Abstract
Coronavirus disease 2019 (COVID-19) is a novel viral infection that has led to a global pandemic. The clinical spectrum of COVID-19 has a wide range from asymptomatic disease to severe disease, including acute respiratory distress syndrome and death. The most common symptoms are fever, cough, myalgia, and fatigue. Diarrhea, headache, sore throat, and hemoptysis are rare symptoms. There is no patient with COVID-19 presenting with massive hemoptysis in the literature. Here we present a case series of 3 patients with COVID-19 who were admitted to the emergency department with massive hemoptysis without any other symptoms.
Keywords: Respiratory Infections, hemoptysis, COVID-19, presentation
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a novel viral infection first identified in Wuhan, China, in December 2019. It has spread rapidly and is now considered a global pandemic. The clinical course of COVID-19 has a wide range from asymptomatic disease to severe disease, including acute respiratory distress syndrome and death [1–3]. The most common symptoms are fever (89.1%), cough (72.2%), myalgia and fatigue (42.5%). Diarrhea, headache, sore throat, and hemoptysis are the rare symptoms [4]. There is no patient with COVID-19 presenting with massive hemoptysis in the literature. Here we present a case series of 3 patients with COVID-19 who were admitted to the emergency department with massive hemoptysis without any other symptoms.
CASE PRESENTATIONS
Case 1
A 55-year-old male patient was admitted to the emergency department with the complaint of new onset of cough and 1 cup of blood expectoration (approximately 200 cm3). He had no fever or other respiratory symptoms. There was no contact with a patient with COVID-19. He had hypertension and was an active smoker (25 packages/year). The vital findings and physical examination of the chest were normal. At the time of admission, hemogram and biochemical markers were within normal limits. Thoracic computed tomography (CT) revealed bilateral diffuse ground-glass opacities especially on the left lung (Figure 1). These findings were reported in accordance with alveolar hemorrhage. It is stated that atypical pneumonia is also included in the differential diagnosis. He was hospitalized in the Chest Diseases Service, and oxygen therapy, tranexamic acid (intravenous), and levodropropizine syrup were started. During his first day of hospitalization, he had hemoptysis up to 100 cm3 2 more times. On the second day of hospitalization, COVID-19 polymerase chain reaction (PCR) was reported as positive, and he was transferred to the COVID service.
Figure 1.
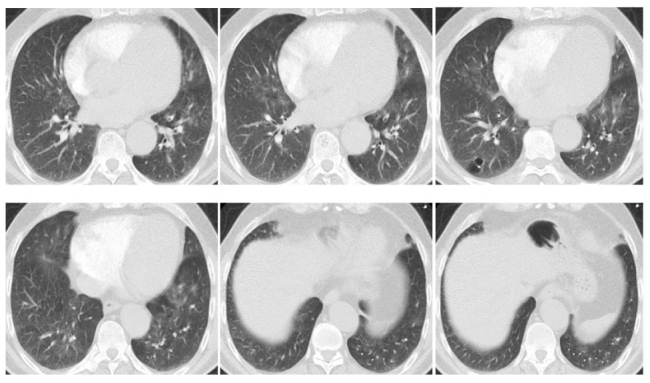
Thoracic CT images of case 1
CT: computed tomography
Case 2
A 56-year-old male patient was admitted to the emergency department with cough and massive hemoptysis (approximately 1.5 cup of blood). He had no chronic disease but was an active smoker (37 packages/year). In his physical examination, there were expiratory rhonchi over the right middle and lower zone. Initial laboratory values were normal except for slight C-reactive protein (CRP) increase (white blood cell [WBC]: 7.7×103/μL, neutrophil: 4.9×103/μL, and CRP: 8.93 mg/L). Thoracic CT revealed tubular bronchiectasis in the right upper lobe and spiculated nodular lesion with 2 cm diameter, and positron emission tomography-CT was recommended for differential diagnosis of the malignancy (Figure 2). Sputum gram and AFB (acid-fast bacilli) staining were negative. Nonspecific sputum culture and fungus culture were normal. However, the COVID-19 PCR result was positive.
Figure 2.
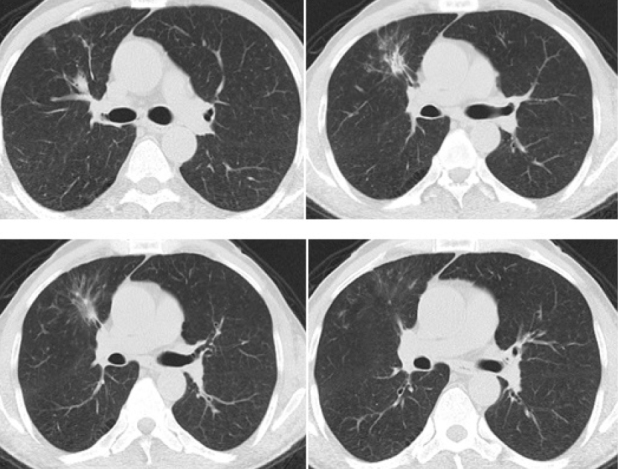
Thoracic CT images of case 2
CT: computed tomography
Case 3
A 48-year-old male patient was admitted to the emergency department with massive hemoptysis (approximately 400 cm3 within 2 hours). He had hypertension and was an active smoker (35 packages/year). On physical examination, there were inspiratory crackles over the left lower zone. Initial laboratory findings were as follows: WBC: 16.2×103/μL; neutrophil: 13.1×103/μL; and CRP: 6.31 mg/L. Troponin I, procalcitonin, and biochemical values were normal. Thoracic CT revealed bronchiectasis, pneumonic infiltrations accompanied by peribronchial thickening and mucus retention in the left lower lobe, and acinar pneumonic infiltration in the right middle lobe (Figure 3). His COVID-19 PCR test was positive.
Figure 3.
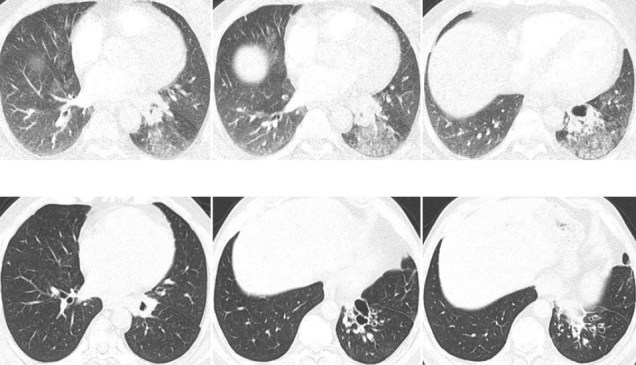
Thoracic CT images of case 3
CT: computed tomography
DISCUSSION
COVID-19, which caused a global epidemic, remains a mystery. It has a wide clinical spectrum. Although it may be asymptomatic in some cases, it may cause severe clinical conditions that may lead to respiratory failure and death in others [2].
Symptoms are usually nonspecific, including fever, dry cough, and fatigue. Multiple systems may be involved, such as respiratory (cough, shortness of breath, sore throat, hemoptysis, and chest pain), gastrointestinal (diarrhea, nausea, and vomiting), musculoskeletal (muscle ache), and neurological (headache or confusion) [1–3].
Hemoptysis is the act of coughing up blood from the trachea and bronchial system. It is one of the emergencies of chest diseases. It may be the symptom of a number of diseases such as tuberculosis, malignancy, bronchiectasis, and pneumonia [5]. However, it is a rare clinical presentation of COVID-19 [6]. The prevalence of hemoptysis was 3% among the patients with COVID-19 in the case series reported in China [7]. There is 1 case report presenting patients with COVID-19 whose initial symptom was hemoptysis [8]. According to our knowledge, this is the first case series reporting COVID-19 cases presenting with massive hemoptysis.
Approximately 5%–15% of the hemoptysis episodes are massive and may require urgent intervention. Massive hemoptysis is defined as 200 to 1000 cc of bleeding in 24 hours [9]. The most widely used criteria for the definition of massive hemoptysis is expectoration of 300–600 cm3 blood in a 24-hour period [10]. It should always be considered as a life-threatening condition that warrants effective assessment and management [5]. In our case series, all the patients had massive hemoptysis with no accompanying symptoms. Based on their clinical and laboratory findings, diagnosis of COVID-19 was not suspected in any of the patients on admission. However, COVID-19 PCR tests, which were essentially performed to exclude the diagnosis because the patients were hospitalized in a non–COVID-19 clinic, were positive in all the patients.
COVID-19 was described as causing a proinflammatory and hypercoagulable state with increased levels of lactate dehydrogenase (LDH), ferritin, CRP, D-dimer, and interleukin [11]. Venous thromboembolism (VTE) may also accompany COVID-19 infection because of hypercoagulability [12]. Hemoptysis may be an initial symptom of VTE, and there is a case presenting with hemoptysis owing to pulmonary emboli associated with COVID-19 [11]. In our patients, hypercoagulability values such as D-dimer, ferritin, and LDH were within normal limits, and no VTE was observed in the radiological examination.
The fact that all of our patients were active smokers suggests that smoking may be related to admitting with hemoptysis symptoms. It is known that cigarette smoke damages the alveolar epithelial cells because of oxidative stress, increases epithelial cell death, and decreases lung repair process [13]. In addition, suspicion of malignancy in 1 of the patients and the presence of bronchiectasis in the other may have contributed to the development of hemoptysis.
In conclusion, patients with COVID-19 may not always present with the predefined frequent symptoms such as fever, cough, and fatigue. COVID-19 is a new disease with many unknown aspects; therefore, atypical presentations such as massive hemoptysis also should raise suspicion about the diagnosis of COVID-19 especially in pandemic conditions.
MAIN POINTS.
Cough and dyspnea are common and well known symptoms of COVID-19 patients.
Hemoptysis is another symptom of COVID-19 but it is rarely seen.
COVID-19 patients can also admit with massive hemoptysis as an atypical clinical presentation.
COVID-19 is a novel virus and still remains a mystery. It should be kept in mind that COVID-19 may present with different clinical findings, especially in pandemic conditions.
Footnotes
Informed Consent: Written informed consent was obtained from all of the patients.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.A.B., İ.S.C., G.S., H.B., İ.B.; Design - S.A.B., İ.S.C., G.S., H.B., İ.B.; Supervision - S.A.B., İ.S.C., G.S., H.B., İ.B.; Resources - S.A.B.; Materials - İ.S.C, G.S.; Data Collection and/or Processing - S.A.B., G.S.; Analysis and/or Interpretation - İ.B.; Literature Search - S.A.B., İ.S.C.; Writing Manuscript - S.A.B.; Critical Review - S.A.B., H.B., İ.B.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 doi: 10.1016/S0140-6736(20)30183-5. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu YC, Chen CS, Chan YJ. The outbreak of COVID-19: An overview. J Chin Med Assoc. 2020;83:217–20. doi: 10.1097/JCMA.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. N Engl J Med. 2020 doi: 10.1016/S0140-6736(20)30211-7. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun P, Qie S, Liu Z, et al. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: A single arm meta-analysis. J Med Virol. 2020;92:612–7. doi: 10.1002/jmv.25818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sakr L, Dutau H. Massive hemoptysis: an update on the role of bronchoscopy in diagnosis and management. Respiration. 2010;80:38–58. doi: 10.1159/000274492. [DOI] [PubMed] [Google Scholar]
- 6.Pal M, Berhanu G, Desalegn C, et al. Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): An Update. Cureus. 2020;12:e7423. doi: 10.7759/cureus.7423. doi: 10.7759/cureus.7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi F, Yu Q, Huang W, Tan C. 2019 Novel Coronavirus (COVID-19) Pneumonia with hemoptysis as the initial symptom: CT and clinical features. Korean J Radiol. 2020;21:537–40. doi: 10.3348/kjr.2020.0181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rali P, Gandhi V, Tariq C. Massive hemoptysis. Crit Care Nurs Q. 2016;39:139–47. doi: 10.1097/CNQ.0000000000000107. [DOI] [PubMed] [Google Scholar]
- 10.Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med. 2000;28:1642–7. doi: 10.1097/00003246-200005000-00066. [DOI] [PubMed] [Google Scholar]
- 11.Casey K, Iteen A, Nicolini R, Auten J. COVID-19 pneumonia with hemoptysis: Acute segmental pulmonary emboli associated with novel coronavirus infection. Am J Emerg Med. 2020;38:1544.e1–1544.e3. doi: 10.1016/j.ajem.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danzi GB, Loffi M, Galeazzi G, et al. Acute pulmonary embolism and COVID-19 pneumonia: A random association? Eur Heart J. 2020;41:1858. doi: 10.1093/eurheartj/ehaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aoshiba K, Nagai A. Oxidative stress, cell death, and other damage to alveolar epithelial cells induced by cigarette smoke. Tob Induc Dis. 2003;1:219–26. doi: 10.1186/1617-9625-1-3-219. [DOI] [PMC free article] [PubMed] [Google Scholar]


