Highlights
-
•
Delay discounting associated with perceived stress.
-
•
Delay discounting associated beliefs about chance locus of control.
-
•
Delay discounting mediates relationship of perceived stress and length of recovery.
-
•
Delay discounting mediates relationship of perceived stress and age.
Keywords: Delay discounting, Recovery, Perceived stress, Locus of control
Abstract
Objective
Understanding individuals who are successful in recovery from substance use disorders will help to inform treatments and preventative measures. Stress has been shown to be associated with both substance use and relapse. Delay discounting is associated with risk of substance use; it is predictive of treatment outcomes and maintained abstinence. Associations between perceived stress, beliefs about locus of control, and delay discounting have yet to be assessed in individuals in recovery from substance use disorder.
Methods
Data from 93 individuals in recovery from substance use recruited from the International Quit and Recovery Registry (IQRR) were analyzed. Individuals completed the adjusting amount delay discounting procedure to obtain delay discounting rates. Level of perceived stress was assessed by the Perceived Stress Scale (PSS). An individual’s belief about locus of control was assessed using the Internality, Powerful Others and Chance Scale (IPCS).
Results
Delay discounting was a significant predictor of perceived stress and scores associated with beliefs about a Chance locus of control (i.e., belief that events that occur in an individual’s life are because of chance or luck), even after controlling for demographic characteristics. Time in recovery was also predictive of levels of perceived stress; this relationship was mediated by delay discounting.
Conclusion
The present study indicates that delay discounting can predict perception of stress and beliefs about a chance locus of control in individuals in recovery. This information may help understand, identify, and assist individuals whomay need different, new, or more intensive interventions for their substance use disorder.
1. Introduction
Substance abuse and substance use disorder are leading public health concerns and contribute considerably to the global burden of disease (Abuse, 2018). In 2017, over 19.5 million people had a substance use disorder in the United States alone (Abuse, 2018). Substance use disorders are highly comorbid with mental disorders (Kelly and Daley, 2013, Ross and Peselow, 2012) including anxiety disorders, depression, bipolar disorder, psychotic illnesses, borderline personality disorder, and schizophrenia (NIDA, 2018). Identifying the mechanisms and phenotype of successful recovery from substance use disorder is of utmost importance.
Psychological stress, an individual’s perception that environmental demands tax or exceed their adaptive capacity, predicts negative health behaviors, disease, and relapse (Cohen et al., 2007, Cohen et al., 1995, Herbert, 1997, Herman, 2012, Kassel et al., 2003). Measurements of an individual’s perception of stress, such as the Perceived Stress Scale (PSS) (Cohen, Kamarck, Mermelstein, & Others. , 1994), have been associated with symptoms of psychiatric disorders, such as anxiety and depression (Ghorbani et al., 2008, Sheffer et al., 2012) and greater levels of nicotine dependence (Cohen & Lichtenstein, 1990). Stress is similarly associated with likelihood to relapse in low-socioeconomic smokers (Ghorbani et al., 2008, Sheffer et al., 2012), the perception of less control over external events (Frazier et al., 2011), treatment outcomes (Berg et al., 2010), and an increased risk to initiate and escalate substance use (Lijffijt, Hu, & Swann, 2014).
The construct of an individual’s locus of control is a measurement of an individual’s perception of events contingent on one’s own behavior or beyond one’s control (Levenson, 1981). Beliefs about locus of control can be measured by expanding the internal versus external control scale into three subscales, Internality, Powerful Others, and Chance (Levenson, 1981). The Internality, Powerful Others, and Chance Scale (IPCS) was developed to assess whether individuals believe events occur due to one’s own behaviors, or due to external factors like fate, chance, or individuals with more power. More recently, another measure of locus of control was developed specific to substance use, the Drug-Related Locus of Control Scale (DRLOC; Ersche, Turton, Croudace, & Stochl, 2012). The DRLOC assesses beliefs about a successful recovery from substance use and decisions to use substances. Similar to the associations of stress mentioned above, beliefs about loci of control are associated with mental health problems, including depression and perceived stress (Costello, 1982, Frazier et al., 2011; Levenson, 1973, Rabani Bavojdan et al., 2011) Additionally, beliefs about locus of control are associated with abstinence from cigarette smoking (Gregor et al., 2008, McKenna and Higgins, 1997, Rosenbaum and Argon, 1979).
Behavioral economics, a field established on principles of psychology and economics, has extensively examined decision-making process in individuals with substance use disorder and mental illness (Amlung et al., 2019, Bickel et al., 2014). Delay discounting is a prominent behavioral economic measure used to assess the subjective change in the value of a reward as a function of time to its receipt (Madden & Bickel, 2010).
As a recent review by Amlung et al. (2019) states, higher delay discounting rates (i.e., propensity to choose smaller, sooner reward; discount future outcomes more) are associated with psychiatric disorders including depression, bipolar disorder, schizophrenia, borderline personality disorder, bulimia nervosa, and binge-eating disorder. A recent meta-analysis reported that stress was also associated with delay discounting with a moderate-large effect size (Fields, Lange, Ramos, Thamotharan, & Rassu, 2014). To our knowledge, the association between locus of control and delay discounting has not been examined.
Previous studies indicate that individuals with addiction and substance use disorders also report significantly higher rates of discounting (i.e., propensity to choose smaller, sooner reward; discount future outcomes more) compared to healthy controls across a number of substances (Amlung et al., 2017, Bickel et al., 2014), including: alcohol (Petry, 2001), cocaine (Coffey et al., 2003, Kirby and Petry, 2004), nicotine (Bickel et al., 1999), and opiates (Kirby et al., 1999, Madden et al., 1999). Delay discounting rates have also been positively associated with risk of substance use (MacKillop et al., 2011) and negatively associated with successful treatment outcomes (Sheffer et al., 2014, Sheffer et al., 2012, Stanger et al., 2012).
Stress, beliefs about external locus of control, and delay discounting have been associated with successful treatment outcomes in short-term recovery from smoking (Berg et al., 2010, Cohen and Lichtenstein, 1990). However, to our knowledge, the relationship between perceived stress, beliefs about locus of control, and delay discounting among individuals in recovery from substance use has not been previously examined.
In this study, we assessed the relationship between demographic characteristics, delay discounting (measured using an adjusting-amount delay discounting task), perceived stress and beliefs about locus of control among individuals in recovery from substance use to ascertain their relationship in individuals in recovery from substance use disorders. We chose to examine the relationship of age to these variables within our sample, as age is a construct related to recovery from substance use disorders as demonstrated by the phenomena of maturing out of addiction (Vergés et al., 2013, Waldorf, 1983, Waldorf and Biernacki, 1981). Data from these measures and demographic characteristics were collected from the International Quit and Recovery Registry (IQRR) (http://quitandrecovery.org), an online community designed to further understand the phenotype of recovery (see also Athamneh et al., 2019, Athamneh et al., 2017). We hypothesized that higher rates of discounting would be associated with higher levels of perceived stress, higher scores regarding beliefs about external locus of control (measured by the IPCS and the DRLOC), and a shorter time in self-reported recovery. Understanding the relationship between delay discounting, perceived stress, and beliefs about locus of control may help identify individuals in recovery who are at a greater risk of relapse.
2. Methodology
2.1. Participants
Participants were recruited through the IQRR. The IQRR was launched in 2011 and recruits individuals who are in self-reported recovery from at least one behavioral or substance addiction. The goal of the IQRR is to enhance our understanding of the recovery process and factors allowing individuals to overcome their addiction. Individuals in recovery from addiction who are interested in registering at the IQRR website are asked to provide an email address and contact information. In addition, members are asked to complete a survey including demographics, family history of addiction and history of substance use. Once an individual is registered, they are able to complete monthly research assessments. Each assessment completed rewards participants with a badge for their website profile and 100–1000 points (depending on the study) which are exchangeable for monetary rewards (100 points is $1.00).
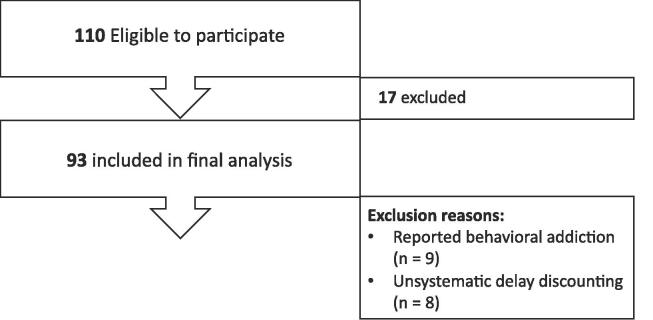
The present study was approved by the Institutional Review Board (IRB) at Virginia Polytechnic Institute and State University. Informed consent was implied by the completion and submission of the survey. One hundred twenty-one participants completed the study. Inclusion criteria for the present study required participants to be 18 years or older and be a member of the IQRR. Participants were excluded if they provided non-systematic delay discounting data (n = 8; Johnson & Bickel, 2008) and if reported a non-substance related primary addiction (n = 9; e.g., sexual activity, pornography, eating disorder, caffeine). Thus, the final sample included 93 participants (Fig. 1).
Fig. 1.
Study sample of respondents to the October 2018 Assessment of the International Quit and Recovery Registry (IQRR).
2.2. Study measures
Demographic data including questions on age, gender, race, ethnicity, annual income, education level, marital status, smoking status, time in recovery, and the primary addiction were collected. Primary addiction was determined by self-report using the question, “What is your primary addiction?” with the following choices: nicotine, alcohol, cannabis, opioids, cocaine, stimulants, prescription pain relievers, hallucinogens, dissociative anesthetics, tranquilizers/depressants, inhalants, caffeine, gambling, overeating, binge eating or other eating disorders, excessive shopping, excessive sexual activity, excessive video gaming, excessive viewing of pornography, and excessive preoccupation with activities on the internet. Examples were provided for each substance and behavior. Time in recovery was assessed by asking participants, “How long have you been in recovery from your primary addiction?” Participants then provided the amount of time they were in self-report recovery from addiction in years, months, and/or days.
Delay discounting was measured using an adjusting amount delay discounting task (Du, Green, & Myerson, 2002). In this task, participants are asked to choose between receiving a smaller, immediate reward (hypothetical monetary rewards) or a larger, delayed reward. The magnitude of the smaller, immediate reward is adjusted until its value is approximately equal to the value of the larger, delayed reward; this value is termed the indifference point at a specific delay. In this study, participants were asked to choose between a monetary reward available immediately or a $1000 available after a delay. Participants answered 6 choice trials for 6 different delays (1 day, 1 month, 6 months, 1 year, 2 years, and 5 years). Indifference points for each delay are plotted and a delay discounting curve is modeled using Mazur’s hyperbolic equation:
where V is the value of the delayed reward, A is the amount of the delayed reward, D is the delay, and k is a free parameter, the estimated index of discounting (Mazur, 1987). A larger k value represents higher discounting (i.e., propensity to choose smaller, sooner reward; discount future outcomes more). Values of k are natural log transformed (ln(k)) in order to normalize the data and stabilize the variance.
The Perceived Stress Scale (PSS) is a validated (Cohen, 1988, Cohen et al., 1983) 10 item scale that assesses the degree to which events in an individual’s life are appraised as stressful (Cohen et al., 1983). The questions of the PSS ask about thoughts and feelings over the past month and how unpredictable, uncontrollable, and overloaded individuals feel their lives are (Cohen et al., 1983). Individuals are asked to rate how often they felt over the past month on a 5-point Likert scale where 0 is never and 4 is very often. Responses to the 10 items are summed. The score for each participant is calculated to provide a perceived stress score, with higher scores indicating higher levels of perceived stress.
The Internality, Powerful Others, and Chance Scale (IPCS) is a 24-item scale comprised of three subscales: the Internality Scale, the Powerful Others Scale, and the Chance Scale. Each subscale contains 8 items and participants are asked to rank each item on a 7-point Likert Scale where −3 is strongly disagree and + 3 is strongly agree. Scores are added together for each subscale and then a constant of 24 is added so that all sum scores are positive values. The range for each subscale of the IPCS is 0 to 48, where higher scores indicate high expectations of control by the designated locus of control (i.e., internality, powerful others, or chance) (Levenson, 1981).
The Drug-Related Locus of Control Beliefs Scale (DRLOC) is a 16-item scale used to assess an individual’s belief about being in control in situations related to drug use (Ersche et al., 2012). The DRLOC has two subscales: Addiction Recovery, and Drug-Taking Decisions. Participants are presented with two statements regarding drug use and asked to choose which they most strongly agree with. Internal related beliefs are scored as 0, and external related beliefs are scored as 1. Scores are summed, with values closer to 1 representing higher beliefs in the external locus of control related to drugs.
2.3. Statistical analysis
First, univariate linear regression analyses were conducted to determine the relationship between delay discounting and each of the 7 study measures (i.e., the PSS, IPCS: Internality Scale, IPCS: Powerful Others Scale, IPCS: Chance Scale, DR-LOC: Total, DR-LOC: Addiction Recovery Scale, and the DR-LOC: Drug-Taking Decisions Scale). Demographics, in addition to ln(k), were included in a multivariate backwards stepwise regression (see Table 3 for a full list of included demographics). Race and ethnicity were not included in the regression model because our sample was 94.6% Caucasian and 95.7% non-Hispanic. All statistical analyses were conducted in R (R Core Team, 2020).
Table 3.
Results of stepwise regressions for the IPCS: Chance Scale and the Perceived Stress Scale. Note: final models for other scales did not include ln(k).
| IPCS: Chance Scale | Perceived Stress Scale | |
|---|---|---|
| Age | – | – |
| Education | – | – |
| Employment Status | – | – |
| Gender | – | – |
| Income | – | – |
| Ln(k) | F = 4.1503 (p = 0.0446) | F = 13.475 (p = 0.0004) |
| Primary Addiction | – | – |
| Time in Recovery | – | F = 8.470 (p = 0.0045) |
2.4. Mediation analyses
Mediation analyses were performed according to the Baron and Kenny method (Baron and Kenny, 1986, MacKinnon et al., 2007). Mediating effects require three linkages: i) that the independent variable (X) and dependent variable (Y) are significantly associated; ii) that X and the mediator variable (M) are significantly associated; and iii) that M significantly affects Y while controlling for X. If all three criteria are met, then the direct effect of X is compared to the total effect of X and M on Y. Two mediation analyses were performed to determine the effect of delay discounting (ln(k); M) on the relationship between levels of perceived stress (Y) and time in recovery (X1) or age (X2). Mediation analyses were structured in this order because (i) lower perceived stress has been associated with higher success in recovery, (ii) time in recovery and age are non-modifiable, and (iii) interventions exist which modify delay discounting. Mediation analyses were performed using the lavaan package in R (Rosseel, 2012). All results from mediation analyses were reported as standardized estimates.
3. Results
Of the 110 respondents of the survey, 93 participants met the inclusion criteria and were included in the final analysis (Fig. 1). Demographic characteristics from the 93 participants are reported in Table 1. The sample included 60 females (64.5%). The majority of participants received an Associate’s degree or higher (n = 58, 62.4%) and were working part or full time (n = 54, 58.1%). The most prevalent primary addiction reported was alcohol (n = 60, 64.5%), followed by opioids (n = 10, 10.8%) and stimulants (n = 9, 9.7%). Time in recovery was assessed through a self-report question that asked participants to type the number of years, months, and days they have been in recovery from their primary addiction. Total time in recovery is defined as the participant’s self-reported time in recovery calculated in years. The mean years in recovery for the study sample is 11.83 years. The mean ln(k) for participants in the study was −5.65, which translates to a half-life of 284.3 days (about 9.5 months) for $1000.
Table 1.
Demographic characteristics for the 93 participants recruited from the International Quit and Recovery Registry (IQRR).
| n | 93 |
|---|---|
| Age (mean (SD)) | 51.53 (12.54) |
| Gender = Female (%) | 60 (64.5) |
| Ethnicity = Not Hispanic (%) | 89 (95.7) |
| Race (%) | |
| White | 86 (94.6) |
| African American | 4 (4.3) |
| Mixed Race | 3 (3.2) |
| Education (%) | |
| Did not finish high school or receive GED | 1 (1.1) |
| Finished high school or received GED | 8 (8.6) |
| Some college with no degree | 26 (28.0) |
| Associate's or Bachelor's degree | 40 (43.0) |
| Advanced degree (e.g. Masters, Doctorate) | 18 (19.4) |
| Employment Status (%) | |
| Disability | 13 (14.0) |
| Homemaker | 3 (3.2) |
| Not working | 6 (6.5) |
| Retired | 17 (18.3) |
| Working full time | 44 (47.3) |
| Working part time | 10 (10.8) |
| Income (%) | |
| <$10,000 | 17 (18.1) |
| $10,000 - $25,000 | 17 (18.1) |
| $25,000 - $50,000 | 17 (18.1) |
| $50,000 - $100,000 | 22 (23.4) |
| > $100,000 | 13 (13.8) |
| Prefer not to say | 5 (5.3) |
| Did not respond | 2 (2.1) |
| Primary Addiction (%) | |
| Alcohol | 60 (64.5) |
| Cannabis | 5 (5.4) |
| Cocaine | 3 (3.2) |
| Nicotine | 3 (3.2) |
| Opioids | 10 (10.8) |
| Prescription Pain Relievers | 3 (3.2) |
| Stimulants | 9 (9.7) |
| Time in Recovery (years) (mean (SD)) | 11.84 (11.26) |
Results of univariate linear regressions are reported in Table 2. The PSS and the IPCS Chance Scale were significantly associated with delay discounting rates (adjusted R-squared = 0.1641, p < 0.0001; adjusted R-squared = 0.036, p = 0.037, respectively).
Table 2.
Results of univariate linear regressions with delay discounting rate, ln(k).
| Variable | Coefficient | P Value |
|---|---|---|
| DR-LOC: Decisions Scale | −0.001 | 0.908 |
| DR-LOC: Recovery Scale | 0.005 | 0.405 |
| DR-LOC: Total Score | 0.002 | 0.762 |
| IPCS: Chance Scale | 0.523 | 0.037 |
| IPCS: Internality Scale | −0.550 | 0.798 |
| IPCS: Powerful Others Scale | 0.422 | 0.138 |
| Perceived Stress Scale | 1.090 | < 0.0001 |
Results of the stepwise regressions are reported in Table 3. The final model for the PSS included time in recovery and ln(k), which both significantly predicted levels of perceived stress measured by the PSS. The final model for the IPCS: Chance scale only included ln(k), which significantly predicted beliefs in a chance locus of control measured by the IPCS: Chance Scale. Final models of stepwise regressions for all other scales did not include ln(k).
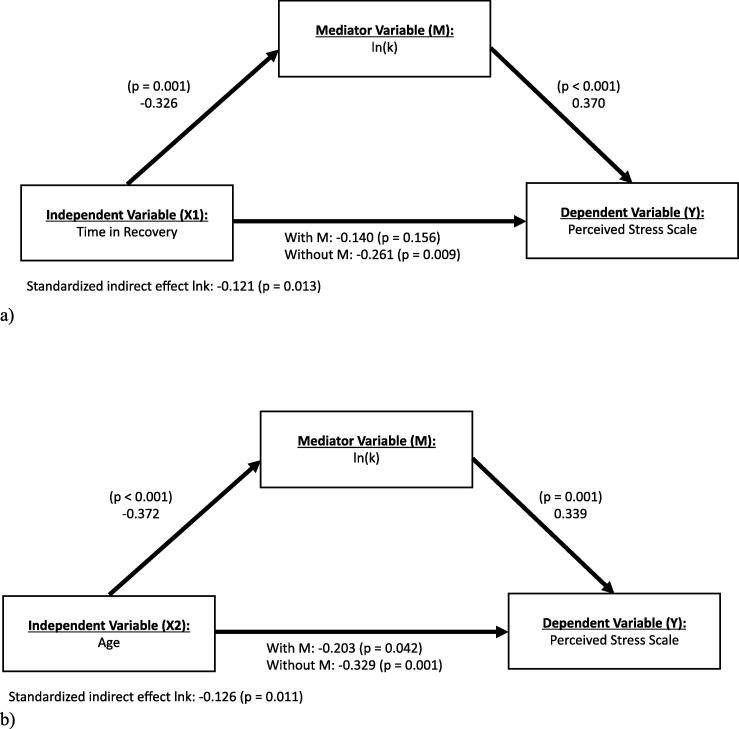
Two mediation analyses were conducted to explore how delay discounting rate influenced the relationship between perceived stress and two independent measures, age and time in recovery. Each component of the mediation model was assessed by multiple regression analyses outlined in Fig. 2 (A, B). First, the role of delay discounting rate (ln(k); M) in mediating the relationship between time in recovery (X1) and the Perceived Stress Scale (Y) was evaluated (Fig. 2A). Time in recovery was negatively associated with the Perceived Stress Scale (standardized ß = −0.261; p = 0.009) and negatively associated with lnk (standardized ß = −0.326; p = 0.001). Ln(k) was positively associated with the Perceived Stress Scale (standardized ß = 0.370; p < 0.001). Since both pathways between time in recovery and discounting rates and between discounting rates and the Perceived Stress Scale were significant, there was evidence for a mediating effect of lnk. Moreover, a significant indirect effect for rates of discounting on the relationship between time in recovery and the Perceived Stress Scale was identified (standardized indirect effect = -0.l21; p = 0.013). Overall, lnk represented 46.3% of the total effect between time in recovery and the Perceived Stress Scale.
Fig. 2.
Mediation analyses for the relationship between independent variables and perceived stress as mediated by delay discounting rate (ln(k)). Panel (A) depicts mediation analysis with time in recovery as the independent variable (X1). Panel (B) depicts mediation analysis with age as the independent variable (X2). Standardized ß estimates of the linear regression between each set of variables are depicted along the arrows. Note panels (A) and (B) represent 2 separate mediation analyses, not 1 analysis with multiple mediators.
Second, the role of delay discounting rate (ln(k); M) in mediating the relationship between age (X2) and the Perceived Stress Scale (Y) was evaluated (Fig. 2B). Age was negatively associated with the Perceived Stress Scale (standardized ß = −0.329; p = 0.001) and negatively associated with lnk (standardized ß = −0.372; p < 0.001). Ln(k) was positively correlated with the Perceived Stress Scale (standardized ß = 0.339; p = 0.001). Since both pathways between age and ln(k) and between ln(k) and the Perceived Stress Scale were significant, there was evidence for a mediating effect of ln(k). Moreover, a significant indirect effect for ln(k) on the relationship between age and the Perceived Stress Scale was identified (standardized indirect effect = -0.l26; p = 0.011). Overall, lnk represented 38.3% of the total effect between age and the Perceived Stress Scale.
4. Discussion
In this study, for the first time we examined the relationship of delay discounting rates with perceived stress and beliefs about locus of control among individuals in recovery from addiction. Delay discounting rate was a significant predictor of both perceived stress, measured by the Perceived Stress Scale, and beliefs about a chance locus of control, measured by the IPCS: Chance subscale, in this sample. Higher rates of delay discounting (i.e., greater propensity to choose smaller, sooner reward; discount future outcomes more) were associated with higher perceived stress levels and higher levels of beliefs about a chance locus of control. In addition, in the current study delay discounting mediated the relationships between time in recovery and perceived stress and age and perceived stress. We did not find a significant association between delay discounting and the IPCS Internality subscale, the IPCS: Powerful Others subscale, or the DRLOC. Below, we discuss these findings in more detail.
Overall, the current findings of significant association between time in recovery and perceived stress with delay discounting accounting for 46.3% of the total effect of time in recovery on perceived stress is consistent with previous research. Our findings are congruent with previous studies indicating that recovery length predicts stress levels in individuals in recovery from crack and heroin over a one year recovery period (Laudet, 2008). We report, consistent with Maleza (2019), that higher rates of delay discounting were associated with higher perceived stress levels. Here, we extend the literature to suggest that one’s future valuation plays an important role in the association between time in recovery and one’s perceived stress among individuals in recovery from SUD.
In the present study, age was significantly associated with levels of perceived stress and with discounting rates. The relationship between age and perceived stress was mediated by delay discounting rate (ln(k)), with significant indirect effects that accounted for 38.3% of the total effect of age on perceived stress. These results are consistent with previous studies that report that delay discounting rates typically decrease with age through adulthood (Green et al., 1994, Harrison et al., 2002, Steinberg et al., 2009) and may increase with advances into older adulthood (Göllner et al., 2017, Read and Read, 2004). These age-related results support the “maturing out” hypothesis (Dawson et al., 2006, Jochman and Fromme, 2010, Labouvie, 1996, Vergés et al., 2013, Waldorf, 1983, Waldorf and Biernacki, 1981), where older individuals report lower rates of delay discounting and lower levels of perceived stress, perhaps aiding in their recovery from substance use.
In the current study, delay discounting rate was significantly associated with beliefs about a chance locus of control (i.e., higher beliefs about chance affecting their experiences and outcomes). Higher rates of delay discounting were associated with higher levels of beliefs about a chance locus of control (IPCS: Chance Scale). One potential explanation of the significant association between DD and the IPCS Chance subscale may be explained partially by the temporal window. Participants with higher scores on the Chance subscale have higher agreement with items that relate to planning ahead and future consequences (e.g., Item 14: “It’s not always wise for me to plan too far ahead because many things turn out to be a matter of good or bad fortune.”). The IPCS includes the Internality, the Powerful Others, and the Chance subscales and assesses whether individuals believe events occur due to their own behaviors, or due to external factors like fate, chance, or individuals with more power. Beliefs about external loci of control, or the belief that individuals do not have control over their own lives, have been reported in a number of psychiatric disorders and have been associated with increased risk of substance use (Bearinger and Blum, 1997, Costello, 1982, Frazier et al., 2011, Gregor et al., 2008, Levenson, 1973, McKenna and Higgins, 1997, Rabani Bavojdan et al., 2011, Rosenbaum and Argon, 1979, Sheffer et al., 2012). To our knowledge, the IPCS Scale has not been analyzed in a context of behavioral economics and delay discounting before; evaluation of an externally focused locus of control has been done primarily using the Rotter’s Locus of Control Scale (Sheffer et al., 2014). Investigating the relationship between the IPCS and delay discounting in a sample of individuals still using substances or individuals with shorter durations of recovery may be warranted.
Contrary to our initial hypothesis, discounting rates were not significantly associated with DRLOC. The DRLOC assesses an individual’s belief about being in control in situations related to drug use (Ersche et al., 2012). The current study is the first to investigate the association between DRLOC scale and delay discounting. Previous findings regarding the association between DRLOC subscales and assessments of substance use are mixed. On one hand, a study by Ersche et al. (2012) indicated that individuals in recovery from substance use report higher levels of internal scores in DRLOC recovery subscale when compared to non-substance using controls; On the other hand, Savulich et al. (2017) indicated no significant difference in DRLOC scores between healthy controls, individuals who use alcohol, and individuals who use drugs and alcohol. Future research replicating the current study including measures of substance use, and investigating the association between the DRLOC in a behavioral economic context between substance using, recovery from substance use, and never substance using populations may be needed to better understand these associations.
The current study presents data from individuals in recovery from a number of substances. These results present opportunities for future investigation. Further research should analyze the ability of delay discounting to predict other factors that are known to be associated with psychiatric disorders and substance use disorders such as stressful life events or family history of psychiatric conditions. Similarly, more research is needed to elucidate the relationship of changes in delay discounting with changes in levels of perceived stress and beliefs about locus of control over time. These results do not reduce the possibility that other factors contribute to time in recovery’s effects on perceived stress; however, it does support that delay discounting rate can help explain the relationship between time in recovery from substance use disorder and perceived stress. These findings support delay discounting as a tool to identify subgroups of individuals in recovery from substance use disorders that are at higher risk of relapse and/or unsuccessful treatment.
While the present study examines a unique population of individuals across the time course of recovery from substance use disorders, several limitations need to be addressed. First, individuals who choose to participate in the IQRR are in self-reported recovery, must use technology, and must have an email address to participate. Individuals who choose to join the IQRR are self-selecting, suggesting potential bias in our sample. Second, while we examined the relationship between delay discounting, perceived stress, and beliefs about loci of control, several variables were not assessed that could affect this relationship. For example, data were not collected regarding other psychiatric disorders, severity of substance use the participants were in recovery from, or coping mechanisms and support systems. Since these variables may affect the relationship between delay discounting and perceived stress or beliefs about locus of control, future research may be needed to determine their effects. Third, the current study asked individuals to self-report how long they have been in recovery from their primary addiction. However, the definition of recovery was not specified. As participants may have different definitions of recovery, using self-reported definition of recovery instead of standard measures to assess the recovery status (e.g., DSM-5, QoL, etc; Betty Ford Institute Consensus Panel …) is a limitation of the present study. Future studies assessing those associations among individuals in recovery as determined by the new evolving definitions (Ashford et al., 2019, Betty Ford Institute Consensus Panel, 2007, Kelly & Hoeppner, 2015, Laudet, 2008) is warranted.
5. Conclusion
The present study expands on research regarding delay discounting and its relationship to substance use and recovery. We report that delay discounting predicts levels of perceived stress and beliefs about chance locus of control in individuals in recovery from substance use disorders. These results may help identify and target subgroups of individuals in recovery from substance use disorder that need different, unique, or more intensive treatments. Future research examining the relationship between delay discounting, perceived stress, and beliefs about a chance locus of control in individuals with other comorbid psychiatric disorders may be warranted.
CRediT authorship contribution statement
Devin C. Tomlinson: Software, Formal analysis, Writing - original draft. Allison N. Tegge: Software, Validation, Writing - review & editing. Liqa N. Athamneh: Project administration, Writing - review & editing. Warren K. Bickel: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
Although the following activities/relationships do not create a conflict of interest pertaining to this manuscript, in the interest of full disclosure, Dr. Bickel would like to report the following: W. K. Bickel is a principal of HealthSim, LLC; Notifius, LLC; BEAM Diagnostics, Inc.; and Red 5 Group, LLC. In addition, he serves on the scientific advisory board for Sober Grid, Inc. and is a consultant for Alkermes, Inc. and Sandoz Inc. None of the other authors have any conflict of interest.
References
- Abuse, S. (2018). Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Rockville, MD: Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration.
- Amlung M., Marsden E., Holshausen K., Morris V., Patel H., Vedelago L.…McCabe R.E. Delay Discounting as a Transdiagnostic Process in Psychiatric Disorders: A Meta-analysis. JAMA Psychiatry. 2019 doi: 10.1001/jamapsychiatry.2019.2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M., Vedelago L., Acker J., Balodis I., MacKillop J. Steep delay discounting and addictive behavior: A meta-analysis of continuous associations. Addiction. 2017;112(1):51–62. doi: 10.1111/add.13535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashford R.D., Brown A., Brown T., Callis J., Cleveland H.H., Eisenhart E.…Whitney Defining and operationalizing the phenomena of recovery: a working definition from the recovery science research collaborative. Addiction Research & Theory. 2019;27(3):179–188. [Google Scholar]
- Athamneh L.N., DeHart W.B., Pope D., Mellis A.M., Snider S.E., Kaplan B.A., Bickel W.K. The phenotype of recovery III: Delay discounting predicts abstinence self-efficacy among individuals in recovery from substance use disorders. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2019;33(3):310–317. doi: 10.1037/adb0000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athamneh L.N., Stein J.S., Quisenberry A.J., Pope D., Bickel W.K. The association between parental history and delay discounting among individuals in recovery from addiction. Drug and Alcohol Dependence. 2017;179:153–158. doi: 10.1016/j.drugalcdep.2017.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bearinger, L. H., & Blum, R. W. (1997). The utility of locus of control for predicting adolescent substance use. In Research in Nursing & Health (Vol. 20, Issue 3, pp. 229–245). https://doi.org/3.0.co;2-k“>10.1002/(sici)1098-240x(199706)20:3<229::aid-nur6>3.0.co;2-k. [DOI] [PubMed]
- Berg C.J., Thomas J.L., Guo H., An L.C., Okuyemi K.S., Collins T.C., Ahluwalia J.S. Predictors of smoking reduction among Blacks. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2010;12(4):423–431. doi: 10.1093/ntr/ntq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betty Ford Institute Consensus Panel What is recovery? A working definition from the Betty Ford Institute. Journal of Substance Abuse Treatment. 2007;33(3):221–228. doi: 10.1016/j.jsat.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Bickel W.K., Johnson M.W., Koffarnus M.N., MacKillop J., Murphy J.G. The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annual Review of Clinical Psychology. 2014;10:641–677. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey S.F., Gudleski G.D., Saladin M.E., Brady K.T. Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Experimental and Clinical Psychopharmacology. 2003;11(1):18–25. doi: 10.1037//1064-1297.11.1.18. [DOI] [PubMed] [Google Scholar]
- Cohen, S. (1988). Perceived stress in a probability sample of the United States. https://psycnet.apa.org/record/1988-98838-002.
- Cohen S., Janicki-Deverts D., Miller G.E. Psychological stress and disease. JAMA: The Journal of the American Medical Association. 2007;298(14):1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. https://www.ncbi.nlm.nih.gov/pubmed/6668417 [PubMed] [Google Scholar]
- Cohen, S., Kamarck, T., Mermelstein, R., & Others. (1994). Perceived stress scale. Measuring Stress: A Guide for Health and Social Scientists, 10. https://www.northottawawellnessfoundation.org/wp-content/uploads/2018/04/PerceivedStressScale.pdf.
- Cohen, S., Kessler, R. C., Gordon, L. U., & Others. (1995). Strategies for measuring stress in studies of psychiatric and physical disorders. Measuring Stress: A Guide for Health and Social Scientists, 3–26. https://books.google.com/books?hl=en&lr=&id=2S3RCwAAQBAJ&oi=fnd&pg=PA3&dq=cohen+kessler+gordon&ots=o-0CoJ0oah&sig=HevAiYFZ-0XbHv-M-EdKu17hltM.
- Cohen S., Lichtenstein E. Perceived stress, quitting smoking, and smoking relapse. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 1990;9(4):466–478. doi: 10.1037//0278-6133.9.4.466. [DOI] [PubMed] [Google Scholar]
- Costello, E. J. (1982). Locus of control and depression in students and psychiatric outpatients. Journal of Clinical Psychology, 38(2), 340–343. https://doi.org/3.0.co;2-d“>10.1002/1097-4679(198204)38:2<340::aid-jclp2270380220>3.0.co;2-d. [DOI] [PubMed]
- Dawson D.A., Grant B.F., Stinson F.S., Chou P.S. Maturing out of alcohol dependence: The impact of transitional life events. Journal of Studies on Alcohol. 2006;67(2):195–203. doi: 10.15288/jsa.2006.67.195. [DOI] [PubMed] [Google Scholar]
- Du W., Green L., Myerson J. Cross-Cultural Comparisons of Discounting Delayed and Probabilistic Rewards. The Psychological Record. 2002;52(4):479–492. doi: 10.1007/BF03395199. [DOI] [Google Scholar]
- Ersche K.D., Turton A.J., Croudace T., Stochl J. Who Do You Think Is in Control in Addiction? A Pilot Study on Drug-related Locus of Control Beliefs. Addictive Disorders & Their Treatment. 2012;11(4):173–223. doi: 10.1097/ADT.0b013e31823da151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields S.A., Lange K., Ramos A., Thamotharan S., Rassu F. The relationship between stress and delay discounting: A meta-analytic review. Behavioural Pharmacology. 2014;25(5–6):434–444. doi: 10.1097/FBP.0000000000000044. [DOI] [PubMed] [Google Scholar]
- Frazier P., Keenan N., Anders S., Perera S., Shallcross S., Hintz S. Perceived past, present, and future control and adjustment to stressful life events. Journal of Personality and Social Psychology (Vol. 2011;100(4):749–765. doi: 10.1037/a0022405. [DOI] [PubMed] [Google Scholar]
- Ghorbani N., Krauss S.W., Watson P.J., Lebreton D. Relationship of perceived stress with depression: Complete mediation by perceived control and anxiety in Iran and the United States. International Journal of Psychology: Journal International de Psychologie. 2008;43(6):958–968. doi: 10.1080/00207590701295264. [DOI] [PubMed] [Google Scholar]
- Göllner L.M., Ballhausen N., Kliegel M., Forstmeier S. Delay of Gratification, Delay Discounting and their Associations with Age, Episodic Future Thinking, and Future Time Perspective. Frontiers in Psychology. 2017;8:2304. doi: 10.3389/fpsyg.2017.02304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L., Fry A.F., Myerson J. Discounting of Delayed Rewards: A Life-Span Comparison. Psychological Science. 1994;5(1):33–36. doi: 10.1111/j.1467-9280.1994.tb00610.x. [DOI] [Google Scholar]
- Gregor K., Zvolensky M., McLeish A., Bernstein A., Morissette S. Anxiety sensitivity and perceived control over anxiety-related events: Associations with smoking outcome expectancies and perceived cessation barriers among daily smokers. Nicotine & Tobacco Research. 2008;10(4):627–635. doi: 10.1080/14622200801978706. [DOI] [PubMed] [Google Scholar]
- Harrison G.W., Lau M.I., Williams M.B. Estimating individual discount rates in Denmark: A field experiment. The American Economic Review. 2002;92(5):1606–1617. doi: 10.1257/000282802762024674. [DOI] [Google Scholar]
- Herbert J. Fortnightly review: Stress, the brain, and mental illness. BMJ. 1997;315(7107):530–535. doi: 10.1136/bmj.315.7107.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J.P. Introduction: Stress and neurological disease. Experimental Neurology. 2012;233(1):1–2. doi: 10.1016/j.expneurol.2011.12.041. [DOI] [PubMed] [Google Scholar]
- Jochman, K. A., & Fromme, K. (2010). Maturing out of substance use: The other side of etiology. In L. Scheier (Ed.), Handbook of drug use etiology: Theory, methods, and empirical findings , (pp (Vol. 689, pp. 565–578). American Psychological Association, xxvi. https://psycnet.apa.org/fulltext/2009-19890-030.pdf.
- Kassel J.D., Stroud L.R., Paronis C.A. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin. 2003;129(2):270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Kelly T.M., Daley D.C. Integrated treatment of substance use and psychiatric disorders. Social Work in Public Health. 2013;28(3–4):388–406. doi: 10.1080/19371918.2013.774673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly J.F., Hoeppner B. A biaxial formulation of the recovery construct. Addiction Research & Theory. 2015;23(1):5–9. [Google Scholar]
- Kirby K.N., Petry N.M. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99(4):461–471. doi: 10.1111/j.1360-0443.2003.00669.x. [DOI] [PubMed] [Google Scholar]
- Kirby K.N., Petry N.M., Bickel W.K. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology. General. 1999;128(1):78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Labouvie E. Maturing out of Substance Use: Selection and Self-Correction. Journal of Drug Issues. 1996;26(2):457–476. doi: 10.1177/002204269602600208. [DOI] [Google Scholar]
- Laudet A.B. The road to recovery: Where are we going and how do we get there? Empirically driven conclusions and future directions for service development and research. Substance Use & Misuse. 2008;43(12–13):2001–2020. doi: 10.1080/10826080802293459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levenson H. Multidimensional locus of control in psychiatric patients. Journal of Consulting and Clinical Psychology. 1973;41(3):397–404. doi: 10.1037/h0035357. [DOI] [PubMed] [Google Scholar]
- Levenson, H. (1981). DIFFERENTIATING AMONG INTERNALITY, POWERFUL OTHERS, AND CHANCE. In Research with the Locus of Control Construct (pp. 15–63). https://doi.org/10.1016/b978-0-12-443201-7.50006-3.
- Lijffijt M., Hu K., Swann A.C. Stress modulates illness-course of substance use disorders: A translational review. Frontiers in Psychiatry / Frontiers Research Foundation. 2014;5:83. doi: 10.3389/fpsyt.2014.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J., Amlung M.T., Few L.R., Ray L.A., Sweet L.H., Munafò M.R. Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology. 2011;216(3):305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D.P., Fairchild A.J., Fritz M.S. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden G.J., Bickel W.K. Impulsivity: The behavioral and neurological science of discounting. American Psychological Association. 2010 https://psycnet.apa.org/psycinfo/2009-18177-000/ [Google Scholar]
- Madden G.J., Bickel W.K., Jacobs E.A. Discounting of delayed rewards in opioid-dependent outpatients: Exponential or hyperbolic discounting functions? Experimental and Clinical Psychopharmacology. 1999;7(3):284–293. doi: 10.1037//1064-1297.7.3.284. [DOI] [PubMed] [Google Scholar]
- Malesza M. Stress and delay discounting: The mediating role of difficulties in emotion regulation. Personality and Individual Differences. 2019;144:56–60. doi: 10.1016/j.paid.2019.02.035. [DOI] [Google Scholar]
- Mazur, J. E. (1987). An adjusting procedure for studying delayed reinforcement. Commons, ML. ; Mazur, JE. ; Nevin, JA, 55–73. https://books.google.com/books?hl=en&lr=&id=1q5mAgAAQBAJ&oi=fnd&pg=PA55&dq=mazur+1987+adjusting&ots=eNqCSNtc8y&sig=aRZsB5M48ERog6_iJl4sPYBlVak.
- McKenna K., Higgins H. Factors influencing smoking cessation in patients with coronary artery disease. Patient Education and Counseling. 1997;32(3):197–205. doi: 10.1016/s0738-3991(97)00042-6. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2018). Common Comorbidities with Substance Use Disorders. Retrieved from: https://www.drugabuse.gov/publications/research-reports/common-comorbidities-substance-use-disorders/part-1-connection-between-substance-use-disorders-mental-illness. [PubMed]
- Petry N.M. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology. 2001;154(3):243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Rabani Bavojdan M., Towhidi A., Rahmati A. The Relationship between Mental Health and General Self-Efficacy Beliefs, Coping Strategies and Locus of Control in Male Drug Abusers. Addiction & Health. 2011;3(3–4):111–118. https://www.ncbi.nlm.nih.gov/pubmed/24494125 [PMC free article] [PubMed] [Google Scholar]
- Read D., Read N.L. Time discounting over the lifespan. Organizational Behavior and Human Decision Processes. 2004;94(1):22–32. doi: 10.1016/j.obhdp.2004.01.002. [DOI] [Google Scholar]
- Rosenbaum, M., & Argon, S. (1979). Locus of control and success in self-initiated attempts to stop smoking. Journal of Clinical Psychology, 35(4), 870–872. https://onlinelibrary.wiley.com/doi/abs/10.1002/1097-4679(197910)35:4%3C870::AID-JCLP2270350437%3E3.0.CO;2-D?casa_token=KIjXQ-js5scAAAAA:RkbR9WEy2Nf5Gt6yKXq-or8aC1cSCfwVlQ6a8rgopjazZsSUo5c3ZYrJiGwkAg7AWel3DzgojZWCNA. [DOI] [PubMed]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A language and environment for statistical computing. URL: Https://www.R-project.org/ [Google Scholar]
- Ross S., Peselow E. Co-occurring psychotic and addictive disorders: Neurobiology and diagnosis. Clinical Neuropharmacology. 2012;35(5):235–243. doi: 10.1097/WNF.0b013e318261e193. [DOI] [PubMed] [Google Scholar]
- Rosseel Y. lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software. 2012;48(2):1–36. http://www.jstatsoft.org/v48/i02/ [Google Scholar]
- Savulich G., Riccelli R., Passamonti L., Correia M., Deakin J.F.W., Elliott R.…Ersche K.D. Effects of naltrexone are influenced by childhood adversity during negative emotional processing in addiction recovery. Translational Psychiatry. 2017;7(3) doi: 10.1038/tp.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffer C.E., Christensen D.R., Landes R., Carter L.P., Jackson L., Bickel W.K. Delay discounting rates: A strong prognostic indicator of smoking relapse. Addictive Behaviors. 2014;39(11):1682–1689. doi: 10.1016/j.addbeh.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffer, C., MacKillop, J., McGeary, J., Landes, R., Carter, L., Yi, R., Jones, B., Christensen, D., Stitzer, M., Jackson, L., & Others. (2012). Delay discounting, locus of control, and cognitive impulsiveness independently predict tobacco dependence treatment outcomes in a highly dependent, lower socioeconomic group of smokers. The American Journal on Addictions / American Academy of Psychiatrists in Alcoholism and Addictions, 21(3), 221–232. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1521-0391.2012.00224.x. [DOI] [PMC free article] [PubMed]
- Stanger C., Ryan S.R., Fu H., Landes R.D., Jones B.A., Bickel W.K., Budney A.J. Delay discounting predicts adolescent substance abuse treatment outcome. Experimental and Clinical Psychopharmacology. 2012;20(3):205–212. doi: 10.1037/a0026543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L., Graham S., O’Brien L., Woolard J., Cauffman E., Banich M. Age differences in future orientation and delay discounting. Child Development. 2009;80(1):28–44. doi: 10.1111/j.1467-8624.2008.01244.x. [DOI] [PubMed] [Google Scholar]
- Vergés A., Haeny A.M., Jackson K.M., Bucholz K.K., Grant J.D., Trull T.J.…Sher K.J. Refining the notion of maturing out: Results from the national epidemiologic survey on alcohol and related conditions. American Journal of Public Health. 2013;103(12):e67–e73. doi: 10.2105/AJPH.2013.301358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldorf D. Natural Recovery from Addiction: Some Social-Psychological Processes of Untreated Recovery. Journal of Drug Issues. 1983;13(2):237–280. doi: 10.1177/002204268301300205. [DOI] [Google Scholar]
- Waldorf D., Biernacki P. The Natural Recovery from Opiate Addiction: Some Preliminary Findings. Journal of Drug Issues. 1981;11(1):61–74. doi: 10.1177/002204268101100104. [DOI] [Google Scholar]