Abstract
Objective
The pathophysiology of idiopathic sudden sensorineural hearing loss (SSNHL) is poorly understood. This study aimed to explore the association of migraine and risk of SSNHL in a meta‐analysis of population‐based cohort studies.
Methods
A systematic literature search of studies published until December 2019 was carried out in Medline, Embase, Scopus, Web of Science, and Google Scholar using appropriate keywords. References of the retrieved articles were also examined for inclusion. Random‐effects meta‐analysis was performed by calculating pooled hazard ratio (HR) and associated 95% confidence interval (CI) using the DerSimonian and Laird method while considering conceptual heterogeneity.
Results
Three eligible cohort studies, with 282 250 participants, were included. In total, 56 450 had migraine, and 225 800 had no migraine. Of those with migraine, 0.88% had SSNHL, and among those without migraine, 0.59% had SSNHL. Pooled HR for the risk of SSNHL was 1.84 (95% CI: 1.11‐2.57; P < .001). In cohort studies on females, migraine was not significantly the risk of SSHL than no migraine. However, in male cohort studies, the migraine had a higher risk of SSHL than no migraine (HR = 1.50; 95% CI: 1.17‐1.83; P < .001). The pooled HR of migraine with the risk of SSNHL was 1.37 (95% CI: 1.16‐1.58, P < .001) in people with <40 years old and 1.39 (95% CI: 1.17‐1.60; P < .001) in people >40 years old.
Conclusions
Individuals with migraine patients are at a higher risk of developing SSHL. Different age and sex migraine subgroups showed a higher proportion of SSNHL cases compared to nonmigraineurs.
Keywords: migraine, risk, sudden sensorineural hearing loss
This study explored the association of migraine and risk of ISSNHL in a meta‐analysis of population‐based cohort studies.
1. INTRODUCTION
Idiopathic sudden sensorineural hearing loss (ISSNHL) or sudden sensorineural hearing loss (SSNHL) is an otolaryngology emergency defined by sensorineural hearing loss of unknown etiology and ≥30 dB over at least three consecutive audiometric frequencies within 72 hours period. 1 Symptoms of the disease include unilateral or bilateral hearing loss, tinnitus, dizziness, and balance problems. 2 , 3 The global incidence rate of SSNHL is reported to be 5 to 30 cases per 100 000 people per year 4 , 5 and is still rising. 6 , 7 , 8
Since the cause of SSNHL remains unknown, there has been no definitive or satisfactory treatment. 9 Therefore, it is essential to know the causes of sudden deafness to treat it. The exact cause of sudden deafness has not yet been determined; But It has been proposed that a higher incidence of migraine in patients with ISSNHL may indicate a link between the two conditions. 10 Migraine is an episodic primary headache disorder that affects 14% to 16% of the world's population. In Western countries, the overall prevalence of migraine is 6% to 8% in men and 15% to 25% in women.
Migraine aura can manifest as disturbances in visual, somatosensory, olfactory, and rarely auditory senses, which can have a vascular basis. In this condition, low‐frequency hearing loss often occurs episodically but may also present as persistent unilateral HL or SSNHL. However, the presentation of migraine aura without headache makes the association of migraine with ISNHL questionable. 11 , 12 Given the relative lack of empirical research on the association of migraine with the risk of SSNHL, we performed a meta‐analysis of human studies on migraine and SSNHL to determine the overall effect size between the two conditions and to assess the degree of variability in effect sizes across studies. It is hoped that these results will provide new insights into the association between migraine and SSNHL, which in turn could be beneficial for finding an effective treatment strategy.
2. METHODS
2.1. Search strategy
A systematic review of studies on migraine and SSNHL was conducted according to PRISMA guidelines for the systematic review of observational studies. Searching for the literature published until December 24, 2019 was carried out using various databases including Medline (via PubMed), Web of Science, Embase, Scopus, Ovid, and ProQuest (Box S1). Books and grey literature, including policy documents, reports, and conference papers were searched using grey literature databases, library databases, and general online searches (eg, websites of university libraries; government organizations and Google). The screening was done by reviewing titles, abstracts, and full‐text of the articles. To ensure comprehensive retrieval of the literature, independent supplemental manual searches were performed on the reference lists of the relevant articles and other databases, including CINAHL, PsycINFO, Cochrane, and Google Scholar. The content of the abstracts or the full‐text articles were reviewed independently by two reviewers (A. R. and M. M.) to determine whether they met the inclusion criteria, including: (a) studies that included SSNHL and (b) migraine. The searches were not limited by publication date, country, or language. Publications were excluded if they did not provide useable data for hazard ratio (HR) estimation.
Two investigators (A. R. and M. M.) independently assessed the identified records for eligibility. Discrepancies were resolved by consensus or determined by the third investigator (M. H. T.).
2.2. ETHICS STATEMENT
The study protocol was approved by the institutional review board of the Golestan University of Medical Sciences, Iran.
2.3. Data extraction and quality assessment
Two investigators (A. R. and M. M.) independently extracted the original data. Any disagreement was resolved by discussion. If a consensus was not reached, the results were reviewed by a third investigator (M. H. T). The extracted data consisted of the following items: the first author's name, publication year, study population (datasets), study design, age (years), sex, migraine assessment method, number of migraine cases, number of sudden sensor neural hearing loss cases, number of migraine with SSNHL cases, methods of diagnosing of migraine, methods of diagnosing of SSNHL, average follow‐up period (year), sample size and adjustment for confounding factors.
Two independent investigators (A. R. and M. M.) assessed the quality of the included studies using the nine‐point Newcastle‐Ottawa scale (NOS), 13 which has eight items divided into three domains (selection, comparability, and outcome). The NOS score ranges from 0 to 9 and is defined as the sum of the scores of the above‐mentioned domains. A score of ≥7 was categorized as good quality (Table S1). Discrepancies were resolved by discussion or through consultation with the third investigator (M. H. T.). The study selection procedure is summarized in Figure 1.
FIGURE 1.
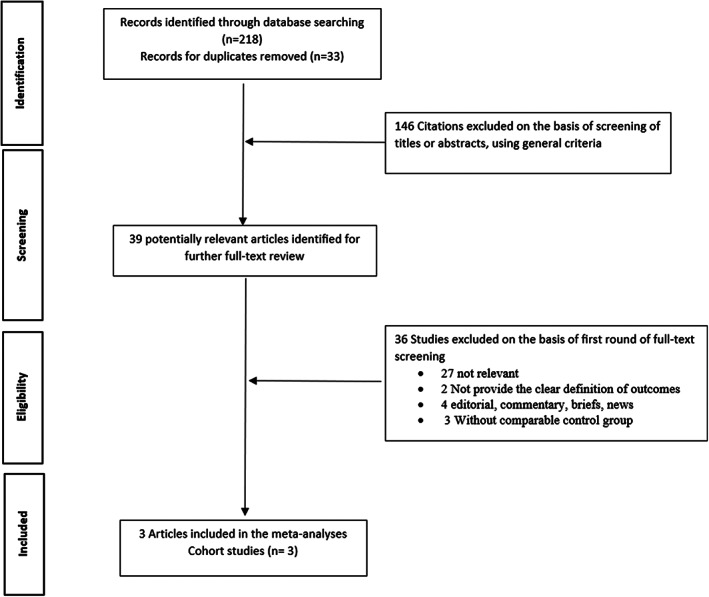
Flowchart of study selection procedure and exclusion criteria
2.4. Statistical analysis
A meta‐analysis was conducted to estimate the risk of SSNHL based on pooled hazard ratio (HR) and 95% confidence interval (CI). Heterogeneity among studies was assessed by the I 2 statistic, and a P‐value of <.10 or an I 2 value of >50% indicated significant heterogeneity. 14 Random‐effects meta‐analysis was used to account for the heterogeneity of study results, and a forest plot was used to assess the crude and adjusted HR and corresponding 95% CIs for visual inspection across studies. Moreover, the effect size, stratified on the same sex and age group, was re‐estimated to produce separate estimations. Random‐effects meta‐analysis was used because of the sense of conceptual heterogeneity with assuming that the biological effects of migraine may vary randomly, at least in various populations. Pooled HRs were calculated using the DerSimonian and Laird random‐effects method. Statistical heterogeneity among studies was assessed using the Cochran's Q test and quantified by I 2 statistic. 15
Statistical analyses were performed using Stata 16 (Stata Corp, College Station, Texas). The admetan, metabias and metafunnel macro commands were used for meta‐analytic procedures. A P‐value of less than .05 was considered statistically significant.
3. RESULTS
We retrieved a total of 218 studies in the literature search. After removing duplicates, 143 unique citations were identified from the Medline, Embase, Scopus, CINAHL, ProQuest, PsycINFO, Cochrane, Web of Science, and Google Scholar databases. After screening and detailed examination, three eligible articles, with 282 250 participants, were included in the meta‐analysis (Figure 1). Publication characteristics, including study population (number, sex, age, and country), year of publication, type of study, No. migraine, No. SSNHL, follow‐up time, and adjusted variables are summarized in Table 1. Also, the quality of the articles included in this study was evaluated on the Newcastle‐Ottawa scale, which showed that all studies sum of the scores of the domains for NOS were more than 7 and good quality (Table S1).
TABLE 1.
The main characteristics of included cohort analysis on the association between migraine and risk of sudden sensorineural hearing loss
| Author, year | Country | Study design | No. migraine | No. sudden sensorineural hearing loss | No. migraine with SSNHL | Diagnose of migraine | Diagnose of SSNHL | Average follow‐up period (year) | Sex and age (year) | Study population and no. of participants | Method of migraine assessment | Results HR (95% CI) | Adjusted variables |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chu.et al, 2012 10 | Taiwan | Cohort study | 10 280 | 134 | 43 | ICD‐9‐CM | ICD‐9‐CM code 388.2 | 10 |
M/F 38.5 (20‐64) No. male: 14 715 No. female: 36 685 |
Taiwan National Health Insurance Research Database (NHIRD) and N = 51 400 | ICD‐9‐CM | 1.80 (1.22‐2.61) | Age and sex |
| Hwang et al, 2018 26 | Taiwan | Cohort study | 1056 | 136 | 55 | Outpatient claims | ICD‐9 | 6.39 |
M/F 36.7 (15.3) No. male: 2049 No. female: 3231 |
Taiwan Longitudinal Health Insurance Database, and N = 5280 | Outpatient claims | 2.71 (1.86‐3.93) | Age per year, sex, comorbidity, use of oral contraceptives, geographic region, urbanization level, and enrollee category |
| Kim et al, 2019 16 | South Korea | Cohort study | 45 114 | 1568 | 399 | ICD‐10: G43 |
ICD‐10 (H912) |
10 |
M/F 0‐85 No. male: No. female: |
The Korean National Health Insurance Service‐National Sample and N = 225 570 | ICD‐10 | 1.34 (1.19‐1.50) | Age, sex, income, the region of residence, hypertension, diabetes, and dyslipidemia, ischemic heart disease, cerebral stroke, depression, Meniere's disease, and tinnitus histories. |
3.1. Association between migraine and the risk of SSNHL
The participants included 56 450 migraineurs and 225 800 nonmigraineurs. Of those with migraine, 0.88% had SSNHL, and among those without migraine, 0.59% had SSNHL. Overall, pooled crude HR and adjusted HR for risk of SSNHL were 1.87 (95% CI: 1.21‐2.9, P < .001) and 1.84 (95% CI: 1.11‐2.57; P < .001), respectively (Figures 2 and 3).
FIGURE 2.
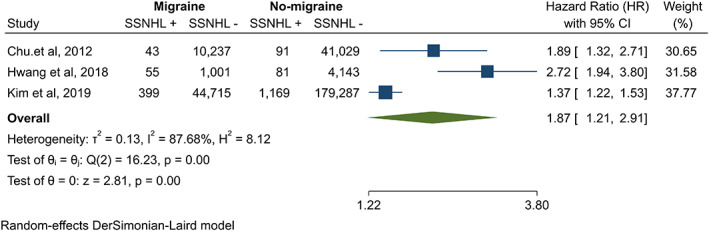
The association between migraine and risk of sudden sensorineural hearing loss in crude HR
FIGURE 3.
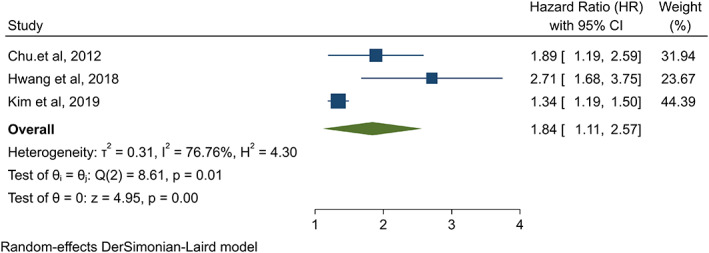
The association between migraine and the risk of sudden sensorineural hearing loss in adjusted HR
We performed a meta‐analysis to evaluate the associations between migraine and risk of SSNHL in gender‐specific cohort studies. The association between migraine and risk of SSNHL is shown in Figure 4. In female cohort studies, migraine was not significantly the risk of SSNHL than no migraine (HR = 1.52; 95% CI: 0.93‐2.11, P = .054). In male cohort studies, the migraine had a higher risk of SSNHL than no migraine (HR = 1.50; 95% CI: 1.17‐1.83; P < .001) (Figure 4). For study of Hwang et al, data based on sex were not available so for subgroup analysis excluded.
FIGURE 4.
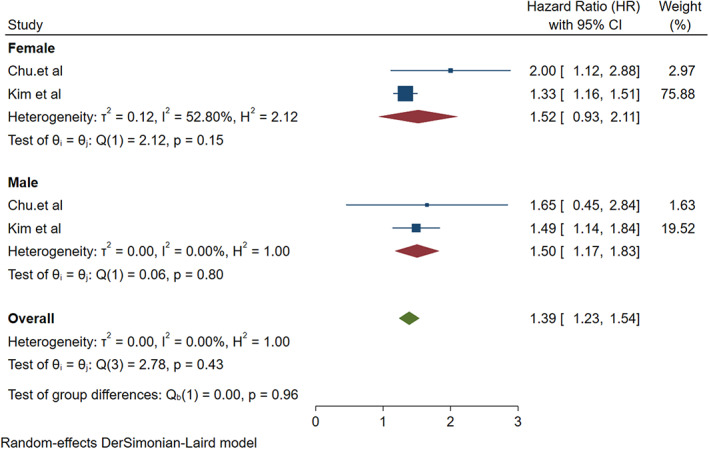
The association between migraine and risk of sudden sensorineural hearing loss in gender‐specific cohort studies
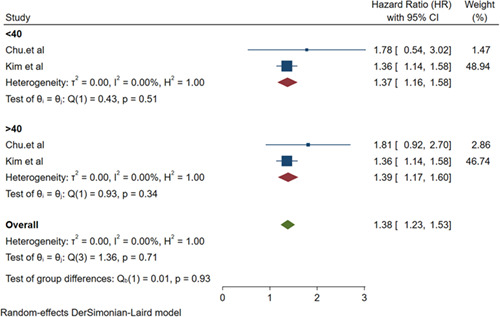
The pooled HR for the association of migraine with the risk of SSNHL was 1.37 (95% CI: 1.16‐1.58; P < .001) in people with <40 years old and 1.39 (95% CI: 1.17‐1.60; P < .001) in people >40 years old (Figure 5). For the study of Hwang et al, the number of migraine and SSNHL by age group were not available for subgroup analysis age group was excluded.
FIGURE 5.
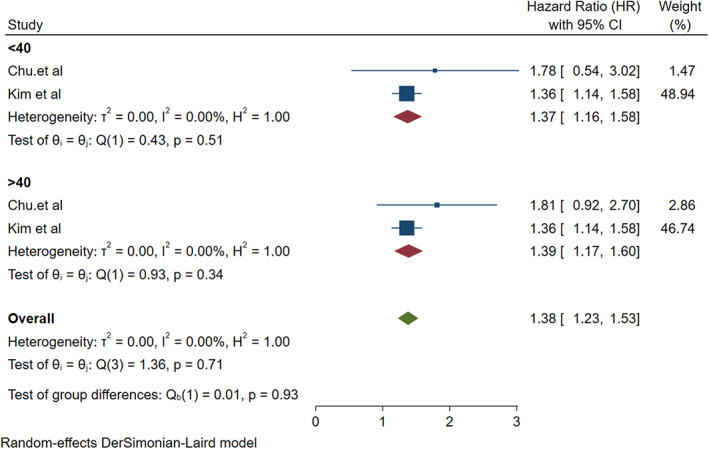
The association between migraine and risk of sudden sensorineural hearing loss by age group
4. DISCUSSION
The present systematic review and meta‐analysis were conducted on three observational studies, involving 282 250 participants, to assess the risk of ISSNHL in patients with migraine. The findings indicated that migraine is associated with a 1.8‐fold increased risk of developing SSNHL. Additionally, this association was present in other subgroups, including the sex and age group of studies. Most primary studies found the association between migraine and ISSNHL. 10 , 16 The results of the present study are consistent with high quality, large cohort studies that reported similar HRs.
Low‐frequency hearing loss (HL) is typically episodic, but permanent unilateral HL and SSNHL have also been reported in migraine cases. Several studies have attempted to find factors involved in the etiology and pathogenesis of ISSNHL. 17 In cases of aura without acute headache in migraineurs, the relationship of SSNHL to migraine is questionable. A few studies have attributed sudden auditory symptoms to migraine, 18 but vasospasms are very commonly associated with migraine and may be the cause of symptoms such as monocular visual loss, paresthesias, and vertigo. Although it is difficult to prove a cause‐effect relationship between migraine and SSNHL, 19 common etiopathological factors that induce vasospasms in the labyrinthine arteries might explain these inner ear symptoms. 18 A study have indicated that some patients with SSNHL exhibit symptoms that can be attributable to migraine and that sudden HL associated with severe migraine headache is linked to ischemic changes in the inner ear. 20 Chu et al reported a 1.8‐fold increase in the risk of SSNHL for patients with migraine, with a very small but detectable increase in the cumulative risk of SSNHL each year during 10 years of observation. Ballesteros et al 21 proposed that idiopathic SSNHL has a vascular etiology because the blood supply to the cochlea arises from two small terminal arteries. Due to the small diameter of the vessels within the arterial supply and the lack of collateral blood supply, the cochlea is susceptible to injury through a variety of vascular issues. Migraine can lead to permanent auditory and vestibular deficits, and the pathophysiology of auditory symptoms may be related to vasospasms in small arterioles within the cochlea and labyrinth, similar to the involvement of only a subset of retinal arterioles in retinal migraine. 22
In a study by Arslan et al, the prevalence of migraine was higher in patients with ISSNHL, although the rate of improvement was slightly higher in those with migraine. The higher prevalence of migraine in people with ISSNHL may be due to the vascular etiopathogenesis shared between the two conditions, such as vasospasm. 22 A migraine aura can manifest as disturbances in visual, somatosensory, olfactory, and rarely auditory senses, which can have a vascular basis. 22 Low‐frequency hearing loss often occurs episodically but may also present as persistent unilateral hearing loss or SSNHL. 11 , 12
The exact mechanism linking migraine and SSNHL is unknown. In 1987, Lipkin et al first described a 62‐year‐old woman who had recurrent hearing loss in conjunction with migraine attacks. 23 Viirre and Baloh later presented 13 cases of individuals with unexplained SSNHL who met the diagnostic criteria for migraine. 19 The only histopathology evidence connecting migraine and SSNHL was provided by Lee et al in 2000. 12 The studies presented a man with longstanding migraine who developed SSNHL at age 50. Postmortem examination of the cochlea showed prominent fibrosis in the stria vascularis and spiral ligament, which are the characteristics of an ischemic insult. Thus, the studies postulated that the deafness might have resulted from migraine‐associated vasospasm. 10 , 24
To date, this is the first meta‐analysis on the association of migraine and risk of SSNHL. Our findings seem to be more stable and valid, as the analysis was based on cohort studies. Also, we performed subgroup analyses to explore the source of heterogeneity and to confirm the stability of HR estimates.
5. LIMITATION
Nevertheless, the low number of relevant studies and limited diversity of study populations (East Asian countries) could be considered as limitations of the present study. However, the prevalence of migraine in SSNHL patients has also been reported in other countries. 25 also, findings from this systematic review must be considered in light of the heterogeneity in participant characteristics, methodological differences, and definition in exposure and outcome. In addition, we only included articles published in English, which may be a potential source of language and publication bias.
6. CONCLUSION
Based on the findings, patients with migraine are at a higher risk of developing ISSNHL. Although ISSNHL is a rare condition, migraine patients with auditory symptoms should be screened for SSNHL. Further studies are needed to clarify the underlying mechanisms through which migraine may increase the risk of SSNHL.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Supporting information
Appendix S1: Supporting Information
ACKNOWLEDGMENTS
This systematic review was approved by Ethics in research of Golestan University of Medical Sciences (IR.GOUMS.REC.1399.113).
Mohammadi M, Taziki Balajelini MH, Rajabi A. Migraine and risk of sudden sensorineural hearing loss: A systematic review and meta‐analysis. Laryngoscope Investigative Otolaryngology. 2020;5:1089–1095. 10.1002/lio2.477
Funding information Golestan University of Medical Sciences, Grant/Award Number: IR.GOUMS.REC.1399.113
BIBLIOGRAPHY
- 1. Cadoni G, Agostino S, Manna R, et al. Clinical associations of serum antiendothelial cell antibodies in patients with sudden sensorineural hearing loss. Laryngoscope. 2003;113(5):797‐801. [DOI] [PubMed] [Google Scholar]
- 2. Fetterman BL, Luxford WM, Saunders JE. Sudden bilateral sensorineural hearing loss. Laryngoscope. 1996;106(11):1347‐1350. [DOI] [PubMed] [Google Scholar]
- 3. Yimtae K, Srirompotong S, Kraitrakul S. Idiopathic sudden sensorineural hearing loss. J Med Assoc Thailand=Chotmaihet thangphaet. 2001;84(1):113‐119. [PubMed] [Google Scholar]
- 4. Schweinfurth JM, Cacace AT, Parnes SM. Clinical applications of otoacoustic emissions in sudden hearing loss. Laryngoscope. 1997;107(11):1457‐1463. [DOI] [PubMed] [Google Scholar]
- 5. Tlumak AI, Kileny PR. Parameters that affect the measurement of otoacoustic emissions. Curr Opin Otolaryngol Head Neck Surg. 2001;9(5):279‐283. [Google Scholar]
- 6. Teranishi M, Katayama N, Uchida Y, Tominaga M, Nakashima T. Thirty‐year trends in sudden deafness from four nationwide epidemiological surveys in Japan. Acta Otolaryngol. 2007;127(12):1259‐1265. [DOI] [PubMed] [Google Scholar]
- 7. Wu C‐S, Lin H‐C, Chao P‐Z. Sudden sensorineural hearing loss: evidence from Taiwan. Audiol Neurotol. 2006;11(3):151‐156. [DOI] [PubMed] [Google Scholar]
- 8. Nosrati‐Zarenoe R, Arlinger S, Hultcrantz E. Idiopathic sudden sensorineural hearing loss: results drawn from the Swedish national database. Acta Otolaryngol. 2007;127(11):1168‐1175. [DOI] [PubMed] [Google Scholar]
- 9. Klingel R, Heibges A, Uygun‐Kiehne S, Fassbender C, Mösges R. Rheopheresis for sudden sensorineural hearing loss. Atheroscler Suppl. 2009;10(5):102‐106. [DOI] [PubMed] [Google Scholar]
- 10. Chu C‐H, Liu C‐J, Fuh J‐L, Shiao A‐S, Chen T‐J, Wang S‐J. Migraine is a risk factor for sudden sensorineural hearing loss: a nationwide population‐based study. Cephalalgia. 2013;33(2):80‐86. [DOI] [PubMed] [Google Scholar]
- 11. Espinosa‐Sanchez JM, Lopez‐Escamez JA. Migraine, Sudden Sensorineural Hearing Loss and Autoimmune Ear Disease. London, England: Sage Publications Sage UK; 2013. [DOI] [PubMed] [Google Scholar]
- 12. Lee H, Lopez I, Ishiyama A, Baloh RW. Can migraine damage the inner ear? Arch Neurol. 2000;57(11):1631‐1634. [DOI] [PubMed] [Google Scholar]
- 13. Peterson J, Welch V, Losos M, Tugwell P. The Newcastle‐Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta‐Analyses. Ottawa Hospital Research Institute: Ottawa; 2011. [Google Scholar]
- 14. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7(3):177‐188. [DOI] [PubMed] [Google Scholar]
- 15. Higgins J, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21(11):1539‐1558. [DOI] [PubMed] [Google Scholar]
- 16. Kim SY, Kim MK, Lim J‐S, Kong IG, Choi HG. Migraine increases the proportion of sudden sensorineural hearing loss: a longitudinal follow‐up study. Auris Nasus Larynx. 2019;46(3):353‐359. [DOI] [PubMed] [Google Scholar]
- 17. Merchant SN, Durand ML, Adams JC. Sudden deafness: is it viral? ORL. 2008;70(1):52‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee H, Whitman GT, Lim JG, et al. Hearing symptoms in migrainous infarction. 2003;60(1):113‐116. [DOI] [PubMed] [Google Scholar]
- 19. Viirre ES, Baloh RWJHTJoH , Pain F. Migraine as a cause of sudden hearing loss. 1996;36(1):24‐28. [DOI] [PubMed] [Google Scholar]
- 20. Cha Y‐H. Migraine a Risk Factor for SSNHL. London, England: Sage Publications Sage UK; 2013. [DOI] [PubMed] [Google Scholar]
- 21. Ballesteros F, Alobid I, Tassies D, et al. Is there an overlap between sudden neurosensorial hearing loss and cardiovascular risk factors? 2009;14(3):139‐145. [DOI] [PubMed] [Google Scholar]
- 22. Piovesan EJ, Kowacs PA, Werneck LC, Siow CJA‐p. Oscillucusis and sudden deafness in a migraine patient. Arq Neuropsiquiatr. 2003;61(3B):848‐850. [DOI] [PubMed] [Google Scholar]
- 23. Lipkin AF, Jenkins HA, Coker NJJAoOH, Surgery N . Migraine and sudden sensorineural hearing loss. 1987;113(3):325‐326. [DOI] [PubMed] [Google Scholar]
- 24. Abouzari M, Goshtasbi K, Chua JT, et al. Adjuvant migraine medications in the treatment of sudden sensorineural hearing loss. Laryngoscope. 2020. Early View [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Arslan Y, Arslan İB, Aydin H, Yağiz Ö, Tokuçoğlu F, Çukurova İ. The etiological relationship between migraine and sudden hearing loss. Otol Neurotol: Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. 2017;38(10):1411‐1414. [DOI] [PubMed] [Google Scholar]
- 26. Hwang J‐HMDP, Tsai S‐J, Liu T‐CP, Chen Y‐CMD, Lai J‐TMD. Association of tinnitus and other cochlear disorders with a history of migraines. JAMA Otolaryngol – Head Neck Surg. 2018;144(8):712‐717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting Information


