Abstract
Background:
There are little data on the psychosocial wellbeing of hip fracture patients. Previous studies lacked a control group to isolate the impact of hip fracturs from general aging. We sought to overcome these limitations and quantify the impact of hip fractures on psychosocial wellbeing.
Methods:
We identified a cohort 65 years and older who were driving and mobile from the National Health and Aging Trends Study. Participants with exactly one hip fracture between 2011 and 2017 were isolated and their outcomes post hip fracture were compared to controls via multivariate logistic regression.
Results:
Hip fracture patients reported a significant decrease in driving frequency and mobility in the first year post fracture, along with an increase in depressive symptomatology and decreased participation in activities. Measures of mobility and activities among survivors returned to peer group levels within two years. A larger social network was associated with improved outcomes.
Discussion:
Hip fracture survivors experience significant declines in function and wellbeing in the first year following a hip fracture compared to peers. While mortality is high, surviving patients experience measurable gains in function and well-being in the three years after fracture. These data aid surgeons in counselling families and patients after hip fracture.
Level of Evidence:
Level I – Prognostic study: Inception cohort study
Introduction
Every year, over 300,000 individuals in the United States alone are hospitalized after sustaining hip fractures.1 Despite a decline in the age adjusted incidence of hip fractures over the last two decades, the public health burden associated with hip fractures will certainly increase in coming years as the proportion of the population age 65 and older rises.2, 3
Hip fracture patients and their families frequently ask about expectations for the recovery process and the likelihood that they will recover their pre-fracture level of function. While some facets of this process are well studied, many questions remain unanswered. Several studies have documented significant hip fracture related mortality, studied declines in physical capacity post hip fracture, and noted the impact that various rehabilitative strategies have on recovery after hip fracture.5-11 Few have studied whether hip fracture patients suffer long-term psychosocial limitations relative to their peers, or estimated the proportion of hip fracture patients who regain full functionality in the months and years after their release from the hospital.12 Of those that have, many were restricted to studying subpopulations, increasing the variance in the results reported.6, 12-19 Some required patients to estimate their pre-fracture levels of function retrospectively, which is associated with significant risk of bias.12, 15, 20, 21 Others were unable to create a matched non-hip fracture control population to isolate the influence of hip fracture from limitations more generally associated with advancing age.22-24
To overcome these limitations and supplement the existing body of literature, we conducted an analysis of trends post hip fracture on a nationally representative sample of subjects aged 65 and older derived from the National Health and Aging Trends Study (NHATS). The NHATS survey is a prospective observational cohort study developed by an interdisciplinary team of researchers in geriatric medicine, epidemiology, and economics and has been featured in several recent studies examining various aspects of the aging process.25-27 Participants are a national representative sample of US persons age 65 and older who have been followed annually since 2011. NHATS data is gathered by trained interviewers who collect detailed information about subject experiences via structured in-person interviews.25 Data collected include information on cognitive and physical capacity, activities of daily living, health status. We hypothesized that that hip fracture patients would experience functional and emotional declines in the year immediately following the incident. We expected to see hip fracture survivors make gradual improvements in these metrics over time. Based on prior literature,7, we also studied the impact of social network size on outcomes post hip fracture.
Methods
Survey data between 2011–2016 was extracted from the NHATS database. Those that sustained exactly one hip fracture between 2011 and 2016 were isolated, and individuals who had a prior history of hip fracture (before intake in 2011) or sustained multiple fractures in the period of interest were removed from the set. In addition, we removed patients who were not driving or leaving the house prior to injury.
Odds ratios were calculated via multivariate logistic regression and were adjusted for age, sex, race, education level, income, response type (proxy vs. sample person), residence in a metropolitan/non-metropolitan region, social network size, heart attack status, heart disease status, lung disease status, diabetes status, stroke status, Alzheimer’s/dementia status, and cancer status. Data regarding the severity of pre-injury comorbidities was not available. Odds ratios were adjusted for region of residence to standardize for disparities in the necessity/availability of public transportation.
Outcome frequencies among hip fracture survivors one, two, and three years after hip fracture were recorded alongside outcome frequencies in the control groups at the same timepoints. If a death occurred, subjects were censored after mortality. The outcomes - mobility, driving frequency, symptomatology of depression, ability to participate in activities, and the ability to work/volunteer – were grouped into binary categories wherever necessary to facilitate comparison. For example, those subjects who reported rarely driving (≤ one day per week) and those who reported never driving were grouped and separated from those who reported driving on some days (≥ two days per week), driving on most days (four to six days per week), and those who reported driving nearly every day.
To examine the impact of patient social network size on recovery following hip fracture, we separated hip fracture survivors with large social networks (≥ 3 people) from those with small social networks (≤ 2 people).
Results
The hip fracture incidence rate in the NHATS sample was 1.3% per year, and the mortality rate one year post hip fracture in the NHATS sample was 20.2% for men and 17.3% for women. There were 82 hip fracture patients and 4,495 control subjects analyzed in this study. Demographics were similar between hip fracture and control patients, except that the hip fracture patients were slightly older and more likely to have dementia (Table 1). In the first year after hip fracture 76% of surviving hip fracture patients reported driving regularly compared to 95% of control subjects (AOR: 0.18, 95% CI: 0.09 – 0.35) (Figure 1). There was no statistically significant difference in driving frequency between surviving subjects in the groups two, or three years post fracture. Similarly, in the first year after hip fracture 86% of surviving hip fracture patients reported leaving the house regularly compared to 99% of control subjects (AOR: 0.13, 95% CI: 0.05 – 0.33) (Figure 2). There was also no statistically significant difference in mobility between surviving subjects in the groups two, or three years post fracture. It is important to note that all subjects included in this study were driving and leaving the house regularly at intake irrespective of hip fracture status later.
Table 1:
Sample Demographics
| HF | % of HF Sample |
No HF |
% of Non - HF Sample |
p value | |
|---|---|---|---|---|---|
| Age (years) | < 0.0001 | ||||
| 65-69 | 13 | 16 | 1101 | 25 | |
| 70-74 | 11 | 13 | 1112 | 25 | |
| 75-79 | 13 | 16 | 953 | 21 | |
| 80-84 | 22 | 27 | 802 | 18 | |
| 85-89 | 18 | 22 | 373 | 8 | |
| 90+ | 5 | 6 | 154 | 3 | |
| Sex | 0.2909 | ||||
| Male | 47 | 57 | 2312 | 51 | |
| Female | 35 | 42 | 2183 | 48 | |
| Race/Ethnicity | 0.7616 | ||||
| White | 66 | 80 | 3425 | 76 | |
| Black | 11 | 13 | 807 | 18 | |
| Hispanic | 2 | 2 | 95 | 2 | |
| Other | 3 | 4 | 168 | 4 | |
| Education | 0.3118 | ||||
| Less than High School | 19 | 23 | 792 | 18 | |
| High School Degree | 18 | 22 | 1240 | 28 | |
| More than High School Degree | 45 | 55 | 2463 | 54 | |
| Proxy Respondent | |||||
| Not a Proxy Respondent | 82 | 100 | 4495 | 100 | |
| Proxy Respondent | 0 | 0 | 0 | 0 | |
| Region of Residence | 0.1522 | ||||
| Metropolitan | 70 | 85 | 3545 | 70 | |
| Non-metropolitan | 12 | 15 | 950 | 21 | |
| Heart Attack | 0.0923 | ||||
| Yes | 4 | 5 | 96 | 2 | |
| No | 78 | 95 | 4399 | 98 | |
| Heart Disease | 0.0158 | ||||
| Yes | 24 | 30 | 842 | 19 | |
| No | 58 | 70 | 3653 | 81 | |
| Diabetes | 0.8196 | ||||
| Yes | 21 | 26 | 1102 | 25 | |
| No | 61 | 74 | 3393 | 75 | |
| Lung Disease | |||||
| Yes | 14 | 17 | 710 | 16 | 0.7533 |
| No | 68 | 83 | 3785 | 84 | |
| Stroke | 0.2567 | ||||
| Yes | 3 | 4 | 86 | 2 | |
| No | 79 | 96 | 4409 | 98 | |
| Alzheimer's/Dementia | < 0.0001 | ||||
| Yes | 7 | 9 | 68 | 2 | |
| No | 75 | 91 | 4427 | 98 | |
| Cancer | 0.3112 | ||||
| Yes | 7 | 9 | 264 | 6 | |
| No | 75 | 91 | 4231 | 94 | |
| Social Network Size | 0.0490 | ||||
| Large (≥ 3 Individuals) | 31 | 38 | 1256 | 28 | |
| Small (≤ 2 Individuals) | 51 | 62 | 3239 | 72 |
Figure 1:
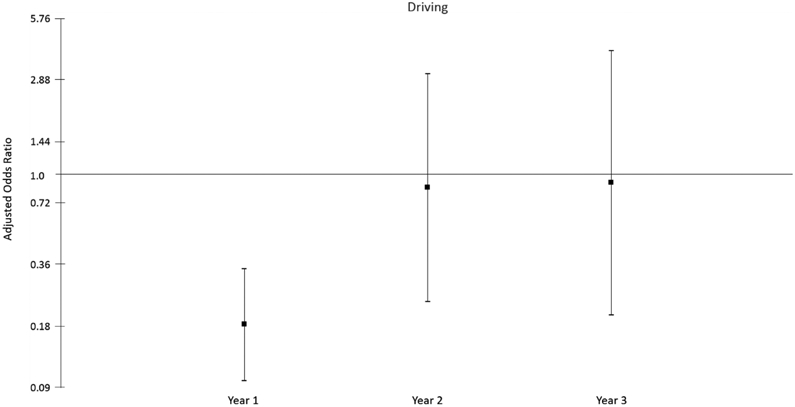
Odds of Driving Frequently – Hip fracture patients reported lower odds of driving frequently within the first-year post fracture (OR: 0.184, 95% CI: 0.098 - 0.346). No significant effect could be detected two (OR: 0. 863, 95% CI: 0.239- 3.114) or three years post fracture (OR: 0.910, 95% CI: 0.205 - 4.041).
Figure 2:
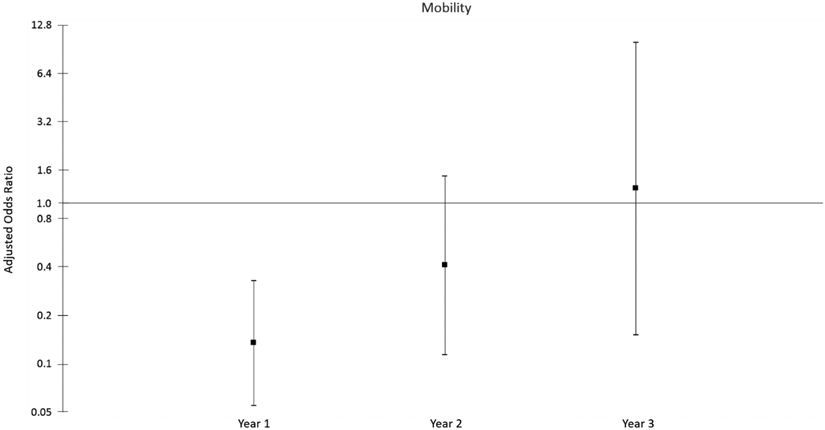
Odds of Leaving the House Frequently – Hip fracture patients reported lower odds of leaving the house frequently within the first-year post fracture (OR: 0.135, 95% CI: 0.055 – 0.331). No significant effect could be detected two (OR: 0.411, 95% CI: 0.411 - 1.477) or three years post fracture (OR: 1.235, 95% CI: 0.152 – 10.039).
In the first year post hip fracture, 44% of surviving hip fracture subjects reported being kept from their favorite activity by their health compared to 18% of control subjects (AOR: 4.09, 95% CI: 2.55 – 6.53) (Figure 3). Surviving hip fracture patients were more likely to be kept from their favorite activities two years post fracture (OR: 1.959, 95% CI: 1.019 – 3.766) (Figure 3). In the first year after hip fracture 17% of surviving hip fracture patients reported working/volunteering in the last month compared to 44% of control subjects (AOR: 0.35, 95% CI: 0.19 – 0.63) (Figure 4). There was no statistically significant difference in working/volunteering rates between the groups two, or three years post fracture.
Figure 3:
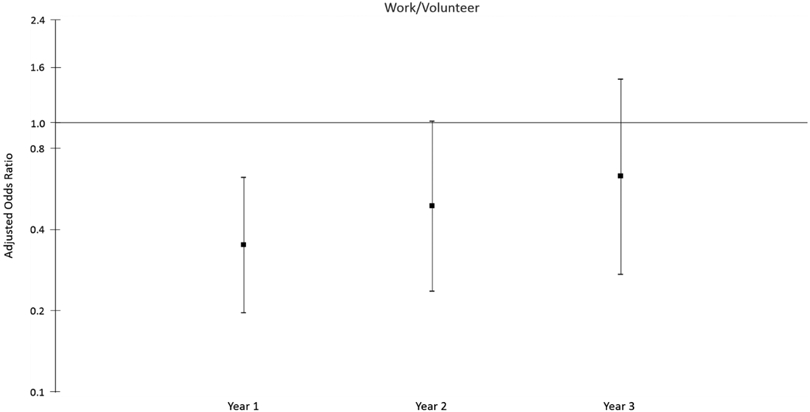
Odds of Working/Volunteering – Hip fracture patients reported lower odds of working/volunteering within the first-year post fracture (OR: 0.353, 95% CI: 0.198 - 0.629). No significant effect could be detected two (OR: 0.491, 95% CI: 0.238 - 1.014) or three years post fracture (OR: 0.633, 95% CI: 0.275 – 1.453).
Figure 4:
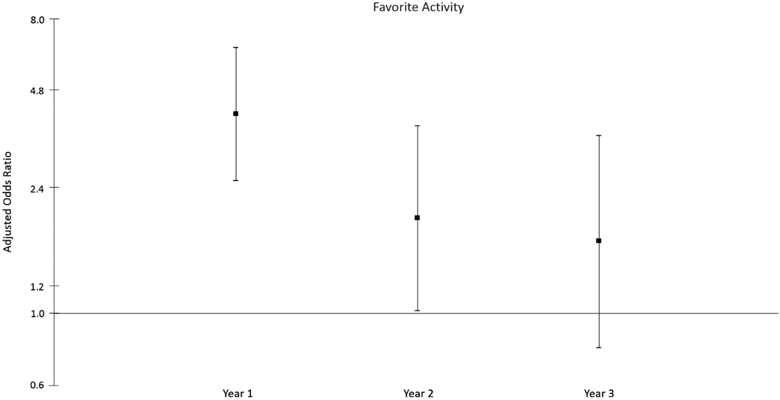
Odds of Participating in Favorite Activities – Hip fracture patients reported increased odds of being kept from favorite activities by their health within the first-year post fracture (OR: 4.086, 95% CI: 2.555 – 6.534). No significant effect could be detected two (OR: 1.959, 95% CI: 1.019 – 3.766) or three years post fracture (OR: 1.662, 95% CI: 0.785 – 3.517).
Finally, in the first year post hip fracture 20% of surviving hip fracture patients reported feeling down, depressed, or hopeless on most days compared to 10% of control subjects (AOR: 2.44, 95% CI: 1.39 – 4.28) (Figure 5). There was no statistically significant disparity between survivors in this regard two, or three years post hip fracture. The social network size of survivors did not appear to have a significant impact on driving frequency, rates of mobility, or rates of depressive symptomatology in the first year post hip fracture. However, among surviving hip fracture subjects, 40% of those with large social networks reported being kept from their favorite activity by their health compared to 68% of those with small social networks (COR: 0.32, 95% CI: 0.14 – 0.69). Similarly, among surviving hip fracture patients, 30% of those with large social networks reported working/volunteering in the last month compared to 12% of those with small social networks (COR: 2.97, 95% CI: 1.17 – 7.52). Patients with large social networks tended to have fewer comorbidities and were less likely live in an urban location (p<0.05 for both).
Figure 5:
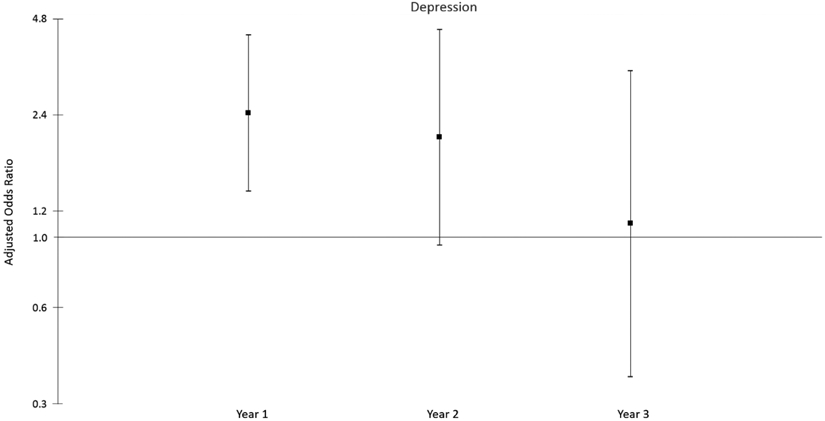
Odds of Reporting Depressive Symptomatology – Hip fracture patients reported increased odds of reporting depressive symptomatology within the first-year post fracture (OR: 2.440, 95% CI: 1.390 – 4.282). No significant effect could be detected two (OR: 2.048, 95% CI: 0.942 – 4.452) or three years post fracture (OR: 1.100, 95% CI: 0.366 – 3.305).
Discussion
Overall, we found the data from the nationally representative NHATS sample reliable. The yearly mortality rate for individuals in the NHATS sample was approximately 7.9%, which is slightly higher than the 6.6% yearly mortality rate for individuals 65 and older extrapolated from data provided by the US Centers for Disease Control and Prevention (CDC).28 The hip fracture incidence rate in the NHATS sample was 1.3% per year which is slightly higher than the 0.7% per year estimate extrapolated from data provided by the CDC and US Census Bureau.1, 29 The mortality rate one year post hip fracture in the NHATS sample was 20.2% for men and 17.3% for women. Several sources estimate the one-year mortality rate for hip fracture patients to be approximately 20% which aligns with the results presented here.2, 22, 30, 31 Others have estimated that hip fracture related mortality at one-year post fracture is between 30% and 50%, but these studies were conducted on smaller subpopulations of patients which increases the variance in the in the results reported.15, 18, 24
It is known that the consequences associated with hip fractures are major. What is not known is how hip fracture patients compare to an uninjured peer group with similar comorbidities. We found that at one year after fracture, surviving hip fracture patients are less likely to drive, less likely to leave the house, less likely to work/volunteer, and more likely to report significant depressive symptomatology. Hip fracture survivors are also more likely to report being kept from their favorite activity by their health for up to two years post fracture. Previous estimates suggest that up to 30% of surviving hip fracture patients experience significant functional limitations at one-year post hip fracture.13, 14, 20, 30, 32 Our data extend these observations to show that there tend to be improvements in function and participation among survivors in years two and three following hip fracture. With regards to emotional wellbeing, studies have documented significant increases in rates of depression among hip fracture patients.5, 13, 22 The literature also suggests that depressive symptomatology in hip fracture patients is correlated with poor outcomes, so ensuring patients are of sound mental health during the recovery process may lead to better outcomes overall.5, 6
Subject social network size was not significantly associated with driving frequency, mobility, or depressive symptomatology. However, in a univariate model, hip fracture subjects with large social networks appeared to be more likely to work/volunteer and participate in their favorite activities relative to their peers with small social networks. Previous studies have found that patients who maintain contact with their social networks throughout the recovery process experience better outcomes, and that hip fracture patients experience a significant increase in their need for social support in the months following the incident.6, 24 Encouraging patients to engage with their friends and family throughout the recovery process may have the potential to improve outcomes, and this area should be explored in future studies.
This study was not without limitations. It is important to note that patients of worse health experience higher mortality rates and are more likely to be lost to follow up, so the estimates provided here are most likely lower limits.19 We understood that those age 65–69 would likely experience significantly faster recovery and lower mortality than those age 80 +, but were unable to isolate this cohort due to power limitations. As such, the estimates provided here likely capture the lower limits of true hip fracture related declines in psychosocial wellbeing. Additionally, the dataset does not distinguish between femoral neck and intertrochanteric fractures, and the literature suggests that there may be differences in the recovery profiles of patients with different types of fractures.33, 34 There was no data regarding the type and extent of postoperative rehabilitative strategies used, which may have also induced differences in recovery dynamics. The absence of a significance in outcome measures at year 2 and 3 may be due to type II error. Social network size was used here to gauge social involvement, but a measure of social interaction quality was not available. Those with large social networks could have lower quality interactions than those with smaller social networks, but the data necessary to answer this question was not available. Finally, the NHATS survey operates on a system of yearly follow up, so higher resolution data regarding patient trajectories in the weeks and months post hip fracture were unavailable. This limited the precision with which we could describe recovery dynamics in this patient population.
Hip fracture patients and their families often ask about what they should expect from the recovery process and when they will be able to return to their pre-fracture level of function. When seeing patients who still have functional deficits within one-year post fracture, orthopedic surgeons can reassure them that most hip fracture survivors experience improvement in mobility, driving, participation in activities, and emotional well-being in years two and three after fracture. In addition, encouraging hip fracture patients to actively reconnect with their friends and family is a simple low-risk intervention that likely will improve recovery.
Acknowledgments
Source of Funding: This research was funded by the Intramural Research Program NIAMS/NIH
Footnotes
Study Design: Prospective - Patients enrolled at uniform point in course of disease and followed over time
Disclosures: The authors have no relevant disclosures.
References:
- 1.HCUPnet. Healthcare Cost and Utilization Project (HCUP) 2012. Agency for Healthcare Research and Quality, Rockville, MD: http://hcupnet.ahrq.gov. Accessed 6 March 2018. [Google Scholar]
- 2.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. Jama. 2009. October 14;302(14):1573–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. (2015)). Report on Ageing and Health. Geneva: World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1 [Google Scholar]
- 4.Young Y, Xiong K, Pruzek RM. Longitudinal functional recovery after postacute rehabilitation in older hip fracture patients: the role of cognitive impairment and implications for long-term care. Journal of the American Medical Directors Association. 2011. July 1;12(6):431–8. [DOI] [PubMed] [Google Scholar]
- 5.Givens JL, Sanft TB, Marcantonio ER. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. Journal of the American Geriatrics Society. 2008. June;56(6):1075–9. [DOI] [PubMed] [Google Scholar]
- 6.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. Journal of gerontology. 1990. May 1;45(3):M101–7. [DOI] [PubMed] [Google Scholar]
- 7.Mutran EJ, Reitzes DC, Mossey J, Fernandez ME. Social support, depression, and recovery of walking ability following hip fracture surgery. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1995. November 1;50(6):S354–61. [DOI] [PubMed] [Google Scholar]
- 8.Zidén L, Kreuter M, Frändin K. Long-term effects of home rehabilitation after hip fracture–1-year follow-up of functioning, balance confidence, and health-related quality of life in elderly people. Disability and rehabilitation. 2010. January 1;32(1):18–32. [DOI] [PubMed] [Google Scholar]
- 9.Beaupre LA, Cinats JG, Senthilselvan A, Scharfenberger A, Johnston DW, Saunders LD. Does standardized rehabilitation and discharge planning improve functional recovery in elderly patients with hip fracture?. Archives of physical medicine and rehabilitation. 2005. December 1;86(12):2231–9. [DOI] [PubMed] [Google Scholar]
- 10.Koval KJ, Skovron ML, Aharonoff GB, Zuckerman JD. Predictors of functional recovery after hip fracture in the elderly. Clinical orthopaedics and related research. 1998. March(348):22–8. [PubMed] [Google Scholar]
- 11.Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM. Factors related to functional prognosis in elderly patients after accidental hip fractures: a prospective cohort study. BMC geriatrics. 2014. December;14(1):124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID, Sherrington C. A critical review of the long-term disability outcomes following hip fracture. BMC geriatrics. 2016. December;16(1):158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boonen S, Autier P, Barette M, Vanderschueren D, Lips P, Haentjens P. Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study. Osteoporosis International. 2004. February 1;15(2):87–94. [DOI] [PubMed] [Google Scholar]
- 14.Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL, Wehren L. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. American journal of epidemiology. 2003. June 1;157(11):1023–31. [DOI] [PubMed] [Google Scholar]
- 15.Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and functional outcomes after hip fracture among nursing home residents. JAMA internal medicine. 2014. August 1;174(8):1273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pitto RP. The mortality and social prognosis of hip fractures. International orthopaedics. 1994. April 1;18(2):109–13. [DOI] [PubMed] [Google Scholar]
- 17.Shah MR, Aharonoff GB, Wolinsky P, Zuckerman JD, Koval KJ. Outcome after hip fracture in individuals ninety years of age and older. Journal of orthopaedic trauma. 2001. January 1;15(1):34–9. [DOI] [PubMed] [Google Scholar]
- 18.Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR. Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: prospective cohort study. Journal of the American Geriatrics Society. 2012. July;60(7):1268–73 [DOI] [PubMed] [Google Scholar]
- 19.Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, Felsenthal G, Kenzora J. Recovery from hip fracture in eight areas of function. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2000. September 1;55(9):M498–507. [DOI] [PubMed] [Google Scholar]
- 20.Norton Meg Butler, Robinson Elizabeth, Trevor Lee-Joe, A. John Campbell R. Declines in physical functioning attributable to hip fracture among older people: a follow-up study of case-control participants. Disability and rehabilitation. 2000. January 1;22(8):345–51. [DOI] [PubMed] [Google Scholar]
- 21.Osnes EK, Lofthus CM, Meyer HE, Falch JA, Nordsletten L, Cappelen I, Kristiansen IS. Consequences of hip fracture on activities of daily life and residential needs. Osteoporosis International. 2004. July 1;15(7):567–74. [DOI] [PubMed] [Google Scholar]
- 22.Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF, Chrischilles EA, Pavlik CE, Wallace RB, Ohsfeldt RL, Jones MP. The aftermath of hip fracture: discharge placement, functional status change, and mortality. American journal of epidemiology. 2009. October 4;170(10):1290–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marottoli R, Berkman LF, Leo-Summers L, Cooney LM Jr. Predictors of mortality and institutionalization after hip fracture: the New Haven EPESE cohort. Established Populations for Epidemiologic Studies of the Elderly. American Journal of Public Health. 1994. November;84(11):1807–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosell PA, Parker MJ. Functional outcome after hip fracture: a 1-year prospective outcome study of 275 patients. Injury. 2003. July 1;34(7):529–32. [DOI] [PubMed] [Google Scholar]
- 25.NHATS Overview. National Health and Aging Trends Study: NHATS Overview. National Institute on Aging. 2019. https://www.nhats.org/scripts/participant/NHATSOverview.htm. (accessed 16 April, 2019). [Google Scholar]
- 26.Chen SP, Bhattacharya J, Pershing S. Association of vision loss with cognition in older adults. JAMA ophthalmology. 2017. September 1;135(9):963–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolff JL, Spillman BC, Freedman VA, Kasper JD. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA internal medicine. 2016. March 1;176(3):372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy SL, Xu J, Kochanek KD, Arias E. Mortality in the United States, 2017. [PubMed] [Google Scholar]
- 29.US Census Bureau. “The Nation’s Older Population is Still Growing, Census Bureau Reports.” United States Census Bureau, 2019. April 10, www.census.gov/newsroom/press-releases/2017/cb17-100.html [Google Scholar]
- 30.Tsuboi M, Hasegawa Y, Suzuki S, Wingstrand H, Thorngren KG. Mortality and mobility after hip fracture in Japan: a ten-year follow-up. The Journal of bone and joint surgery. British volume. 2007. April;89(4):461–6. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Congress, Office of Technology Assessment, Hip Fracture Outcomes in People Age 50 and Over – Background Paper, OTA-BP-H-120 (Washington DC: U.S. Government Printing Office, July 1994). [Google Scholar]
- 32.Bertram M, Norman R, Kemp L, Vos T. Review of the long-term disability associated with hip fractures. Injury prevention. 2011. December 1;17(6):365–70. [DOI] [PubMed] [Google Scholar]
- 33.Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clinical orthopaedics and related research. 1995. January(310):150–9. [PubMed] [Google Scholar]
- 34.Fox KM, Magaziner J, Hebel JR, Kenzora JE, Kashnei TM. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 1999. December 1;54(12):M635–40. [DOI] [PubMed] [Google Scholar]


