Abstract
With the rapid spread of coronavirus disease 2019 (COVID-19), a particularly sharp increase in the number of confirmed cases in Daegu and Gyeongbuk regions at the end of February, Korea faced an unprecedented shortage of medical resources, including hospital beds. To cope with this shortage, the government introduced a severity scoring system for patients with COVID-19 and designed a new type of quarantine facility for treating and isolating patients with mild symptoms out of the hospital, namely, the Residential Treatment Center (RTC). A patient with mild symptoms was immediately isolated in the RTC and continuously monitored to detect changes in symptoms. If the symptoms aggravate, the patient was transferred to a hospital. RTCs were designed by creating a quarantine environment in existing lodging facilities capable of accommodating > 100 individuals. The facilities were entirely divided into a clean zone (working area) and contaminated zone (patient zone), separating the space, air, and movement routes, and the staff wore level D personal protective equipment (PPE) in the contaminated zone. The staffs consisted of medical personnel, police officers, soldiers, and operation personnel, and worked in two or three shifts per day. Their duty was mainly to monitor the health conditions of quarantined patients, provide accommodations, and regularly collect specimens to determine if they can be released. For the past two months, RTCs secured approximately 4,000 isolation rooms and treated approximately 3,000 patients with mild symptoms and operated stably without additional spread of the disease in and out of the centers. Based on these experience, we would like to suggest the utilization of RTCs as strategic quarantine facilities in pandemic situations.
Keywords: COVID-19, Coronavirus, Residential Treatment Center, Isolation, Korea
Graphical Abstract
INTRODUCTION
In Korea, the first confirmed case of coronavirus disease 2019 (COVID-19) was identified on January 19, 2020. The number of confirmed cases gradually increased until late February but rapidly surged after that period, exceeding 1,000 confirmed cases a day. The sharp increase in the number of patients resulted in a shortage of isolation beds and medical personnel and even death of patients who were waiting for hospitalization. To tackle this challenge, the Korean government and medical society decided to secure additional hospital beds and set up patient management teams in each city and province to allocate hospital beds in accordance with the severity of the confirmed patients. Since then, patients with mild symptoms, which account for > 80% of all confirmed cases, have been quarantined at the Residential Treatment Center (RTC), an out-of-hospital isolation facility1. At that time, approximately 40% of the patients were quarantined at the center; thus, the number of confirmed patients awaiting hospitalization sharply reduced and treatment could be offered depending on the symptoms of patients.1,2
The first author of this article is a leading researcher who has been responsible for the development of the standardized model of RTC management launched by the COVID-19 Central Disaster Management Headquarters in April 2020. She also supported in establishing guidelines applicable to on-site work and analyzing strategies as a non-government expert of the Headquarters since February 2020. The purpose of this article is to share practical information drawn from the process of RTC management standardization and empirical lessons learned from the current experience regarding RTCs. The data analyzed included the current status of the RTCs offered by the COVID-19 Central Disaster Management Headquarters, and it was categorized into four sub-items and re-constructed for daily units (such as facility, workforce, patients, and other issues related to management). The period of analysis spanned from March 2 to April 30, when the number of confirmed cases of COVID-19 has been the highest so far as of the end of October. Thus, we would like to suggest a future direction for more effective management of RTCs and more appropriate treatment for COVID-19 patients with mild symptoms by sharing the latest experience.
OVERVIEW OF RTC
A total of 18 RTCs were designed and operated in Daegu, Gyeongsang-do, Chungcheong-do, Joella-do, and Gyeonggi-do in March and April 2020. The largest number of confirmed cases was noted at that time throughout the country. They secured approximately 4,000 single-person isolation rooms and treated approximately 3,000 patients with mild symptoms (Table 1).2
Table 1. Designation and operation status of residential treatment centers.
| No. | Name | Operation period | No. of Isolation rooms | Original usage of the facility | Region | ||
|---|---|---|---|---|---|---|---|
| Launch, date | Close, date | Term, day | |||||
| 1 | Daegu 1 | Mar 02, 2020 | Apr 29, 2020 | 58 | 160 | Dormitory | Daegu |
| 2 | Gyeongbuk-daegu 1 | Mar 04, 2020 | Apr 30, 2020 | 57 | 210 | Group education | Gyeongbuk |
| 3 | Gyeongbuk-daegu 2 | Mar 03, 2020 | Apr 16, 2020 | 44 | 235 | Group education | Gyeongbuk |
| 4 | Gyeongbuk-daegu 3 | Mar 05, 2020 | Apr 10, 2020 | 36 | 99 | Group education | Gyeongbuk |
| 5 | Gyeongbuk-daegu 4 | Mar 05, 2020 | Mar 30, 2020 | 25 | 100 | Group education | Gyeongbuk |
| 6 | Gyeongbuk-daegu 5 | Mar 06, 2020 | Apr 16, 2020 | 41 | 67 | Group education | Gyeongbuk |
| 7 | Gyeongbuk-daegu 7 | Mar 09, 2020 | Apr 24, 2020 | 46 | 376 | Group education | Gyeongbuk |
| 8 | Gyeongbuk-daegu 8 | Mar 10, 2020 | Apr 20, 2020 | 41 | 280 | Group education | Gyeongbuk |
| 9 | Chungnam-daegu 1 | Mar 06, 2020 | Mar 27, 2020 | 21 | 600 | Group education | Chungnam |
| 10 | Gyeongbuk 1 | Mar 05, 2020 | Apr 25, 2020 | 51 | 56 | Group education | Gyeongbuk |
| 11 | Daegu 2 | Mar 08, 2020 | Mar 28, 2020 | 20 | 490 | Dormitory | Daegu |
| 12 | Chungbuk-daegu 1 | Mar 09, 2020 | Apr 05, 2020 | 27 | 136 | Group education | Chungbuk |
| 13 | Chungbuk-daegu 2 | Mar 08, 2020 | Mar 29, 2020 | 21 | 170 | Recreation | Chungbuk |
| 14 | Jeonbuk-daegu 1 | Mar 11, 2020 | Apr 07, 2020 | 27 | 210 | Group education | Jeonbuk |
| 15 | Chungbuk-daegu 3 | Mar 12, 2020 | Apr 08, 2020 | 27 | 179 | Group education | Chungbuk |
| 16 | Chungbuk-daegu 4 | Mar 13, 2020 | Apr 10, 2020 | 28 | 450 | Group education | Chungbuk |
| 17 | Gyeonggi-international 1a | Mar 25, 2020 | Apr 28, 2020 | 31 | 70 | Group education | Gyeonggi |
| Apr 29, 2020 | Continue | - | 45 | Group education | Gyeonggi | ||
| 18 | Gyeonggi-international 2 | Mar 27, 2020 | May 15, 2020 | 50 | 200 | Group education | Gyeonggi |
RTC is a temporary quarantine facility other than a hospital that isolates patients with mild symptoms of COVID-19. It was operated by creating an isolation environment in a large-scale accommodation facility capable of accommodating approximately 100 individuals and deploying medical personnel.3
The types of RTC can be divided into centers for local patients and centers for foreign patients according to the patient's nationality. Of the 18 centers, 16 were for locals and two were for foreigners. The centers for local patients were operated by local governments, and RTC rooms were assigned to patients based on their residential district. Meanwhile, the centers for foreign patients were operated by the Central Disaster Management Headquarters, and foreigners who do not have residence in Korea or Korean individuals who are difficult to move to the RTC located in their residence were admitted in these centers. The centers for foreigners were established in Gyeonggi-do near Incheon International Airport.
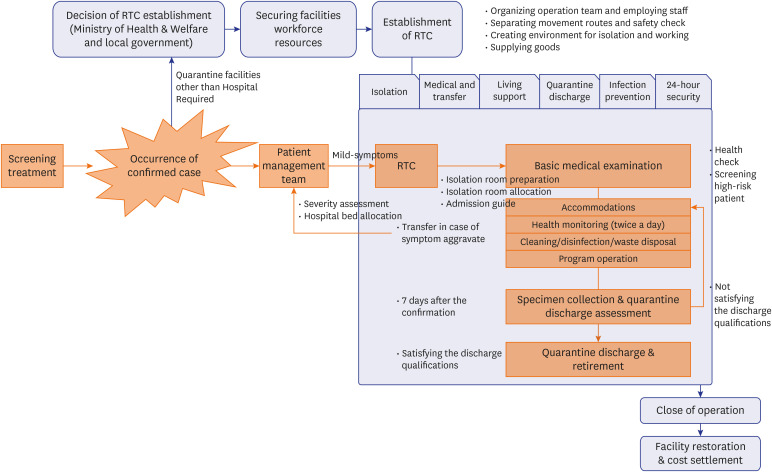
Although the two types of RTC differ in their operation agent, they manage patients in the same way (Fig. 1). However, in the case of centers for foreigners, interpretation was required for various guidance programs and health examinations, and the culture of each country, including foods, should be considered.
Fig. 1. Establishment and operation flow of RTC.
Blue Box (establishment, operation, and close of RTC): The Ministry of Health & Welfare and local governments may decide to establish the RTC. They secure facilities for RTCs and carry out planning, staffing, and resources management.
Orange Box (admission, isolation, and discharge of patients): when a COVID-19 patient is confirmed through screening treatment, the patient management team immediately assesses the severity and assigns a bed. Patients with mild symptoms are admitted immediately after being assigned to RTC, undergoing a basic medical examination, and quarantined until criteria for lifting isolation is satisfied.
RTC = residential treatment center, COVID-19, coronavirus disease 2019.
REQUIREMENTS OF RTC AND ZONE SEPARATION
All facilities used as RTCs were pre-existing facilities for group education, recreation, and dormitory, and they were originally managed by public organizations, private corporations, colleges or universities. They usually have large-scale sites consisting of several buildings and are located relatively far from downtown. Therefore, location conditions were favorable for controlling the spread of infectious diseases between RTCs and the community and also between confirmed patients and non-confirmed individuals in the RTC (Table 2).
Table 2. Requirements of residential treatment center.
| Item | Requirements |
|---|---|
| Location | - (Geography) Facilities away from downtown and residential area |
| - (Structure) Separation of movement routes and air circulation between contaminated and clean zone | |
| System | - (CCTV and Broadcasting) 24-hr CCTV and broadcasting system for maintenance of order and breakaway prevention |
| - (Ventilation) Blocking air circulation between zones and natural ventilation through air conditioning system | |
| Isolation Rooms | - A room for one person (two or more people from the same group permitted restrictively) |
| - Providing bedroom, shower facility (water supply/drainage), and toilet | |
| - Air separation between rooms and natural ventilation | |
| - Treatment facilities (for simple treatment and first aid) | |
| - TV, Internet, and telephone available | |
| Working and living facility | - Creating an office environment based on work details and movement routes |
| - Air separation between the zones and natural ventilation | |
| - A room for one or two people as for living facility and maintaining optimal temperature | |
| - Providing individual or shared shower facility, toilet, and laundry facility | |
| - TV, Internet, and telephone available | |
| Area separation | - Separation of contaminated zone and clean zone by designating individual building as each zone |
| - Separation of movement routes and floor in case of contaminated zone and clean zone existing in the same building | |
| - Installation of PPE changing room outdoor or in separate structure (i.e. containers) | |
| - Installation of temporary waste storage outdoor or in separate structure (i.e. containers) | |
| Safety & security | - (Outside) Securing transportation for patients’ transfer to hospital |
| - (Inside) Measures to prevent fall accidents from balconies and stairs | |
| - (Inside) Securing fire prevention facilities (preparation of fire extinguisher, sprinkler, and emergency exit map) | |
| - (Inside) Access control for facilities that can damage the body | |
| - (Outside & Inside) 24-hr CCTV for prevention of breakaway, and maintenance of security and order | |
| - (Outside & Inside) Broadcasting system for announcement |
PPE = personal protective equipment.
The facilities within the RTC were composed of a quarantine facility in which the confirmed patient is isolated and a working and living facility in which medical and operation personnel live and work. The entire facility was defined as a contaminated zone or clean zone by assessing the risk of infection. In accordance with the zone definition, entrance and movement were separated between zones, and the air conditioning system should be adjusted to block air circulation so that the airflow in each zone is not connected.
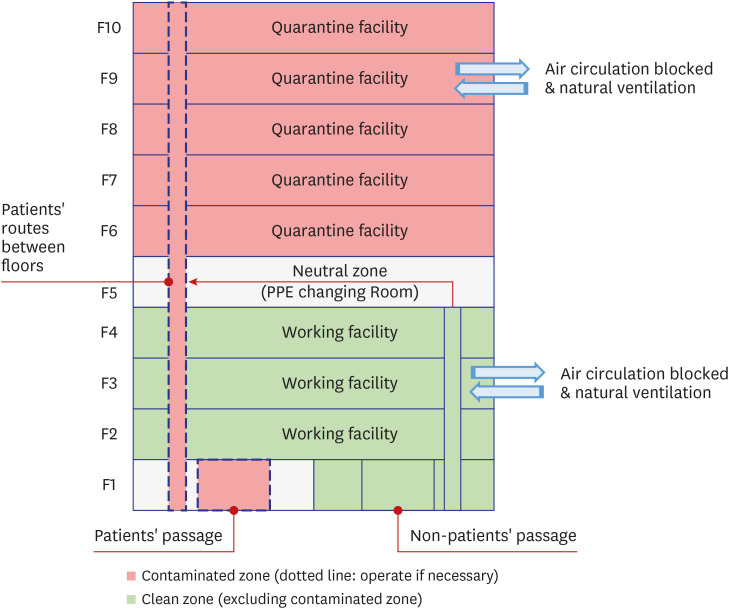
The quarantine facilities were entirely managed as contaminated zones, while most working facilities were managed as clean zones. Of the 18 centers, 17 consist of two or more buildings, and each building was defined as a quarantine facility (contaminated zone) or a working and living facility (clean zone).4,5 Only one center installed both facilities in the same building. Therefore, this center set independent entrance and movement routes for confirmed patients and staff and separated each floor into a clean floor (working facilities), neutral floor (protective gear changing rooms), and contaminated floor (isolation rooms) (Fig. 2).
Fig. 2. Separating zones of the one-building center.
• Designating contaminated/clean zone by floor.
• Blocking indoor air circulation and natural ventilation in all zones.
• Preparing a neutral zone between contaminated zone and clean zone.
• Restriction on patients' movement between floors (permit only when admission, waste disposal, etc.).
The entire building (or floor) of a quarantine facility was a contaminated zone. It consists of isolation rooms, hallways, stairs, and a nursing room. The isolation room was a single-person room, and there were bedroom, shower facility, and toilet in the room. TV and Internet were also available. Once a confirmed patient was admitted to the center, they could not leave their own room until they were released from quarantine, with the exception of meal supply, medical examination, and specimen collection, and transferred to a hospital if symptoms appear and worsen. Staffs should wear level D PPE when entering the quarantine facility for medical treatment, specimen collection, food and beverage supply, disinfection, and cleaning.
As for a working facility, all or most spaces were clean zones. A working facility was composed of offices, medical support rooms, storages, security and broadcasting rooms, conference rooms, restrooms, PPE changing rooms, and living rooms. The confirmed patients could not enter this zone, and staff should wear a mask. Among the working facilities, a room for specimen collection and temporary waste storage were considered contaminated zones and were installed in a separate area with smooth ventilation or in a separate structure (i.e., containers and tents) near the entrance of the building. The PPE changing room was installed in a separate area outside the entrance to a contaminated zone, where the clean and contaminated zones were converted.
All facilities should be sterilized at least once a day and immediately disinfected if the following events occur: when the area is exposed to a confirmed patient; when an individual, wearing PPE, directly contacts a patient and stays in the area; when disposing of waste; and when a patient is discharged. In addition, further measures were taken to prevent the spread of the disease and ensure safety, such as no access to unauthorized personnel, 24-hour CCTV operation, broadcasting for regulations, and regular inspection to prevent damage and fire.
WORKFORCE OF RTC
The personnel who worked at the RTC were classified into five groups: public officials from the Ministry of Health and Welfare, the Ministry of Public Administration and Security, and local governments; police officers, military personnel, and firefighters from the National Police Agency, the Ministry of National Defense, and the National Fire Agency; employees of public institutions, such as National Health Insurance Corporation and National Pension Service; medical personnel from the affiliated hospitals of each RTC; and medical professionals who personally volunteered for medical support. They worked in two or three shifts.
An average of 98 patients were admitted to each center, and an average of 56.3 staffs (nonmedical, 60.5% and medical 39.5%) worked in each center. Among the medical personnel, an average of 6 physicians and 8.8 nurses were employed (Table 3).
Table 3. The average number of patients and staffs at residential treatment center (n = 18) (unit: person).
| No. of patients | No. of staffs | ||||||
|---|---|---|---|---|---|---|---|
| Total | Non-medical | Medical | |||||
| Subtotal | Physician | Nurse | Others | ||||
| Mean (n = 18) | 98.4 ± 77.8 | 63.71 ± 23.96 | 34.1 ± 13.8 | 29.6 ± 14.6 | 6.0 ± 2.8 | 8.8 ± 3.9 | 7.4 ± 4.6 |
| < 100 (n = 4)a | 36.1 ± 26.9 | 44.94 ± 12.23 | 26.1 ± 11.7 | 18.8 ± 7.9 | 4.9 ± 1.5 | 6.0 ± 2.0 | 4.0 ± 3.5 |
| 100–199 (n = 5)b | 87.0 ± 41.7 | 58.65 ± 17.88 | 30.7 ± 11.0 | 27.9 ± 8.1 | 5.4 ± 1.9 | 7.3 ± 2.2 | 7.6 ± 2.7 |
| 200–299 (n = 5)c | 111.9 ± 70.6 | 64.58 ± 11.34 | 37.8 ± 6.2 | 26.8 ± 7.5 | 5.0 ± 1.6 | 9.0 ± 1.8 | 6.4 ± 3.3 |
| 300–399 (n = 4)d | 178.9 ± 96.2 | 95.91 ± 27.71 | 43.5 ± 18.5 | 52.4 ± 14.6 | 10.1 ± 3.4 | 14.5 ± 4.6 | 13.8 ± 3.7 |
Values are presented as mean ± standard deviation.
aGyeongbuk-daegu 3/Gyeongbuk-daegu 5/Gyeongbuk 1/Gyeonggi-international 1; bDaegu 1/Gyeongbuk-daegu 4/Chungbuk-daegu 1/Chungbuk-daegu 2/Chungbuk-daegu 3; cGyeongbuk-daegu 1/Gyeongbuk-daegu 2/Gyeongbuk-daegu 8/Jeonbuk-daegu 1/Gyeonggi-international 2; dGyeongbuk-daegu 7/Chungnam-daegu 1/Daegu 2/Chungbuk-daegu 4.
They were in charge of medical support tasks, such as daily health examinations, regular specimen collection and test requests, and hospital transfer and quarantine discharge. Furthermore, they also conducted operation tasks, such as establishment of isolation rooms and facility management, supply of food and beverage, living support, cleaning/disinfection/waste disposal, purchase of goods, and contracts and budgeting (Table 4).
Table 4. Workforce of RTC and duties.
| Workforce | Duty |
|---|---|
| Public officials and operation personnel | - Administrative action including contraction and buying for disinfection, cleaning, waste disposal, laundry, and food & beverage supply |
| - Daily action report including RTC’s situation and waste disposal declaration | |
| - Purchase of supplies including food & beverages, daily necessities, and office equipment (procuring food & beverages from nearby restaurant or lunch box suppliers) | |
| Medical personnel | - Checking health status for patients newly admitted to the center |
| - Daily examination and monitoring for patients and staffs (twice a day), and simple medical treatment | |
| - Collecting specimens and requesting tests | |
| - Patients’ transfer to hospital and decision making on quarantine discharge | |
| - Informing patients on matters to observe after quarantine discharge | |
| - Prevention of further infection within the center by training non-medical workers to wear PPE properly | |
| - Recording all kinds of medical treatment or measurements | |
| Police officers | - Control over breakaway from and access to the center via 24 hr CCTV, and maintenance of order |
| Firefighters | - Taking a patient to an affiliated hospital, deploying workforce urgently, and doing safety inspection |
| Soldiers | - Distributing food & beverages, daily necessities, and waste container |
| Facility managers | - Functional checkout and adjustment of the installation in the center |
| Disinfection/cleaning/laundry companies | - Disinfection and general cleaning of the center, collecting and washing staff’s laundry (at least once a day) |
| - Isolated patients’ clothes must be washed individually within the room | |
| Waste disposal companies | - Disposal of waste from the center (once a day) |
RTC = residential treatment center, PPE = personal protective equipment.
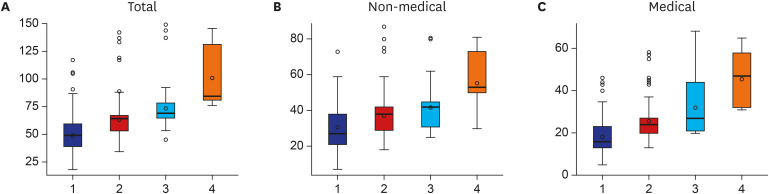
The more the number of patients admitted to the RTC, the more staff worked there (Fig. 3). Particularly, as the number of patients increases, the workload related to the supply of food and beverages, admission to quarantine, and sample collection increases.
Fig. 3. Staff distribution by the number of patients. Group 1 implies less than 100 patients, Group 2 implies 100 to less than 200 patients, Group3 implies 200 to less than 300 patients, and Group 4 implies more than 300 patients.
Since it is a critical issue to prevent staffs from obtaining COVID-19 infection, all personnel in the center have minimized direct contact with patients, excluding arranged contacts, such as admission, specimen collection, face-to-face treatment, and transfer. When distributing food, beverages, and supplies, personnel should wear level D PPE to enter a quarantine facility, check that the doors of each isolation room are closed, and distribute the goods in front of each door. Meanwhile, the security officer observes the situation through CCTV and announces the time of the start and end of the supply of goods through broadcasting so that the patients and staff do not contact each other during the time. Medical personnel used mobile applications and mobile phones to monitor the health condition of patients daily. In all circumstances that staff should contact patients, including admission guidance, specimen collection, and face-to-face medical treatment, staff were supposed to wear level D PPE and ensure natural ventilation. Finally, medical personnel trained non-medical workers to wear PPE properly and checked their health status daily.
PATIENT MANAGEMENT AT RTC
Those who were admitted to the center are able to engage in physical activity and are asymptomatic or have mild symptoms, such as coughing, sputum, and muscle pain.5,6
After getting off the transport vehicle, patients entered the isolation room following the staff’s guide and along movement routes. They were supposed to be isolated in the room until they were released from quarantine, excluding arranged schedules, such as food and beverage supply and specimen collection.
The isolation room was a single room for one person, and TV, internet access, shower facility, and toilet were available. A thermometer, toiletries, hand sanitizers, and masks were provided in the room, and food, drinks, and waste disposal supplies (i.e., containers and envelopes) were also provided daily. Some centers provided leisure items, such as exercise props and art tools.
DISCUSSION
In the midst of the rapid spread of COVID-19, RTCs quickly secured quarantine facilities by utilizing pre-existing accommodations with personal bedrooms and individual toilets. The first RTC was launched on March 2, 2020, 12 days after February 19 when the surge in the number of confirmed cases of COVID-19 was detected in the Daegu and Gyeongbuk regions. As for the capital area, a decision on the RTC operation was made on August 16, two days after August 14, when the spread of the disease around the metropolitan area increased, and the RTCs in the capital area have been operating since August 19. In other words, RTCs usually began to operate three to four days after the decision was made on its establishment, and secured as many isolation rooms as possible in a short duration. Further spread of the disease inside and outside the center has not been reported so far within the operation period of RTCs. Regular health checks for the patients (more than twice a day) by the medical team residing in RTCs allowed for the quick identification of patients with worsening symptoms and consequently, their immediate transfer to a designated hospital for proper management. Through this, patients with mild symptoms could be safely isolated and treated on time. These strengths of RTCs can be considered as a critical strategy to secure beds in the face of the spread of COVID-19.7 As of late October 2020, eight RTCs and approximately 2,000 isolation rooms located nationwide (Seoul, Gyeonggi, and Incheon), are controlled by the COVID-19 Central Disaster Management Headquarters.
However, there are discussion points and practical limitations to be dealt with for more stable operation of RTCs. First, the fixed cost of operating a center is high. The establishment of RTCs requires regular payment, such as rent of the facility, creation of an isolation environment, labor costs, and disinfection, regardless of the number of quarantined patients. Therefore, it may be irrational to operate an RTC if there are relatively fewer patients. Second, RTCs are not medical institutions. Medical personnel dispatched to RTCs are in a situation where they have to take care of patients with infectious disease at accommodations, not at hospitals. In fact, for medical personnel at RTCs, the way to check patients' health status is basically contact-free using devices such as mobile phones, and face-to-face treatment is allowed only when medical personnel wear level D PPE. The equipment available for examination is limited to thermometers, blood pressure monitoring devices, blood glucose monitoring devices, X-ray machines, and pulse oximeters. Thus, the range of services offered by RTCs needs to be clarified as follows: strict quarantine of COVID-19 patients with mild symptoms, immediate transfer to a designated hospital in case of symptom change, and judgement of release. Third, RTCs cannot provide an environment where negative pressure ventilation is possible. Therefore, as an alternative measure, an air conditioning system is utilized to prevent air mixing in the center. However, each facility has different air conditioning system, and some facilities have systems where air conditioning and heating functions work simultaneously. To block indoor air mixing, RTCs modify the air conditioning system to 100% ambient air mode or circulate the air depending solely on natural ventilation. Therefore, if an RTC is restricted to operate the heating and cooling system for the aforementioned reasons, supplementary equipment such as a heating pad would be required. In addition, system and equipment maintenance should be carried out regularly because problems related to ventilation and humidity within the building might occur.
Besides, many other countries abroad have recently experienced the re-spread of COVID-19, and we should also be prepared for the greater spread of the disease that is more severe than we have ever experienced before. Therefore, it is necessary to discuss a counterplan to operate RTCs more efficiently and stably in the event of a rapid spread of the infectious disease. There are three main points to be considered: 1) securing the facilities in which an RTC can be established immediately and preparing for weakness depending on each regional specification, 2) efficient allocation of medical personnel, and 3) providing patients with a psychological support program.
First, as for securing the facilities, most facilities used to install RTCs, mainly lodgings, were relatively far from downtown and residential areas and composed of two or more buildings, which makes it easier to create a quarantine environment. However, not all accommodations meet the qualifications for quarantine. Facing the need for even more RTCs than previously operated, it is necessary to consider creating an isolated environment in facilities that are not qualified. To prepare for this situation, the location, building structure, and air conditioning of facilities that can be used as RTCs should be investigated and listed in advance. Based on the results of the investigation, the facility’s usability, requirements for creating an isolation environment, number of available isolation rooms, and their distribution by region should be checked in advance to analyze limitations and establish with countermeasures.
Second, the efficient allocation of medical personnel is also crucial. An RTC managed an average of 98 patients with 6.0 physicians and 8.8 nurses. This was a very efficient method in terms of medical personnel for the number of quarantined patients. However, a sharp increase in the number of confirmed cases will lead to a shortage of medical personnel in hospitals that treat patients with severe symptoms and may limit medical resource availability at RTCs. To cope with this shortage, the government should prepare measures to allocate medical resources more efficiently in RTCs. RTCs usually have a team of physicians and nurses working in two or three shifts a day, and these medical teams treat patients without direct contact by using mobile devices. However, they should prepare all the time to respond to changes in the health conditions of the inmates and immediately transfer in case a patient's symptoms worsen. Furthermore, the day of sample collection, which is approximately 2–3 times a week, and the day of new admission require more medical personnel than usual. Therefore, based on this process of work, a more flexible operation should be considered, which operate the medical team normally with a minimal capacity but immediately deploy skilled personnel, if necessary. For instance, medical personnel can be placed at a minimum for regular health monitoring at all times, and an independent medical support team, which is dedicated to admission and sample collection, can be deployed on a schedule or upon request. In addition to the flexibility of the medical personnel arrangement, the suggested operation method can be expected to affect the education and training of staff at the newly installed RTCs.
Finally, there is a need for a psychological support program for patients. In addition to the prevention of additional spread of the disease and living support in the RTCs, another major issue was the negative psychological state of the inmates. Many isolated patients complained of depression and lethargy due to the situation in which they were confirmed to have COVID-19 and must live in isolation for a long time in a strange place and might have spread it to someone else.8 That the inmates were isolated in one room per person and direct contact with others, including medical personnel, was strictly minimized is one of the risk factors of negative psychological state. To overcome this problem, staffs continuously communicate with their inmates via mobile phones and check their psychological conditions during health monitoring. Moreover, some centers provided entertainment by creating an environment where media, such as TV and internet, could be used; operated their own programs, such as radio broadcasting, small-scaled concert, and exercise/smoking cessation clinics; offered books, sports equipment, and art tools for leisure in the individual room; and provided counseling services through psychological counselors. However, these programs are an inconsistent policy in RTCs but are achieved by the ideas and active responses of the center's staffs and only possible when the center is stable. Therefore, a system should be established, through which the psychological state of the inmates can be monitored more actively and remains stable even when the number of confirmed cases increases rapidly. For example, once a patient is admitted to the center, their mental health should be monitored daily, and the change in mental state is checked. It is also necessary to analyze in advance if a patient has any factors that have a negative impact on others, such as stigma, uncertainty, and loneliness, and immediately respond to the patient, converting the program from regular monitoring to specialized counseling. Moreover, operating the same group isolation, by which the patients can communicate with and support each other, can be considered.
ACKNOWLEDGMENTS
The authors cordially thank the Korea Ministry of Health and Welfare and the National Health Insurance Service for offering the opportunity to participate in the project of management standardization of RTCs. The authors appreciate the COVID-19 Central Disaster Management Headquarters for sharing useful data and practical experience.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yang YS.
- Writing - original draft: Yang YS.
- Writing - review & editing: Kim HJ, Hwang JE.
References
- 1.Kim SW, Lee KS, Kim K, Lee JJ, Kim JY, Daegu Medical Association A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci. 2020;35(15):e152. doi: 10.3346/jkms.2020.35.e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ministry of Health and Welfare. A Round-table Conference with Cooperating Hospitals for the COVID-19 RTCs. Sejong: Ministry of Health and Welfare; 2020. [Google Scholar]
- 3.Central Disaster Management Headquarters, Central Disease Control Headquarters. Guidelines for the Operation of COVID-19 Residential Treatment Centers. Sejong: Ministry of Health and Welfare; 2020. [Google Scholar]
- 4.Kang E, Lee SY, Jung H, Kim MS, Cho B, Kim YS. Operating protocols of a community treatment center for isolation of patients with coronavirus disease, South Korea. Emerg Infect Dis. 2020;26(10):2329–2337. doi: 10.3201/eid2610.201460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park PG, Kim CH, Heo Y, Kim TS, Park CW, Kim CH. Out-of-hospital cohort treatment of coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J Korean Med Sci. 2020;35(13):e140. doi: 10.3346/jkms.2020.35.e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choe PG, Kang EK, Lee SY, Oh B, Im D, Lee HY, et al. Selecting coronavirus disease 2019 patients with negligible risk of progression: early experience from non-hospital isolation facility in Korea. Korean J Intern Med. 2020;35(4):765–770. doi: 10.3904/kjim.2020.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seoul Health Foundation, Seoul Center for Infectious Diseases Control and Prevention. The Daily News Review. Seoul: Seoul Health Foundation; 2020. [Google Scholar]
- 8.Hyun J, You S, Sohn S, Kim SJ, Bae J, Baik M, et al. Psychosocial support during the COVID-19 Outbreak in Korea: activities of multidisciplinary mental health professionals. J Korean Med Sci. 2020;35(22):e211. doi: 10.3346/jkms.2020.35.e211. [DOI] [PMC free article] [PubMed] [Google Scholar]