042–1042r. 10.1093/ije/dyy022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Chapman BP, Gruenewald TL, & Mroczek DK (2015). Personality and the leading behavioral contributors of mortality. Health Psychology, 34(1), 51–60. 10.1037/hea0000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Mroczek DK, Moynihan J, & Chapman BP (2013). Big 5 personality traits and interleukin-6: Evidence for healthy Neuroticism in a US population sample. Brain Behavior and Immunity, 28, 83–89. 10.1016/j.bbi.2012.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Whiteman SD, Hampson SE, Roberts BW, & Mroczek DK (2012). Personality and substance use in midlife: Conscientiousness as a moderator and the effects of trait change. Journal of Research in Personality, 46(3), 295–305. 10.1016/j.jrp.2012.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Erp S, Verhagen J, Grasman RP, & Wagenmakers E-J (2017). Estimates of between-study heterogeneity for 705 meta-analyses reported in psychological bulletin from 1990–2013. Journal of Open Psychology Data, 5(1). 10.5334/jopd.33 [DOI] [Google Scholar]
- Vazire S (2018). Implications of the Credibility Revolution for Productivity, Creativity, and Progress. Perspectives on Psychological Science, 13(4), 411–417. 10.1177/1745691617751884 [DOI] [PubMed] [Google Scholar]
- Viechtbauer W (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. Retrieved from http://www.jstatsoft.org/v36/i03/ [Google Scholar]
- Vollrath M, & Torgersen S (2002). Who takes health risks? A probe into eight personality types, 32(7), 1185–1197. 10.1016/S0191-8869(01)00080-0 [DOI] [Google Scholar]
- Weinberger AH, Pilver CE, Mazure CM, & McKee SA (2014). Stability of smoking status in the us population: A longitudinal investigation. Addiction, 109(9), 1541–1553. 10.1111/add.12647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston SJ, & Jackson JJ (2015). Identification of the healthy neurotic: Personality traits predict smoking after disease onset. Journal of Research in Personality, 54(C), 61–69. 10.1016/j.jrp.2014.04.008 [DOI] [Google Scholar]
- Weston SJ, & Jackson JJ (2016). How do people respond to health news? The role of personality traits. Psychology & Health, 31(6), 637–654. 10.1080/08870446.2015.1119274 [DOI] [PubMed] [Google Scholar]
- Weston SJ, Graham EK, & Piccinin A (2019). Coordinated data analysis: A new method for the study of personality and health In Hill P & Allemand M (Eds.), Personality and healthy aging in adulthood. Springer Nature; 10.31234/osf.io/k9up8 [DOI] [Google Scholar]
- Weston SJ, Hill PL, Edmonds GW, Mroczek DK, & Hampson SE (2018). No Evidence of healthy neuroticism in the Hawaii Personality and Health Cohort. Annals of Behavioral Medicine, 11(5), 426–441. 10.1093/abm/kay055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H (2009). Ggplot2: Elegant graphics for data analysis. Springer-Verlag; New York: Retrieved from http://ggplot2.org [Google Scholar]
- Zelinski EM, & Kennison RF (2008). The Long Beach Longitudinal Study: Evaluation of Longitudinal Effects of Aging on Memory and Cognition. Home Health Care Services Quarterly, 19(3), 45–55. 10.1300/J027v19n03_04 [DOI] [PubMed] [Google Scholar]


