Abstract
The need for brief, low-cost, easily disseminable and effective interventions to promote healthy lifestyles is high. This is especially true for mental health providers. We developed two studies to compare the impacts of Cognitive Behavioral Stress Management (CBSM) and Yoga Based Stress Management (YBSM) interventions for healthcare professionals. Study 1 offered an 8-week YBSM intervention to 37 mental healthcare participants and collected health data pre and post. Study 2 offered YBSM and CBSM classes to 40 randomly assigned mental healthcare providers and collected mental and physical health data at four time points. In Study 1, using t-tests, the YBSM intervention affected a number of mental and physical wellbeing indices pre to post. In Study 2, using linear mixed modeling, both YBSM and CBSM groups improved significantly (p <.05) in fruit and vegetable intake, heart rate, alcohol consumption, relaxation and awareness, professional quality of life, compassion satisfaction, burnout, depression, and stress levels. There was a group by time effect for coping confidence (CBSM increased more, p<.05, F = 4.34), physical activity (YBSM increased more, p<.05, F = 3.47), overall mental health (YBSM increased more, p<.10, F =5.32), and secondary traumatic stress (YBSM decreased more, p<.10, F = 4.89). YBSM and CBSM appear to be useful for healthcare professionals’ mental and physical health. YBSM demonstrates some benefit above and beyond the extremely well-studied and empirically supported CBSM, including increased physical activity, overall mental health, and decreased secondary traumatic stress benefits.
Keywords: workplace, health, stress, stress management, intervention, yoga
Workplace stress can compromise employees’ mental and physical health and significantly contribute to corporate health care costs (Eisen, Allen, Bollash, & Pescatello, 2008). Stress is associated with elevated blood pressure, weight gain, anger, depression, anxiety, and poorer health-related quality of life along with worse health behaviors such as diet, exercise, and alcohol use (Park & Iacocca, 2014). Recent estimates put the overall annual cost of work-related stress to the United States economy at $300 billion (European Agency for Safety and Health at Work, 2014). These costs are due in large part to turnover and absenteeism, both of which increase with higher levels of workplace stress (Bureau of Labor Statistics, 2001).
While studies have found high levels of work-related stress across occupations, frontline mental healthcare providers—personnel who provide direct services to those with serious mental health issues, including nurses, social workers, psychologists, aides, case managers, and occupational therapists-- may be particularly prone to stress exposure (e.g., Gaither et al., 2008; Lee et al., 2012; Thorsteinsson et al., 2014). Frontline mental healthcare providers’ stressors include a high workload, demanding caregiving relationships with patients, secondary traumatization, and potentially difficult interactions with other mental health professionals on multidisciplinary teams. Finally, patient suicide is a major stressor, after which a majority of mental healthcare providers report symptoms of post-traumatic stress (Rossler, 2012). This group’s high stress levels may adversely affect their mental and physical health as well as their work performance and satisfaction. For example, burnout, involving work-related anger, frustration, and exhaustion, is particularly prevalent among frontline mental health providers (Leiter & Maslach, 2004; Aiken et al., 2002; Janssen et al., 1999; Laschinger et al., 2001; Acker, 2011; Lasalvia et al., 2009; Paris & Hoge, 2010). Reducing stress may be essential for maintaining job satisfaction and preventing turnover among frontline mental health providers as well as for promoting their mental and physical well-being.
Employer-based stress management and yoga programs
Research has accrued supporting the benefits of short-term stress management programs on mental and physical wellbeing (e.g., Cognitive Behavioral Stress Management [CBSM; Antoni, 2006], cognitive-behavioral therapy (Granath, Ingvarsson, von Thiele, & Lundberg, 2006), relaxation, and mindfulness-based stress reduction [MBSR; Kabat-Zinn, 2001]; Shapiro et al., 2011; Winterdyk et al., 2008). An earlier meta-analysis of workplace-based stress management interventions found cognitive-behavioral interventions to be more effective than relaxation-based and other stress management modalities (van der Klink et al., 2001). However, the most recent review of 36 studies of stress management interventions, including cognitive-behavioral, relaxation, organizational, alternative, and multimodal, found that all five categories of stress management interventions were effective in reducing workplace stress (Richardson & Rothstein, 2008).
Only in the past decade has yoga been examined as a workplace wellness modality, with emerging literature suggesting that yoga may successfully reduce workplace stress (e.g., Granath et al., 2006; Shu-Ling Lin et al., 2015). Yoga is unique in its mindfulness and exercise components for stress management, in addition to being more desired by many participants than more traditional stress management interventions (e.g., Chong et al, 2011; Shu-Ling Lin et al., 2015). In one study, a group receiving yoga reported significant reductions in perceived stress and back pain, and a substantial improvement in psychological well-being, compared to a control group (Hartfiel et al., 2012). These findings have been replicated and extended by studies demonstrating that yoga improved musculoskeletal fitness, state anxiety (Cheema et al., 2013), perceived stress, sleep quality, and heart rate variability (Wolever et al., 2012). Yoga has been shown to be efficacious in improving a range of health conditions, including depression obesity, diabetes, substance abuse, and asthma (Ross, 2010). One study of employee wellness in a large financial company found that both yoga and cognitive stress management programs were related to improvements in well-being and decreases in stress (Granath et al., 2006). Therefore, we anticipated that combining the documented salutary effects of yoga with the strong, well-supported aspects of cognitive stress management may provide a potent intervention in the workplace.
The Present Study
We designed and tested an eight-week workplace wellness intervention combining yoga and aspects of cognitive stress management, or Yoga Based Stress Management (YBSM; Wilson & Cope, 2010). To our knowledge, no such intervention combination has been studied in previous literature. This new type of intervention is a manualized yoga intervention is based on the principles of Kripalu yoga, which conceptualizes yogic practices as an opportunity to cultivate mindfulness. This intervention also integrates psychoeducation on stress management consistent with yogic techniques and principles, similar to Mindfulness-Based Stress Reduction.
We tested this intervention and its impacts on mental and physical health in frontline mental healthcare providers in a pre-post pilot study for feasibility and preliminary efficacy (Study 1). We then conducted a second study in which we compared it directly to a traditional Cognitive-Behavioral Stress Management (CBSM; Antoni et al., 2006) intervention with mental healthcare providers, measuring changes in a range of well-being indices for a period of eight months (Study 2). CBSM was originally developed to reduce stress and improve a range of psychological and physical benefits for persons with HIV and cancer survivors. Reported effects include more positive and less negative affect, decreased stress, and less depression and anxiety (Antoni et al., 2000a,b; Antoni et al., 2006; Penedo et al., 2006). CBSM has been shown to be efficacious for a number of clinical populations and samples, though has yet to be tested in a non-clinical population. For the present study the CBSM protocol was adapted from the 10 week, 1.5 hour per session per week protocol to an 8 week, 1 hour per session per week protocol. This study provides a secondary aim of examining the effects and potential feasibility of CBSM in a non-clinical population.
We selected an understudied but highly stressed group, mental healthcare providers (Gökçen et al., 2013; Weaver, 1984; Chen et al., 2014; Corrigan, 1995). In spite of their high workplace stress, this group has rarely been the focus of workplace stress management interventions. Further, this population allowed us to test whether stress management programs reduce burnout, a serious and common issue for this group.
There are two additional strengths of Study 2. First, because nearly all of the research on workplace stress-management or wellness programs have short-term follow-up periods (i.e., most measured participants only at end of intervention), the extent to which effects endure beyond the intervention itself remains unknown. Thus, we implemented a longer-term follow up to determine whether the effects of such programs last. Second, because many stress management programs have specifically focused only on stress and emotional well-being (e.g., Sidle, 2008; Horan, 2002; McCraty et al., 2003; Lapp et al., 2000), we aimed to determine whether such programs have broader impacts on well-being, including quality of life and health behaviors as well as stress and burnout.
In sum, building on preliminary evidence that suggests that both cognitive stress management interventions and yoga interventions are effective in promoting health and reducing stress, this study sought to add useful elements from cognitive stress management to yoga to form a yoga-based stress management intervention (YBSM), and then examine the differential effectiveness of YBSM and standard CBSM on a set of mental and physical health indices, including diet, exercise, sleep, stress, depression, anxiety, alcohol use and compassion fatigue/burnout. The ultimate goal of this line of research is to test yoga-based and cognitive behavioral-based stress management interventions for preventive and health-promotive impacts, understand more about how and why such interventions can be efficacious, and refine and disseminate them to at-risk populations such as frontline mental healthcare providers through work-based yoga interventions and interventions. This study also examined feasibility of these interventions in a non-clinical yet highly stressed population.
Study 1
Study 1 aimed to examine preliminary feasibility and efficacy of a YBSM intervention for frontline mental healthcare providers and to examine preliminary effects of this intervention on a range of psychological and physical wellbeing outcomes in a pre-post study.
Method
Participants
Forty four employees of Clinical and Support Options (CSO), a multi-site mental health center with locations throughout western Massachusetts, were recruited and enrolled. Thirty-seven participants completed both time 1 (baseline) and time 2 (end of intervention) surveys; 7 participants completed only the time 1 survey. There were no statistically significant differences between those who completed both surveys and those who did not on major demographic variables. Of the final 37 participants who completed both surveys, 83.8% were female and 83.8% were Caucasian. Mean age was 41.2 (5.7).
Procedure
CSO has several hundred employees including frontline mental healthcare providers and administrative staff. The CSO conducted a workplace wellness program with the YBSM intervention. Once participants signed up for the program, they were invited via email and phone to participate in a research study by completing questionnaires.
Participants who expressed interest in participating in the study were sent a link for an online survey and an online consent form two to three weeks before the start of the study and one week following the end of the eight week intervention. Study participants completed the online surveys before the start of the first class.
Measures
Depression, Anxiety, and Stress.
Distress was assessed with the 21-item Depression, Anxiety and Stress Scale (DASS-21) (Lovibond & Lovibond, 1995). The DASS-21 comprises three seven-item subscales: depression (“I found it difficult to work up the initiative to do things”), anxiety (“I found it hard to wind down”), and stress (“I found it difficult to relax”). For each statement, participants are asked to rate how much a given statement applied to them “over the past week.” The DASS has good reliability and validity (e.g., Gloster et al., 2008; Lovibond & Lovibond, 1995).
Health-related quality of life: Physical and mental health.
The SF-12 health-related quality of life measure consists of 12 items and produces separate scores for a mental health-related quality of life component (MCS) and a physical health-related quality of life component (PCS; Ware, Kosinski, & Keller, 1996). An example of a mental health item is “how much of the time in the past two weeks have you felt downhearted and blue?” on Likert scale from 1 (all of the time) to 6 (none of the time). An example of a physical health item includes “during the past four weeks, how much did pain interfere with your normal work (including both work outside the home and housework)?” Items were answered on yes/no or Likert scales. The SF-12 is widely used in research on quality of life (Grozdev, 2012).
Coping Skills.
Coping skills were assessed with the 13-item Measure of Current Status (MOCS-A; Carver, 2006). Participants respond to each question on a 5-point Likert scale from 1 (I cannot do this at all) to 5 (I can do this extremely well). The MOCS-A has been shown to be reliable and valid (Philips et al, 2011; Antoni et al, 2006). The MOCS-A has five subscales; we examined three subscales as a part of this study: coping skills, awareness, and relaxation subscales. A coping skills subscale item is “It’s easy for me to decide how to cope with whatever problems arise,” an awareness subscale item is “I notice right away whenever my body is becoming tense,” and a relaxation subscale is “I am able to use mental imagery to reduce any tension I have.” This scale has shown good validity and reliability in previous studies (Carver, 2006).
Emotion regulation.
Emotion regulation was assessed with the 36-item Difficulties in Emotion Regulation Scale (DERS). Six subscales include non-acceptance, goals, impulse, strategies, clarity, and awareness. Items are rated on a 5-point scale from 1 (Almost never) to 5 (Almost always) (Gratz & Roemer, 2004). The DERS was initially validated in adults (Gratz & Roemer, 2004).
Mindfulness.
The Five Facet Mindfulness Questionnaire (FFMQ) is a 39-item scale. Responses are given on a 5-point Likert scale and measure five facets of mindfulness: observing (attending to or noticing internal and external stimuli), describing (noting or mentally labeling these stimuli with words), acting with awareness (attending to one’s current actions), non-judging of inner experience (refraining from evaluations), and non-reactivity (allowing thoughts and feeling to come and go). The FFMQ has been widely studied and has been normed in non-clinical samples (Gill et al., 2007),
Self compassion.
Self-Compassion was assessed with the 26-item Self-Compassion Scale-Short Form (SCS; Raes, Pommier, Neff, & Van Gucht, 2011). Items are rated from 1 (Almost never) to 5 (Almost always) The SCS includes 6 subscales: self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. The SCS measures one’s ability to be forgiving and kind to oneself in difficult circumstances and was developed and validated on a non-clinical sample (Neff, 2003; Raes et al., 2011).
Results
To examine the feasibility of the YBSM intervention, participants reported on a scale of 1–10 (not at all to very much), the perceived enjoyment of this intervention (8.24), the perceived utility of this intervention (7.93), and how much they anticipate to use the skills learned in the future (8.12). Results demonstrated that participants found the intervention to be useful and enjoyable.
To examine preliminary efficacy of the YBSM intervention, we examined changes from pre-intervention to post-intervention on all measures. We used repeated measures t-tests for all comparisons. Analyses showed statistically significant (p<.05) increases in relaxation, coping confidence, self-kindness, self-compassion, general mental health, general physical health, and mindfulness (See Table 1). Further, depression, anxiety, stress, impulse control difficulties, and limited access to emotion regulation strategies all decreased. There was no change in assertiveness, self-judgment, isolation, lack of emotional awareness, or lack of emotional clarity pre- to post- intervention.
Table 1.
Study 1 T-tests and chi square tests for pre- to post-intervention outcomes
| Time 1 Mean (SD) | Time 2 Mean (SD) | |
|---|---|---|
| DASS Depression* | 2.72 (1.49) | 1.63 (1.26) |
| DASS Anxiety† | 3.10 (1.07) | 2.12 (1.16) |
| DASS Stress** | 5.78 (1.16) | 4.08 (1.15) |
| MOCS Relaxation* | 2.87 (.96) | 3.30 (1.06) |
| MOCS Awareness | 3.56 (.90) | 3.66 (.86) |
| MOCS Assertion | 3.38 (.86) | 3.58 (.96) |
| MOCS Coping Confidence* | 3.54 (.60) | 3.81 (.61) |
| SCS Self Kindness** | 3.89 (1.32) | 4.64 (1.52) |
| SCS Self Judgment | 3.46 (.98) | 3.32 (.92) |
| SCS Common Humanity* | 3.97 (1.43) | 4.58 (1.31) |
| SCS Isolation | 3.84 (1.09) | 3.80 (1.01) |
| SCS Mindfulness | 4.63 (1.45) | 4.93 (1.23) |
| SCS Overidentification | 3.68 (.87) | 3.76 (.78) |
| SF-12 MCS Mental Health† | 35.02 (9.17) | 42.68 (9.41) |
| SF-12 PCS Physical Health* | 40.85 (10.83) | 49.09 (6.54) |
| DERS Nonacceptance | 10.95 (3.80) | 10.19 (4.23) |
| DERS Difficulties Goals | 13.09 (2.87) | 12.57 (2.93) |
| DERS Impulse Control† | 11.45 (1.97) | 10.91 (2.14) |
| DERS Emotional Awareness | 23.05 (4.35) | 23.57 (4.23) |
| DERS Limited Access to Emotion Regulation Strategies* | 23.05 (4.37) | 23.57 (4.24) |
| DERS Lack of Emotional Clarity | 11.91 (1.16) | 11.83 (1.61) |
| FFMQ Mindfulness*** | 33.83 (6.07) | 42.76 (6.83) |
Note.
= p < .05,
= p <.01,
= p <.001,
= p < .10.
Discussion
Study 1 provided preliminary support for the feasibility and effectiveness of the YBSM intervention, suggesting this workplace-based intervention for mental healthcare providers may improve a range of aspects of mental and physical wellbeing, and that participants found the interventions appealing. These results suggest that YBSM may be successfully implemented into a wellness program in a mental healthcare system. Study 1 limitations include lack of a control group and short-term follow-up.
Study 2
After demonstrating preliminary feasibility and efficacy of YBSM in Study 1, we implemented Study 2 to provide a more rigorous and comprehensive test of YBSM by comparing its effects to those of another stress-management program that has been shown to be effective. In this randomized trial, we added additional outcomes including additional physical and health behavior outcomes and a measure of burnout, all important sequelae of stress that could be impacted by these interventions. These additional health measures provide a more comprehensive and holistic assessment of wellness and have been shown to provide invaluable and unique health information about wellbeing in previous research (e.g., Chae, Lee, Rifai, & Ridker, 2001). Additionally, including a measure of burnout has been shown to be important when examining workplace wellness and workplace intervention (e.g., Jacobson, 2008). Study 2 also examined longer-term treatment effects and included two longer-term follow-up assessments.
Method
Participants
Thirty-eight participants completed baseline questionnaires (YBSM = 19, CBSM = 19), 28 participants completed post-intervention Time 2 questionnaires, 25 participants completed Time 3 2-month-followup questionnaires, and 19 completed 6-month post-follow-up questionnaires. Based on t-tests and chi-square tests, drop-out participants did not differ significantly on any baseline variable from those who remained in the study. Groups did not differ significantly in attrition rate or demographic characteristic. Of the 38 participants who were recruited for the study, 84.2% were female and 94.7% were Caucasian. Mean age was 44.6 (6.2).
Procedure
Frontline mental health care providers were recruited via informational fliers that were distributed throughout the Department of Psychiatry at a large regional hospital in New England. Flyers included a contact number for interested employees to contact research coordinators for more information. To determine eligibility, potential participants completed the Physical Activity Readiness Questionnaire (PAR-Q; Canadian Society for Exercise Physiology, 2002), a 7-item questionnaire assessing individuals’ ability to engage in exercise without risk. Only potential participants who answered “No” to all of the PAR-Q items were eligible to participate in this study. Employees who attested to meeting all eligibility requirements underwent an informed consent process.
Participants were directed to an online, secure website (Qualtrics) to complete the online survey assessments at each of the four study timepoints. Baseline survey assessments were completed within three days after completing informed consent. After completing baseline measures, participants were emailed their randomized group assignment (CBSM or YBSM) and information on the meeting time and place of the assigned group. Two eight week sessions of the intervention were conducted with 20 participants; participants were randomized to one of the four treatment groups (2 sessions of 20 participants each). These 2 sessions were conducted partly simultaneously, with a 4 week overlap in start date. The two YBSM teachers were certified Kripalu yoga instructors and the two CBSM leaders were licensed clinical psychologists with training in cognitive behavioral therapy. Both interventions lasted 8 weeks and assessments were made pre- and post-intervention and at 2-month and 6-month follow-up. Participants received a small financial incentive ($20) for their time spent completing each set of questionnaires.
Measures
Measures from Study 1 and also included in Study 2 include depression, anxiety, and stress (DASS-21), health-related quality of life (SF-12), and coping skills (MOCS-A). Additional physical and mental wellbeing measures added to Study 2 are listed below.
Heart Rate, Blood Pressure, BMI.
Heart rate, blood pressure, height, and weight were measured by research assistants at the hospital at each time point. BMI was calculated by researchers using height and weight.
Fruit and Vegetable Intake.
Both fruit intake and vegetable intake were assessed with short, focused assessments referring to the past week using the NCI fruit and vegetable screener. This measure is listed on the NCI website (http://riskfactor.cancer.gov/diet/screeners/fruitveg/). Scoring algorithms produced a single number of average daily fruit and vegetable intake and percent energy from fat. Both assessments have been used in large-scale and more focused studies and have demonstrated reasonable validity (Thompson et al., 2002).
Physical Activity.
The Paffenbarger Physical Activity Questionnaire assessed habitual physical activity levels over the past month, including informal activities of daily living (e.g., city blocks walked, stairs climbed), leisure-time activities, and formal exercise (PPAQ; Paffenbarger, Wing, & Hyde, 1978). Activity scores in Kcal/wk were calculated based on sum of calories expended across durations and intensities of the different activities. The PPAQ has excellent reliability (Pereira et al., 1997) and predictive validity (Harris et al., 1994) and has been shown to be sensitive to changes during interventions (Jeffrey et al., 1998).
Alcohol Use.
Participants reported their intake of alcohol in the past two weeks. Consumption was assessed in terms of quantity and frequency, as well as the number of binge drinking episodes, as recommended by Kushner et al. (1994). One drink was defined as one 12-oz bottle of beer, one 4-oz glass of wine, one 12-oz bottle of wine cooler, or 1-oz of liquor straight or in a mixed drink. This measure has been used successfully in many studies of alcohol use, and shows good reliability and validity (e.g., Park, Armeli, & Tennen, 2004; Park & Levenson, 2002).
Tobacco Use.
Participants reported current smoking status, including how many cigarettes they smoked per day, a method of assessing cigarette smoking that are widely used and have demonstrated good validity in previous research (e.g., Welte et al., 2011).
Sleep Disturbance.
The NIH PROMIS instrument for sleep disturbance (SD), short form (4 items), was used to assess sleep disturbance. Items were rated on a 5-point Likert scale. PROMIS instruments are reliable and well-validated (www.nihpromise.org).
Depression.
In addition to the DASS-21 depression subscale, we administered the PHQ-9, which consists of 9 items designed to assess symptoms of depression based directly on the diagnostic criteria for major depressive disorder in the Diagnostic and Statistical Manual Fourth Edition (DSM-IV; Kroenke, Spitzer, & Williams, 2001). We removed the suicidality item because we were sampling a high-functioning population (Simon, 2013). The PHQ is widely used and has good psychometrics (Rathore et al., 2014).
Burnout, Compassion Satisfaction, Secondary Traumatic Stress.
The Professional Quality of Life (ProQol 5; Stamm, 2009) included 30 items that assessed burnout, compassion satisfaction, and secondary traumatization. The ProQol 5 has good psychometric qualities and has been widely used in mental health care provider populations (Stamm, 2009).
Results
Descriptive Statistics
The two intervention groups were statistically similar to each other on most demographic baseline variables. However, the sample of mental healthcare providers was, on average, significantly less stressed than national norms (Table 2). Additionally, maladaptive professional quality of life scores (compassion satisfaction, burnout, and secondary traumatic stress) were low compared to norms, but these published averages were drawn from those “helping people who experience suffering and trauma,” suggesting the possibility that this measure was normed among those dealing with greater trauma than would frontline mental healthcare providers, as in the current sample (See Table 2). The groups were slightly more depressed than national averages, at a trending significance (YBSM p = .086, CBSM p = .064). Additionally, this sample smoked less than the national average, with only two smokers in the study (one per group).
Table 2:
Comparison to national averages, t-tests
| National Norm Means (SD) | Group Means (SD) | |
|---|---|---|
| Heart Rate: | 80 (20) | CBSM: 68.10 (8.06) Yoga: 68.70 (10.01) |
| BMI | 26.6 (7.61) | CBSM: 28.98 (6.21) Yoga: 27.56 (5.28) |
| Fruit: | 1.12 (.58) | CBSM: 2.83 (4.37)** Yoga: 2.18 (1.50)* |
| Vegetable: | 1.65 (.70) | CBSM: 1.22 (.52) Yoga: 1.37 (.50) |
| Exercise: | 31.2 (8.26) | CBSM: 41.2 (10.1) Yoga: 35.4 (12.2) |
| Alcohol Amt: | 1.54 (1.12) | CBSM: 1.36 (1.22) Yoga: 2.46 (3.07)* |
| Alcohol Binge: | .32 (.22) | CBSM: .10 (.29)* Yoga: .31 (.63) |
| Tobacco Use: | 20.6 (3.2) | CBSM: 4.8 (1.2)** Yoga: 11.1 (3.1)** |
| Sleep: | 5.25 (1.32) | CBSM: 2.70 (.30) Yoga: 2.66 (.31) |
| MCS: | 50 | CBSM: 42.97 (6.25) Yoga: 42.29 (5.80) |
| PCS: | 50 | CBSM: 48.61 (5.04) Yoga: 48.34 (6.54) |
| MOCS aware: | 2.26 (.09) |
CBSM: 3.03 (.69) Yoga: 3.44 (.97) |
| MOCS cope: | 3.31 (.08) |
CBSM: 3.29 (.58) Yoga: 3.32 (.81) |
| MOCS relax | 2.81 (.21) | CBSM: 2.79 (.59) Yoga: 2.32 (.62) |
| DASS dep: | 3.18 (5.39) |
CBSM: 4.26 (3.82) Yoga: 2.66 (3.10) |
| DASS anx: | 2.25 (7.48) |
CBSM: 2.21 (1.69) Yoga: 1.89 (2.47) |
| DASS stress: | 5.16 (8.04) |
CBSM: 6.68 (3.62) Yoga: 6.22 (3.51) |
| Compassion Satisfaction: | 5 (1) | CBSM: 3.98 (.59) Yoga: 3.92 (.38) |
| Burnout: | 5 (1) | CBSM: 2.21 (.52)* Yoga: 2.32 (.41)* |
| Secondary Traumatic Stress: | 5 (1) | CBSM: 1.98 (.54)** Yoga: 1.85 (.48)** |
| Blood Pressure: | 122 (23.1) | CBSM:127 (2.8) Yoga: 131 (3.2) |
| PHQ-9: | 3.3 (3.8) | CBSM: 4.72 (1.70)t Yoga: 4.05 (1.75)t |
YBSM participants attended an average of 6.43 sessions (SD = 1.78) and CBSM participants attended an average of 6.13 sessions (SD = 1.86), a difference that was not statistically significantly different.
Linear Mixed Modeling
We used linear mixed modeling to examine time, group, and time by group interactions for the YBSM and CBSM groups on all outcomes (see Table 3). Linear mixed modeling controls for missing data by estimation (REML). Unstructured, compound symmetry, and AR1 models were run for each outcome variable. −2 Log Likelihood, AIC, and BIC levels were compared in the context of parameter and chi square differences for all presented models in order to choose the best fitting model for each outcome, and presented data met acceptable levels for good model fit (Burnham & Anderson, 2002).
Table 3.
Model summaries
| Estimated Marginal Means (Std Error) T1, T2, T3, T4 | F (p) Statistics | ||||
|---|---|---|---|---|---|
| Intercept | Group | Time | Group* Time | ||
| Heart Rate: | CBSM: 68.10 (1.99), 66.36 (2.38), 69.78 (2.97), 64.50 (2.57) Yoga: 68.70 (1.99), 68.73 (2.29), 67.33 (2.57), 62.72 (2.65) |
173.20 | 4.38 (.141) | 4.07 (.018)* | 4.12 (.122) |
| Blood Pressure: | CBSM: 122.10 (1.99), 124.36 (2.38), 132.78 (2.97), 122.50 (2.57) Yoga: 124.70 (1.99), 120.73 (2.29), 121.33 (2.57), 121.72 (2.65) |
1186.32 | .551 (.462) | 3.32 (.025)* | 2.09 (.108)* |
| BMI | CBSM: 21.54 (3.03), 22.18 (3.62), 23.69 (3.91), 21.48 (5.53) Yoga: 24.16 (3.03), 22.76 (3.62), 23.92 (4.29), 22å.39 (3.91) |
37.18 | 3.85 (.14) | .730 (.395) | 1.70 (.192) |
| Fruit: | CBSM: 2.83 (.67), 2.38 (.78), 2.65 (.87), 4.46 (.91) Yoga: 2.18 (.71), 1.91 (.78), 2.34 (.83), 3.98 (.91) |
4.66 | 55(4.6) | 2.98 (.037)* | .132 (.94) |
| Veg: | CBSM: 1.22 (.38), 2.11 (.44), 1.98 (.49), 5.71 (.52) Yoga: 1.37 (.40), 2.29 (.46), 2.16 (.48), 6.37 (.52) |
2.98 | 80(.38) | 25.15 (<.001)* | .128 (.94) |
| Exercise: | CBSM: 40.55 (11.07), 50.19 (12.99), 122.00 (21.20), 47.00 (25.98) Yoga: 35.20 (16.43), 41.00 (13.88), 55.69 (13.88), 55.79 (13.88) |
75.09 | 2.28 (.141) | 4.42 (.011)** | 2.83 (.046)* |
| Alc Amt: | CBSM: 1.35 (.57), 1.46 (.65), 1.22 (.71), 1.80 (.68) Yoga: 2.46 (.59), 2.22 (.72), 2.50 (.62), 2.72 (.65) |
23.71 | 1.55(.22) | .34 (.799) | 1.81 (.10) |
| Alc Binge: | CBSM: .08 (.24), 1.00 (.22), 0.0 (.28), .09 (.26) Yoga: .31 (.24), 1.00 (.22), .64 (.26), .60 (.27) |
1.13 | 1.55(.22) | 1.87 (.056)* | 1.86 (.11) |
| Tobacco Use: | CBSM: .95 (.22), .87 (.34), 1.00 (.11), .91 (.30) Yoga: .89 (.32), 1.93 (.26), .92 (.28), 1.00 (.10) |
1.13 | 1.55(.22) | .87 (.213) | .85 (.43) |
| Sleep: | CBSM: 21.35 (1.21), 21.29 (1.34), 20.8 (1.58), 20.82 (1.51) Yoga: 20.00 (1.24), 21.67 (1.44), 20.36 (1.51), 20.2 (1.58) |
1085.99 | .165 (.68) | .311 (.817) | .158 (.924) |
| MCS: | CBSM: 37.51 (2.73), 44.14 (3.27), 43.64 (3.53), 33.10 (5.00) Yoga: 41.23 (2.73), 40.84 (3.27), 43.40 (3.87), 46.62 (3.53) |
768.50 | .984 (.330) | 1.08 (.376) | 2.11 (.048)* |
| PCS: | CBSM: 47.54 (3.03), 45.18 (3.62), 43.69 (3.91), 54.48 (5.53) Yoga: 40.16 (3.03), 40.76 (3.62), 48.92 (4.29), 37.39 (3.91) |
837.18 | 3.85 (.06) | .630 (.601) | 2.70 (.061) |
| MOCSaware: | CBSM: 3.03 (.17), 3.64 (.20), 3.58 (.22), 3.49 (.23) Yoga: 3.44 (.18), 3.87 (.20), 4.09 (.21), 3.49 (.23) |
1209.34 | .457 (.503) | 8.32 (<.001)*** | 2.77 (.063) |
| MOCSrelax | CBSM: 3.29 (.15), 3.56 (.17), 3.50 (.20), 3.88 (.20) Yoga: 3.32 (.16), 3.45 (.17), 3.85 (.19), 3.46 (.20) |
1110.34 | .457 (.503) | 3.99 (.011)* | 2.77 (.072) |
| MOCScope: | CBSM: 3.29 (.15), 3.56 (.17), 3.50 (.20), 3.88 (.20) Yoga: 3.32 (.16), 3.45 (.17), 3.85 (.19), 3.46 (.20) |
1127.36 | .489 (.489) | 4.303 (.014)* | 3.42 (.038)* |
| PHQ-9 | CBSM: 4.26 (.63), 1.80 (.71), 2.50 (80), 1.92 (.83) Yoga: 2.67 (.65), 1.64 (.74), 1.23 (.77), 1.00 (.83) |
45.22 | 1.32(.26) | 4.56 (.004)** | .466 (.71) |
| DASS dep: | CBSM: 4.26 (.63), 1.80 (.71), 2.50 (80), 1.92 (.83) Yoga: 2.67 (.65), 1.64 (.74), 1.23 (.77), 2.00 (.83) |
45.22 | 1.32(.26) | 5.58 (.002)** | .466 (.71) |
| DASS anx: | CBSM: 2.21 (.47), 1.73 (.53), 1.50 (.59), 1.63 (.62) Yoga: 1.89 (.48), 1.60 (.55), 2.15 (.57), 1.64 (.62) |
1122.57 | .003 (.957) | 1.58 (.232) | 1.51 (.236) |
| DASS stress: | CBSM: 6.68 (.74), 3.80 (.83), 4.00 (.93), 3.54 (.97) Yoga: 6.22 (.76), 5.12 (.86), 5.46 (.90), 3.67 (.97) |
112.57 | .003 (.957) | 7.89 (.001)*** | 1.51 (.236) |
| Compassion Satisfaction: | CBSM: 3.99 (.13), 4.08 (.14), 3.98 (.16), 3.84 (.17) Yoga: 3.93 (.13), 4.00 (.14), 4.21 (.15), 4.16 (.17) |
2555.41 | .243 (.625) | 7.62 (.003)** | .651 (.590) |
| Burnout: | CBSM: 2.20 (.10), 3.08 (.11), 2.92 (.12), 3.14 (.13) Yoga: 2.32 (.10), 3.18 (.11), 3.21 (.12), 3.13 (.13) |
2650.82 | 142 (.244) | 4.57 (<.001)*** | .261 (.853) |
| Secondary Traumatic Stress: | CBSM: 1.98 (.11), 1.66 (.12), 1.71 (.13), 1.66 (.14) Yoga: 1.86 (.11), 1.81 (.121), 1.55 (.13), 1.63 (.14) |
639.02 | .001(.971) | 9.476 (<.001)*** | 1.92 (.096)* |
Time effects.
A number of indices improved significantly in both groups over the 8 month course of the study at the p=.05 level, including fruit intake (F = 2.98, p =.037), vegetable intake (F= 25.15, p <.001), MOCS relaxation (F= 9.93, p = <.001), MOCS awareness (F= 8.32, p = <.001), and compassion satisfaction (F= 762, p = .003). Measures that decreased included depression, as measured by both the DASS (F= 5.58, p = .002) and PHQ-9 (F= 4.56, p = .004), stress (F= 7.89, p = <.001), heart rate (F= 4.07, p = .018), alcohol consumption (binging; F= 1.87, p = .056), and burnout (F= 4.57, p = <.001).
Group effects.
There were no main effects by group for any variable; there were, however, time by group interactions.
Time by group interactions.
There were significant group by time interactions, such that one group improved above and beyond another on measured indices over time. The CBSM group increased more on MOCS Coping Confidence (F = 3.42, p < .05; see Figure 1). The YBSM group increased significantly more than the CBSM group on self-reported physical activity (F = 2.83, p<.05; see Figure 2). The YBSM group also decreased on secondary traumatic stress (F = 1.92; see Figure 3) and increased on the SF-12 MCS (F = 2.11; see Figure 4) at the p >.10 level. All figures were created from estimated marginal means.
Figure 1.
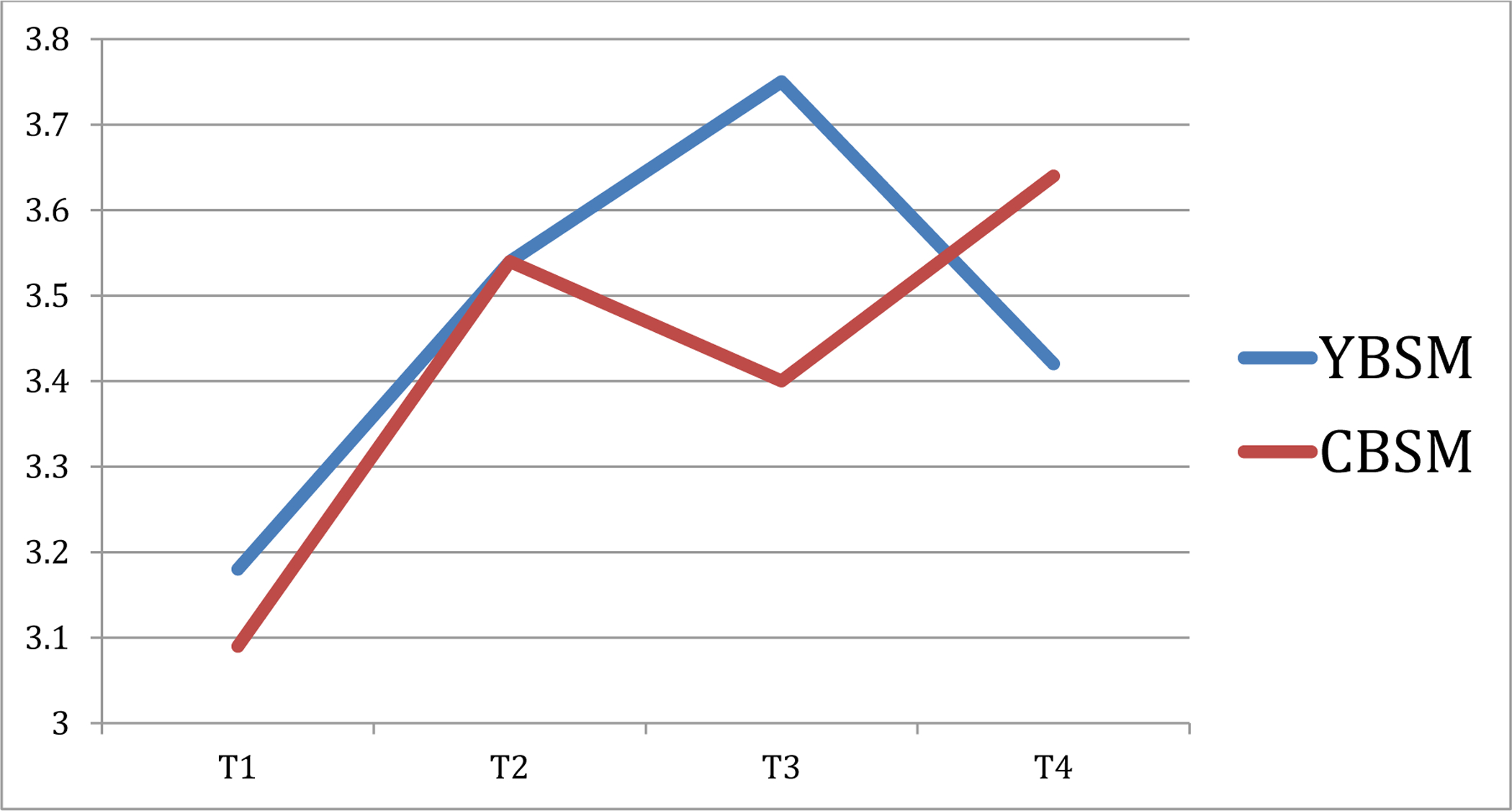
Time by Group Interaction, MOCS Coping Confidence
Figure 2.
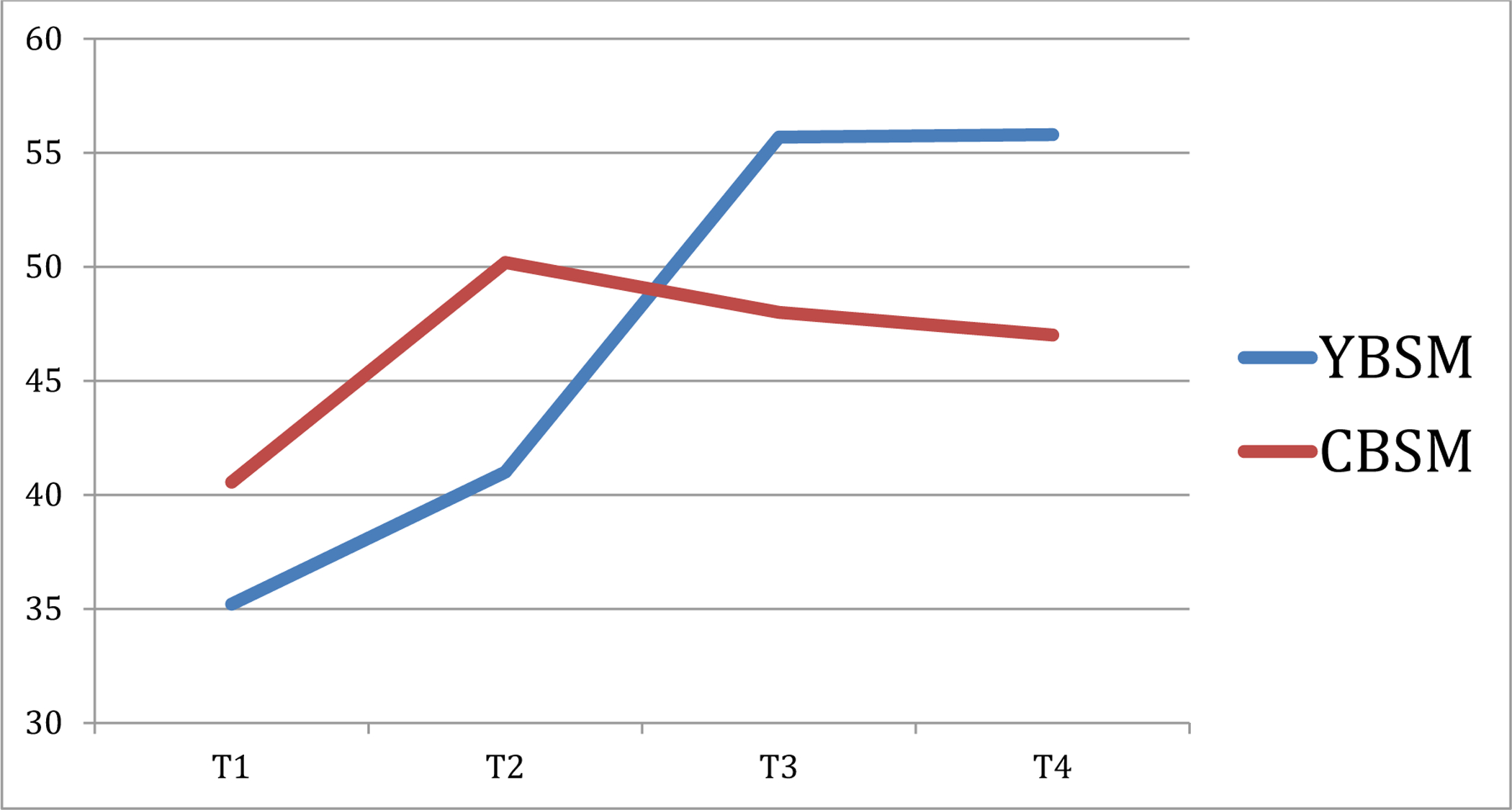
Time by Group Interaction, PAFF
Figure 3.
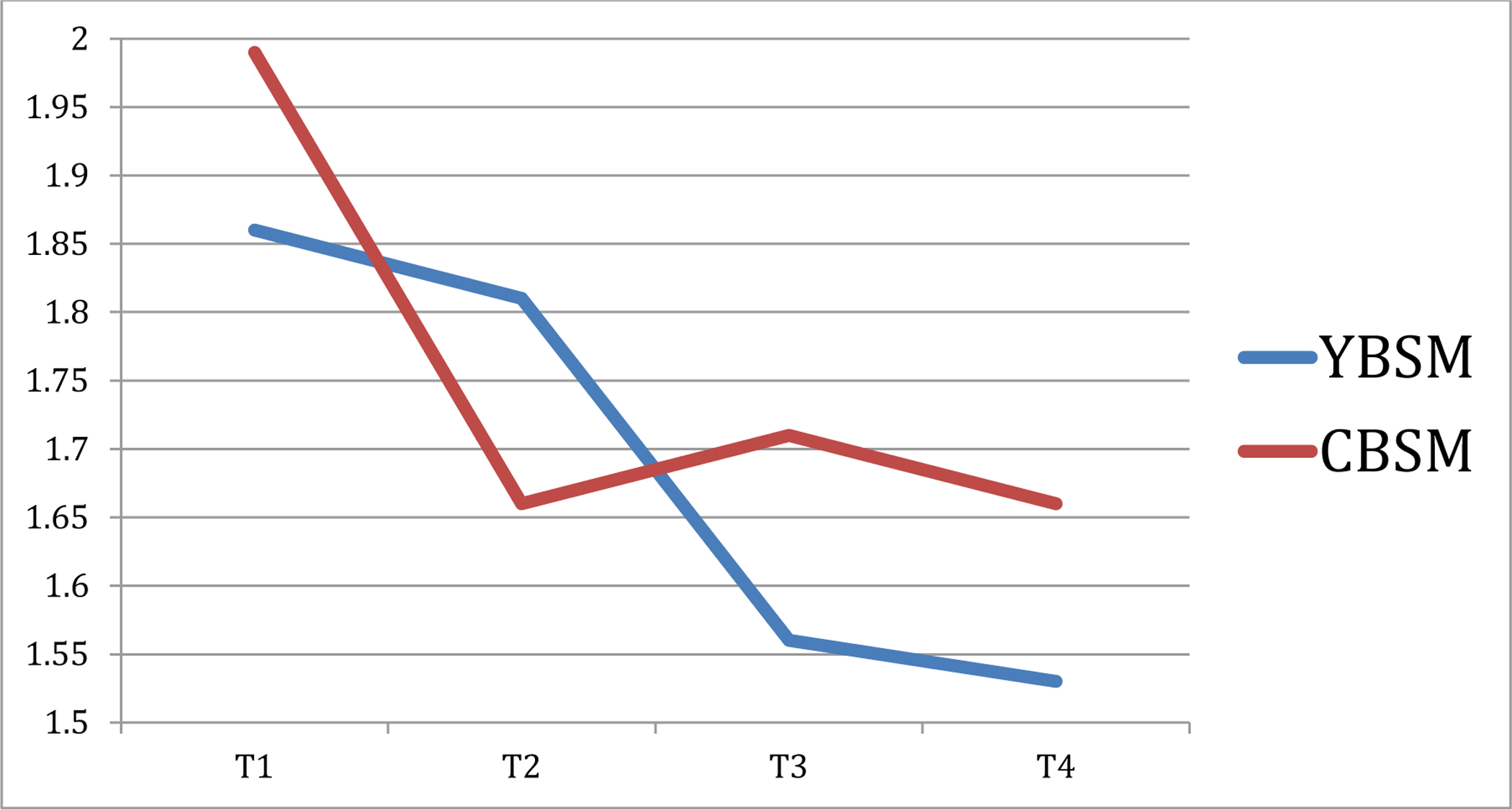
Time by Group Interaction, PROQOL Secondary Traumatic Stress
Figure 4.
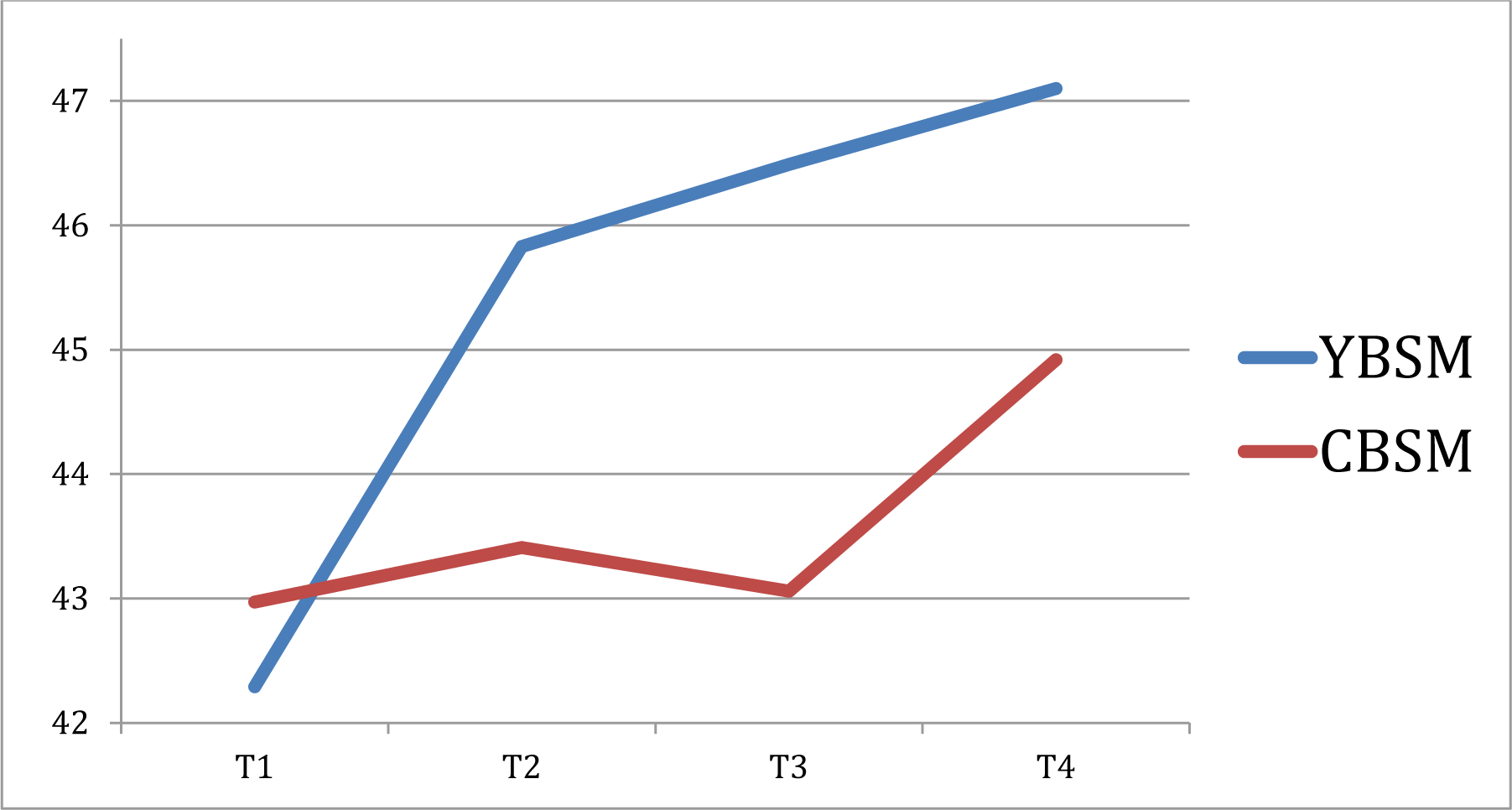
Time by Group Interaction, MCS Mental Health
No change.
There were no significant changes by group or over time in sleep quality, alcohol (total amount consumed), BMI, anxiety, cigarette smoking, or PCS.
Discussion
Study 2 showed that both the CBSM and YBSM groups evidenced significant improvements in health behaviors (fruit and vegetable intake, alcohol bingeing) and physical (decreased heart rate) health. Many improvements in mental health for both groups were also observed, including relaxation and awareness, professional quality of life (i.e., compassion satisfaction and burnout), depression, and stress. These findings indicate that two diverse programs that target the shared mechanism of stress management yield similarly beneficial effects on health.
Despite these similarities, differences between the group outcomes suggest important differential contributions or mechanisms of action between YBSM and CBSM. While the CBSM intervention appeared more effective at improving participants’ confidence in their ability to cope, YBSM was more effective at increasing non-yoga self-reported physical activity, mental health-related quality of life, and decreasing secondary traumatic stress. Given that the YBSM intervention included stress management psychoeducation as well as yogic techniques and practices, differential effects between the two groups suggest that the effects of yoga practice may be particularly salient in fostering the latter improvements. For example, yoga may act as a gateway to other exercise, helping individuals find a sense of comfort and ease in their physical body that may attenuate exercise avoidance, increase awareness of endogenous needs for movement, and foster enhanced engagement in physical movement. These findings also align with prior evidence linking yoga practice to improved mental health (e.g., Uebelacker, Epstein-Lubow, Gaudiano, & Tremont et al., 2010), including PTSD symptoms (Dick, Niles, Street, & DiMartino et al., 2014); such findings suggest the embodied nature of the practice may exert additive mechanisms of action beyond those deployed in CBSM.
Finally, no changes in either group were observed for sleep quality, alcohol (total amount consumed), BMI, anxiety, tobacco use, and physical health-related quality of life. The lack of change in these variables is difficult to explain, particularly given prior work documenting consistent improvements in these factors following stress management interventions (e.g., Lee et al., 2007). While some studies have suggested that yoga may facilitate weight loss (Rioux, 2013), the brief amount of time spent in yoga during this 8 week YBSM intervention may have blunted our ability to detect change in BMI. Change in BMI has not, to our knowledge, been assessed following CBSM previously. The lack of findings here suggests that alterations in BMI do not occur following these stress management interventions, although future research should examine outcomes over a longer time period. The null findings for tobacco intake were likely attributable to the low base-rate of smoking, with only two smokers in the sample. Change would thus have been difficult to detect.
Study 2 has a number of strengths and limitations. This is the first published study to examine the comparative effectiveness of YBSM and a strong CBSM program on physical, mental, and behavioral health outcomes. However, important considerations follow. Yoga itself is a health behavior, and for sustained benefits, continued practice may be necessary. CBSM, conversely, teaches a set of skills that, once retained, are at least theoretically, permanent, without continued instruction. Finally, a meta-analysis of occupational stress management interventions found cognitive-behavioral interventions to consistently produce larger effects than interventions characterized as relaxation, organizational, multimodal, or alternative in nature (Richardson & Rothstein, 2008). Given that CBSM improved only coping skills above and beyond YBSM in this study, continued investigation of their differential effectiveness seems important.
Given the high stress environments that frontline mental health care providers face, the improvements noted in compassion satisfaction and both components of compassion fatigue—burnout and secondary traumatization—are particularly noteworthy. Maintaining and bolstering frontline providers’ welfare is critical, given the influence of their well-being on the patients they care for. The present results suggest that a brief intervention provided in the workplace can substantially improve their functioning. Such results are promising and suggest that mental health treatment facilities should consider implementing and evaluating stress management programs such as YBSM as part of their efforts to promote good patient care as well as to promote employee wellness.
General Discussion
The observed results suggest that both YBSM and CBSM are beneficial in promoting myriad aspects of health and well-being among frontline mental health providers, that both are feasible interventions for inclusion in workplace wellness interventions, that the YBSM intervention proved efficacious compared to the well-studied and well-supported CBSM intervention, and that each had important and somewhat different effects.
The YBSM intervention was rated as enjoyable and useful. Previous studies have pointed to high attendance and retention rates in the CBSM study as speaking to the “extremely high satisfaction rates” (Lechner et al., 2012). While we did not assess for perceived satisfaction ratings in Study 2, we did compare number of sessions attended. While YBSM participants attended on average slightly more sessions, compared to CBSM participants, the difference was not statistically significantly different. With the growing popularity of yoga (Castaneda, 2014), and the decreasing popularity of more traditional in-person stress management interventions in the workplace (e.g., Eisen et al., 2008), it may be that more mental healthcare workers would be likely to attend a yoga class than a stress management class. It will be important to determine the likelihood of an offered stress management class (YBSM, CBSM, or other) in drawing participants within the workplace in a future study.
These studies also demonstrate preliminary efficacy for the YBSM intervention as a novel and useful intervention that produces similarly beneficial effects as the well-supported CBSM intervention, while providing some benefits above and beyond CBSM, including increased physical activity, increased health-related quality of life, and decreased secondary traumatic stress. CBSM does seem to provide an added benefit in terms of coping skills. If improved coping skills are a target of the intervention, perhaps the YBSM protocol could be slightly modified to include more discussion of coping skills, an idea awaiting future research.
As mentioned previously, it is important to interpret the generalizability of these preliminary findings with caution, as the sample size was small, limiting statistical power to detect change, and as the participant pool was limited to two hospital systems in one geographic area. Therefore, inferences around outcomes should be made with the utmost caution. More research with larger sample sizes is needed for confirmation and replicability of these findings.
However, both interventions, including the new YBSM intervention, seem to suggest efficacy with regards to mental healthcare professionals, a non-clinical yet stress-prone population. These interventions may be useful for other similar populations such as other healthcare providers and first responders.
References
- Acker GM (2011). Burnout among mental health care providers. Journal of Social Work, 12, 475–490. doi: 10.1177/1468017310392418 [DOI] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, & Silber JH (2002). Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association, 288, 1987–1993. doi: 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- Alexander G, Innes KE, Bourguignon C, Bovbjerg VE, Kulbok P, & Taylor AG (2012). Patterns of yoga practice and physical activity following a yoga intervention for adults with or at risk for type 2 diabetes. Journal of Physical Activity & Health, 9, 53–61. Retrieved from http://journals.humankinetics.com/jpah [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni MH, Lechner SC, Kazi A, Wimberly SR, Sifre T, Urcuyo KR, … Carver CS (2006). How stress management improves quality of life after treatment for breast cancer. Journal of Consulting and Clinical Psychology, 74, 1143–1152. doi: 10.1037/0022-006X.74.6.1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS (2006). Measure of current status. http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html
- Braun TD, Park CL, & Conboy LA (2012). Psychological well-being, health behaviors, and weight loss among participants in a residential, Kripalu yoga-based weight loss program. International Journal of Yoga Therapy, 22, 9–22. doi: 10.17761/ijyt.22.1.y47k2658674t1212 [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. (2001). [Table R67] Number and percent distribution of nonfatal occupational injuries and illnesses involving days away from work by nature of injury or illness and number of days away from work, 2001.
- Burnham KP, & Anderson DR (2002). Model selection and multimodel inference: A practical information-theoretic approach. Springer Science & Business Media: New York. [Google Scholar]
- Canadian Society for Exercise Physiology, 2002. PAR-Q [Google Scholar]
- Castenada C (2014). American the yogiful: Insights into American yoga culture today. Master of Liberal Arts Thesis: Rollins. [Google Scholar]
- Chae CU, Lee RT, Rifai N, & Ridker PM (2001). Blood pressure and inflammation in apparently healthy men. Hypertension, 38, 399–403. [DOI] [PubMed] [Google Scholar]
- Chen H, Chen Y, Lu Y, Cao Q, Chen X, Zheng T, & Ye M (2014). Sleep problem and its association with job stress among female nurses from emergency departments of general hospitals. Chinese Mental Health Journal, 28, 253–257. doi: 10.1037/t03609 [DOI] [Google Scholar]
- Cheema BS, Houridis A, Busch L, Raschke-Cheema V, Melville GW, Marshall PW, … & Colagiuri B (2013). Effect of an office worksite-based yoga program on heart rate variability: outcomes of a randomized controlled trial. BMC Complementary and Alternative Medicine, 13, 82. doi: 10.1186/1472-6882-13-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PD (1995). Burnout and collegial support in state psychiatric hospital staff. Journal Of Clinical Psychology, 51(5), 703–710. doi: 10.1002/1097 [DOI] [PubMed] [Google Scholar]
- Dick AM, Niles BL, Street AE, DiMartino DM, & Mitchell KS (2014). Examining mechanisms of change in a yoga intervention for women: the influence of mindfulness, psychological flexibility, and emotion regulation on PTSD symptoms. Journal of Clinical Psychology, 70, 1170–1182. Doi: 10.1002/jclp.22104 [DOI] [PubMed] [Google Scholar]
- Duraisingam V, Pidd K, & Roche AM (2009). The impact of work stress and job satisfaction on turnover intentions: A study of Australian specialist alcohol and other drug workers. Drugs: Education, Prevention & Policy, 16, 217–231. doi: 10.1080/09687630902876171 [DOI] [Google Scholar]
- Eisen KP, Allen GJ, Bollash M, & Pescatello LS (2008). Stress management in the workplace: A comparison of a computer-based and an in-person stress-management intervention. Computers in Human Behavior, 24, 486–496. doi: 10.1016/j.chb.2007.02.003 [DOI] [Google Scholar]
- Figley CR (2002). Compassion fatigue: Psychotherapists’ chronic lack of self care. Journal of Clinical Psychology, 58, 1433–1441. doi: 10.1002/jclp.10090 [DOI] [PubMed] [Google Scholar]
- Field T (2011). Yoga clinical research review. Complementary Therapies in Clinical Practice, 17, 1–8. doi: 10.1016/j.ctcp.2010.09.007 [DOI] [PubMed] [Google Scholar]
- Gaab JI, Sonderegger L, Scherrer S, & Ehlert U (2006). Psychoneuroendocrine effects of cognitive-behavioral stress management in a naturalistic setting—a randomized controlled trial. Psychoneuroendocrinology, 31, 428–438. doi: 10.1016/j.psyneuen.2005.10.005 [DOI] [PubMed] [Google Scholar]
- Gaither CA, Kahaleh AA, Doucette WR, Mott DA, Pederson CA, & Schommer JC (2008). A modified model of pharmacists’ job stress: The role of organizational, extra-role, and individual factors on work-related outcomes. Research in Social & Administrative Pharmacy, 4, 231–243. doi: 10.1016/j.sapharm.2008.04.001 [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Anderson DR, Whitmer RW, Ozminkowski RJ, Dunn RL, Wasserman J, & The Health Enhancement Research Organization (HERO) Research Committee. (1998). The relationship between modifiable health risks and health care expenditures: An analysis of the multi-employer HERO health risk and cost database. Journal of Occupational and Environmental Medicine, 40, 843–854. [DOI] [PubMed] [Google Scholar]
- Gökçen C, Zengin S, Oktay MM, Alpak G, Al B, & Yıldırım C (2013). Burnout, job satisfaction and depression in the healthcare personnel who work in the emergency department. Anatolian Journal of Psychiatry, 14, 122–128. doi: 10.5455/apd,36379. [DOI] [Google Scholar]
- Grozdev I, Kast D, Cao L, Carlson D, Pujari P, Schmotzer B, … Korman NJ (2012). Physical and Mental Impact of Psoriasis Severity as Measured by the Compact Short Form-12 Health Survey (SF-12) Quality of Life Tool, Journal of Investigative Dermatology, 132, 1111–1116. doi: 10.1038/jid.2011.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granath J, Ingvarsson S, von Thiele U, & Lundberg U (2006). Stress management: a randomized study of cognitive behavioural therapy and yoga. Cognitive Behaviour Therapy, 35, 3–10. doi: 10.1080/16506070500401292 [DOI] [PubMed] [Google Scholar]
- Harris JK, French SA, Jeffery RW, McGovern PG, & Wing RR (1994). Dietary and physical activity correlates of long-term weight loss. Obesity Research, 2, 307–313. doi: 10.1002/j.1550-8528.1994.tb00069. [DOI] [PubMed] [Google Scholar]
- Hartfiel N, Burton C, Rycroft-Malone J, Clarke G, Havenhand J, Khalsa SB, & Edwards RT (2012). Yoga for reducing perceived stress and back pain at work. Occupational Medicine, 62, 606–612. doi: 10.1093/occmed/kqs168 [DOI] [PubMed] [Google Scholar]
- Horan AP (2002). An effective workplace stress management intervention: Chicken soup for the soul at work(TM) employee groups. Work: Journal of Prevention, Assessment & Rehabilitation, 18, 3–13. Retrieved from http://www.iospress.nl/journal/work/ [PubMed] [Google Scholar]
- Jacobsen JM (2008). Compassion fatigue, compassion satisfaction, and burnout. Journal of Workplace Behavioral Health, 21, 133–152. [Google Scholar]
- Janssen PM, deJonge J, & Bakker AB (1999). Specific determinants of intrinsic work motivation, burnout and turnover intentions: A study among nurses. Journal of Advanced Nursing, 29, 1360–1369. doi: 10.1046/j.1365-2648.1999.01022. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Wood MD, & Wood PK (1994). Anxiety and drinking behavior: Moderating effects of tension-reduction alcohol outcome expectancies. Alcoholism: Clinical and Experimental Research, 18, 852–860. doi: 10.1111/j.1530-0277.1994.tb00050. [DOI] [PubMed] [Google Scholar]
- Lapp J, & Attridge M (2000). Worksite interventions reduce stress among high school teachers and staff. International Journal of Stress Management, 7, 229–232. doi: 10.1023/A:1009570316599 [DOI] [Google Scholar]
- Laschinger HKS, Leiter M, Day A, & Glin D (2009). Workplace empowerment, incivility, and burnout: Impact on staff nurse recruitment and retention outcomes. Journal of Nursing Management, 17, 302–311. doi: 10.1111/j.1365-2834.2009.00999 [DOI] [PubMed] [Google Scholar]
- Laschinger HKS, Shamian J, & Thomson D (2001). Impact of magnet hospital characteristics on nurses’ perceptions of trust, burnout, quality of care, and work satisfaction. Nursing Economics, 19, 209–219. Retrieved from http://www.nursingeconomics.net/cgi-bin/WebObjects/NECJournal.woa [Google Scholar]
- Lasalvia A, Bonetto C, Bertani M, Bissoli S, Cristfalo D, Marella G, & Ruggeri M (2009). Influence of perceived organizational factors on job burnout: Survey of community mental health staff. British Journal of Psychiatry, 195, 537–544. doi: 10.1192/bjp.bp.108.060871 [DOI] [PubMed] [Google Scholar]
- Lechner SC, Ennis-Whitehead N, Robertson BR, Annane DW, Vargas S, Carver CS, & Antoni MH (2009). Adaptation of a psycho-oncology intervention for black breast cancer survivors. TCP The Counseling Psychologist, 41, 286–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SH, Ahn SC, Lee YJ, Choi TK, Yook KH, & Suh SY (2007). Effectiveness of a meditation-based stress management program as an adjunct to pharmacotherapy in patients with anxiety disorder. Journal of Psychosomatic Research, 62, 189–195. doi: 10.1016/j.jpsychores.2006.09.009 [DOI] [PubMed] [Google Scholar]
- Lee H, Lim Y, Jung HY, & Shin Y (2012). Turnover intention of graduate nurses in South Korea. Japan Journal of Nursing Science, 9, 63–75. doi: 10.1111/j.1742-7924.2011.00187. [DOI] [PubMed] [Google Scholar]
- Leiter MP, & Harvie PL (1996). Burnout among mental health workers: A review and a research agenda. International Journal of Social Psychiatry, 42, 90–101. doi: 10.1177/002076409604200203 [DOI] [PubMed] [Google Scholar]
- Leiter MP, & Maslach C (1988). The impact of interpersonal environment on burnout and organizational commitment. Journal of Organizational Behavior, 9, 297–308. doi: 10.1002/job.4030090402 [DOI] [Google Scholar]
- Leiter MP, & Maslach C (2004). Areas of work life: A structured approach to organizational predictors of job burnout In Perrewé P & Ganster CD (Eds.), Research in occupational stress and well-being: Vol. 3, Emotional and physiological processes and positive intervention strategies (pp. 91–134). Oxford, England: JAI Press/Elsevier. [Google Scholar]
- Martin RC, & Dahlen ER (2005). Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences, 39, 1249–1260. doi: 10.1016/j.paid.2005.06.004 [DOI] [Google Scholar]
- McCraty R, Atkinson M, & Tomasino D (2003). Impact of a workplace stress reduction program on blood pressure and emotional health in hypertensive employees. The Journal of Alternative and Complementary Medicine, 9, 355–369. doi: 10.1089/107555303765551589. [DOI] [PubMed] [Google Scholar]
- Paffenbarger R, Wing A, & Hyde R (1978). Paffenbarger Physical Activity Questionnaire. American Journal of Epidemiology, 108, 161–175. [DOI] [PubMed] [Google Scholar]
- Paris M, & Hoge MA (2010). Burnout in the mental health workforce: A review. Journal of Behavioral Health Services & Research, 37, 519–528. doi: 10.1007/s11414-009-9202-2 [DOI] [PubMed] [Google Scholar]
- Park CL, Armeli S, & Tennen H (2004). The daily stress and coping process and alcohol use among college students. Journal of Studies on Alcohol and Drugs, 65, 126–135. doi: 10.15288/jsa.2004.65.126 [DOI] [PubMed] [Google Scholar]
- Park CL, & Iacocca MO (2014). A stress and coping perspective on health behaviors: Theoretical and methodological considerations. Anxiety, Stress & Coping, 27, 123–137. doi: 10.1080/10615806.2013.860969 [DOI] [PubMed] [Google Scholar]
- Park CL, & Levenson MR (2002). Drinking to cope among college students: Prevalence, problems and coping processes. Journal of Studies on Alcohol and Drugs, 63, 486–497. doi: 10.15288/jsa.2002.63.486 [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Molton I, Dahn JR, Shen BJ, Kinsinger D, Traeger, … Antoni M (2006). A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine, 31, 261–270. doi: 10.1207/s15324796abm31038 [DOI] [PubMed] [Google Scholar]
- Pereira MA, FitzerGerald SJ, & Gregg EW (1997). A collection of physical activity questionnaires for health-related research. Kriska and Caspersen, Eds. Medicine & Science in Sports & Exercise, 29, S1–205. [PubMed] [Google Scholar]
- Perez GK, Haime V, Jackson V, Chittenden E, Mehta DH, & Park ER (2015). Promoting resiliency among palliative care clinicians: Stressors, coping strategies, and training needs. Journal of Palliative Medicine, 18, 332–337. doi: 10.1089/jpm.2014.0221 [DOI] [PubMed] [Google Scholar]
- Rathore JS, Jehi LE, Fan Y, Patel SI, Foldvary-Schaefer N, Ramirez MJ, … Tesar GE (2014). Validation of the Patient Health Questionnaire-9 (PHQ-9) for depression screening in adults with epilepsy. Epilepsy & Behavior, 37, 215–220. doi: 10.1016/j.yebeh.2014.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray SL, Wong C, White D, & Heaslip K (2013). Compassion satisfaction, compassion fatigue, work life conditions, and burnout among frontline mental health care professionals. Traumatology, 19, 255–267. doi: 10.1177/1534765612471144 [DOI] [Google Scholar]
- Richardson KM, & Rothstein HR (2008). Effects of occupational stress management intervention programs: A meta-analysis. Journal of Occupational Health Psychology, 13, 69–72. doi: 10.1037/1076-8998.13.1.69 [DOI] [PubMed] [Google Scholar]
- Rioux J, & Ritenbaugh C (2013). Narrative review of yoga intervention clinical trials including weight-related outcomes. Alternative Therapies in Health and Medicine, 19, 46–60. Retrieved from http://www.alternative-therapies.com/openaccess/ATHM_19-3_Rioux.pdf [PubMed] [Google Scholar]
- Rössler W (2012). Stress, burnout, and job dissatisfaction in mental health workers. European Archives of Psychiatry and Clinical Neuroscience, 262, 65–69. doi: 10.1007/s00406-012-0353-4 [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Brown KW, & Astin J (2011). Toward the integration of meditation into higher education: A review of research evidence. Teachers College Record, 113, 493–528. Retrieved from http://www.tcrecord.org/ [Google Scholar]
- Sidle SD (2008). Workplace stress management interventions: What works best?. The Academy of Management Perspectives, 22, 111–112. doi: 10.5465/AMP.2008.34587999 [DOI] [Google Scholar]
- Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, … Ludman EJ (2013). Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatric Services, 64, 1195–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamm BH (2009). Professional Quality of Life: Compassion Satisfaction and Fatigue Version 5 (ProQOL). www.isu.edu/~bhstammorproqol.org.
- Thompson FE, Subar AF, Smith AF, Midthune D, Radimer KL, Kahle LL, & Kipnis V (2002). Fruit and vegetable assessment: Performance of 2 new short instruments and a food frequency questionnaire. Journal of the American Dietetic Association, 102, 1764–1772. doi: 10.1016/S0002-8223(02)90379-2 [DOI] [PubMed] [Google Scholar]
- Thorsteinsson EB, Brown RF, & Richards C (2014). The relationship between work-stress, psychological stress and staff health and work outcomes in office workers. Psychology, 5, 1301–1311. doi: 10.4236/psych.2014.510141 [DOI] [Google Scholar]
- Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, & Miller IW (2010). Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. Journal of Psychiatric Practice, 16, 22–33. doi: 10.1097/01.pra.0000367775.88388.96 [DOI] [PubMed] [Google Scholar]
- Van der Klink JJ, Blonk RW, Schene AH, & Van Dijk FJ (2001). The benefits of interventions for work-related stress. American Journal of Public Health, 91, 270–276. Doi: 10.2105/AJPH.91.2.270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, & Keller SD (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220–233. [DOI] [PubMed] [Google Scholar]
- Weaver JD (1984). Work-related stressors and means of coping among crisis intervention workers and their spouses. Emotional First Aid: A Journal of Crisis Intervention, 1, 14–24. [Google Scholar]
- Winterdyk J, Ray H, Lafave L, Flessati S, Huston M, Danelesko E, & Murray C (2008). The evaluation of four mind/body intervention strategies to reduce perceived stress among college students. College Quarterly, 11, 1–10. Retrieved from https://collegequarterly.ca/ [Google Scholar]
- Wolever RQ, Bobinet KJ, McCabe K, Mackenzie ER, Fekete E, Kusnick CA, & Baime M (2012). Effective and viable mind-body stress reduction in the workplace: A randomized controlled trial. Journal of Occupational Health Psychology, 17, 246–258. doi: 10.1037/a0027278 [DOI] [PubMed] [Google Scholar]
- Yang K, & James KA (2014). Yoga, as a transitional platform to more active lifestyle: A 6- month pilot study in the USA. Health Promotion International, 1–7. doi: 10.1093/heapro/dau108 [DOI] [PubMed] [Google Scholar]


